The effects of exercise training on walking function
and perception of health status in elderly patients
with peripheral arterial occlusive disease
J . C . T S A I1, P . C H A N2, C . H . W A N G1, C . J E N G1, M . H . H S I E H2, P . F . K A O2, Y . J . C H E N2 & J . C . L I U2
From the1Institute of Nursing, Taipei Medical University, and2Department of Medicine, Taipei Medical University-Wan Fang Hospital, Taipei,
Taiwan
Abstract. Tsai JC, Chan P, Wang CH, Jeng C, Hsieh MH, Kao PF, Chen YJ, Liu JC (Taipei Medical Uni-versity-Wan Fang Hospital, Taipei, Taiwan). The effects of exercise training on walking function and perception of health status in elderly patients with peripheral arterial occlusive disease. J Intern Med 2002; 252: 448–455.
Objective. To determine the effects of 12-week exercise programme on ambulatory function, free-living daily physical activity and health-related quality of life in disabled older patients with inter-mittent claudication.
Design. Prospective, randomized controlled trial. Setting. University Medical Center and Veterans Affairs Medical Center, Taipei, Taiwan.
Subjects. Thirty-two of 64 patients with Fontaine stage II peripheral arterial occlusive disease (PAOD) were randomized to exercise training and 32 to usual care control. Five patients from the exercise group and six patients from the control group dropped out, leaving 27 and 26 patients, respect-ively, completing the study in each group.
Interventions. Twelve weeks of treadmill exercise training.
Main outcome measures. Treadmill walking time to onset of claudication pain and to maximal
claudication pain, 6-min walk distance, self-reported ambulatory ability and perceived health-related quality of life (QOL).
Results. Compliance of exercise programme was 83% of the possible sessions. Exercise training increased treadmill walking time to onset of claudi-cation pain by 88% (P < 0.001), time to maximal pain by 70% (P < 0.001), and 6-min walk distance by 21% (P < 0.001).
Subjects. Perception of health-related QOL improved from 12% to 178% in the exercise group. These improvements were significantly better than the changes in the control group (P < 0.05).
Conclusions. Significant improvements in claudi-cation following 12-week exercise training in elderly PAOD patients were observed. Increase in treadmill walking time to maximal claudication pain in these patients translated into the improve-ment of perceived physical health, which enabled the patients to become more functionally inde-pendent.
Keywords: exercise training, intermittent claudi-cation, peripheral arterial occlusive disease, quality of life, treadmill.
Introduction
Peripheral arterial occlusive disease (PAOD) is a leading cause of morbidity in elderly persons because of ambulatory limitations associated with intermittent claudication [1]. Symptomatic PAOD is
common in western industrialized countries [2]. PAOD patients frequently experience intermittent claudication during ambulation because peripheral circulation is inadequate to meet the energy needs of the active leg musculature. Ambulatory dysfunction in patients with intermittent claudication [3–6]
results in a sedentary lifestyle [7], self-perceived ambulatory dysfunction [8] and lower health-related quality of life (QOL) [9]. Patients who have ischaemic pain at rest or limb-threatening ischaemia may undergo intervention therapy (e.g. percutane-ous transluminal angioplasty or peripheral arterial bypass). Because the majority of PAOD patients are not at risk for immediate tissue loss, the primary therapeutic goal is to improve ambulatory function through exercise rehabilitation [10]. Consequently, interventions should focus on improving ambula-tory function to maintain functional independence in PAOD patients with intermittent claudication.
The impact of improved claudication symptoms following exercise rehabilitation on quantitative measures of ambulatory function in the community setting is not well known. Because a low level of daily physical activity is an independent risk factor for coronary heart disease incidence and mortality [11–13], increased free-living daily physical activity in PAOD patients following exercise rehabilitation may improve their poor prognosis for long-term survival [14–16].
The purpose of this prospective, randomized controlled trial was to determine whether a 12-week progressive treadmill exercise rehabilitation programme was more effective than nonexercise usual care in improving ambulatory function, self-reported ambulatory ability and health-related QOL in older PAOD patients functionally limited by intermittent claudication.
