ISSN: 1524-4628
Copyright © 2001 American Heart Association. All rights reserved. Print ISSN: 0039-2499. Online Stroke is published by the American Heart Association. 7272 Greenville Avenue, Dallas, TX 72514
2001;32;2265-2271
Stroke
and Yuan-Teh Lee
Ta-Chen Su, Jiann-Shing Jeng, Kuo-Liong Chien, Fung-Chang Sung, Hsiu-Ching Hsu
Community-Based Study in Taiwan
Hypertension Status Is the Major Determinant of Carotid Atherosclerosis: A
http://stroke.ahajournals.org/cgi/content/full/32/10/2265
located on the World Wide Web at:
The online version of this article, along with updated information and services, is
http://www.lww.com/reprints
Reprints: Information about reprints can be found online at
journalpermissions@lww.com 410-528-8550. E-mail:
Fax: Kluwer Health, 351 West Camden Street, Baltimore, MD 21202-2436. Phone: 410-528-4050. Permissions: Permissions & Rights Desk, Lippincott Williams & Wilkins, a division of Wolters
http://stroke.ahajournals.org/subscriptions/
Subscriptions: Information about subscribing to Stroke is online at
at NATIONAL TAIWAN UNIV on April 29, 2009 stroke.ahajournals.org
Atherosclerosis
A Community-Based Study in Taiwan
Ta-Chen Su, MD; Jiann-Shing Jeng, MD; Kuo-Liong Chien, MD; Fung-Chang Sung, PhD, MPH;
Hsiu-Ching Hsu, PhD; Yuan-Teh Lee, MD, PhD
Background and Purpose—Extracranial carotid artery (ECCA) atherosclerosis has been associated with
hypertension-related stroke. The present study was aimed at investigating the determinants of ECCA atherosclerosis in patients with hypertension in Taiwan.
Methods—The extent and severity of ECCA atherosclerosis were measured by high-resolution B-mode ultrasonography
and expressed as maximal intima-media thickness (IMT) of the common carotid artery, ECCA plaque score, and carotid stenosisⱖ50%. From July through December 1996, 263 hypertensive patients (146 with hypertension and 117 with borderline hypertension) and 270 normotensive adults from the Chin-Shan Community Cardiovascular Cohort participated in this study. Risk factors and ECCA atherosclerosis were stratified by the blood pressure status.
Results—A significant dose-response relationship was found between the status of hypertension and the severity of carotid
atherosclerosis. Multivariate logistic regression models revealed that hypertension (including borderline), male gender, smoking, and age ⱖ65 years significantly increased the risk of thicker IMT. The risk of ECCA plaque score ⬎6 increased significantly in conjunction with hypertension, age ⱖ65 years, left ventricular hypertrophy on ECG, and smoking. However, hypertension and smoking were the 2 evident determinants of carotid stenosis ⱖ50% after adjustment for other covariates. Compared with the normotensive subjects, the ORs (and 95% CIs) for the hypertensive patients to develop carotid atherosclerosis were 5.0 (3.0 to 8.4) indexed by maximal common carotid artery IMTⱖ75th percentile, 3.7 (1.8 to 7.9) by ECCA score⬎6, and 4.8 (1.4 to 16.5) by carotid stenosis ⱖ50%.
Conclusions—Hypertension strongly influence carotid atherosclerosis. Our findings reinforce the hypothesis that
hypertension has a major role in the pathogenesis of atherosclerosis. (Stroke. 2001;32:2265-2271.)
Key Words: Atherosclerosis 䡲 Carotid arteries 䡲 Hypertension 䡲 Taiwan
O
ver the past 2 decades in Taiwan, cerebrovascular and cardiovascular diseases have ranked as the second and the fourth leading causes of death, respectively, and have been the most important causes of morbidity and mortality, especially among the elderly.1 Hypertension is one of themost important risk factors in the development of atheroscle-rosis, coronary artery diseases (CAD), and cerebrovascular disease (CVD).2– 4 Common carotid artery (CCA)
intima-media thickness (IMT), extracranial carotid artery (ECCA) atherosclerosis, and maximal carotid stenosis have been proved to have significant association with CAD and CVD.5– 8
Bodies of evidence support early detection of atheroscle-rosis and its associated risk factors in the prevention of atherosclerotic diseases. The measurement of carotid athero-sclerosis by ultrasound has been widely used for its simple and reliable detection of early preclinical atherosclerosis9,10
and for the high correlation between measured IMT and the actual pathological change it produces.11Some studies have
documented the association between carotid atherosclerosis and hypertension.12–14 However, the progressive structural
changes in extracranial carotid beds in response to blood pressure increment remain unclear. This association was addressed in the present study on the basis of data obtained from a cohort of the Chin-Shan Community Cardiovascular Cohort (CCCC) study in Taiwan.15–18The other risk factors
that are associated with carotid atherosclerosis were also investigated.
Subjects and Methods
Study Subjects
The CCCC study has been established since 1990 as a longitudinal, prospective, community-based surveillance on cardiovascular and cerebrovascular diseases. There were 3602 participants agedⱖ35
Received December 13, 2000; final revision received April 4, 2001; accepted June 28, 2001.
From the Departments of Internal Medicine (T.-C.S., K.-L.C., H.-C.H., Y.-T.L.) and Neurology (J.-S.J.), National Taiwan University Hospital, and College of Public Health (F.-C.S.), National Taiwan University, Taipei, Taiwan.
