Available online at www.sciencedirect.com
Vaccine 25 (2007) 8508–8511
Low seroprevalence of hepatitis B surface antibody among nursing
students in Taiwan: An implication for boosting
Ching-Chiang Lin
a,b,c, Chen-Kang Chang
d, Yeou-Lih Huang
c,e, Hung-Fu Tseng
f,∗aDepartment of Laboratory Medicine, Fooyin University Hospital, Pingtong, Taiwan bBasic Medical Science Education Center, Fooyin University, Kaohsiung, Taiwan cGraduate Institute of Medicine, College of Medicine, Kaohsiung Medical University, Taiwan dDepartment of Sport Management and Sport Science Research Center, National Taiwan College
of Physical Education, Taiwan
eDepartment of Biomedical Laboratory Science, Kaohsiung Medical University, Kaohsiung, Taiwan fInstitute of Health Care Management, College of Management,
National Sun Yat-sen University, No. 70, Lian-Hai Road, Kaohsiung City 804, Taiwan
Received 21 May 2007; received in revised form 1 October 2007; accepted 7 October 2007 Available online 26 October 2007
Abstract
The national hepatitis B vaccination program in Taiwan began in July 1984. The purpose of this repeated survey was to investigate the levels of anti-HBs (hepatitis B surface antibody) in the first-year students of a 5-year nursing program in Taiwan. Each year during 2000–2006, the entering students of the 5-year nursing program at Fooyin University, a vocational university located in southern Taiwan, were examined for their HBsAg and anti-HBs status using commercially available microparticle enzyme immunoassay. The seroprevalence of HBsAg (+) showed a significant trend of decrease, dropping 57% from 4.9% in 2000 to 2.1% in 2006. The seroprevalence of anti-HBs (+) also showed a significant trend of decrease, dropping 49% from 77.1% in 2000 to only 39.7% in 2006. With the relatively low seroprevalence of anti-HBs (+) of the future healthcare workers and high HBV endemicity in Taiwan, recommendation of serology test before boosting to nursing students before they proceed their clinical practice is prudent.
© 2007 Elsevier Ltd. All rights reserved.
Keywords: Hepatitis B virus; Vaccination; Seroprevalence
1. Introduction
The national hepatitis B vaccination program in Taiwan has been considered as one of the most successful and effec-tive public health programs to control hepatitis B virus (HBV) infection in the world. The national HBV vaccination pro-gram in Taiwan began in July 1984. During the first 2 years of the program, only the newborn infants of mothers who were HBsAg (hepatitis B surface antigen) carriers were vac-cinated. After July 1986, the program was extended to include all newborn infants and in July 1987 to cover all children of preschool age. All vaccinated newborns received four doses
∗Corresponding author. Tel.: +886 7 5252000x4529.
E-mail address:tsenghf2000@yahoo.com.tw(H.-F. Tseng).
of plasma-derived hepatitis B vaccine at 0, 1, 2, and 12 months of age. In addition, newborns of mother who had positive HBV e antigen were also given 0.5 mL of hepati-tis B immunoglobulin. Since November 1992, the vaccine used in this program was changed to recombinant vaccine with three doses at 0, 1, and 6 months of age. In the first 15 months after the vaccination program was implemented, hep-atitis B vaccine coverage rates for the first, second, third, and fourth doses were 88%, 86%, 84%, and 71%, respectively, among infants born to 55,620 carrier mothers[1]. The overall vaccine coverage rates during mass vaccination period until December 2002 were 96.6%, 95.2%, and 92.8% for the first, second, and third doses, respectively, among 5,188,929 new-borns, according to Center for Disease Control in Taiwan[2]. The vaccination program has significantly reduced mortality
0264-410X/$ – see front matter © 2007 Elsevier Ltd. All rights reserved. doi:10.1016/j.vaccine.2007.10.018
C.-C. Lin et al. / Vaccine 25 (2007) 8508–8511 8509
from fulminant hepatitis and the incidence of hepatocellular carcinoma in children[3].