Materials and methods
All patients lived independently at home and had Fontaine Stage II PAOD [17], defined by the following criteria: (1) a positive Rose questionnaire for intermittent claudication [18], and (2) an ankle/brachial systolic blood pressure index (ABI) of £ 0.95 [8, 19]. The self-reported duration of intermittent claudication in years and the number of blocks walked before claudication pain were recor-ded. Patients were excluded from participation for the following reasons: (1) rest pain; (2) history of exertional angina; (3) exercise tolerance limited by leg pain of nonvascular origin (e.g. arthritis, ortho-paedic pain) and by factors other than intermittent claudication (e.g. dyspnoea, fatigue, dizziness); (4) surgery related to PAOD during the preceding 3 months; (5) myocardial infarction within the
preceding 3 months and (6) unstable claudication symptoms during the preceding 3 months. The procedures used in this study were approved by the institutional review board at the Taipei Medical University. A written informed consent was obtained from each patient before this investigation. Data were collected before and after the 12-week exercise training programme.
Treadmill exercise test
Patients performed a progressive, graded treadmill protocol (2 mph, 0% grade with 2% increase every 2 min) until maximal claudication pain. The sever-ity of claudication pain experienced by the patient was recorded on a scale of 0–4 with 0¼ no pain, 1¼ onset claudication, 2 ¼ mild, 3 ¼ moderate and 4 ¼ severe pain [20]. The time walked to onset of claudication pain (score 1 out of a possible range of 0–4), and time to maximal claudication pain (score 4) for each subject were measured. During treadmill tests, each subject was fitted with a 12-lead electrocardiogram system. Arm blood pressures were monitored every 2 min. The exercise test was terminated if any subject exhibited >1 mm ST-segment change, significant dysrhythmias, an appropriate blood pressure response to increasing workloads, or reported a score of maximal claudi-cation pain. In this study, all subjects reached a maximal level of claudication pain that limited exercise during the graded treadmill test.
Six-minute walk test
Each patient was administered a 6-min walk test by two trained technicians twice within 1 week. Each technician administered the 6-min walk test blinded from the results of the other. Two cones were placed 20 m apart in a marked corridor. Patients were instructed to walk as many laps around the cones as possible and to inform the technician when the onset of claudication occurred. A calibrated elec-tronic pedometer (Omron Health Care Corporation, Vernon Hills, IL, USA) was worn on the hip of each patient to obtain the total number of steps taken during the test. The technician stood at the centre of the 20-m course and provided encouragement every 2 min. Patients were permitted to stop walking during the test if their claudication became intoler-able, but the time continued to run during the rest
period. Patients who stopped walking because of claudication pain were encouraged to continue walking as soon as possible. The technician recorded the total distance walked and total number of steps taken during the rest. Using these procedures, we have established high intertechnician reliability in our laboratory; the intraclass correlation coefficient (R) for the 6-min walk measurements ranged between 0.93 and 1.00, and the coefficient of variation (CV) ranged between 0.5% and 1.5%.
Ankle/brachial index (ABI) test
Patients refrained from smoking and drinking caffeinated beverages during the morning of testing. Ankle systolic blood pressure and brachial systolic blood pressure were measured, and ABI was calcu-lated as ankle systolic pressure/brachial systolic pressure.
The patients rested supine for 10 min under standardized laboratory condition before the ABI measurement. The ankle systolic blood pressure was obtained in the posterior tibial and dorsalis pedis arteries of both legs by a Parks Medical Electronics, Inc. nondirectional Doppler flow detector (Model 810 A, Aloka, Tokyo, Japan), a pencil probe (9.3 MHz), and standard size ankle blood pressure cuffs (10 cm width). The artery yielding the highest pressure in the more severely diseased leg was used for the ankle systolic blood pressure. The test–retest R and CV values were 0.95% and 11.8% for ankle systolic pressure and 0.95% and 12.8% for ABI using this methodology [4].