Correspondence and reprint requests to Yuan-Teh Lee, MD, PhD, FACC, Professor, Internal Medicine, College of Medicine, National Taiwan University, and Superintendent of National Taiwan University Hospital, No. 7, Chung-Shan South Road, Taipei 10020, Taiwan. E-mail ytlee@ha.mc.ntu.edu.tw
© 2001 American Heart Association, Inc.
Stroke is available at http://www.strokeaha.org
years residing in the community of Chin-Shan, 20 miles north of Taipei, Taiwan.15–18Sociodemographics, medical history, and
vas-cular risk factors were evaluated in each subject. Physical examina-tion included general condiexamina-tion, body weight, body height, waist and hip circumferences, and brachial and ankle blood pressures. ECG, echocardiography, and carotid ultrasonography (since 1994) were performed for every subject.
For the carotid atherosclerosis evaluation conducted from July through December 1996, 1802 individuals were randomly selected as study population from the CCCC study cohort and participated in the biennial follow-up evaluation in 1994. Among them, 451 subjects were classified as cases of hypertension or borderline hypertension. From the rest of 1351 normotensives, 451 were randomly selected by frequency matching for gender and age. These individuals were contacted by telephone and home visit for participation: 146 hyper-tensives, 117 borderline hyperhyper-tensives, and 270 normotensive con-trols received the carotid atherosclerosis evaluation throughout the study. There were no significant differences between participants and nonparticipants in regard to the distribution of age and sex and the prevalence rates of hypertension, diabetes mellitus, and smoking.
Assessment of Vascular Risk Factors
Hypertension was defined according to the criteria established by the Fifth Joint National Committee on Detection, Evaluation, and Treatment.19Blood pressure measurements were performed with a
mercury sphygmomanometer in a standardized fashion cuff size adjusted to the circumference of the arm. The arm was placed with the cuff at the level of heart. Blood pressure was recorded using the means of 2 measurements taken after 5 minutes of rest in the supine position. Systolic and diastolic blood pressures were defined accord-ing to Korotkoff sounds I and V. Diabetes mellitus was defined as fasting serum glucose level ofⱖ7.8 mmol/L (140 mg/dL) in at least 2 different measurements and/or a history of use of oral hypoglyce-mic agents or insulin injection. Overweight was defined as a body mass index (BMI) ofⱖ26.4 kg/m2, which was about 20%
over-weight, on the basis of recent Health and Nutrition Examination Surveys in Taiwan for Chinese adults.20
Data on alcohol use and smoking were obtained by self-reported questionnaire. Alcohol use was calculated from frequency and amount and was summarized as the average number of alcoholic drinks consumed per week.
Evident cardiovascular disease was defined as the presence of history of acute myocardial infarction or angina pectoris verified by coronary angiogram and/or medical records reviewed by at least one cardiologist. CVD was defined as the presence of history of stroke or transient ischemic attack verified by at least one neurologist. Left ventricular hypertrophy (LVH) was diagnosed from ECG according to the criteria of LVH defined in the Physician’s Guide to Marquette Electronics Resting ECG.21
ECCA Ultrasonographic Measurement
Carotid atherosclerosis was assessed by using 3 indexes: the maxi-mal CCA IMT, the ECCA plaque score, and the maximaxi-mal ECCA stenosis. A Hewlett-Packard SONO 1500 ultrasound system, equipped with a 7.5-MHz real-time B-mode scanner and a 5.6-MHz pulsed-Doppler mode scanner, was used for the evaluation. The examination included the observation of longitudinal and transverse views of the ECCA bilaterally. Trained physicians performed carotid ultrasonography while patient was supine with the neck extended in mild lateral rotation. For future and subsequent off-line analysis, all scans were recorded on super-VHS videotape.
The maximal IMT on the CCA proximal to the carotid bifurcation was obtained bilaterally. The CCA1 and CCA2 are points located 0 to 1 cm and 1 to 2 cm, respectively, on the CCA distal from the carotid bifurcation. The IMT of the posterior wall of the distal CCA was measured as the distance from the leading edge of the first echogenic line (lumen-intima interface) to the leading edge of the second line (media-adventitia interface).22Observers were blinded to
subjects’ health status and risk factors. The interobserver correlation coefficients were 0.86 to 0.93, and the intraobserver correlation coefficients were 0.70 to 0.87 for both sides of CCA IMT
measure-ments.23 Maximal CCA IMT ⱖ75th percentile was considered
thicker IMT.
The plaque scoring quantified method has been mentioned else-where.24,25In brief, carotid artery segments, including the proximal
CCA (⬎20 mm proximal to the bulb bifurcation), distal CCA, bulb, internal carotid artery, and external carotid artery were examined bilaterally. A grade was assigned for each chosen segment: grade 0 for normal or no observable plaque, grade 1 for 1 small plaque with diameter stenosis⬍30%, grade 2 for 1 medium plaque with 30% to 49% diameter stenosis or multiple small plaques, grade 3 for 1 large plaque with 50% to 99% diameter stenosis or multiple plaques with at least 1 medium plaque, and grade 4 for 100% occlusion. The plaque score was computed by summing the plaque grades at each of the segments of the ECCA.
