ORIGINAL ARTICLE
Comparison of clinical outcome and urodynamic findings
using
“Perigee and/or Apogee” versus “Prolift anterior
and/or posterior
” system devices for the treatment
of pelvic organ prolapse
Cheng-Yu Long&Chun-Shuo Hsu&Mei-Yu Jang&Cheng-Min Liu&Po-Hui Chiang&Eing-Mei Tsai
Received: 11 June 2010 / Accepted: 23 August 2010 / Published online: 10 September 2010 # The International Urogynecological Association 2010
Abstract
Introduction and hypothesis This study aims to compare clinical outcome using the Perigee/Apogee® vs. Prolift® devices for the treatment of pelvic organ prolapse (POP). Methods One hundred and eight women with POP stages II to IV were scheduled for either Perigee/Apogee® (Perigee group; n=60) or Prolift® device (Prolift group; n=48). Preoperative and postoperative assessments included pelvic examination, urodynamic study, and a personal interview about urinary and sexual symptoms.
Results Despite different follow-up period (20 months for the Perigee group vs. 12 months for Prolift group; P<0.01), the success rates for two groups were comparable (P>0.05).
Postoperative points Aa and Ba of Prolift group were significantly higher than the other group (P<0.01). The prevalences of detrusor overactivity and urinary symptoms decreased significantly postoperatively in both groups (P<0.05). Comparisons of all operative complications revealed no significant differences between the two groups (P>0.05).
Conclusions Perigee/Apogee® and Prolift® devices for POP repair have comparable success rates, mesh-related morbidities, and similar impacts on functional outcome. Keywords Pelvic organ prolapse . Perigee . Prolift . Urodynamic study
Cheng-Yu Long and Chun-Shuo Hsu contributed equally to this work. C.-Y. Long
:
C.-M. Liu:
E.-M. TsaiGraduate Institute of Medicine,
Center of Excellence for Environmental Medicine, Kaohsiung Medical University,
Kaohsiung, Taiwan C.-Y. Long
Department of Obstetrics and Gynecology, Kaohsiung Municipal Hsiao-Kang Hospital, Kaohsiung Medical University,
Kaohsiung, Taiwan C.-S. Hsu
Department of Obstetrics and Gynecology, Buddhist Dalin Tzu Chi General Hospital, Chiayi, Taiwan
M.-Y. Jang
Department of Urology, Kaohsiung Municipal Hsiao-Kang Hos-pital, Kaohsiung Medical University,
Kaohsiung, Taiwan
P.-H. Chiang
Department of Urology,
Chang Gung Memorial Hospital-Kaohsiung Medical Center, Chang Gung University, College of Medicine,
Kaohsiung, Taiwan
E.-M. Tsai
Department of Obstetrics and Gynecology, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
E.-M. Tsai (*)
Department of Obstetrics and Gynecology, Kaohsiung Municipal Hsiao Kang Hospital, 482 Shan-Ming Road, Hsiao-Kang Dist. 812, Kaohsiung, Taiwan
e-mail: K83263@kmhk.kmu.edu.tw DOI 10.1007/s00192-010-1262-6
Abbreviations
POP Pelvic organ prolapse
POP-Q POP quantification
TVT Tension-free vaginal tape
USI Urodynamic stress incontinence
DO Detrusor overactivity
OAB Overactive bladder
TOT Transobturator tape
Introduction
It has been estimated that 11% of all women will undergo some type of operation for pelvic organ prolapse (POP) or urinary incontinence in their lifetime, with 29% needing a second operation for recurrence within 5 years [1]. Traditional anterior and posterior colporrhaphies have been the established treatment for POP over the last century but carry a higher rate of recurrence [1]. Therefore, surgery with implantation of mesh or graft materials has become increasingly popular over the last decade due to the excellent short-term cure rate [2,3].
Recently, a number of mesh materials and devices have been designed by different companies. Perigee/Apogee® (AMS, Inc., Minnetonka, MN, USA) and Prolift® system (Gynecare Prolift, Ethicon, Inc., Piscataway, NJ, USA) are examples of synthetic mesh kits recently developed and adopted in pelvic reconstruction. These non-absorbable meshes allow surgeons to reinforce the pubocervical and the rectovaginal fascia via minimally invasive approaches. However, limited comparative data are available on the comparisons of efficacy and safety following these two graft-reinforced POP surgeries.
