With increasing numbers of patients with cancer, AIDS, and other chronic, life-threatening illnesses, the care of patients with a terminal illness is be-coming an important issue for doctors. Physicians’ knowledge of palliative care and competence re-lating to ethical decision-making about end-of-life care are widely accepted to be deficient, which results in patients near the end of their
lives receiving unsatisfactory care.1 Two major reasons for unsatisfactory care are inadequate or inappropriate education about palliative care and the paucity of ethical decision-making training in the care of dying patients and their families. Before 1995, the average palliative care training time was < 10 hours in the United States and Canada.2 Previously, palliative care curricula in
©2009 Elsevier & Formosan Medical Association
. . . .
1Department of Family Medicine, College of Medicine and Hospital, National Taiwan University, Bei-Hu Branch; 2School of Nursing, and 3Department of Medical Education, National Taiwan University Hospital; and 4Department of Family Medicine, College of Medicine and Hospital, National Taiwan University, Taipei, Taiwan.
Received: September 4, 2008 Revised: January 7, 2009 Accepted: January 12, 2009
*Correspondence to: Dr Tai-Yuan Chiu, Department of Family Medicine, College of Medicine and Hospital, National Taiwan University, 7 Chung-Shan South Road, Taipei 100, Taiwan.
E-mail: tychiu@ntuh.gov.tw
Reflections on an End-of-life Care Course for
Preclinical Medical Students
Hao-Hsiang Chang,1Wen-Yu Hu,2Stanley S.L. Tsai,3Chien-An Yao,4Chin-Yu Chen,4Tai-Yuan Chiu4*
Background/Purpose: Undergraduate medical education lacks standardized curricula for teaching
end-of-life care and only sporadic curricula evaluations have been reported. The objectives of this study were to evaluate the effect of a multimodal teaching program on preclinical medical students’ knowledge of palliative care, and their beliefs relating to ethical decision-making.
Methods: This study had a quasi-experimental design. The teaching formats included didactic lectures,
bedside patient care, and interactive discussions. A structured questionnaire evaluated the effects of educa-tional intervention—in terms of knowledge of palliative care and beliefs about common ethical dilemmas relating to end-of-life care in Taiwan.
Results: All 118 students who participated in the study completed the questionnaire. Students showed
sig-nificant improvement (score of 9.97 pre-test vs. 12.73 post-test; p< 0.001) in the 18-item palliative care knowledge questionnaire after educational intervention. Among the four common ethical dilemmas, stu-dents’ beliefs of truth-telling (4.22 vs. 4.54; range 1–5; t= –4.66; p < 0.001) and place of care (4.37 vs. 4.52; range 1–5; t= −2.43; p < 0.05) were significantly improved. Logistic regression showed that the improve-ment in beliefs about ethical decision-making was not significantly influenced by improved knowledge of palliative care.
Conclusion: A 1-week multimodal curriculum for preclinical medical students can improve the knowledge
and beliefs about ethical decision-making in managing terminally ill patients. Clinical skills of symptom management, especially pain control, and ethical decision-making regarding artificial nutrition and hydra-tion should be emphasized in medical educahydra-tion, to promote students’ competence in end-of-life care. [J Formos Med Assoc 2009;108(8):636–643]
the majority of US medical schools consisted of sporadic and isolated lectures. After recognizing this shortcoming, educational programs devel-oped for palliative and end-of-life care have in-creased, and later reports have shown that most medical schools provided palliative or end-of-life care curricula in the United States and the United Kingdom.3,4
There is an increasing awareness of the need for more effective undergraduate curricula for end-of-life and palliative care, and the number of training courses has increased in the past decade. For better quality end-of-life care, education is required to enhance physicians’ ability to care for terminally ill patients. Several types of teach-ing programs have been developed, includteach-ing lectures, the use of role models, clinical problem solving, standardized patients, and multimodal learning courses.5–7Undergraduate medical edu-cation lacks standardized curricula for teaching palliative care and debate continues about what should be taught and how, and when and where the teaching should occur.