Carotid stenosis was assessed by the velocity criteria and the real-time B-mode images. It was computed from the difference in residual lumen diameter and the original diameter at the site of maximal stenosis in each segment of the arteries and by dividing each difference by the original diameter. Carotid stenosis ofⱖ50% was also defined in the presence of peak systolic velocityⱖ1.25 m/s.24Reproducibility of plaque grade scoring showed good
agree-ment, with a value of 0.70.25ECCA plaque score⬎6 or a maximal
carotid stenosis ⱖ50% was defined as significant carotid atherosclerosis.
Lipid and Lipoprotein Assays
Serum levels of lipid profiles, including total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides, were analyzed in a central laboratory, as described previously.15–18Blood samples of 9
to 12 hours overnight fasting for lipid and glucose determination were drawn from the antecubital vein with the patient in a seated position.
Statistical Analyses
In the data analysis, clinical features and cardiovascular risk factors of study subjects were first compared by hypertension status, ie, between hypertensives and controls. Continuous variables are ex-pressed as mean⫾SD. Both t test and ANOVA were used to make comparisons among these groups. For categorical data, the2test for
trend was used to test the significance level among different groups. The average carotid artery IMT measurements at CCA1 and CCA2 on the right side and on the left side were compared separately, also by hypertension status. The frequency of ECCA plaques was compared by hypertension status. Plaque scores were also stratified into 4 levels (0, 1 to 3, 4 to 6, and⬎6) to evaluate the differences in the percentage distributions of ECCA plaques between hypertensives and controls. Percentages of subjects with stenosis at the 50% level and above were evaluated as well. The strength of associations between carotid atherosclerosis and hypertension and other potential risk factors was measured in terms of ORs in the 95% CIs by using multivariate logistic regression analysis. An IMT at or above the 75th percentile, ECCA score⬎6, or carotid stenosis at the 50% level and above was considered as an indicator of significant carotid atherosclerosis in performing these analyses. Significant variables identified from the univariate analyses were included as covariate in the multivariate logistic regression models with stepwise procedure to estimate the risks of thicker IMT, significant ECCA plaque score, and significant carotid stenosis.
Results
No significant differences in the distributions of sex, average ages, and lifestyles were found among hypertensives patients and normotensive control subjects (Table 1). Normotensives were significantly less likely than hypertensives to have hypertriglyceridemia, diabetes mellitus, CVD, and LVH (on ECG), and they had lower average BMI and waist-to-hip ratio (P⬍0.001).
2266 Stroke October 2001
at NATIONAL TAIWAN UNIV on April 29, 2009 stroke.ahajournals.org
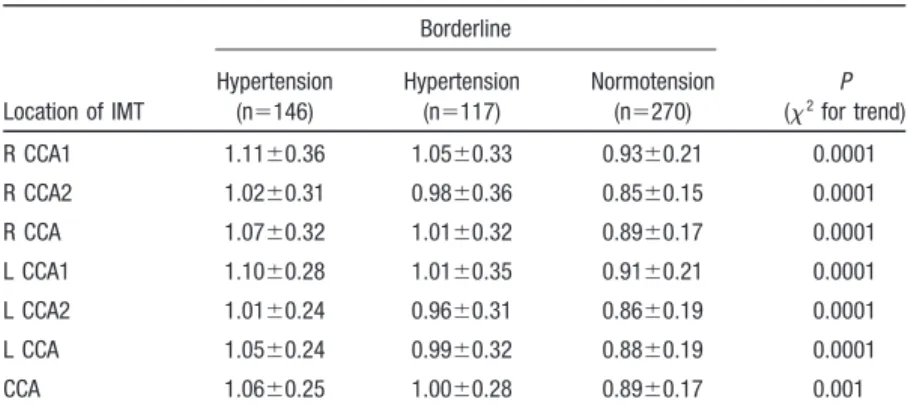
Average CCA IMT measurements at different carotid locations all showed significant trends (P⬍0.001) of IMT progression, as graded by the extent of hypertension (Table 2). The overall average CCA increased from 0.89⫾0.17 mm for normotensives, 1.00⫾0.28 mm for borderline hyperten-sives, and 1.06⫾0.25 mm for hypertensives.
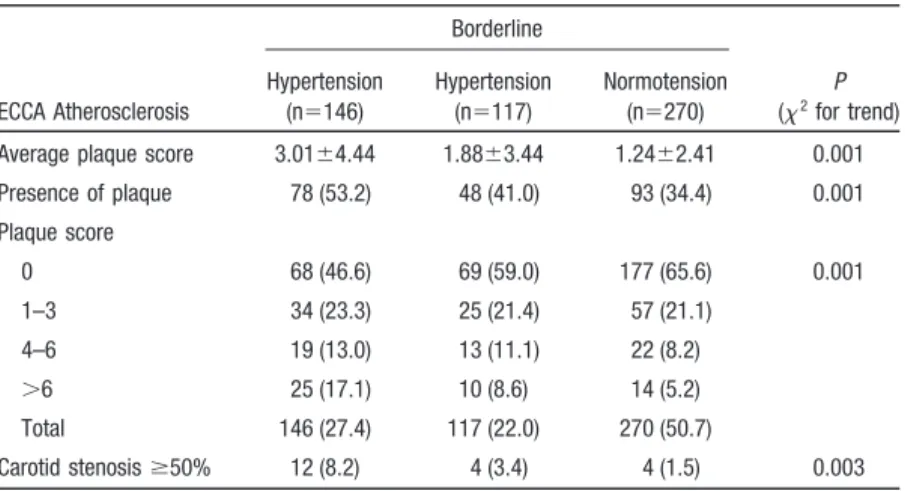
Table 3 shows significant trends of carotid plaque forma-tions by the status of blood pressure. About 53% of hyper-tensives were observed to have plaques with an average plaque score of 3.01, while the corresponding values
de-creased to 41% with 1.88 score for borderline hypertensives, and to 34% with 1.24 score for normotensives. About 17.6% of the hypertensives (the highest prevalence) and 5.2% of the normotensives (the lowest prevalence) had plaque scores⬎6. The prevalence of carotid stenosis at the 50% level and above was observed to be highest in hypertensives as well.