Over 75% women undergoing POP repair fall into the age group of postmenopausal women [2]. It remains a critical issue that should be discussed with patients regarding changes in urinary and sexual symptoms following the POP surgery. Reviewing the literature, few papers have studied both surgical efficacy and functional results. Besides, lack of standardized surgical techniques further complicates interpretation of these literatures. Thus, we selected two marketed commercial kits (Perigee/Apogee® and Prolift® system) with synthetic meshes in this study and compared their clinical effects on POP.
Materials and methods
From June 2004 through December 2008, 130 consecutive women with POP stages II to IV defined by the POP quantification (POP-Q) staging system [4] were referred for transvaginal mesh procedures (70 Perigee and/or Apogee;
60 Prolift devices) at our hospital. Concomitant midurethral sling operations, including tension-free vaginal tape (TVT; Gynecare TVT, Ethicon, Inc., Piscataway, NJ, USA), TVT-O (Gynecare TVT-Obturator System, Ethicon, Inc., Somerville, NJ, USA), and Monarc (AMS, Inc., Minnetonka, MN, USA), were performed in women with current or occult urodynamic stress incontinence (USI). Twenty-two patients were excluded due to various reasons, including incomplete medical records (n=12; seven women in Perigee group, five in Prolift group) and current use of anticholinergic drugs (n=10; five women in Perigee group, five in Prolift group). Finally, the remaining 108 women were divided into the Perigee group (n=60) and Prolift group (n=48).
Preoperative and postoperative assessments included pelvic examination using the POP-Q system, multichannel urodynamic study, and a personal interview to identify urinary and sexual symptoms with the standardized questionnaire taking into account the 2002 ICS definitions [5] and the Female Sexual Function Index [6]. Nocturia was defined as“the complaint that the individual has to wake at night one or more times to void. Urge urinary incontinence was defined as ‘the complaint of involuntary leakage accompanied by or immediately preceded by urgency”.
Urodynamic studies, including spontaneous uroflowmetry, filling and voiding cystometry, and urethral pressure profilometry, were performed according to the recommenda-tions by the International Continence Society [7] with a six-channel urodynamic monitor (MMS; UD2000, Enschede, The Netherlands). Any uninhibited detrusor contraction during filling cystometry was deemed positive for idiopathic detrusor overactivity (DO). USI was defined as involuntary urine leakage with cough in the absence of detrusor contraction during cystometry. The diagnosis of occult USI was made by the occurrence of urinary leakage during the reduction of POP.
Perigee–Apogee and Prolift systems are similar with only subtle differences in the posterior procedure involved. In the Prolift procedure for apical and posterior prolapse, the trocar is inserted 3 cm lateral and inferior to the anus. The needle is designed to pass through the sacrospinous ligament at a level of 2 cm posterior and medial to the ischial spine. The Apogee system uses the same insertion location, but with a more helical trocar that pierces the ileococcygeus muscle rather than the sacrospinous ligament at the level of the ischial spine. During anterior mesh repair, superior trocars of both devices are inserted through the upper medial angle of the obturator foramen at the level of the clitoris, while the inferior trocars are inserted 2 cm inferior and 1 cm lateral to the upper incisions [8]. All trocars are designed to pass through the arcus tendineus and emerge with the vaginal incision.
The synthetic mesh arms of both systems are then connected to the corresponding passers and brought out
through the skin wounds. Then, cystoscopy was performed to exclude any bladder injury and to confirm intact ureters. The synthetic mesh is positioned under the bladder and fixed with 3–0 Prolene sutures proximally and distally. The vaginal mucosa is closed with 3–0 polyglactin sutures. The skin incisions are closed using Dermabond® and vaginal packing is placed for 24–48 h. All patients were given antibiotic prophylaxis (intravenous Cefazolin 1 g; Cefamezin, Fujisawa, Tokyo, Japan) administered before surgery. The operations were carried out with the patients under spinal, epidural, or general anesthesia. All surgeries were performed mainly by the first author (C.Y.L.), with individual experience of more than 100 transvaginal POP repairs.
Postoperative follow-up was scheduled at 1, 3, 6, and 12 months and then yearly beyond 1 year. All POP-Q points were measured by the first author. Recurrence was defined as most distal portion of POP stage II or greater, regardless of primary or new site. Ethics approval by the Institutional Review Board of our hospitals had been obtained for retrospective data analysis. A statistical analysis was performed using Student’s t test, Mann– Whitney U, McNemar’s or Wilcoxon signed rank test for continuous variables, and the chi-square or Fisher’s exact test for categorical variables. A difference was considered statistically significant when P<0.05.