In July 2001, a new undergraduate curriculum was implemented at the Medical College of the National Taiwan University. The new curriculum was designed to increase emphasis on humanity in end-of-life care. The teaching formats included didactic lectures, bedside patient care, and inter-active discussions. The goals of the integrated curriculum were to help students understand the needs of terminal patients and their families, to provide total care using the palliative care team, and to increase students’ knowledge of palliative care. The study also aimed to evaluate the effects of a multimodal teaching program on medical students’ knowledge of palliative care, and their beliefs relating to ethical decision-making.
Methods
ParticipantsA total of 118 third-year medical students, who voluntarily attended the 1-week educational pro-gram in the palliative care unit of National Taiwan
University Hospital from 2001 to 2004 were recruited. Undergraduate medical education in Taiwan is composed of six curricular years and a 1-year internship. The third-year medical students were at the preclinical stage. The researchers dis-tributed questionnaires to medical students at the beginning and at the end of the curriculum. The selection of participants and the design of this study were approved by the National Science Council in Taiwan and the Ethics Committee of the hospital.
Description of curriculum
A 1-week end-of-life curriculum called “Humans and Medicine” was developed in 2001 for pre-clinical medical students at the Medical College of the National Taiwan University. The teaching program is provided at the Palliative Care Unit of the National Taiwan University Hospital, and is composed of three learning modules, including a lecture series, bedside patient care, and interac-tive discussions (Table 1). The multidisciplinary faculty consisted of palliative care physicians, clin-ical social workers with expertise in palliative care, a chaplain who has provided spiritual care for several years, and a nurse practitioner who is the leader of the nursing staff in the Palliative Care Unit. The daily training course began with a series of 1-hour lectures on the roles of the physician, nurse, psychologist, social worker, and chaplain, followed by a 6-hour session at the bedside of terminally ill patients and their families, and ended with an interactive discussion with experi-enced palliative-care consultants in the evening.
Instrument
The investigators constructed the instrument in accordance with Taiwanese palliative care charac-teristics, after careful review of the literature in this area.8,9The instrument included demographic information about the participants, knowledge of palliative care, and beliefs relating to ethical decision-making. Demographic data included age, sex, school, religion, and whether or not family or friends have had cancer or have received pal-liative care.
There were 32 statements relating to knowl-edge of palliative care. The participants were asked to answer “true”, “false”, or “not sure”, in response to the description in each statement. Each accu-rate answer was worth 1 point and the answer of not sure was not counted. The reliability index calculated by the Kruder–Richardson Formula 20 was 0.79. According to item discrimination and difficulty analysis, 18 items were retained for analysis, and their Kruder–Richardson index of reliability was 0.71. Of the 18 retained for analy-sis, six items were related to theoretical under-standing of palliative care, and the other 12 were concerned with knowledge of clinical manage-ment. The students were asked to rate the beliefs about ethical decision-making on a 5-point Likert scale from 1, “strongly disagree” to 5, “strongly agree”. The instrument was validated by an expert for content validity. Three medical students com-pleted the questionnaire in order to establish face validity.
Statistical analysis
Data management and statistical analysis were performed using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA). The demographic data were described with frequency, mean, and standard deviation. Wilcoxon signed rank test was used to test the improvement in palliative care knowledge after educational intervention (pre-test vs. post-test). The changes in beliefs toward the common ethical issues in palliative care were assessed with the paired t test. Analysis of variance (ANOVA) was used to test the differences in knowledge and beliefs between subgroups. Univariate analysis
was performed on the improvement of beliefs about ethical issues and the factors potentially contributing to improvement, by independent t tests, χ2tests, and one-way ANOVA. Logistic re-gression was carried out to determine the adjusted values of the factors relating to the improvement in ethical beliefs. Statistical significance was assumed when p< 0.05.
