The Epidemiology of Pleural Infection in Taiwan from 1997 through 2008 Hsiu-Nien Shen1,2,*, MD; Chin-Li Lu2,3, MS; Chung-Yi Li, PhD2,4
1 Department of Intensive Care Medicine, Chi Mei Medical Center, No. 901 Chung-Hwa Road, Yong-Kang Region, Tainan, Taiwan.
2 Department of Public Health, College of Medicine, National Cheng Kung University, Tainan, Taiwan.
3 Department of Medical Research, Chi Mei Medical Center, No. 901 Chung-Hwa Road, Yong-Kang Region, Tainan, Taiwan.
4 Department of Public Health, College of Public Health, China Medical University, Taichung, Taiwan.
*Corresponding author Hsiu-Nien Shen
Department of Intensive Care Medicine, Chi Mei Medical Center, No. 901 Chung-Hwa Road, Yong-Kang District, Tainan, Taiwan.
Tel: +886-6-2812811 Ext 57106 Fax: +886-6-2828928
Email: HNS: hsiunian@gmail.com
Summary at a glance
Pleural infection is changing over time with respect to the incidence, management and outcome. In Taiwan, the incidence of pleural infection reached a plateau in recent years, resource use and hospital charges increased substantially, and short-term mortality fell over time despite an increasing proportion of older and sicker patients.
ABSTRACT
Background and objectives: Population-based data on pleural infection are limited. We
aimed to describe temporal trends in incidence, management and outcome of pleural infection in Taiwan.
Methods: We analyzed 26,385 patients with first-episode pleural infection from the
Taiwan National Health Insurance Research Database between 1997-2008.
Results: During the study period, the median age of the patients increased from 60 to 65
years. Most patients were men (75%) and the proportion was stable over time. The standardized annual incidence of pleural infection increased from 5.2 per 100,000 in 1997 to a plateau of 8.4 to 9.6 per 100,000 between 2002-2008. There was increasing use of computed tomography (from 47.3% in 1997-1998 to 59.4% in 2007-2008), pigtail catheters (from 1.5% to 18.9%), fibrinolytics (from 0.9% to 9.3%) and surgery (from 27.7% to 33.6%) for treating pleural infection over time. Meanwhile, usage of life-supporting resources, including hemodialysis, mechanical ventilation and intensive care, also increased by 3.1%, 11.0% and 12.8%, respectively. Median hospital charges per patient rose by 63.6% in 12 years. Although the proportion of patients with organ dysfunction, i.e. severe sepsis, increased from 26.5% to 47.7%, 30-day mortality decreased from 15.0% to 13.1% (p for trend=0.001).
infection and subsequent severe sepsis might have reduced the risk of short-term mortality.
Key words: Pleural infection; epidemiology; management; resource use; outcome.
Short title: Pleural infection in Taiwan
Author contributions:
HNS is responsible for the integrity of the entire manuscript, as he designed the study, obtained funding, performed data mining and processing, did statistical analyses, drafted the initial manuscript, and revised important content. CLL contributed to the study design, data analyses and interpretation of results, and revision for important content. CYL participated in interpretation of results and revision for important content.
INTRODUCTION
Pleural infection occurs in less than 10 cases per 100,000 person-years.1 Despite relatively uncommon, the incidence is increasing in both children2-5 and adults.1,2,6 A
greater increase in incidence has been reported in pleural infection accompanied with pneumonia,6 which accounts for about 70% of the patients with pleural infection.7 If treatment is delayed, pleural infection can progress to systemic inflammation and organ dysfunction or failure (i.e. severe sepsis), causing significant morbidity and mortality.7-9 The reported case-fatality rates vary between 7%18%.1,6,8,9 Population-based studies suggest that there is no mortality decline since 1990s.1,6
Treatment for pleural infection remains largely un-standardized.9-12 In addition to systemic antibiotics, options for treating pleural infection include serial thoracentesis, small- or large-bore tube drainage, intrapleural fibrinolytics and surgery (including thoracoscopy, thoracotomy, decortication and open drainage).12,13 Recent single-institutional reports showed increasing uses of pigtail (or small-bore) catheters for simple drainage and video-assisted thoracoscopic surgery (VATS) for surgical drainage and decortication.14,15 However, population-based data on the trend of various interventions for pleural infection are limited.1 These data can not only help to understand change of practice in the treatment of pleural infection, but help to suggest potential clinical questions for future research. Therefore, we conducted this population-based study using a national database to examine the temporal trends in incidence, management and outcome of pleural infection in Taiwan.