We assessed the power of tests for differentiating the surgical outcome between groups, and power analysis showed that around 50 to 70 women in each group would have a power of 80%. Although some comparisons, such as recurrent rate, could not reach sufficient power because of the limited numbers of the two groups, we used multiple parameters of POP-Q system, especially the points Aa and Ba, to evaluate the postoperative changes. We found that with >40 women in each group, there was a power of more than 85% for discrimination.
Results
Participant characteristics of both groups are compared in Table1. There was no difference between the two groups with regards to age, parity, current hormone use, diabetes, hypertension, prior history of hysterectomy or POP repair, and concomitant procedures (P>0.05). However, we found that the mean follow-up time was significantly longer in the Perigee group (20 vs. 12 months; Mann–Whitney U test; P<0.01).
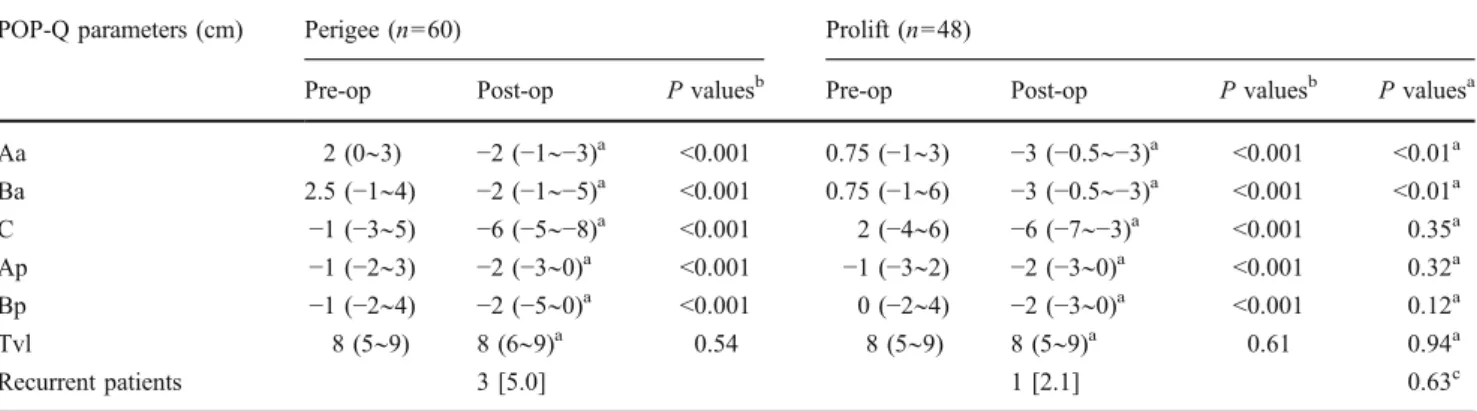
As for the POP-Q analysis, there was a significant improvement at points Aa, Ba, C, Ap, and Bp (P<0.001) in both groups except for total vaginal length (P>0.05; Table2). Moreover, postoperative points Aa and Ba of the Prolift group were significantly higher than those in the Perigee group (P<0.01), and other POP-Q points between the two groups did not differ significantly (P>0.05;
Table2). The overall success rate for our two groups was 96.3% (104 out of 108) after average follow-up period of 12–20 months. The rate of recurrence was comparable in both groups (P>0.05; Table2).
The prevalences of urinary symptoms in both groups, including urinary frequency, stress incontinence, incomplete bladder emptying, urinary hesitancy, and nocturia, were found to be significantly lower following transvaginal mesh repair (P<0.01). In addition, the rate of urge urinary incontinence decreased significantly in the Prolift group (P=0.012), but this was not the case in the Perigee group (P>0.05; Table3).