The hepatitis B vaccine is very effective with more than 90% vaccinees reached 10 mIU/mL, the suggested protec-tive levels of anti-HBs (hepatitis B surface antibody), after
a primary course [4,5]. The proportion of vaccinees with
protective anti-HBs levels decreased to approximately 80% after 5 years and 50–70% after 10–12 years of the primary
vaccination [6–8]. It has been shown that approximately
30–62% Taiwanese children had anti-HBs levels lower than 10 mIU/mL 15 years after neonatal vaccination, suggesting waning immunity. Although immunologic memory was still present in all subjects 10 years after the primary vaccination regardless of their anti-HBs levels[9,10], HB core anti-gen was detected in 4.4% of apparently healthy Taiwanese children whose anti-HBs levels were below 10 mIU/mL[11]. A single booster administered several years after the pri-mary vaccination could increase anti-HBs levels to higher
than 10 mIU/mL in majority of the subjects [11]. Several
international agencies have recommended against the use of boosters in general population as no vaccinee has been identi-fied as a carrier several years after the primary immunization
[12–14]. On the other hand, advisory organizations in sev-eral countries stated that boosters should be administered in high-risk groups such as healthcare workers if their anti-HBs
levels were below 10 mIU/mL[15–17].
The rates of exposure to HBV were estimated as 0.015–0.028 per healthcare worker per year in Taiwan in dif-ferent categories of related jobs. There are estimated 308–924 healthcare workers at risk for seroconversion to HBV per year, based on 10–30% seroconversion rate after a needle
stick injury [18]. However, most of the recommendations
of using boosters in healthcare workers are based on sero-logical data from general populations. There is no available information on the seroprevalence of anti-HBs in Taiwanese healthcare workers to provide solid evidence for policy on boosters. The purpose of this study was to investigate the lev-els of anti-HBs in the first-year students of a 5-year nursing program in Taiwan.
2. Methods 2.1. Subjects
Each year during 2000–2006, the entering students of the 5-year nursing program at Fooyin University, a vocational university located in southern Taiwan, were examined for their HBsAg and anti-HBs status. The 5-year nursing pro-gram is designed for students graduated from regular junior high schools. The majority of the students entered the pro-gram at the age of 15. According to the statistics of Ministry of Education, the study population represented 14.5% and 34.6% of all students entering the similar program nation-wide and in southern Taiwan in 2003, respectively. These proportions became 11.8% and 24.6% in 2006 because the
total number of students entering the similar program in Tai-wan has increased. The subjects in this study represented a cohort of individuals who participated in the first 7 years of the national HBV vaccination program in Taiwan. Students entering in 2000 and 2001 experienced the vaccination pro-gram covered newborns of HBsAg carrier mothers, while students entering from 2002 to 2006 experienced the uni-versal newborn vaccination. The study was approved by the Institution Review Board of Fooyin University Hospital (No. FYH-IRB-96003).
2.2. Serology and statistical tests
All studied individuals received tests for the presence of HBsAg and anti-HBs using commercially available microparticle enzyme immunoassay (AxSYM, Abbott, North Chicago, IL, USA). Samples with HBsAg greater than 2.0 S/N were considered positive. Samples with anti-HBs above 10 mIU/mL were considered positive. The differences in the prevalence of HBsAg and anti-HBs among students entering in different years were examined byχ2-test for linear trend using SPSS for Windows 10.0 (SPSS Inc., Chicago, IL, USA). A p-value less than 0.05 was considered statistically significant. The sample size of over 850 each year allowed us to estimate the seroprevalence with 95% confidence interval less than 3.4%, assuming the seroprevalence was 50% and the sampling fraction was 25%.
3. Results
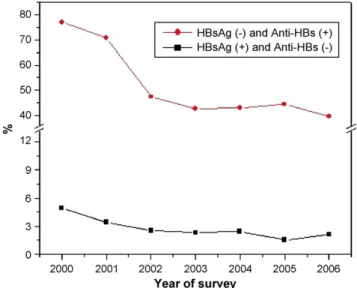
There were 6184 nursing students (97.2% female, 2.8% male) in this study. The seroprevalence of HBsAg (+) showed a significant trend of decrease, dropping 57% from 4.9% in 2000 to 2.1% in 2006.The HBsAg (+) seroprevalence of sub-jects who were born in the first 2 years of the vaccination program when only newborns of HBsAg (+) mothers were vaccinated was 4.2%, comparing to only 2.2% in subjects who were universally vaccinated during infancy. The dif-ference was statistically significant. The seroprevalence of anti-HBs (+) also showed a significant trend of decrease, dropping 49% from 77.1% in 2000 to only 39.7% in 2006. The anti-HBs (+) seroprevalence of those who were born in the first 2 years of vaccination was 74.0%, while it was only 43.4% for students who had been vaccinated universally during infancy (Table 1;Fig. 1).