Multivariate logistic regression analyses showed that hy-pertension, being a male, smoking, and age ⱖ65 years increased the risk of thicker IMT after adjustment for other associated factors (Table 4). However, the results also noted
TABLE 1. Clinical Features and Cardiovascular Risk Factors by Hypertension Status Characteristic Borderline P Hypertension (n⫽146) Hypertension (n⫽117) Normotension (n⫽270) Male, % 44.5 42.7 41.8 0.87 Age, y 65.7⫾9.0 63.8⫾10.7 64.3⫾9.5 0.26 Systolic BP, mm Hg 152.2⫾19.2 140.2⫾18.9 122.9⫾16.6 0.0001 Diastolic BP, mm Hg 85.9⫾10.3 83.9⫾9.9 76.6⫾9.0 0.0001 Body mass index, kg/m2 25.4⫾3.7 24.6⫾3.5 23.8⫾4.0 0.0001
Waist-to-hip ratio 0.89⫾0.07 0.89⫾0.07 0.87⫾0.07 0.0015 Cholesterolⱖ6.21 mmol/L, % 35.6 36.7 34.1 0.87 Triglycerideⱖ2.26 mmol/L, % 19.9 14.5 8.9 0.006 Diabetes mellitus, % 28.1 14.5 13.3 0.001 Smoke, % Current 21.9 17.1 20.7 Former 9.6 6.0 6.3 0.53 Never 68.5 76.9 73.0 Alcohol, % Current 17.1 24.8 23.3 Former 13.7 6.0 10.0 0.19 Never 69.2 69.2 66.7 CVD, % 10.3 3.2 3.0 0.003 CAD, % 4.1 4.3 3.3 0.87 LVH on ECG, % 17.1 9.4 6.3 0.002
Values for age, systolic and diastolic blood pressures (BPs), body mass index, and waist-to-hip ratio are mean⫾SD.
TABLE 2. Measurements of IMT in Different CCA Locations, by Hypertension Status Location of IMT Borderline P (2for trend) Hypertension (n⫽146) Hypertension (n⫽117) Normotension (n⫽270) R CCA1 1.11⫾0.36 1.05⫾0.33 0.93⫾0.21 0.0001 R CCA2 1.02⫾0.31 0.98⫾0.36 0.85⫾0.15 0.0001 R CCA 1.07⫾0.32 1.01⫾0.32 0.89⫾0.17 0.0001 L CCA1 1.10⫾0.28 1.01⫾0.35 0.91⫾0.21 0.0001 L CCA2 1.01⫾0.24 0.96⫾0.31 0.86⫾0.19 0.0001 L CCA 1.05⫾0.24 0.99⫾0.32 0.88⫾0.19 0.0001 CCA 1.06⫾0.25 1.00⫾0.28 0.89⫾0.17 0.001
Values are mean⫾SD thickening, in millimeters. R CCA indicates mean IMT of both R CCA1 and R CCA2; L CCA, mean IMT of both L CCA1 and L CCA2; and CCA, mean IMT of both R CCA and L CCA.
that an inverse relationship was found between subjects with regular alcohol consumption and CCA IMT (OR 0.5; 95% CI 0.2 to 0.9). Hypertension remained consistently a strong risk factor of ECCA atherosclerosis by the other 2 indexes (ECCA score ⬎6 and carotid stenosis ⱖ50%). When the subjects with ECCA score⬎6 were evaluated, age ⱖ65 years, current smoking, and LVH on ECG were also found to be significant covariates. However, if significant carotid stenosis (ⱖ50% stenosis) was considered, hypertension and current smoking were the 2 evident determinants after adjustment for other covariates. Compared with normotensives, the corresponding ORs (95% CIs) for development of carotid atherosclerosis in hypertensives were 5.0 (3.0 to 8.4) indexed by maximal CCA IMTⱖ75th percentile, 3.7 (1.8 to 7.9) indexed by significant ECCA score ⬎6, and 4.8 (1.4 to 16.5) indexed by carotid stenosisⱖ50%.
Discussion
Stroke is prevalent in Taiwan.26The present study is well
in line with other findings on the association between IMT
and hypertension. Furthermore, we demonstrated that a dose-response relationship exists between them and that hypertension is the most important risk factor for carotid IMT and carotid atherosclerosis. Cross-sectional analysis suggests that age is related to carotid wall thickening in all carotid beds, and carotid wall IMT is greater in men than in women aged 45 to 64 years in the Atherosclerosis Risk in Communities (ARIC) Study.27 The Cardiovascular
Health Study28 (CHS) revealed that among the elderly
(ⱖ65 years), women have less carotid atherosclerosis than men, and the prevalence and severity of carotid artery disease continue to increase with age even in the late decades of life. Prevalence of vascular structural adapta-tion and increased risk factors associated with aging are atherosclerosis related.