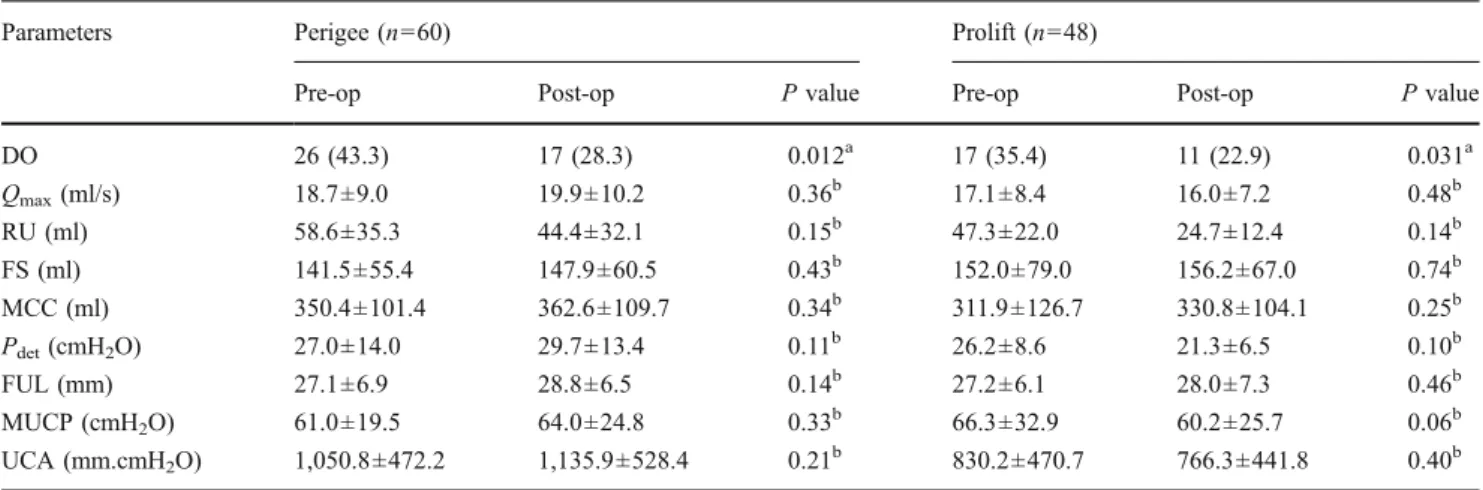
The percentage of DO decreased significantly postoper-atively in both groups (P<0.05; Table 4). However, other urodynamic parameters, including maximum flow rate, residual urine, maximum cystometric capacity, functional urethral length, maximum urethral closure pressure, and urethral closure area, revealed that analogous parameters were not significantly different following the Perigee and Prolift procedures (P>0.05; Table4).
In regard to intraoperative complications including bladder injury, rectal injury, and transfusion, none was suspected and confirmed by cystoscopic and rectal examinations. All postoperative complications in both groups included urinary tract infection in 15 women (13.9%), voiding dysfunction (difficulty initiating the void) in three (2.8%), pelvic hematoma in one (0.9%), and de novo dyspareunia in 22 (20.4%). The insignifi-cant rates of de novo or worsened dyspareunia were 25% and 16.7% in the Prolift and Perigee groups, respectively. Chi-square and Fisher’s exact tests showed no significant differences between both devices in other intraoperative and postoperative comparisons (P>0.05; Table 5).
The rate of vaginal erosion was higher in the Prolift group (eight out of 48; 16.7% vs. six out of 60; 10%), but did not reach statistical significance (P>0.05; Table 5). In the Perigee group, there were four erosions found in anterior vaginal wall and two in posterior vaginal wall, and the corresponding figures of the Prolift group were four erosions in each wall. One woman had both erosions in the Prolift group. All vaginal erosions were detected on pelvic examination between 6 and 24 weeks after POP surgery and only one woman with erosion larger than 2 cm in size. All women were initially treated conservatively with vaginal estrogen cream, although 11 of them (seven in the Prolift group, four in Perigee group) subsequently required debridement of the exposed mesh. One woman had persistent erosion requiring repeat excision after 2 months.
Discussion
With the advance of graft materials for the treatment of female POP, synthetic mesh has the advantages of strength
and durability over traditional anterior and posterior colporrhaphies [3]. Biological grafts were developed to overcome the possibility of erosion and rejection, yet one concern is their ability to provide long-term support to the weakened fascia. Recent report of Ramanah et al. [9] found that the use of biocompatible porcine dermal graft was well tolerated but had similar efficacy to traditional colporrhaphy and sacrospinous ligament suspension. Moreover, criticism has been directed as to whether the DNA found in a biologic graft is transmissible or immunological [10], and a graft-vs.-host disease following transobturator tape (TOT) with porcine small intestine submucosa was reported recently [11]. Therefore, we
included the two most popular marketed kits (Perigee® and Prolift® systems) for comparison in this study.