Brachial blood pressures and heart rate were measured from both arms with a Critikon Dinamap Vital Signs Monitor (Parks, Model 1846, TX, USA), using a standard adult size blood pressure cuff (14 cm width). Brachial systolic pressure, diastolic pressure and heart rate were recorded from the arm yielding the higher systolic pressure. In a subsample of 44 participants tested twice in our laboratory within 2 weeks, the test–retest R and CV values were 0.82% and 11.4% for systolic pressure, 0.83% and 8.7% for diastolic pressure, and 0.84% and 11.8% for heart rate [21, 22].
Walking impairment questionnaire (WIQ)
Self-reported ambulatory ability was assessed using a questionnaire validated for PAOD patients in
which the patients evaluated their walking ability at various speeds and distances and their ability to climb stairs [23]. A scale ranging between 0 and 100 assesses each aspect; a score of 0 represents inability and a score of 100 represents no difficulty in performing the task. The WIQ has been widely used in PAOD population to examine the effect of exercise rehabilitation on patients’ functional status [23, 24].
Quality of life
Health-related QOL was assessed with the Medical Outcomes Study Short-Form 36 (MOS SF-36) Chinese version [25, 26]. The MOS SF-36 is a reliable and valid generic instrument that includes the following eight multi-item subscales that assess the physical and mental health components of QOL: physical function, role limitations caused by phys-ical problems (role limitations/physphys-ical), general health, bodily pain, social function, role limitations caused by emotional problems (role limitations/ emotional), mental health and vitality. Respondents were asked to evaluate their own health during the past 30 days. Each domain of these scales is scored from 0 (poorest health) to 100 (optimal health). The psychometric properties of the MOS SF-36 have been examined extensively and support its validity and reliability [25–27]. The MOS instrument also has been widely used in studies to evaluate multiple aspects of life function in PAOD population [8, 10, 24].
Exercise training protocol
Patients in the exercise group performed the treadmill exercise three times each week until 12 weeks. Exercise training began with 5 min of warm-up and ended with 5 min of cool down. During exercise, patients’ heart rate and 12-lead electrocardiogram were continuously monitored to detect any exercise-induced dysrhythmias. Arm blood pressure values and claudication pain scores were collected every 5 min Exercise intensity star-ted from 2 mph, 0% grade, with 1% grade increase every 10 min if patients reported a claudication pain score below 2. Patients were encouraged to exercise up to 30 min with their claudication pain scores between 2 and 3 (pain levels between mild and moderate).
Statistical analyses
Descriptive data are given as mean ± SD for baseline variables. For treatment effects, Wilcoxon sign rank test or Mann–Whitney U nonparametric tests were used. The absolute change compared with baseline was used for the analysis of treatment effect for each group as well as for the comparison between groups. Correlations were analysed as Spearman’s rank correlations. P < 0.05 in two-sided tests were regarded as statistically significant.
Results
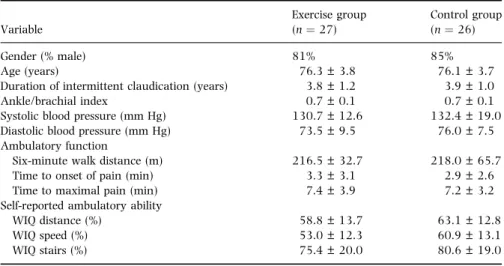
The mean age of the patients in this study was 76.2 years. The baseline clinical characteristics and ambulatory function were comparable in both the groups (Table 1). Baseline characteristics of the five exercise and six controls who withdrew after randomization were also similar to the patients who completed the study. Body mass index did not differ significantly between the exercise and control groups (23.6 ± 2.0 vs. 23.0 ± 3.0 kg m)2) and did not change with the intervention.
The mean compliance rate in the 27 exercises was 82 ± 16% (SD), with 22 patients attending at least 80% of the sessions. The skewed nature of data towards higher compliance did not permit calculation of the dose–response effect of exercise. Nevertheless, the intention-to-treat analyses inclu-ded the patients who were less compliant with the
exercise programme. There were no complications during the exercise sessions or in the control patients that could be attributed to participation in the study.