4. Discussion
This study showed that in this group of future healthcare workers, 26% of selected vaccination cohort and 56.6% of mass vaccination cohort had undetectable level of anti-HBs. In a nationwide study in Taiwan, 38% of the selected vac-cination cohort and 34.6% of mass vacvac-cination cohort had undetectable level of anti-HBs when entering elementary
8510 C.-C. Lin et al. / Vaccine 25 (2007) 8508–8511
Table 1
HBsAg and anti-HBs status for the first-year nursing students surveyed during 2000–2006 in southern Taiwan
Year of survey 2000 2001 2002 2003 2004 2005 2006 Birth cohort of entering students September 1984–August 1985 September 1985–August 1986 September 1986–August 1987 September 1987–August 1988 September 1988–August 1989 September 1989–August 1990 September 1990–August 1991 Vaccination
program for the cohort Selected vaccination program Mass vaccination program Number of students 974 957 840 824 848 870 871 HBsAg (−) and anti-HBs (−) 175 (18.0%) 246 (25.7%) 421 (50.1%) 454 (55.1%) 463 (54.6%) 471 (54.1%) 507 (58.2%) (16.0–20.0%)a (23.0–28.4%) (46.7–53.5%) (51.7–58.5%) (51.3–57.9%) (50.8–57.4%) (54.9–61.5%) HBsAg (−) and anti-HBs (+) 751 (77.1%) 678 (70.8%) 398 (47.4%) 351 (42.6%) 365 (43.0%) 386 (44.4%) 346 (39.7%) (74.5–79.7%) (67.9–73.7%) (44.0–50.8%) (39.2–46.0%) (39.7–46.3%) (41.1–47.7%) (36.5–42.9%) HBsAg (+) and anti-HBs (−) 48 (4.9%) 33 (3.4%) 21 (2.5%) 19 (2.3%) 20 (2.4%) 13 (1.5%) 18 (2.1%) (3.5–6.3%) (2.3–4.5%) (1.5–3.5%) (1.3–3.3%) (1.4–3.4%) (0.7–2.3%) (1.1–3.1%) a95% confidence interval.
school[19]. This proportion increased to 60.1% in adoles-cents who were born in mass vaccination era[20].
The HBsAg (+) seroprevalence rate in selected vaccination cohort in our study was similar to that reported by Lin et al., which showed that the HBsAg carrier rates for teenagers who were born in 1985 and 1986 were 4.7% and 3.4% in eastern Taiwan[21]. The mass vaccination program has resulted in a significant decline in HBsAg (+) seroprevalence rate due to reduced incidence of vertical and horizontal transmission.
Shiao et al. reported that 87.3% of the healthcare work-ers in Taiwan had experienced recent sharps injuries [18]. The risk of transmission of HBV to nonimmuned healthcare workers after a needle stick depends on the titer of viri-ons in the contaminant and correlates with the presence or absence of hepatitis B e antigen in the source patient, rang-ing from 2% (HBeAg negative) to 40% (HBeAg positive)
Fig. 1. Seroprevalence of HBsAg (+) and anti-HBs (+) among nursing stu-dents in Taiwan, 2000–2006.
[22,23]. Other tissues and body fluid may also be infectious
[24]. The virus can be transferred through undetected cuts, pre-existing breaches in the epithelium, or bites[17]. With the estimated HBV seroprevalence rate of 15–21% in Taiwan
[25], the risk for infection of HBV among healthcare workers could be considerable.