Results
Demographic characteristics
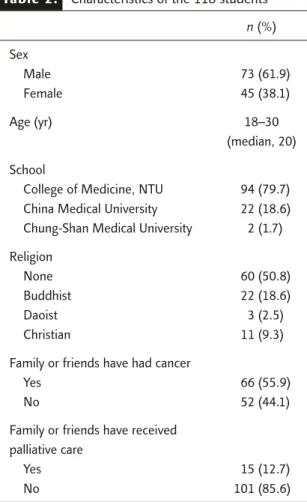
Demographic characteristics of the participants are shown in Table 2. A total of 118 medical stu-dents completed the questionnaires, with a 100% response rate both before and after the educa-tional program. The participants were mainly men (61.9%) and students of National Taiwan University (78.7%). For religious beliefs, 50.8% of the respondents did not have a religious belief, while 18.6% were Buddhists. Only a small propor-tion of the students (12.7%) reported that their friends or family had received palliative care.
Knowledge of palliative care
Participants showed a 14.7% absolute improve-ment in palliative care knowledge, with a total mean score of 9.97 (rate of correct response to the questions, 55.4%) pre-test, and 12.73 (rate of correct response, 70.1%) post-test (range, 0–18; z= 7.790; p < 0.001). The medical students had greater knowledge scores for items relating to theoretical understanding of palliative care, with a mean score of 4.09 (rate of correct response, Table 1. Schema of a 1-week palliative care curriculum
Time Day 1 Day 2 Day 3 Day 4 Day 5
08:00–09:00 Lectures Pre-test; Nursing in Spiritual care in Psychologist in Physician in orientation palliative care palliative care palliative care palliative care 09:00–12:00 Bedside learning: patient care and teamwork
13:00–16:00 Bedside learning: patient care and teamwork Team meeting: Bedside
13:00–15:00 learning 16:00–17:00 Case presentation and discussion with palliative care physicians Post-test
68.2%) and 4.78 (rate of correct response, 79.7%; range, 0–6; z= 4.075; p < 0.001) before and after the curriculum, respectively. A greater absolute improvement (17%) in clinical management was noted, with a mean score of 5.88 (rate of correct response, 49.0%) before the curriculum and 7.95 (rate of correct response, 66.2%) after the cur-riculum (range, 0–12; z= 7.119; p < 0.001). The scores for palliative care knowledge did not differ significantly between different schools, religions, or ages.
Theoretical understanding
The mean rates of correct responses to the state-ments on theoretical understanding of palliative care pre- and post-test are listed in Table 3. The students showed significant improvements for five out of six statements. The statement that did not show improvement was “Men generally rec-oncile their grief more quickly than women” (pre-test, 66%; post-test, 63%). The statement “The palliative care team provides bereavement support for family after the patient’s death” had the highest rate of correct responses at pre-test (87%) and post-pre-test (100%). The statement Table 2. Characteristics of the 118 students
n (%) Sex Male 73 (61.9) Female 45 (38.1) Age (yr) 18–30 (median, 20) School
College of Medicine, NTU 94 (79.7) China Medical University 22 (18.6) Chung-Shan Medical University 2 (1.7) Religion
None 60 (50.8)
Buddhist 22 (18.6)
Daoist 3 (2.5)
Christian 11 (9.3)
Family or friends have had cancer
Yes 66 (55.9)
No 52 (44.1)
Family or friends have received palliative care
Yes 15 (12.7)
No 101 (85.6)
NTU = National Taiwan University.
Table 3. Improvement in palliative care knowledge in theoretical understanding after the curriculum in the 118 students
Rate of correct response (%) Pre-test Post-test
p
1. Palliative care is appropriate only in situations where there 34 51 0.005* is evidence of a downhill trajectory or deterioration
2. Men generally reconcile their grief more quickly than 66 63 0.516
women
3. The philosophy of palliative care is compatible with that 62 75 0.009* of aggressive treatment
4. The palliative care team actively manages pain and other 80 96 < 0.001†
symptoms of terminal patients
5. The palliative care team provides bereavement support 87 100 < 0.001†
for family after the patient’s death
6. Palliative care is an alternative for the curative 81 94 0.002*
non-responsive patient
Mean 68.1 79.7 < 0.001†
Total 4.09 4.78
“Palliative care is appropriate only in situations where there is evidence of a downhill trajectory or deterioration” had the lowest rate of correct responses at pre-test (34%) and post-test (51%).