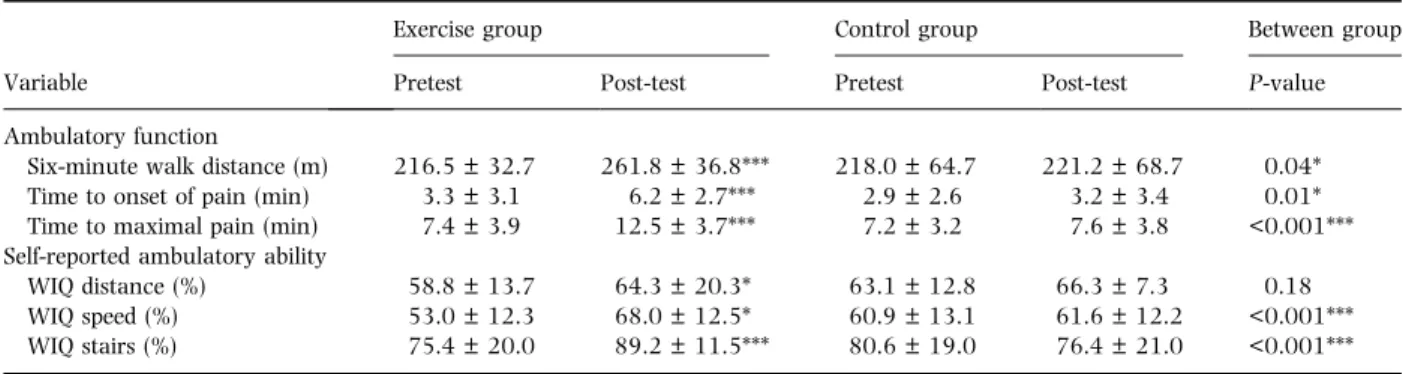
The exercise training programme increased time to onset of claudication pain and to maximal pain during treadmill tests by an average of 88% and 70% (P < 0.001), respectively. These improvements were significantly better than those observed in the controls (Table 2). The total 6-min walk distance increased by 21% (P < 0.05) in the exercise group, these changes were also significantly better than in the controls (Table 2). In the exercise group, the change in the 6-min walk distance correlated with the change in time to onset of claudication pain (r¼ 0.48, P < 0.05) and time to maximal pain (r¼ 0.53, P < 0.001).
The baseline scores on the three WIQ subscales were similar between the two groups (Table 1). The exercise group reported significant higher scores on the distance, speed and stair subscales on the WIQ after the training programme. The changes in speed and stair subscales were most remarkable and were significantly different from the changes in the controls (Table 2).
Individual subscales of the MOS SF-36 were also analysed for each patient. There were no signifi-cant differences in all subscores of the MOS SF-36 between the two groups at baseline. In comparison with the baseline data, the exercise group reported significantly higher scores on five subscales of the
Table 1 Baseline clinical charac-teristics of patients with peripheral arterial occlusive disease and intermittent claudication who completed the study
Variable Exercise group (n¼ 27) Control group (n¼ 26) Gender (% male) 81% 85% Age (years) 76.3 ± 3.8 76.1 ± 3.7
Duration of intermittent claudication (years) 3.8 ± 1.2 3.9 ± 1.0 Ankle/brachial index 0.7 ± 0.1 0.7 ± 0.1 Systolic blood pressure (mm Hg) 130.7 ± 12.6 132.4 ± 19.0 Diastolic blood pressure (mm Hg) 73.5 ± 9.5 76.0 ± 7.5 Ambulatory function
Six-minute walk distance (m) 216.5 ± 32.7 218.0 ± 65.7 Time to onset of pain (min) 3.3 ± 3.1 2.9 ± 2.6 Time to maximal pain (min) 7.4 ± 3.9 7.2 ± 3.2 Self-reported ambulatory ability
WIQ distance (%) 58.8 ± 13.7 63.1 ± 12.8
WIQ speed (%) 53.0 ± 12.3 60.9 ± 13.1
WIQ stairs (%) 75.4 ± 20.0 80.6 ± 19.0
Values are percentage of patients for gender and the remaining variables are mean ± SD in each category.