The efficacy of anatomical correction was comparable in both groups even if the longer follow-up in the Perigee group. Later launch of the Prolift® device accounted for the shorter mean follow-up time in this group. The overall success rate of 96.3% (104 out of 108) for our two groups is similar to other studies by Abdel-fattah and Ramsay [2] and Fatton et al. [12], both reporting the same 95% cure rates at 3-month follow-up. Interestingly, we found that postoperative points Aa and Ba of the Prolift group were significantly deeper than those in the Perigee group. A possibility was that penetration of sacrospinous ligament
Perigee (n=60) Prolift (n=48) P values
Mean age (years) 57.7±12.0 60.9±10.2 0.14a
Mean parity 3.2±1.4 3.5±1.5 0.32a
Mean BMI (kg/m2) 24.5±3.1 25.0±3.4 0.39a
Menopause 41 (68.3) 37 (77.1) 0.31
Current hormone therapy 11 (19.4) 10 (20.8) 0.74b
Current smokers 2 (3.3) 1 (2.1) >0.99c
Diabetes mellitus 9 (15.0) 7 (14.6) 0.95b
Hypertension 23 (38.3) 18 (37.5) 0.93b
History of hysterectomy 7 (11.7) 9 (18.8) 0.30b
History of POP repair 5 (8.3) 3 (6.3) 0.73b
Procedures in this study
Anterior mesh repair 36 (60.0) 23 (47.9) 0.21b
Anterior and posterior mesh repair 24 (40.0) 25 (52.1) 0.21b
Posterior repair 1 (1.7) 2 (4.2) 0.58c
Vaginal hysterectomy 6 (10.0) 2 (4.2) 0.30c
Suburethral sling 35 (58.3) 30 (62.5) 0.51b
Follow-up time (months) 20 [12–60] 12 [12–38] <0.01d
Table 1 Clinical background of patients with pelvic organ prolapse in both groups
Data are given as mean ± standard deviation, median [range], or n (percent) BMI body mass index, POP pelvic organ prolapse
aStudent’s t test b
Chi-square test
cFisher’s exact test dMann–Whitney U test
Table 2 Pelvic organ prolapse quantification values in both groups before and after surgery
POP-Q parameters (cm) Perigee (n=60) Prolift (n=48)
Pre-op Post-op P valuesb Pre-op Post-op P valuesb P valuesa
Aa 2 (0∼3) −2 (−1∼−3)a <0.001 0.75 (−1∼3) −3 (−0.5∼−3)a <0.001 <0.01a Ba 2.5 (−1∼4) −2 (−1∼−5)a <0.001 0.75 (−1∼6) −3 (−0.5∼−3)a <0.001 <0.01a C −1 (−3∼5) −6 (−5∼−8)a <0.001 2 (−4∼6) −6 (−7∼−3)a <0.001 0.35a Ap −1 (−2∼3) −2 (−3∼0)a <0.001 −1 (−3∼2) −2 (−3∼0)a <0.001 0.32a Bp −1 (−2∼4) −2 (−5∼0)a <0.001 0 (−2∼4) −2 (−3∼0)a <0.001 0.12a Tvl 8 (5∼9) 8 (6∼9)a 0.54 8 (5∼9) 8 (5∼9)a 0.61 0.94a Recurrent patients 3 [5.0] 1 [2.1] 0.63c
Data are given as median (range) or n [percent]
Pre-op preoperative, Post-op postoperative, Tvl total vaginal length
aMann–Whitney U test bWilcoxon signed rank test cFisher’s exact test
provided better postoperative support of the apical com-partment in Prolift group. However, it is hard to draw a conclusion due to the shorter follow-up and the less advanced anterior vaginal prolapse of the Prolift group.
Nearly half of our patients undergoing POP surgery will have multi-compartmental types of prolapse requiring repair of each. It would therefore be impractical to identify a population undergoing anterior mesh alone. Dysfunctional voiding in itself can be multi-factorial and should not be considered to be solely related to anterior vaginal wall prolapse. As such, the inclusion of repairs from other compartments may be an additional advantage and results in a higher resolution of voiding dysfunction [13]. As expected, significant improvement of obstructive and irritative urinary symptoms were observed in both groups. The cure of stress urinary incontinence was mainly related to the combination of midurethral sling with the POP surgery in women with current or occult USI.