It has been shown that a booster administered several years after the primary vaccination can induce a protective level of anti-HBs in almost all subjects[9]. The guidelines recently provided by The Steering Committee for the Prevention and Control of Infectious Diseases in Asia include boost-ing approximately 10–15 years after the primary vaccination and boosting healthcare workers based on the endemicity of the particular country[26]. On the other hand, European Consensus Group on Hepatitis B Immunity recommended against providing boosters to healthcare workers because no known instance of any patient being infected by health-care workers who had lost their immunity and developed a breakthrough infection[12]. However, they did not con-sider the incidence of healthcare workers being infected by patients. The Immunization Practices Advisory Committee in
US[13]and National Advisory Committee on Immunization
in Canada[27]also recommended against providing boosters to healthcare workers. In Taiwan and other Asian countries where HBV endemicity was higher than that in Europe and North America, the likelihood of non-protected healthcare workers being exposed to HBV may be higher compared to that in Europe and North America.
The necessity of booster vaccination to prevent hepatitis B has been under debate in the last decade and more studies are needed to elucidate this issue. A recent study has sug-gested that universal HBV vaccination provides long-term protection up to 20 years, and a universal booster is not necessary before adulthood in Taiwan[28]. The healthcare workers whose antibody titer waned below the protective level are probably protected from the HBV infection due
C.-C. Lin et al. / Vaccine 25 (2007) 8508–8511 8511
to immunologic memory[9,10]. However, those who were
non-responders to the vaccination are susceptible to the infection. Unfortunately, it is often difficult to identify the non-responders because post-vaccination antibody testing
has not been a common practice [29]. With the relatively
low seroprevalence of anti-HBs (+) in these future healthcare workers and high HBV endemicity in Taiwan, recommen-dation of serology test before boosting to nursing students before they proceed their clinical practice is prudent.
Acknowledgement
Conflict of interest statement: There is no financial or other
relationships that might lead to a conflict of interests.
References
[1] Chen DS, Hsu NH, Sung JL, Hsu TC, Hsu ST, Kuo YT, et al. A mass vaccination program in Taiwan against hepatitis B virus infec-tion in infants of hepatitis B surface antigen-carrier mothers. JAMA 1987;257:2597–603.
[2] Chien YC, Jan CF, Kuo HS, Chen CJ. Nationwide hepatitis B vacci-nation program in Taiwan: effectiveness in the 20 years after it was launched. Epidemiol Rev 2006;28:126–35.
[3] Chang MH, Shau WY, Chen CJ, Wu TC, Kong MS, Liang DC, et al. Hepatitis B vaccination and hepatocellular carcinoma rates in boys and girls. JAMA 2000;284:3040–2.
[4] Lee CY, Huang LM, Chang MH, Hsu CY, Wu SJ, Sung JL, et al. The protective efficacy of recombinant hepatitis B vaccine in new-born infants of hepatitis B e antigen-positive-hepatitis B surface antigen carrier mothers. Pediatr Infect Dis J 1991;10:299–303.
[5] Stevens CE, Toy PT, Taylor PE, Lee T, Yip HY. Prospects for control of hepatitis B virus infection: implications of childhood vaccination and long-term protection. Pediatrics 1992;90:170–3.
[6] Lee PI, Lee CY, Huang LM, Chang MH. Long-term efficacy of recom-binant hepatitis B vaccine and risk of natural infection in infants born to mothers with hepatitis B e antigen. J Pediatr 1995;126:716–21. [7] Coursaget P, Leboulleux D, Soumare M, Le Cann P, Yvonnet B, Chiron
JP, et al. Twelve-year follow-up study of hepatitis B immunization of Senegalese infants. J Hepatol 1994;21:250–4.
[8] Resti M, Azzari C, Mannelli F, Rossi ME, Lionetti P, Vierucci A. Ten-year follow-up study of neonatal hepatitis B immunization: are booster injections indicated? Vaccine 1997;15:1338–40.
[9] Huang LM, Chiang BL, Lee CY, Lee PI, Chi WK, Chang MH. Long-term response to hepatitis B vaccination and response to booster in children born to mothers with hepatitis B e antigen. Hepatology 1999;29:954–9.