A significantly beneficial effect of alcohol consumption on the CCA IMT was observed in this study, although the relationship between alcohol use and carotid atherosclero-sis remains controversial. An inverse relationship between
TABLE 3. Average Plaque Scores and Distributions of ECCA Plaque, ECCA Plaque Score, and Carotid Stenosis >50%, by Hypertension Status
ECCA Atherosclerosis Borderline P (2for trend) Hypertension (n⫽146) Hypertension (n⫽117) Normotension (n⫽270)
Average plaque score 3.01⫾4.44 1.88⫾3.44 1.24⫾2.41 0.001 Presence of plaque 78 (53.2) 48 (41.0) 93 (34.4) 0.001 Plaque score 0 68 (46.6) 69 (59.0) 177 (65.6) 0.001 1–3 34 (23.3) 25 (21.4) 57 (21.1) 4–6 19 (13.0) 13 (11.1) 22 (8.2) ⬎6 25 (17.1) 10 (8.6) 14 (5.2) Total 146 (27.4) 117 (22.0) 270 (50.7) Carotid stenosisⱖ50% 12 (8.2) 4 (3.4) 4 (1.5) 0.003 Values are n (%), except average plaque score (mean⫾SD).
TABLE 4. Multivariate Logistic Regression Models for Different Indexes of Carotid Atherosclerosis
Characteristic IMTⱖ75th Percentile ECCA Score⬎6 Carotid Stenosisⱖ50% Hypertension status Hypertension 5.0 (3.0–8.4)‡ 3.7 (1.8–7.9)‡ 4.8 (1.4–16.5)† Borderline 3.1 (1.8–5.4)‡ 1.9 (0.8–4.6) 3.2 (0.7–14.0) Male 1.9 (1.1–3.3)* 1.1 (0.5–2.5) 1.8 (0.5–6.0) Smoking, current 2.2 (1.2–4.0)* 2.4 (1.0–5.6)* 3.5 (1.0–11.8)* Alcohol, current 0.5 (0.2–0.9)* 0.7 (0.3–1.8) 0.4 (0.1–1.5) Ageⱖ65 years 3.7 (2.3–5.9)‡ 6.2 (2.5–15.3)‡ 3.2 (1.0–10.6) BMIⱖ26.4 kg/m2 1.3 (0.8–2.2) 0.9 (0.4–1.9) 1.0 (0.3–3.1) Cholesterolⱖ6.21 mmol/L 1.1 (0.6–2.2) 1.1 (0.4–3.0) 0.2 (0.0–1.2) HDL-C⬍0.91 mmol/L 1.0 (0.6–1.5) 1.0 (0.5–1.9) 1.4 (0.5–3.7) LDL-Cⱖ4.14 mmol/L 1.5 (0.8–2.8) 0.6 (0.2–1.8) 2.6 (0.6–10.5) Diabetes mellitus 1.4 (0.7–2.9) 1.8 (0.7–4.9) 1.5 (0.3–7.6) LVH on ECG 0.9 (0.5–1.8) 2.4 (1.1–5.2)* 1.9 (0.6–6.3)
Values are given as OR (95% CI). *P⬍0.05; †P⬍0.01; ‡P⬍0.005. 2268 Stroke October 2001
at NATIONAL TAIWAN UNIV on April 29, 2009 stroke.ahajournals.org
alcohol and carotid wall IMT has been noted in some studies.29,30However, alcohol drinking was found to have
no relation with carotid wall IMT in the ARIC study.31
Small to moderate amounts of alcohol drinking may have a protective effect in the very early stages of carotid atherosclerosis; however, the effect may be attenuated by established hypertension.
Both the ARIC31and CHS32studies found that increased
exposure to cigarette smoking is significantly related to increased carotid artery IMT and carotid stenosis.32Active
and passive smoking are also associated with increased carotid wall thickness.33Smoking has a detrimental effect,
being associated with greater IMT and carotid plaque score, and thereby moderate-to-severe carotid atheroscle-rosis, in this study. The high prevalence (61.9% of male participants) of smoking was noted with the CCCC study.18
Cigarette smoking also has been demonstrated to be a more important risk factor for stroke and cerebral infarction than excessive drinking of alcohol in a population study in Taiwan.34 Thus, the high mortality rate from stroke in
Taiwan makes the need for public policy to reduce the smoking rate more urgent.
The Framingham study35has shown that in the presence
of LVH, the incidence rates of acute myocardial infarction and sudden death increase 6- to 8-fold, irrespective of blood pressure. The CHS further demonstrated that LVH on ECG is a risk factor for maximal CCA and ICA IMT and maximal percent stenosis of carotid arteries.28 The
results of the current study are consistent with these findings: there is moderate but significant increased risk for significant ECCA score⬎6 for individuals with LVH on ECG (OR 2.4), which indicates that LVH is an important indicator of end-organ change and is strongly associated with carotid atherosclerosis.