Previous studies reported that the incidence of overactive bladder (OAB) symptoms increased significantly when
POP repair and TVT were performed together [14].
Although concomitant midurethral slings were implanted in the majority of our patients (65 out of 108), we did not observe this phenomenon. This may be due to the fact that the majority of our patients underwent the TOT rather than TVT procedure. The horizontal orientation of the TOT tape may be less obstructive [15, 16] and causes less irritative symptoms. However, whether the TOT is more suitable in women with preoperative OAB symptoms remains unclear. There is a high prevalence of changeable urinary symptoms in postmenopausal women, while most women undergoing POP surgery fall into this age group [2]. Previous studies have also shown the aging process as a significant etiologic factor of OAB symptoms [17]. Post-operative changes in urinary symptoms therefore were assessed within a short-term interval (6 months) in our study to control for this confounding factor. In spite of this
Table 4 Urodynamic changes in both groups before and 6 months after surgery
Parameters Perigee (n=60) Prolift (n=48)
Pre-op Post-op P value Pre-op Post-op P value
DO 26 (43.3) 17 (28.3) 0.012a 17 (35.4) 11 (22.9) 0.031a Qmax(ml/s) 18.7±9.0 19.9±10.2 0.36b 17.1±8.4 16.0±7.2 0.48b RU (ml) 58.6±35.3 44.4±32.1 0.15b 47.3±22.0 24.7±12.4 0.14b FS (ml) 141.5±55.4 147.9±60.5 0.43b 152.0±79.0 156.2±67.0 0.74b MCC (ml) 350.4±101.4 362.6±109.7 0.34b 311.9±126.7 330.8±104.1 0.25b Pdet(cmH2O) 27.0±14.0 29.7±13.4 0.11b 26.2±8.6 21.3±6.5 0.10b FUL (mm) 27.1±6.9 28.8±6.5 0.14b 27.2±6.1 28.0±7.3 0.46b MUCP (cmH2O) 61.0±19.5 64.0±24.8 0.33b 66.3±32.9 60.2±25.7 0.06b UCA (mm.cmH2O) 1,050.8±472.2 1,135.9±528.4 0.21b 830.2±470.7 766.3±441.8 0.40b
Data are given as n (%) or mean ± standard deviation
DO detrusor overactivity, Qmaxmaximum flow rate, RU residual urine, FS first sensation to void, MCC maximum cystometric capacity, Pdet
detrusor pressure at peak flow, FUL functional urethral length, MUCP maximum urethral closure pressure, UCA urethral closure area
aMcNemar’s test b
Paired t test
Perigee (n=60) Prolift (n=48)
Symptoms Pre-op Post-op P value Pre-op Post-op P value
Urinary frequency 40 (66.7) 16 (26.7) <0.01a 37 (77.1) 17 (35.4) <0.01a SUI 45 (75.0) 9 (15.0) <0.01a 26 (54.2) 12 (25.0) <0.01a UUI 25 (41.7) 19 (31.7) 0.18a 18 (37.5) 9 (18.8) 0.012a Incomplete emptying 38 (63.3) 5 (8.3) <0.01a 37 (77.1) 2 (4.2) <0.01b Urinary hesitancy 23 (38.3) 1 (1.7) <0.01b 32 (66.7) 0 <0.01b Nocturia 29 (48.3) 17 (28.3) <0.01a 25 (52.1) 15 (31.3) <0.01a
Table 3 Urinary symptoms of patients with pelvic organ prolapse in both groups before and 6 months after surgery
Data are given as n (percent) SUI stress urinary incontinence, UUI urge urinary incontinence
a
McNemar’s test
retrospective analysis, all of our data were collected prospectively as standard surveys for patient care visits. We believe that this can minimize the limitation of the study design.
In our study, the postoperative rate of DO was observed to be significantly lower in both groups. A possible explanation would be that severe POP could cause bladder outlet obstruction by urethral kinking or external compres-sion [18], which can promote uninhibited detrusor contrac-tions. Our findings of postoperative OAB improvement after mesh repair can be simply related to the release of urethral obstruction. In addition, urge urinary incontinence decreased significantly in the Prolift group and not in Perigee group. This may be partly due to the fact of lower detrusor pressure after the Prolift procedure, although the changes did not reach statistical significance.