METHODS Database
The National Health Insurance System (NHIS) in Taiwan is compulsory and covers all citizens except prisoners.17 The National Health Insurance Research Database (NHIRD), released for research purposes by the National Health Research Institute,16 has been used in studies on pediatric empyema and severe sepsis.18,19 Information included in the inpatient database incorporated sex, date of birth, encrypted patient identification
numbers, dates of admission and discharge, medical institutions providing the services, the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes of diagnoses (up to five) and procedures (up to five), outcome at hospital discharge (recovered, died or transferred out), order codes and hospital charges. Patients and Definitions
Between 1995 and 2008 (inclusive), we identified 43,875 hospitalizations with a discharge diagnosis of pleural infection, defined as empyema with or without fistula (ICD-9-CM codes 510.0, 510.9) or infected pleural effusion (511.1) in any position of the five diagnoses, from the NHIRD. To ensure the inclusion of first-episode pleural infection, we excluded 5,015 readmissions for pleural infection and 155 patients who had ever been hospitalized for the disease in 1995-1996 when the NHIS was implemented. To reduce misclassification, we also excluded 6,896 patients who did not receive any interventional management of pleural infection during hospitalization. The intervention was defined by procedure codes1 or physician-order codes (Appendix Table 1) and included thoracentesis, tube thoracostomy, pleural drainage by operation, decortication and closure of a bronchopleural fistula. Finally, we excluded 5,424 patients with procedure codes of thoracic operations for conditions other than pleural infection during hospitalization. The definitions of the procedure codes for the aforementioned interventions and operations were the same as those defined by Farjah
and coworkers in a population-based study.1 The remaining patients (n=26,385) admitted for the first time in the years between 1997 and 2008 were included in the analysis. Human subjects institutional review board approval and informed consent from the patients were exempt due to the use of the encrypted administrative database. Measurements
Demographic and clinical characteristics of the patients at their first-episode admissions were examined, including age, sex, year of admission, hospital level, prevalence of selected comorbid conditions, Charlson comorbidity index,20,21 acute organ dysfunction,18 interventions for pleural infection (including uses of pigtail or small-bore catheters and fibrinolytics and open or thoracoscopic surgery), resource uses (including hemodialysis and vasopressors and mechanical ventilation), hospital charges, length of stay in ICU and hospital, death (including 30-day and hospital mortality) and readmission within 30 days after hospital discharge.1 Acute organ dysfunction was defined in our earlier report;18 however, regarding acute renal dysfunction, only ICD-9-CM code 584 (excluding 580, 586 and 39.95) was used in the present study to reduce potential misclassification of a chronic renal failure as an acute episode found in the prior validation step.18 Fibrinolytics included urokinase and streptokinase. Hospital charges were converted to 2008 price levels in United States dollars (USD).
We validated the ICD-9-CM code for the identification of pleural infection by chart analysis of 50 patients randomly selected, using the study method, from the inpatient claims database of Chi Mei Medical Center, a 1,200-bed teaching hospital in southern Taiwan, between 2007 and 2009. Pleural infection was ascertained by the presence of a pleural effusion containing pus, bacteria in Gram stain and/or culture, or features suggestive of complicated parapneumonic effusion in biochemistry of pleural effusion (a pH of ≤7.2, a glucose level of ≤40 mg/dL or a lactate dehydrogenase level of ≥1,000 U/L)9,22 and/or histopathology of decorticated specimen. Positive predictive value was estimated.
Statistics
Continuous variables are described as median (inter-quartile range) because most of them are not symmetrically distributed and the measure of median would not be affected by extreme values; and discrete ones as count or percentage. The number of beneficiaries in Taiwan from 1997 to 2008, reported by the National Health Insurance Statistics, was used as the denominator for estimating crude rates. Incidence rates were further standardized for age and sex by the direct method using the WHO World Population in 2000 as the standard population. To investigate yearly trends, we performed ANOVA for linearity of scaled variables and linear-by-linear association chi-square test for categorical data. Finally, we stratified patients by the presence or absence
of acute organ dysfunction to examine whether the 30-day mortality trend differ. Data were analyzed with SPSS for Windows, version 17.0. (SPSS Inc., Illinois, U.S.A.). A two-tailed p value of <0.05 was considered significant.