MOS SF-36 following the 12-week exercise training programme (Table 3). The improvements in the physical health component (physical function, role limitations caused by physical problems, bodily pain and general health) were more pronounced than that in the mental health component on the MOS SF-36. The improvements in perceived phys-ical function and bodily pain subscores correlated well with the increase in time to maximal claudi-cation pain (r¼ 0.66 and 0.65, P < 0.05). No changes in all subscores of the MOS SF-36 were observed in the controls during the study period (Table 3).
Discussion
Patients with intermittent claudication have an impact on walking ability that may limit their
function to meet the personal or social demands of daily living. A structured exercise programme helps to improve exercise performance and possibly, functional status in PAOD patients [8, 10]. Prelim-inary results in a study by Regensteiner et al. [24] also suggested that a supervised treadmill training programme was more effective for improving exer-cise performance than an unsupervised, home-based programme. In our study, treadmill walking was used as the mode of training to enhance patients’ walking ability. Training intensity was set to the workload that brought on mild to moderate claudi-cation pain in the patients.
The primary findings of this study were that 12 weeks of exercise training increased the time to onset of claudication pain by 88% and to maximal claudication pain by 70%. These improvements in ambulatory function translated into an increase in
Table 2 Ambulatory functions in patients with peripheral arterial occlusive disease and intermittent claudication before and after randomization into 12 weeks of exercise training (n¼ 27) or usual care control (n ¼ 26)
Variable
Exercise group Control group Between group Pretest Post-test Pretest Post-test P-value Ambulatory function
Six-minute walk distance (m) 216.5 ± 32.7 261.8 ± 36.8*** 218.0 ± 64.7 221.2 ± 68.7 0.04* Time to onset of pain (min) 3.3 ± 3.1 6.2 ± 2.7*** 2.9 ± 2.6 3.2 ± 3.4 0.01* Time to maximal pain (min) 7.4 ± 3.9 12.5 ± 3.7*** 7.2 ± 3.2 7.6 ± 3.8 <0.001*** Self-reported ambulatory ability
WIQ distance (%) 58.8 ± 13.7 64.3 ± 20.3* 63.1 ± 12.8 66.3 ± 7.3 0.18 WIQ speed (%) 53.0 ± 12.3 68.0 ± 12.5* 60.9 ± 13.1 61.6 ± 12.2 <0.001*** WIQ stairs (%) 75.4 ± 20.0 89.2 ± 11.5*** 80.6 ± 19.0 76.4 ± 21.0 <0.001*** Values are mean ± SD, *P < 0.05, ***P < 0.001. Between group P-value are pretest–post-test differences between exercise and control groups.
Table 3 Health-related quality of life and self-perceived ambulatory measures in patients with peripheral arterial occlusive disease and intermittent claudication before and after randomization into 12 weeks of exercise training
Variable
Exercise group Control group Between group Pretest Post-test Pretest Post-test P-value Physical function 39.5 ± 0.1 58.0 ± 10.6*** 49.2 ± 11.5 48.0 ± 9.6 <0.001*** Role limitations/Physical 22.5 ± 30.0 62.5 ± 31.7** 22.9 ± 19.8 33.3 ± 16.3 0.04* Bodily pain 64.8 ± 15.9 81.5 ± 18.4* 71.1 ± 20.4 77.3 ± 17.8 0.03* General health 54.0 ± 13.4 64.8 ± 0.1* 57.5 ± 11.6 56.4 ± 16.0 0.02* Mental health 70.9 ± 14.6 80.1 ± 0.1 77.6 ± 9.4 78.7 ± 6.6 0.08 Role limitations/emotional 83.3 ± 36.0 93.3 ± 21.1 90.0 ± 0.2 91.0 ± 3.2 0.12 Social function 76.3 ± 20.8 85.0 ± 17.5 78.1 ± 26.7 82.3 ± 15.5 0.23 Vitality 54.5 ± 15.2 70.0 ± 12.9*** 60.8 ± 16.2 63.8 ± 2.1 0.02* Values were obtained from the Medical Outcomes Study Short-Form 36 and are presented as mean ± SD, *P < 0.05, **P < 0.01, ***P < 0.001, Between group P-value are pretest–post-test differences between exercise and control groups.