Theoretically, low flow rate and higher residual urine on urodynamic study should be improved following the POP surgery. However, we did not find any significant changes in all urodynamic parameters postoperatively, in accordance with another study [19]. Urodynamic study may not have been sensitive enough to detect all subtle changes in voiding dysfunction. Not every woman experiencing POP stage IV in this study may be the other reason why we did not observe this correlation.
The use of blind introducers of commercial available kits has given rise to some concerns. A systemic review showed a total of 1.9% of visceral injury for anterior and/or posterior mesh repair [3]. We were fortunate to avoid these complications completely in both groups. We evaluated transfusion rate instead of the amount of blood loss because the source is not only from the repair of POP but also from concomitant procedures such as midurethral sling or hysterectomy.
The vaginal erosion rate for the Prolift group (eight out of 48; 16.7%) was higher than the Perigee group (six out of 60; 10%), but it did not reach statistical significance. The conservative management of these women with vaginal erosion was disappointing. Although all women were initially treated conservatively with vaginal estrogen cream, the majority subsequently required debridement of the exposed mesh. The overall vaginal erosion rate (14 out of 108; 13%) in our study was similar to the figure of 12.7% reported by Collinet et al. [20], yet it was much higher than the 4.7% reported by Fatton et al. [12]. A previous study showed that mesh erosion after POP repair is more likely to occur with concomitant hysterectomy [21]. Similar results were observed in our series; four mesh erosions occurred in women undergoing concomitant hysterectomy (four out of eight; 50%) and another ten in women without hysterectomy (ten out of 100; 10%).
Previous study reported a higher rate of dyspareunia following transvaginal mesh repair, although an improve-ment was observed with time and a resolution at 24 weeks follow-up [22]. Therefore, we assessed the sexual function at 6 months after surgery. In spite of the larger size of the Prolift mesh, the insignificant rates of de novo or worsened dyspareunia were 25% and 16.7% in the Prolift and Perigee groups, respectively. Interestingly, combination of posterior and anterior mesh repair appeared to have limited impact on dyspareunia compared with anterior mesh only. The majority of postmenopausal subjects in this study may contribute to a higher postoperative rate of de novo or worsened dyspareunia than the report of Nguyen and Burchette [23].
In conclusion, the results of our study suggested that Perigee® and Prolift® devices for POP repair had compa-rable success rates and mesh-related morbidities. A
weak-Perigee (n=60) Prolift (n=48) P values
Intraoperative complications
Bladder injury 0 0
Rectal injury 0 0
Blood transfusion 0 0
Postoperative complications
Urinary tract infection 7 (11.7) 8 (16.7) 0.46a
Voiding dysfunction 2 (3.3) 1 (2.1) 0.69b
Perineal hematoma 0 1 (2.1) 0.26b
De novo or worsened dyspareunia 10 (16.7) 12 (25.0) 0.29a
Anterior mesh only 7 (11.7) 6 (12.5) 0.90a
Anterior plus posterior mesh 3 (5.0) 6 (12.5) 0.18b
Mesh complications
Vaginal erosion 6 (10.0) 8 (16.7) 0.31a
Bladder erosion 0 0
Table 5 Intraoperative, postop-erative, and mesh-related complications of patients with pelvic organ prolapse in both groups
Data are given as n (percent)
aChi-square test bFisher’s exact test
ness of the study was that we did not collect data regarding the satisfaction of patients and quality of life after the procedure. Although the Prolift mesh created a deeper anatomical position of anterior vaginal wall than the Perigee device, it did not have a greater impact on functional outcome. Women with advanced POP can expect significant resolution of irritative and obstructive symptoms after transvaginal mesh repair. More prospective randomized trials and longer follow-up of anatomical and functional results are urgently needed to guide the appropriate use of mesh or graft in the future.
Acknowledgments This study was supported by grants from Kaohsiung Municipal Hsiao Kang Hospital (kmhk-98-0330). The authors appreciate the artwork provided by Dr. Sin-Di Lee.
Conflicts of interest None.