RESULTS Incidence
The age- and sex-standardized incidence rates of pleural infection increased from 5.2 per 100,000 in 1997 to a plateau of 8.4 to 9.6 per 100,000 between 20022008 (Figure 1). These trends persisted irrespective of age and sex. The age- and sex-specific incidence rates of pleural infection showed a J-shaped distribution (Figure 2).
In the validation step, 44 of the 50 patients coded with pleural infection were confirmed by chart review, yielding a positive predictive value of 88.0% (95% confidence interval, 76.7%–95.0%).
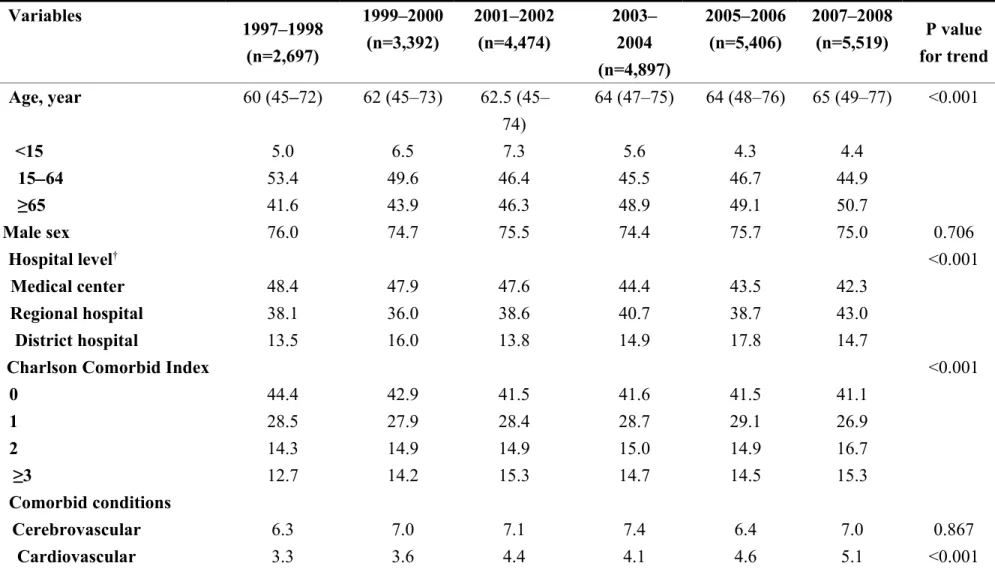
Patient characteristics
Table 1 shows the trends in characteristics of the 26,385 patients with pleural infection. The patients were getting older; the proportion of elderly (≥65 years) increased by 9.1% over the 12-year period. The proportions of boys and girls were about equal (51.2% vs.
48.8%), whereas most of the adults were men (76.6%). The sex distribution was stable both in children and adults over time. The proportion of patients treated in regional hospitals increased over time and surpassed that in medical centers in the last two years (43.0% vs. 42.3%).
Comorbidity was common (58.1%) and the proportion of patients with multiple comorbidities slightly increased. The most common comorbid conditions were diabetes (overall 19.6%), cancer (13.2%), pulmonary (10.3%) and hepatic (10.0%) diseases; among them, only incidence of cancer rose with time, along with two other less common comorbid conditions (renal and cardiovascular diseases).
Pneumonia was coded in less than half of the patients, but the proportion increased by 15.9% in 12 years. The disease severity also increased, as reflected by the prevalence of acute organ (≥1 system) dysfunction, which increased by 21.2% during the study period. Of note, patients with multi-organ (≥2 systems) dysfunction almost doubled, as the presence of dysfunction in all organ systems except hepatic and metabolic ones also doubled at the same time.