6-min walk distance. Patients with claudication rarely need to walk at the intensity attained during a maximal, graded treadmill test. Thus a 6-min walk test provides more clinically relevant information on the benefits of exercise training in allowing these patients with PAOD to perform activities of daily living.
Different mechanisms appear to explain the exercise-mediated increase in ambulatory function. Improvements in walking economy and calf perfu-sion are two mechanisms that act synergistically to relieve claudication by decreasing the metabolic demand of walking and increasing oxygen delivery, respectively. However, exercise-mediated improve-ments in peripheral circulation in PAOD patients with intermittent claudication is not a consistent finding, as some studies report an increase [29–32], although others report no change in perfusion [33– 35]. The better energy utilization in the calf may be the factor which contributes to a delay in the development of claudication, therefore, manifested by increased distances walked.
Furthermore, exercise training improved the self-reported QOL as assessed by the MOS SF-36 and the disease-specific WIQ instrument. This study demon-strates that exercise training improves ambulatory function, perceived walking ability and health related QOL in older PAOD patients with intermittent clau-dication, and supports current recommendations for exercise training in this patient population [28]. This finding is also partially compatible with the signifi-cant increase of 24% to 28% gains in self-reported physical functioning following exercise programmes found in smaller samples of claudicatants [8].
Exercise training resulted in significant changes in health related QOL, especially the increase in physical health components on the MOS SF-36 survey. However, changes in the mental health components on the MOS SF-36 were less remark-able than that in the physical health components amongst our subjects. Several factors may account for this result. In our cohort of chronically ill PAOD patients, ambulatory dysfunction may be the most important factor influencing self-perceived health-related QOL. It is also possible that the perceived improvements in the mental health component of QOL may lag behind the improvements in ambu-latory function achieved at 12 weeks. Regensteiner and colleagues [8] found that a supervised treadmill
training programme improved the functional status in PAOD, with 24 weeks of training more effective than 12 weeks. In our study, training profits were obvious even in the 12 weeks of training. Further studies are needed to confirm what training duration can be most beneficial for patients with PAOD.
In our study, the majority of patients were men aged 65 or older (male:female ratios were approxi-mately 8:1). One explanation for this discrepancy in male:female ratios may be the higher prevalence rate for PAOD in man. Another plausible explan-ation is that men with symptomatic claudicexplan-ation are more likely to obtain medical attention than women [36]. None of the baseline characteristics of our patients, except for age (r¼)0.47, P < 0.05), were independent predictors of the change in 6-min walk distance in response to an exercise training programme. Consequently, PAOD patients with inter-mittent claudication who are not excluded because of severe coronary artery disease, dyspnoea, and poorly controlled blood pressure are capable of increasing their treadmill walking time to onset and to maximal claudication pain following exercise, regardless of gender, laterality of intermittent claudication, duration of claudication symptoms and cardiovascular disease risk factors. Further-more, previous study suggests that baseline mea-sures of claudication distances, perceived ambulatory function, ABI and calf perfusion, and body composi-tion did not predict response [37]. This suggests that all PAOD patients with intermittent claudication, who can safely exercise from a clinical, cardiopul-monary, and orthopaedic standpoint, should be considered as candidates for a treadmill walking programme to improve their symptomatology.