Hypertension has been recognized as a strong risk factor for cardiovascular disease, stroke, and peripheral vascular disease. Isolated systolic hypertension and isolated border-line hypertension are associated with a higher risk of cardiovascular disease36 and subclinical atherosclerotic
disease.13Mechanisms by which hypertension predisposes
to atherosclerosis may include endothelial dysfunction, hyperinsulinemia, hemodynamic stress, and multiple met-abolic alterations. Impaired production of endothelium-derived relaxing factors and increased activity of endothe-lium-derived contractile substances have been demonstrated in hypertensive patients,37 preceding overt
atherosclerotic disease.38 In addition, enhanced smooth
muscle cell proliferation with intimal wall thickening and proteoglycan accumulation accelerates atherosclerosis.39
Hypertension increases the wall shear stress and baro-trauma to the arterial intima.40Increased flow velocity and
wall shear stress are considered to be the important factors that caused hypertension-induced intima-media hypertro-phy and thickness. Hypertension is also associated with insulin resistance and considered a manifestation of met-abolic syndrome.41 A cluster of insulin-resistance
syn-drome has been noted among the individuals with hyper-tension in this study cohort, leading to increased risk for atherosclerosis, thrombosis, and other coronary heart
dis-ease.16 Another study conducted in Taiwan shows that
hypertension, hypercholesterolemia, and hypertriglyceri-demia are pathogenic in carotid atherosclerosis and stroke.6 The present study links only hypertension as the
most prominent risk factor for thicker IMT and clinically for the development of carotid stenosis, and thereby for higher ECCA plaque score. In fact, this is the first study to demonstrate by an apparent dose-response relationship that hypertension is the most important determinant in the development of carotid atherosclerosis.
The thickening of carotid IMT is initiated when hyper-tension is borderline14,42 but does not to a significant
degree affect the development of advanced carotid plaques and carotid stenosis (after adjusting for other associated factors). This finding indicates that borderline hyperten-sion (a transition state to full-blown hypertenhyperten-sion) may increase the risk of atherosclerosis, implying that the increase in IMT is an earlier preclinical atherosclerotic change. Possibly, as atherosclerosis progresses to an ad-vanced lesion stage, the status of borderline hypertension changes to evident hypertension.
It remains debatable whether to refer to increased IMT as atherosclerosis. It represents end-organ disease of mainly hypertensive medial hypertrophy. Adams et al43
found only a weak correlation between IMT and severity of CAD; they point out that IMT is approximately 80% media and only 20% intima, whereas atherosclerosis is an intimal process. Furthermore, there is a fundamental con-ceptual fallacy in the construct: IMT is continuous along the length of the vessel, whereas atherosclerosis is focal. O’Leary et al44showed that the R2for prediction of IMT by
Framingham risk factors was only 0.15 in the internal carotid artery and 0.18 in the CCAs. Spence et al,45on the
other hand, showed that Framingham risk factors explain 50% of carotid plaque area. Others46,47have shown a better
correlation between IMT and left ventricular mass than with atherosclerosis; 2 studies48,49 have shown a better
correlation of plaque measurements than IMT with athero-sclerotic events. O’Leary et al8had demonstrated that IMT
predicted events and showed that IMT is a stronger predictor of stroke than myocardial infarction; this is probably because IMT predicts events due to hypertensive small-vessel disease or because of other aspects of physi-ological aging. Carotid plaque is an even stronger predictor of atherosclerotic events (myocardial infarction) than stroke, which is partly nonatherosclerotic.50 Our previous
work24 has demonstrated that in patients with ischemic
stroke, hypertension is prevalent (49% to 66%) and ECCA atherosclerosis is common. The present study showed hypertension to be the most important risk factor for carotid atherosclerosis among individuals with or without ischemic stroke.
The current study is limited by the cross-sectional design. However, it is reasonable to conclude that carotid atherosclerosis progresses with the transition of normoten-sion to borderline hypertennormoten-sion and then to hypertennormoten-sion. Carotid atherosclerosis evaluation by carotid ultrasound is useful and sensitive in clinical practice, especially for patients with hypertension. Blood pressure measurement
also should be performed routinely for every adult in clinical practice. The pathogenesis of hypertension in atherosclerosis deserves greater concern and further study. Optimal control of hypertension for the prevention of atherosclerotic disease can never be overestimated, espe-cially in a country such as Taiwan with high prevalence of stroke.
Acknowledgments
This study was sponsored in part by the Power Development Foundation of Taiwan Power Company and National Science Coun-cil (NSC 90-2314-B-002-117) in Taiwan. We thank the cardiologists at National Taiwan University Hospital and Yu-Jenn Huang, Hui-Ping Hung, and Ching-Chu Chien for their assistance in this study.
References
1. Department of Health, Executive Yuan. Health and Vital Statistics II of the Republic of China, 1998. Taipei, Republic of China; 1998. 2. Kannel WB. Blood pressure as a cardiovascular risk factor: prevention
and treatment. JAMA. 1996;275:1571–1576.
3. Palmer AJ, Bulpitt CJ, Fletcher AE, Beevers G, Coles EC, Ledingham JGG, O’Riodan PW, Petrie JC, Rajagopallan BE, Webeter J. Relation between blood pressure and stroke mortality. Stroke. 1992;20: 601– 605.
4. MacMahon S, Peto R, Cutler J, Collins R, Sorlie P, Neaton J, Abbott R, Godwin J, Dyer J, Stamler J. Blood pressure, stroke, and coronary heart disease, part I: prolonged differences in blood pressure: pro-spective observational studies corrected for the regression dilution bias. Lancet. 1990;335:765–774.
5. Craven TE, Ryu JE, Espeland MA, Kahl FR, McKinney WM, Toole JF, MacMahan MR, Tompson CJ, Heiss G, Crouse JR III. Evaluation of the association between carotid artery atherosclerosis and coronary artery stenosis: a case-control study. Circulation. 1990;82: 1230 –1242.