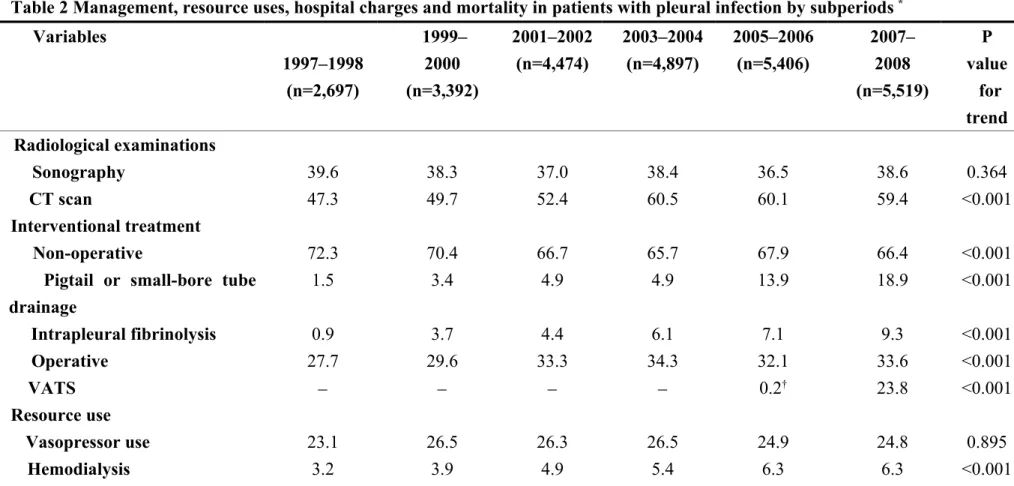
Management of pleural infection
While the proportion of patients receiving computed tomography examinations increased by 12.1%, that of those undergoing sonography changed little (Table 2). A temporal increase was observed in pigtail catheter placement (from 1.5% to 18.9%) and
fibrinolytic therapy (from 0.9% to 9.3%) for pleural infection. Although most patients received non-operative treatment, the proportion of surgery increased from 27.7% in 1997-1998 to 33.6% 2007-2008 when the insurance coverage for VATS started and 71.6% of the surgery was done by VATS.
Resource use, hospital charges and outcomes
Table 2 also shows trends in resource use, hospital charges and outcomes of the patients. Consistent with the increasing disease severity, the patients increasingly treated with life-supporting measures including hemodialysis, mechanical ventilation and intensive care. The duration of ICU stay increased slightly, whereas the duration of mechanical ventilation and hospital stay changed little. The median hospital charges per patient continuously increased from $2,697 to $4,413, representing an increase of 63.6% in 12 years.
Mortality increased with age (Figure 3). The death rate was slightly greater at hospital discharge than at 30 days because some patients who died at hospital discharge had a length of hospital stay of 30 days or longer, but the declining trends were similar (Table 2). In patients with acute organ dysfunction, 30-day mortality rate fell by 14.1% in 12 years. Among patients alive at hospital discharge, on average 14.2% of them were readmitted within 30 days; during the study period, this figure did not have a statistically significant change.
DISCUSSION
In this study, we found that the incidence of pleural infection in Taiwan reached a plateau in recent years after an initial rise from 1997 to 2002. The trend was observed in all age groups. Computed tomography and several interventions including pigtail-catheter drainage, fribinolysis and surgery, especially VATS, were increasingly adopted to treat pleural infection. Despite increasing patient age and disease severity, mortality declined over time. However, resource use and hospital charges rose considerably and a high readmission rate remained sustained during the study period.
The population incidence of pleural infection in Taiwan was comparable to other reports.1-6,23 However, we found that a rising trend was only present in the years before 2002. Although the rise was found in most countries,1-6,19 a recent decline in the incidence of pediatric empyema was also reported in England.23 The reason for the decline has been attributed to the introduction of the seven-valent pneumococcal conjugate vaccination for all children in England since 2006.23 Although the 23-valent and 7-valent pneumococcal conjugate vaccines have been introduced into Taiwan since 2001 and 2005, respectively, the vaccination is not routine and still not covered by the insurance. Therefore, the steady incidence since 2002 in this study cannot be
entirely explained by immunization alone. Although coding errors (i.e. under- or over-coding) were likely to occur, they cannot explain the change in incidence because using the same codes over the study period would retain the internal validity of the temporal trend analyses. On the other hand, increasing awareness and detection of pleural infection, as reflected by an increasing use of computed tomography, might explain the initial increase; but they cannot explain the recent plateau in incidence.