In summary, the primary findings of this pros-pective, randomized controlled trial are that a 12-week programme of exercise training effectively improves ambulatory function by increasing time to onset and to maximal claudication pain, and 6-minutes walk distance in older patients with PAOD functionally limited by claudication. These functional gains translated into increased perceived physical function, which enabled these patients to become more functionally independent. Therefore, exercise training should be considered as part of standard medical care for older patients limited by intermittent claudication.
References
1 Vogt MT, Wolfson SK, Kuller LH. Lower extremity arterial disease and the aging process: a review. J Clin Epidemiol 1992; 45: 529–42.
2 Weitz JI, Byrne J, Clagett GP et al. Diagnosis and treatment of chronic arterial insufficiency of the lower extremities: a crit-ical review. Circulation 1996; 94: 3026–49.
3 Gardner AW. Claudication pain and hemodynamic responses to exercise in younger and older peripheral arterial disease patients. J Gerontol 1993; 48: M231–M236.
4 Gardner AW, Skinner JS, Cantwell BW, Smith LK. Progressive vs. single-stage treadmill tests for evaluation of claudication. Med Sci Sports Exerc 1991; 23: 402–8.
5 Harris KA, Meads GE. A single treadmill exercise test dose not accurately quantitate claudication. Can J Surg 1987; 30: 446–8.
6 Hiatt WR, Nawaz D, Regensteiner JG, Hossack KF. The evaluation of exercise performance in patients with periph-eral vascular disease. J Cardiopulmonary Rehabil 1988; 12: 525–32.
7 Sieminski DJ, Grander AW. The relationship between daily physical activity and the severity of peripheral arterial occlusive disease. Vasc Med 1997; 2: 286–91.
8 Regensteiner JG, Steiner JF, Hiatt WR. Exercise training improves functional status in patients with peripheral arterial disease. J Vasc Surg 1996; 23: 104–15.
9 Feinglass J, McCarthy WJ, Slavensky R, Manheim LM, Martin GS and the Chicago Claudication Outcomes Research Group. Effect of lower extremity blood pressure on physical func-tioning in patients who have intermittent claudication. J Vasc Surg 1996; 24: 503–12.
10 Hiatt WR, Hirsch AT, Regensteiner JG, Brass EP. Clinical trials for claudication: assessment of exercise performance, func-tional status, and clinical endpoints. Circulation 1995; 92: 614–21.
11 Lakka TA, Venalainen JM, Rauramaa R, Salonen R, Tuomilehto J, Salonen JT. Relation of leisure-time physical activity and cardiorespiratory fitness to the risk of acute myo-cardial infarction in men. N Engl J Med 1994; 330: 1549–54. 12 Leon AS, Connett J, Jacobs DR Jr, Rauramaa R. Leisure-time physical activity levels and risk of coronary heart disease and death: the Multiple Risk Factor Intervention Trial. JAMA 1987; 258: 2388–95.
13 Paffenbarger RS Jr, Hyde RT, Wing AL, Hsieh C-C. Physical activity all-cause mortality, and longevity of college alumni. N Engl J Med 1986; 314: 605–13.
14 McGrae-McDermott M, Feinglass J, Slavensky R, Slavensky R, Pearce WH. The ankle-brachial index as a predictor of sur-vival in patients with peripheral vascular disease. J Gen Intern Med 1994; 9: 445–9.
15 McKenna M, Wolfson S, Kuller L. The ratio of ankle and arm arterial pressure as an independent predictor of mortality. Atherosclerosis 1991; 87: 119–28.
16 Vogt MT, Cauley JA, Newman AB, Kuller LH, Hulley SB. Decreased ankle/arm blood pressure index and mortality in elderly women. JAMA 1993; 270: 465–9.
17 Pentecost MJ, Criqui MH, Dorros G et al. Guidelines for per-ipheral percutaneous transluminal angioplasty of the abdominal aorta and lower extremity vessels. Circulation 1994; 89: 511–31.
18 Rose G, McCartney P, Reid DD. Self-administration of a questionnaire on chest pain and intermittent claudication. Br J Prev Soc Med 1977; 31: 42–8.