6. Pan WH, Bai CH, Chen JR, Chiu HC. Associations between carotid atherosclerosis and high factor VIII activity, dyslipidemia, and hyper-tension. Stroke. 1997;28:88 –94.
7. Chen WH, Ho DSW, Ho SL, Cheung RTF, Cheng SWK. Prevalence of extracranial carotid and vertebral artery disease in Chinese patients with coronary artery disease. Stroke. 1998;29:631– 634.
8. O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK Jr, for the Cardiovascular Health Study Collaborative Research Group. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med. 1999;340:14 –22.
9. O’Leary DH, Polak JF, Wolfson SK Jr, Bond MG, Bommer W, Sheth S, Psaty BM, Sharrett A R, Manolio TA, on behalf of the CHS Collaborative Research Group. Use of sonography to evaluate carotid atherosclerosis in the elderly: the Cardiovascular Health Study. Stroke. 1991;22:1155–1163.
10. Li R, Cai J, Tegeler C, Sorlie P, Metcalf PA, Heiss G. Reproducibility of extracranial carotid atherosclerotic lesions assessed by B-mode ultrasound: the Atherosclerosis Risk In Communities Study. Ultrasound Med Biol. 1996;22:791–799.
11. Wong M, Edelstein J, Wollman J, Bond MG. Ultrasonic-pathological comparison of human arterial wall: verification of intima-media thickness. Arterioscler Thromb. 1993;13:482– 486.
12. Ferrara LA, Mancini M, Celentano A, Galderisi M, Iannuzzi R, Marotta T, Gaeta I. Early changes of the arterial carotid wall in uncomplicated primary hypertensive patients. Arterioscler Thromb. 1994;14:1290 –1296.
13. Psaty BM, Furberg CD, Kuller LH, Borhani NO, Rautaharju PM, O’Leary DH, Bild DE, Robbins J, Fried L, Reid C. Isolated systolic hypertension and subclinical cardiovascular disease in the elderly: initial findings from the Cardiovascular Health Study. JAMA. 1992; 268:1287–1291.
14. Lemne C, Jogestrand T, de Faire U. Carotid intima-media thickness and plaque in borderline hypertension. Stroke. 1995;26:34 –39. 15. Chien KL, Lee YT, Sung FC, Su TC, Hsu HC, Lin RS. Lipoprotein (a)
level in the population in Taiwan: relationship to sociodemographic and atherosclerotic risk factors. Atherosclerosis. 1999;143:267–273.
16. Chien KL, Lee YT, Sung FC, Hsu HC, Su TC, Lin RS. Hyperinsu-linemia and related atherosclerotic risk factors in the population at risk: community-based study. Clin Chem. 1999;45:838 – 846. 17. Torng PL, Su TC, Sung FC, Chien KL, Huang SC, Chow SN, Lee YT.
Effects of menopause and obesity on lipid profiles in middle-aged Taiwanese women: the Chin-Shan Community Cardiovascular Cohort Study. Atherosclerosis. 2000;153:413– 421.
18. Lee YT, Lin RS, Sung FC, Yang CY, Chien KL, Chen WJ, Su TC, Hsu HC, Huang YC. Chin-Shan Community Cardiovascular Cohort in Taiwan: baseline data and five-year follow-up morbidity and mor-tality. J Clin Epidemiol. 2000;53:838 – 846.
19. Joint National Committee. The fifth report of the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure (JNC V). Arch Intern Med. 1993;153:154 –183.
20. Huang PJ, Yu SL, Lin YM, Chu CL. Body weight of Chinese adults by sex, age and body height and criterion of obesity based on body mass index. J Chin Nutr Soc. 1992;17:157–172.
21. Physician’s Guide to Marquuette Electronics Resting ECG Analysis. Milwaukee, Wis: Marquette Electronics Inc; 1991.
22. Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation. 1986;74:1399 –1406.
23. Su TC, Jeng JS, Chien KL, Torng PL, Sung FC, Lee YT. Measurement reliability of common carotid artery intima-media thickness by ultra-sonographic assessment. J Med Ultrasound. 1999;7:73–79. 24. Jeng JS, Chung MY, Yip PK, Hwang BS, Chang YC. Extracranial
carotid atherosclerosis and vascular risk factors in different types of ischemic stroke in Taiwan. Stroke. 1994;25:1989 –1993.
25. Chen CC, Chung MY, Jeng JS, Yip PK, Hwang BS, Chang YC. A scoring system for evaluation of the extent of extracranial carotid atherosclerosis with B-mode imaging. Acta Neural Sin. 1995;4:29 –33. 26. Huang ZS, Chiang TL, Lee TK. Stroke prevalence in Taiwan: Findings from the 1994 National Interview Survey. Stroke. 1997;28: 1579 –1584.
27. Howard G, Sharrett AR, Heiss G, Evans GW, Chambless LE, Riley WA, Burke GL, for the ARIC Investigators. Carotid intimal-medial thickness distribution in general populations as evaluated by B-mode ultrasound. Stroke. 1993;24:1297–1304.
28. O’Leary DH, Polak JF, Kronmal RA, Kittner SJ, Bond G, Wolfson SK Jr, Bommer W, Price TR, Gardin JM, Savage PJ. Distribution and correlates of sonographic detected carotid artery disease in the Car-diovascular Health Study. Stroke. 1992;23:1752–1760.