Traditionally, pleural infection is usually drained by large-bore chest tubes.13 We found that the use of small-bore tubes (or pigtail catheters) was increasing, which is consistent with recent reports.14,15 For example, in a clinical trial assessing the efficacy of fibrinolytics for pleural infection, a small-bore (1014 F) chest tube was inserted in 65% of the 405 patients receiving drains.9,24 This figure increased to 86.7% in a subsequent trial.25 Small-bore catheters have been shown to have comparable efficacy to, but caused lesser pain, than larger ones.24 This may help to explain the marked increase of pigtail catheter uses in Taiwan in recent years.
The increasing use of fibrinolytics for pleural infection found in this study, although consistent with previous guidelines,26 raises concerns because it seems to be conflict with current guidelines.12 Due to a lack of efficacy,9 fibrinolytics are reserved only for selected patients such as those with loculated or septated pleural effusions.7,12,13 Perhaps, the more frequent use of computed tomography might have
caused the increased use of fibrinolytics because the scan could be more efficient in detecting loculated effusions.
A rise in surgery for pleural infection has been reported in a population-based study.1 In the Washington State of the US, the proportion of patients receiving surgery for pleural infection increased from 42.4% in 1987 to 58.4% in 2004,1 which is much higher than that in Taiwan. However, the proportion of VATS could not be obtained in that study.1 We demonstrate that most of the operations are being done by VATS in recent years. The rising trend might be due to an improved imaging technology, the availability of experienced thoracic surgeons and a greater acceptance by patient and physician for the minimally invasive and apparently effective operation.1, 27-33 However, because there are no validated measures on which to base the decision to refer patients to surgery, the apparent increase in the use of surgical techniques may reflect simply a change in medical culture rather than a true change in either severity or incidence of pleural infection. In addition, financial incentives through insurance coverage for patients undergoing VATS might also have contributions.
The short-term mortality of patients with pleural infection in this study is in the range of prior reports (10%18%).1,8,9 Although Grijalva and coworkers reported a lower mortality rate (7%8%) in a US national study, this figure is likely to be underestimated because of the inclusion of readmissions,6 which was about 4.4%
within 30 days after hospital discharge, as shown in a statewide study in the US.1 Of note, the 30-day readmission rate in our study was more than 3 times higher than that in the US.1 Although readmission rates are usually considered as appropriate indicators for disease management during hospitalization, they can also be affected by health-related policies.34 Thus, difference in findings between our study and previous studies might be affected not only by appropriate management of patients with pleural infection but also by differing policies of admission adopted by different hospitals. Because the NHI dataset does not cover those factors mentioned above, we were unable to examine specifically the factors that truly cause the variant readmission rates in different areas. Clearly, further studies are needed to tackle the sustained high readmission rate.
Unlike prior reports,1,6 the case-fatality rate of pleural infection declined in Taiwan, especially in patients with acute organ dysfunction, i.e. severe sepsis.18,35 Although pleural infection may cause death in the context of a chronic infection rather than acute bacterial sepsis, we found that more and more patients developed severe pleural infection with organ failure. Therefore, incorporation of the severe sepsis bundle 36,37 into source control interventions for the treatment of pleural infection is important and might have contributed to the mortality decline. However, this has not been addressed in a recent published guideline.12
The implications of the study are as follows. First, the substantial increase in resource use and costs of treating pleural infection calls for a need to assess the cost-effectiveness of these treatments. Of note, the results of several recent studies in pediatric pleural infection have not established the role of VATS or surgery as the first line therapy.29-32 Second, there is also room for improving quality of care delivered to the hospitalized patients with pleural infection to yield further reduction in unsatisfactory rate of readmission.
Several other limitations deserve comments. First, an inability to determine the time course between pleural infection and development of organ dysfunction renders it impossible to differentiate whether the organ dysfunction was infection related or not. Second, because the database does not contain data on the out-of-pocket fees, the hospital charges might be underestimated, especially in the years before 2007 when VATS was still not covered by the insurance. And finally, mortality could also be underestimated due to being unable to verify through linkage with death-certificate data. In conclusion, after an initial increase, the incidence of pleural infection plateaued in Taiwan in recent years. Advancement in management of pleural infection and subsequent severe sepsis might have reduced the risk of short-term mortality, but it substantially increased resource utilization and hospital charges, which call for evaluations of the clinical and cost effectiveness of these treatments.