Knowledge of clinical management
Table 4 shows the scores of 12 items regarding knowledge of clinical management in palliative care. Students demonstrated a significant improve-ment for eight out of 12 items according to the Wilcoxon signed rank test. The students had a high knowledge level for the following three items: “Adjuvant therapies are important in managing
pain” (pre-test, 93%; post-test, 97%); “General malaise is the most common symptom of ad-vanced cancer patients; both pharmacological and non-pharmacological therapy are important” (pre-test, 83%; post-(pre-test, 94%); and “Support is an important treatment for dyspnea in terminal patients” (pre-test, 72%; post-test, 88%).
Particularly low scores were noted for the fol-lowing three items: “Drug addiction is a major concern when morphine is used on a long-term basis for pain management” (pre-test, 14%; post-test, 37%); “During the terminal stages of an ill-ness, drugs that can cause respiratory depression Table 4. Improvement in palliative care knowledge in clinical management after the curriculum in the
118 students
Rate of correct response (%) Pre-test Post-test
p
1. Morphine is the standard used to compare the analgesic effect 50 70 < 0.001* of other opioids
2. The extent of the disease determines the method of pain 72 80 0.117
treatment
3. Adjuvant therapies are important in managing pain 93 97 0.059
4. During the last days of life, the drowsiness associated with 32 55 < 0.001* electrolyte imbalance may decrease the need for sedation
5. Drug addiction is a major concern when morphine is used on 14 37 < 0.001* a long-term basis for pain management
6. Individuals who are taking morphine should also follow a bowel 52 86 < 0.001* regimen
7. During the terminal stages of an illness, drugs that can cause 24 32 0.086 respiratory depression are appropriate for the treatment of
severe dyspnea
8. At high doses, codeine causes more nausea and vomiting than 24 32 0.050†
morphine
9. The loss of a distant or contentious relationship is easier 29 42 0.019†
to resolve than the loss of one that is close or intimate
10. General malaise is the most common symptom of advanced 83 94 0.005‡
cancer patients; both pharmacological and non-pharmacological therapy are important
11. Morphine is commonly used in cancer pain and should follow 43 81 < 0.001* the rules of by mouth, by the clock and by ladder
12. Support is an important treatment for dyspnea in terminal 72 88 < 0.001* patients
Mean 49.0 66.3 < 0.001*
Total 5.88 7.95
are appropriate for the treatment of severe dys-pnea” (pre-test, 24%; post-test, 32%); and “At high doses, codeine causes more nausea and vomiting than morphine” (pre-test, 24%; post-test, 32%).
The students showed greater absolute im-provements for items relating to opioid use, such as: “Morphine is commonly used in cancer pain and should follow the rules of by mouth, by the clock and by ladder” (which improved by 38% from pre-test to post-test); “Individuals who are taking morphine should also follow a bowel regimen” (which improved by 34%); and “Drug addiction is a major concern when morphine is used on a long-term basis for pain management” (which improved by 23%).
Beliefs relating to ethical decision-making Table 5 shows the strength of the students’ beliefs (measured using a 5-point Likert scale) relating to the four common ethical decision-making items, and the comparisons between pre-and post-test scores (a high belief score indicates that more students belief that the statement is true). Medical students had the highest level of belief for the issue “Discharge planning and home care is ethical for terminal patients” (mean, 4.37; range, 1–5) at pre-test and “Truth telling is helpful to a good death” (mean, 4.54; range, 1–5) at post-test. The participants showed signif-icant improvements between pre- and post-test scores for these two issues. The participants had the lowest belief score for the issue “Artificial nutrition and hydration have no benefit for ter-minal patients” either before (mean, 3.69; range,
1–5) or after (mean, 3.64; range, 1–5) the edu-cational program.