19 Carter S. Response of ankle systolic pressure to leg exercise in mild or questionable arterial disease. N Engl J Med 1972; 287: 578–82.
20 American College of Sports Medicine. ACSM’s Guideline for Exercise Testing and Prescription, 5th edn. Media, PA: Williams & Wilkins, 2000.
21 Gardner AW, Sieminski DJ, Montgomery PS. Physical activity is related to ankle/brachial index in subjects without peri-pheral arterial occlusive disease. Angiology 1997; 48: 883– 91.
22 Gardner AW, Sieminski DJ, Killewich LA. The effect of cigarette smoking on free-living daily physical activity in older claudication patients. Angiology 1997; 48: 947–55. 23 Regensteiner JG, Steiner JF, Panzer RJ, Hiatt WR. Evaluation
of walking impairment by questionnaire in patients with peripheral arterial disease. J Vasc Med Biol 1990; 2: 142–52. 24 Regensteiner JG, Meyer TJ, Krupski WC, Cranford LS, Hiatt WR. Hospital vs home-based exercise rehabilitation for patients with peripheral arterial occlusive disease. Angiology 1997; 48: 291–300.
25 Fuh JL, Wang SJ, Lu SR, Juang KD, Lee SJ. Psychometric evaluation of a Chinese (Taiwanese) version of the SF-36 health survey among middle-age women from a rural com-munity. Quality Life Res 2000; 9: 679–83.
26 Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). Med Care 1992; 30: 473–83.
27 McHorney CA, Ware JE, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): psychometric and clinical tests of validity in measuring physical and mental health con-structs. Med Care 1993; 31: 247–63.
28 Hiatt WR, Hirsch AT, Regensteiner JD, Brass EP. Clinical trials for claudication: assessment of exercise performance, func-tional status, and clinical end points. Circulation 1995; 92: 614–21.
29 Womack CJ, Sieminski DJ, Katzel LI, Yataco A, Gardner AW. Improved walking economy in patients with peripheral arterial occlusive disease. Med Sci Sports Exerc 1997; 29: 1286–90. 30 Alpert JS, Larsen A, Lassen NA. Exercise and intermittent
claudication: blood flow in the calf muscle during walking studied by the Xenon-133 clearance method. Circulation 1969; 39: 353–9.
31 Hall JA, Barnard RJ. The effects of an intensive 26-day pro-gram of diet and exercise on patients with peripheral vascular disease. J Cardiac Rehabil 1982; 2: 569–74.
32 Jonason T, Ringqvist I. Effect of training on the post-exercise ankle blood pressure reaction in patients with intermittent claudication. Clin Physiol 1987; 7: 63–9.
33 Dahllof AG, Bjorntorp P, Holm J, Schersten T. Metabolic activity of skeletal muscle in patients with peripheral arterial insufficiency: effect of physical training. Eur L Clin Invest 1974; 4: 9–15.
34 Larsen OA, Lassen NA. Effect of daily muscular exercise in patients with intermittent claudication. Lancet 1966; 2: 1093–6.
35 Ruell PA, Imperial ES, Bonar FJ, Thursby PF, Gass GC. Intermittent claudication: the effect of physical training on walking tolerance and venous lactate concentration. Eur J Appl Physiol 1984; 52: 420–5.
36 McDermoff MM, McCarthy W. Intermittent claudication: the natural history. Surg Clin N Am 1995; 75: 581–91. 37 Gardner AW, Katzel LI, Sorkin JD et al. Exercise rehabilitation
improves functional outcomes and peripheral circulation in patients with intermittent claudication: a randomized con-trolled trial. J Am Geriatr Soc 2001; 49: 755–62.
Received 13 June 2002; revision received 22 August 2002; accepted 5 September 2002.
Correspondence: Dr Jen-Chen Tsai, Institute of Nursing, Taipei Medical University, #250 Wu-Hsing Street, Taipei, Taiwan 110 (fax: 886 22377 2842; e-mail: jenchent@tmu.edu.tw).