Acknowledgments
This study was supported by grant CMFHR9855 from Chi Mei Medical Center and based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by National Health Research Institutes. The interpretation and conclusions contained herein do not represent those of Bureau of National Health Insurance, Department of Health or
National Health Research Institutes.
REFERENCES
1. Farjah F, Symons RG, Krishnadasan B et al. Management of pleural space infections: a population-based analysis. J. Thorac. Cardiovasc. Surg. 2007; 133: 34651.
2. Finley C, Clifton J, FitzGerald JM et al. Empyema: an increasing concern in Canada.
Can. Resp. J. 2008; 15: 859.
3. Li STT, Tancredi DJ. Empyema hospitalizations increased in US children despite pneumococcal conjugate vaccine. Pediatrics 2010; 125: 2633.
4. Roxburgh CSD, Youngson GG, Townend JA et al. Trends in pneumonia and empyema in Scottish children in the past 25 years. Arch. Dis. Child. 2008; 93: 3168.
5. Strachan R, Jaffe A. Assessment of the burden of paediatric empyema in Australia. J.
Paediatr. Child. Health 2009; 45: 4316.
6. Grijalva CG, Zhu Y, Nuorti JP et al. Emergence of parapneumonic empyema in the USA. Thorax 2011; 66: 6638.
7. Sahn SA. Diagnosis and management of parapneumonic effusions and empyema.
Clin. Infect. Dis. 2007; 45: 14806.
8. Ferguson A, Prescott R, Selkon J et al. The clinical course and management of thoracic empyema. Q.J.M. 1996; 89: 2859.
9. Maskell NA, Davies CW, Nunn AJ et al. U.K. controlled trial of intrapleural streptokinase for pleural infection. N. Engl. J. Med. 2005; 352: 86574.
10. Balfour-Lynn IM, Abrahamson E, Cohen G et al. BTS guidelines for the management of pleural infection in children. Thorax 2005; 60(Suppl 1): i121.
11. Mahant S, Cohen E, Weinstein M et al. Video-Assisted Thorascopic Surgery vs Chest Drain With Fibrinolytics for the Treatment of Pleural Empyema in Children: A Systematic Review of Randomized Controlled Trials. Arch. Pediatr. Adolesc. Med. 2010; 164: 2013.
12. Davies HE, Davies RJ, Davies CW. Management of pleural infection in adults: British Thoracic Society pleural disease guideline 2010. Thorax 2010; 65(Suppl 2): ii4153.
13. Heffner JE, Klein JS, Hampson C. Interventional management of pleural infections.
Chest 2009; 136: 114859.
14. Wozniak CJ, Paull DE, Moezzi JE et al. Choice of first intervention is related to outcomes in the management of empyema. Ann. Thorac. Surg. 2009; 87: 152531. 15. Liu YH, Lin YC, Liang SJ et al. Ultrasound-guided pigtail catheters for drainage of various pleural diseases. Am. J. Emerg. Med. 2010; 28: 91521.
16. National Health Insurance Research Database. http://w3.nhri.org.tw /nhird//en/index.htm Accessed: 30 October 2011.
17. Bureau of National Health Insurance, Department of Health, Executive Yuan. http://www.nhi.gov.tw/English/webdata/webdata.aspx?
menu=11&menu_id=296&webdata_id=1942&WD_ID=296 Accessed: 30 October 2011.
18. Shen HN, Lu CL, Yang HH. Epidemiologic trend of severe sepsis in Taiwan from 1997 through 2006. Chest 2010; 138: 298304.
19. Wu PS, Huang LM, Chang IS et al. The epidemiology of hospitalized children with pneumococcal/lobar pneumonia and empyema from 1997 to 2004 in Taiwan. Eur. J.
Pediatr. 2010; 169: 8616.
20. Charlson ME, Pompei P, Ales KL et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic. Dis. 1987;
40: 37383.
21. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 1992; 45: 6139.
22. Heffner JE, Brown LK, Barbieri C et al. Pleural fluid chemical analysis in parapneumonic effusions. A meta-analysis. Am. J. Respir. Crit. Care Med. 1995; 151: 17008.
23. Koshy E, Murray J, Bottle A et al. Impact of the seven-valent pneumococcal conjugate vaccination (PCV7) programme on childhood hospital admissions for bacterial pneumonia and empyema in England: national time-trends study, 1997-2008.
Thorax 2010; 65: 7704.