References
1. Olsen A, Smith V, Bergstrom J, Colling J, Clark A (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
2. Abdel-fattah M, Ramsay I (2008) Retrospective multicentre study of the new minimally invasive mesh repair devices for pelvic organ prolapse. BJOG 115:22–30
3. Jia X, Glazener C, Mowatt G, MacLennan G, Bain C, Fraser C et al (2008) Efficacy and safety of using mesh or grafts in surgery for anterior and/or posterior vaginal wall prolapse: systematic review and meta-analysis. BJOG 115:1350–1361
4. Bump RC, Mattiasson A, Bo K et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
5. Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21:167–178
6. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R et al (2000) The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26:191–208
7. Abrams P, Blaivas JG, Stanton SL et al (1990) The standardization of terminology of low urinary tract function recommended by the international continence society. Int Urogynecol J 1:45–58 8. Debodinance P, Berrocal J, Clave H, Cosson M, Garbin O,
Jacquetin B et al (2004) Changing attitudes on the surgical treatment of urogenital prolapse: birth of the tension-free vaginal mesh. J Gynécol Obstét Biol Reprod 33:577–588
9. Ramanah R, Mairot J, Clement MC, Parratte B, Maillet R, Riethmuller D (2010) Evaluating the porcine dermis graft InteXen in three-compartment transvaginal pelvic organ prolapse repair. Int Urogynecol J Pelvic Floor Dysfunct 21:1151–1156
10. Choe JM, Bell T (2002) Genetic material is present in cadaveric dermis and cadaveric fascia lata. J Urol 166:122–124
11. Wang CL, Hsu CS, Long CY (2009) Graft-versus-host disease following transobturator tape procedure with small intestinal submucosa (surgisis): a case report. Int Urogynecol J Pelvic Floor Dysfunct 20:1149–1151
12. Fatton B, Amblard J, Debodinance P, Cosson M, Jacquetin B (2007) Transvaginal repair of genital prolapse: preliminary results of a new tensionfree vaginal mesh (Prolift technique)—a case series multicentric study. Int Urogynecol J 18:743–752
13. Dietz H, Haylen B, Vancaillie T (2002) Female pelvic organ prolapse and voiding function. Int Urogynecol J 13:284–288 14. Diez-Itza I, Aizpitarte I, Becerro A, Sarasqueta C (2009)
Incidence of overactive bladder after vaginal hysterectomy and associated repairs for pelvic organ prolapse. Gynecol Obstet Investig 68:65–70
15. Long CY, Hsu CS, Lo TS, Liu CM, Chen YH, Tsai EM (2008) Ultrasonographic assessment of tape location following tension-free vaginal tape and transobturator tape procedure. Acta Obstet Gynecol Scand 87:116–121
16. Long CY, Hsu CS, Wu MP, Liu CM, Wang TN, Tsai EM (2009) Comparison of tension-free vaginal tape and transobturator tape procedure for the treatment of stress urinary incontinence. Curr Opin Obstet Gynecol 21:342–347
17. Chen GD, Lin TL, Hu SW, Chen YC, Lin LY (2003) Prevalence and correlation of urinary incontinence and overactive bladder in Taiwanese women. Neurourol Urodyn 22:109–117
18. Long CY, Long CY, Hsu SC, Wu TP, Sun DJ, Su JH, Tsai EM (2004) Urodynamic comparison of continent and incontinent women with severe uterovaginal prolapse. J Reprod Med 49:33–37
19. Chin HY, Chiang CH, Lin KC, Wang CJ, Lee CL, Soong YK (2009) Prospective assessment of overactive bladder symptoms in women who have undergone transvaginal surgery for advanced vaginal wall prolapse: a preliminary report. J Obstet Gynaecol Res 35:732–737
20. Collinet P, Belot F, Debodinance P, Ha Duc E, Lucot JP, Cosson M (2006) Transvaginal mesh technique for pelvic organ prolapse repair: mesh exposure management and risk factors. Int Urogynecol J Pelvic Floor Dysfunct 17:315–320
21. Cervigni M, Natale F, La Penna C, Panei M, Mako A (2008) Transvaginal cystocele repair with polypropylene mesh using a tension-free technique. Int Urogynecol J Pelvic Floor Dysfunct 19:489–496
22. Shah DK, Paul EM, Rastinehad AR, Eisenberg ER, Badlani GH (2004) Short-term outcome analysis of total pelvic reconstruction with mesh: the vaginal approach. J Urol 171:261–263
23. Nguyen JN, Burchette RJ (2008) Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol 111:891–898