29. Salonen JT, Seppanen R, Rauramaa R, Salonen R. Risk factors for carotid atherosclerosis: the Kuopio Ischemic Heart Disease Risk Factor Study. Ann Med. 1989;21:227–229.
30. Bogousslavsky J, Van Melle G, Despland PA, Regli F. Alcohol consumption and carotid atherosclerosis in the Lausanne Stroke Registry. Stroke. 1990;21:715–720.
31. Demirovic J, Naabulsi A, Folsom AR, Carpenter MA, Szklo M, Sorlie PD, Barnes RW, for the ARIC Study Investigators. Alcohol con-sumption and ultrasonographically assessed carotid artery wall thickness and distensibility. Circulation. 1993;88:2787–2793. 32. Tell GS, Polak JF, Ward BJ, Kittner SJ, Savage PJ, Robbins J, for the
Cardiovascular Health Study (CHS) Collaborative Research Group. Relation of smoking with carotid artery wall thickness and stenosis in older adults. Circulation. 1994;90:2905–2908.
33. Howard G, Burke GL, Szklo M, Tell GS, Eckfeldt, Evans G, Heiss G. Active and passive smoking are associated with increased carotid wall thickness. Arch Intern Med. 1994;154:1277–1282.
34. Lee TK, Huang ZS, Ng SK, Chen KWA, Wang YS, Liu HW, Lee JJ. Impact of alcohol consumption and cigarette smoking on stroke among the elderly in Taiwan. Stroke. 1995;26:790 –794.
35. Kannel WB. Prevalence and natural history of electrocardiographic left ventricular hypertrophy. Am J Med. 1983;75(suppl 3A):4 –11. 36. O’Donnell CJ, Ridker PM, Glynn RJ, Berger K, Ajani U, Manson JE,
Mennekens CH. Hypertension and borderline isolated systolic hyper-tension increased risks of cardiovascular disease and mortality in male physicians. Circulation. 1997;95:1132–1137.
37. Panza JA, Quyyuami AA, Brush JE, Epstein SE. Abnormal endothe-lium-dependent vascular relaxation in patients with essential hyper-tension. N Engl J Med. 1990;323:22–27.
38. Iiyama K, Nagano M, Yo Y, Nagano N, Kamide K, Higaki J, Mikami H, Ogihara T. Endothelial dysfunction exists in patients with hyper-tension and precedes overt atherosclerotic disease. Am Heart J. 1996; 132:779 –782.
2270 Stroke October 2001
at NATIONAL TAIWAN UNIV on April 29, 2009 stroke.ahajournals.org
39. Chobanian AV. Corcoran lecture: adaptive and maladaptive responses of the arterial wall to hypertension. Hypertension. 1990;1989:15: 666 – 674.
40. Glagov S, Zarins C, Giddens DP, Ku DN. Hemodynamics and ath-erosclerosis. Arch Pathol Lab Med. 1988;112:1018 –1031.
41. Reaven GM, Lithell H, Landsberg L. Hypertension and associated metabolic abnormalities: the role of insulin resistance and the sym-pathoadrenal system. N Engl J Med. 1996;334:374 –381.
42. Pauletto P, Palatini P, Da Ros S, Pagliara V, Santipolo N, Baccillieri S, Casiglia E, Mormino P Pessina AC. Factors underlying the increase in carotid intima-media thickness in borderline hypertensives. Arte-rioscler Thromb Vasc Biol. 1999;19:1231–1237.
43. Adams MR, Nakagomi A, Keech A, Robinson J, McCredie R, Bailey BP, Freedman SB, Celermajer DS. Carotid intima-media thickness is only weakly correlated with the extent and severity of coronary artery disease. Circulation. 1995;92:2127–2134.
44. O’Leary DH, Polak JF, Kronmal RA, Savage PJ, Borhani NO, Kittner SJ, Tracy R, Gardin JM, Price TR, Furberg CD. Thickening of the carotid wall: a marker for carotid atherosclerosis in the elderly? Stroke. 1996;27:224 –231.
45. Spence JD, Barnett PA, Bulman DE, Hegele RA. An approach to ascertain probands with a non-traditional risk factor for carotid ath-erosclerosis. Athath-erosclerosis. 1999;144:429 – 434.
46. Cuspidi C, Lonati L, Sampieri L, Pelizzoli S, Pontiggia G, Leonetti G, Zanchetti A. Left ventricular concentric remodeling and carotid structural changes in essential hypertension. J Hypertens. 1996;14: 1441–1446.
47. Linhart A, Gariepy J, Giral P, Levenson J, Simon A. Carotid artery and left ventricular structural relationship in asymptomatic men at risk for cardiovascular disease. Atherosclerosis. 1996;127:103–112. 48. Ebrahim S, Papacosta O, Whincup P, Wannamethee G, Walker M,
Nicolaides AN, Dhanjil S, Griffin M, Belcaro G, Rumley A, Lowe GD. Carotid plaque, intima-media thickness, cardiovascular risk factors, and prevalent cardiovascular disease in men and women: the British Regional Heart Study. Stroke. 1999;30:841– 850.
49. Aminbakhsh A, Frohlich J, Mancini GB. Detection of early athero-sclerosis with B mode ultrasonography: assessment of a new quanti-tative approach. Clin Invest Med. 1999;22:265–274.
50. Spence JD, Hackam DG, Eliasziw M. Carotid plaque area as a tool for identifying patients at high coronary risk. Stroke. 2000;31:293. Abstract.