24. Rahman NM, Maskell NA, Davies CW et al. The relationship between chest tube size and clinical outcome in pleural infection. Chest 2010; 137: 53643.
25. Rahman NM, Maskell NA, West A et al. Intrapleural use of tissue plasminogen activator and DNase in pleural infection. N. Engl. J. Med. 2011; 365: 51826.
26. Davies CW, Gleeson FV, Davies RJ; Pleural Diseases Group, Standards of Care Committee, British Thoracic Society. BTS guidelines for the management of pleural infection. Thorax 2003; 58(Suppl 2): ii1828.
27. Luh SP, Chou MC, Wang LS et al. Video-Assisted Thoracoscopic Surgery in the Treatment of Complicated Parapneumonic Effusions or Empyemas. Chest 2005; 127:
142732.
28. Wait MA, Sharma S, Hohn J et al. A randomized trial of empyema therapy. Chest 1997; 111: 154851.
29. Bilgin M, Akcali Y, Oguzkaya F. Benefits of early aggressive management of empyema thoracis. A.N.Z. J. Surg. 2006; 76: 1202.
30. Aziz A, Healey JM, Qureshi F et al. Comparative analysis of chest tube thoracostomy and video-assisted thoracoscopic surgery in empyema and parapneumonic effusion associated with pneumonia in children. Surg. Infect. (Larchmt) 2008; 9: 31723.
31. Sonnappa S, Cohen G, Owens CM et al. Comparison of urokinase and video-assisted thoracoscopic surgery for treatment of childhood empyema. Am. J. Respir.
Crit. Care Med. 2006; 174: 2217.
32. St Peter SD, Tsao K, Spilde TL et al. Thoracoscopic decortication vs tube thoracostomy with fibrinolysis for empyema in children: a prospective, randomized trial. J. Pediatr. Surg. 2009; 44: 10611.
33. Li STT, Gates RL. Primary operative management for pediatric empyema: decreases in hospital length of stay and charges in a national sample. Arch. Pediatr. Adolesc. Med. 2008; 162: 448.
admissions in the Emilia-Romagna region of Italy. J Health Serv Res Policy 2008; 13: 2028.
35. Bone RC, Balk RA, Cerra FB et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992; 101: 164455.
36. Dellinger RP, Levy MM, Carlet JM et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care
Med. 2008; 34: 1760.
37. Levy MM, Dellinger RP, Townsend SR et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med. 2010; 36: 22231.
Figure Legends Figure 1
Time trends in crude and age- and sex-standardized incidence rates of pleural infection
Figure 2
Age- and sex-specific incidence rates for patients with pleural infection
Figure 3
Table 1 Characteristics of patients with pleural infection by subperiods* Variables 1997–1998 (n=2,697) 1999–2000 (n=3,392) 2001–2002 (n=4,474) 2003– 2004 (n=4,897) 2005–2006 (n=5,406) 2007–2008 (n=5,519) P value for trend Age, year 60 (45–72) 62 (45–73) 62.5 (45– 74) 64 (47–75) 64 (48–76) 65 (49–77) <0.001 <15 5.0 6.5 7.3 5.6 4.3 4.4 1564 53.4 49.6 46.4 45.5 46.7 44.9 ≥65 41.6 43.9 46.3 48.9 49.1 50.7 Male sex 76.0 74.7 75.5 74.4 75.7 75.0 0.706 Hospital level† <0.001 Medical center 48.4 47.9 47.6 44.4 43.5 42.3 Regional hospital 38.1 36.0 38.6 40.7 38.7 43.0 District hospital 13.5 16.0 13.8 14.9 17.8 14.7
Charlson Comorbid Index <0.001
0 44.4 42.9 41.5 41.6 41.5 41.1 1 28.5 27.9 28.4 28.7 29.1 26.9 2 14.3 14.9 14.9 15.0 14.9 16.7 ≥3 12.7 14.2 15.3 14.7 14.5 15.3 Comorbid conditions Cerebrovascular 6.3 7.0 7.1 7.4 6.4 7.0 0.867 Cardiovascular 3.3 3.6 4.4 4.1 4.6 5.1 <0.001
Pulmonary 8.9 11.0 10.4 10.4 10.5 10.1 0.497 Renal 3.4 4.2 5.5 5.5 5.4 5.9 <0.001 Hepatic 11.8 10.1 9.8 9.3 9.6 9.9 0.028 Diabetes 19.6 19.4 19.4 20.3 19.7 19.0 0.750 Cancer 11.6 12.4 12.9 12.7 13.6 14.8 <0.001 Pneumonia‡ 30.5 38.2 41.7 44.4 45.5 46.4 <0.001
No. of organ dysfunction <0.001
0 73.5 66.4 61.6 53.0 52.7 52.3 1 20.5 25.1 28.1 35.0 34.8 35.6 2+ 6.1 8.5 10.3 12.0 12.5 12.1 Organ dysfunction Respiratory 12.2 18.6 23.5 32.9 32.0 33.5 <0.001 Renal 2.9 4.1 4.8 5.4 6.0 6.1 <0.001 Cardiovascular 2.3 3.5 4.1 3.8 4.5 4.8 <0.001 Neurological 0.9 0.7 0.7 1.2 1.1 1.6 <0.001 Hepatic 1.0 0.8 1.3 1.0 1.0 1.2 0.386 Hematologic 0.3 0.8 0.8 0.6 0.9 0.8 0.034 Metabolic 0 0.1 0.1 0 0.1 0.1 0.132
* Values were expressed as median (interquartile range, IQR) or percentages.