[10] Wang RX, Guo Y, Yang CH, Song Y, Chen J, Pang FS, et al. Can HB vaccine yield a booster effect on individuals with positive serum anti-HBs and anti-HBc markers? World J Gastroenterol 2004;10:306–8. [11] Lu CY, Chiang BL, Chi WK, Chang MH, Ni YH, Hsu HM, et al. Waning immunity to plasma-derived hepatitis B vaccine and the need for boost-ers 15 years after neonatal vaccination. Hepatology 2004;40:1415–20.
[12] European Consensus Group on Hepatitis B Immunity. Are booster immunisations needed for lifelong hepatitis B immunity? Lancet 2000;355:561–65.
[13] Immunization Practices Advisory Committee. Hepatitis B virus: a comprehensive strategy for eliminating transmission in the United States through universal childhood vaccination. Recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR Recomm Rep 1991;40:1–25.
[14] Holton D. Revised guidelines for booster vaccination against hepatitis B. Can Med Assoc J 1992;147:1029–32.
[15] Thompson SC, Norris M. Hepatitis B vaccination of personnel employed in Victorian hospitals: are those at risk adequately protected? Infect Control Hosp Epidemiol 1999;20:51–4.
[16] Barash C, Conn MI, DiMarino Jr AJ, Marzano J, Allen ML. Serologic hepatitis B immunity in vaccinated health care workers. Arch Intern Med 1999;159:1481–3.
[17] Davies GR, Porra M. The need for post-vaccination serology and the timing of booster vaccinations against hepatitis B in dental health care workers. Aust Dent J 1994;39:238–41.
[18] Shiao J, Guo L, McLaws ML. Estimation of the risk of bloodborne pathogens to health care workers after a needlestick injury in Taiwan. Am J Infect Control 2002;30:15–20.
[19] Hsu HM, Lu CF, Lee SC, Lin SR, Chen DS. Seroepidemiologic survey for hepatitis B virus infection in Taiwan: the effect of hepatitis B mass immunization. J Infect Dis 1999;179:367–70.
[20] Lu SN, Chen CH, Chen TM, Lee PL, Wang JH, Tung HD, et al. Hepatitis B virus infection in adolescents in a rural township—15 years subsequent to mass hepatitis B vaccination in Taiwan. Vaccine 2006;24:759–65.
[21] Lin HH, Wang LY, Hu CT, Huang SC, Huang LC, Lin SS, et al. Decline of hepatitis B carrier rate in vaccinated and unvaccinated subjects: six-teen years after newborn vaccination program in Taiwan. J Med Virol 2003;69:471–4.
[22] Alter HJ, Seeff LB, Kaplan PM, McAuliffe VJ, Wright EC, Gerin JL, et al. Type B hepatitis: the infectivity of blood positive for e antigen and DNA polymerase after accidental needlestick exposure. N Engl J Med 1976;295:909–13.
[23] Werner BG, Grady GF. Accidental hepatitis-B-surface-antigen-positive inoculations. Use of e antigen to estimate infectivity. Ann Intern Med 1982;97:367–9.
[24] Karayiannis P, Novick DM, Lok AS, Fowler MJ, Monjardino J, Thomas HC. Hepatitis B virus DNA in saliva, urine, and seminal fluid of carriers of hepatitis B e antigen. Br Med J 1985;290:1853– 5.
[25] Chen HL, Chang MH, Ni YH, Hsu HY, Lee PI, Lee CY, et al. Seroepi-demiology of hepatitis B virus infection in children: ten years of mass vaccination in Taiwan. JAMA 1996;276:906–8.
[26] John TJ, Cooksley G. Hepatitis B vaccine boosters: is there a clin-ical need in high endemicity populations? J Gastroenterol Hepatol 2005;20:5–10.
[27] National Advisory Committee on Immunization (NACI). Revised guidelines for booster vaccination against hepatitis B. Can Commun Dis Rep 1992;18:121–22.
[28] Ni YH, Huang LM, Chang MH, Yen CJ, Lu CY, You SL, et al. Two decades of universal hepatitis B vaccination in taiwan: impact and implication for future strategies. Gastroenterology 2007;132:1287–93. [29] Gerberding JL. Management of occupational exposures to blood-borne