† Hospitals are periodically accredited by Taiwan Joint Commission on Hospital Accreditation and Quality Improvement (authorized by the government) and classified into three levels (including medical center [>500 beds], regional [250–500 beds] and district hospitals
‡ Pneumonia was defined by ICD-9-CM codes 481486.
Table 2 Management, resource uses, hospital charges and mortality in patients with pleural infection by subperiods *
Variables 1997–1998 (n=2,697) 1999– 2000 (n=3,392) 2001–2002 (n=4,474) 2003–2004 (n=4,897) 2005–2006 (n=5,406) 2007– 2008 (n=5,519) P value for trend Radiological examinations Sonography 39.6 38.3 37.0 38.4 36.5 38.6 0.364 CT scan 47.3 49.7 52.4 60.5 60.1 59.4 <0.001 Interventional treatment Non-operative 72.3 70.4 66.7 65.7 67.9 66.4 <0.001
Pigtail or small-bore tube drainage 1.5 3.4 4.9 4.9 13.9 18.9 <0.001 Intrapleural fibrinolysis 0.9 3.7 4.4 6.1 7.1 9.3 <0.001 Operative 27.7 29.6 33.3 34.3 32.1 33.6 <0.001 VATS 0.2† 23.8 <0.001 Resource use Vasopressor use 23.1 26.5 26.3 26.5 24.9 24.8 0.895 Hemodialysis 3.2 3.9 4.9 5.4 6.3 6.3 <0.001
MV 35.1 39.7 44.5 48.3 45.8 46.1 <0.001 ICU stay 37.0 43.8 49.1 51.5 49.1 49.8 <0.001 MV duration, d 4 (214) 5 (215) 5 (216) 5 (218) 4 (214) 4 (214) 0.826 ICU LOS, d 4 (212) 5 (211) 4 (211) 5 (213) 5 (212) 5 (212) 0.035 Hospital LOS, d 21 (1332) 20 (1333) 20 (1332) 21 (1335) 20 (1332) 19 (1231) 0.679
Hospital charges, USD
2,697 (1,4475,24 5) 3,124 (1,6386,4 27) 3,447 (1,8117,0 54) 4,104 (2,2348,13 6) 4,252 (2,4307,95 7) 4,413 (2,4978,1 58) <0.001 30-day mortality 15.0 14.9 14.9 14.1 13.5 13.1 0.001
Without organ dysfunction 7.2 6.0 4.9 4.4 3.7 4.6 <0.001
With organ dysfunction 36.6 32.3 30.8 25.0 24.5 22.5 <0.001
Hospital mortality 17.6 18.5 17.3 17.1 16.4 16.0 0.002
30-day readmission 14.9 14.7 14.6 13.6 14.2 13.6 0.087
* Values were expressed as median (inter-quartile range) or percentages.
† These patients were admitted in 2006 and received video-assisted thoracoscopic surgery (VATS) in 2007 when the insurance coverage for VATS started. CT, computed tomography; MV, mechanical ventilation; ICU, intensive care unit; LOS, length of stay; USD, United States dollars.