Comparisons of beliefs between demographic characteristics revealed that students who had fam-ily members who had died from cancer agreed more with the belief about artificial nutrition and hydration (mean difference± standard devi-ation, 0.89± 0.34). Factors potentially contribut-ing to the improvement of beliefs about ethical decision-making, such as demographic charac-teristics, knowledge scores of principles, and clin-ical knowledge scores of skills, were analyzed by univariate and stepwise logistic regression anal-ysis. These factors did not appear to be signifi-cant predictors of improvements in beliefs about ethical decision-making.
Discussion
To the authors’ knowledge, this study is one of the first to assess the effects of a 1-week, multimodal, palliative-care curriculum in the Asia-Pacific region. Medical students showed sig-nificant improvements in palliative care knowl-edge and beliefs about ethical decision-making after participating in the curriculum. The stu-dents showed a 14.7% improvement in knowl-edge from pre-test to post-test, a finding similar to those of previous studies.6,10
The majority of medical students in Taiwan did not have adequate palliative care knowledge (mean rate of correct response, 55.5% pre-test) before an end-of-life curriculum. They had Table 5. Beliefs relating to common ethical decisions before and after the curriculum in the 118 students
Pre-test Post-test t p
1. Truth-telling is helpful to a good death 4.22 4.54 −4.666 < 0.001*
2. Discharge planning and home care is ethical 4.37 4.52 −2.429 0.017†
for terminal patients
3. Artificial nutrition and hydration have no 3.69 3.64 0.267 0.790
benefit for terminal patients
4. It is ethical to give sedation for refractory 3.78 4.16 −0.926 0.356
symptoms in terminal patients
especially low scores for questions relating to clinical management, but showed improvement after the curriculum. Previous studies have dem-onstrated similar findings.11,12 The modest im-provement in theoretical understanding after educational intervention may have been the re-sult of the high scores before the curriculum. Compared with primary care physicians and dis-trict nurses in Taiwan,12,13 students had lower scores in theoretical understanding principles (students, 79.8%; physicians, 92.7%; nurses, 88.5%), but higher scores in knowledge of clini-cal management (students, 66.3%; physicians, 61.0%; nurses, 43.0%) after the curriculum. The comparisons also demonstrated the effect on the promotion of clinical management knowledge by the curriculum.
About one half of the participants responded correctly to the concept of early intervention and suffering prevention, which is detrimental to quality of end-of-life care. Before the curriculum, only 43.2% of participants knew that opioid use, which relies on the World Health Organization stepwise approach to cancer pain, should be given preferably orally and around the clock. Most of the students thought that addiction would be a major problem when using opioids for cancer pain control. It is worth reinforcing these con-cepts for future education.
Truth disclosure to terminally ill patients is advocated and practiced in Western countries but is thought to have a negative psychological im-pact on patients in Oriental societies. A study in Taiwan has shown that truth disclosure is asso-ciated with a good death in terminal cancer pa-tients.14 The majority of students also strongly agreed that truth disclosure is helpful to a good death, which is consistent with the result of the previous study. Continuing education on truth disclosure in palliative care should be emphasized. In Taiwan, the majority of terminal patients expect to be taken care of at home, but eventu-ally stay in the hospital at the end of their life. The barriers to staying at home include not being able to manage emergency medical conditions, having an insufficient number of caregivers, and
the comfort and convenience of staying in the hospital.15Most students believe that transferring terminal patients from the hospital to a home care program is ethically appropriate, although it is usually difficult. Should palliative care be pro-vided at home, then family caregiver education should be emphasized to overcome barriers.
The study also found that students had the lowest level of belief for the statement “Artificial nutrition and hydration have no benefit for ter-minal patients”. The result is similar to that of a previous study.16 The finding suggests that pa-tients and medical students in Taiwan still believe that ANH can prevent patients from starving to death. However, a study in the United States has shown that medical students had the most sig-nificant improvement on questions relating to this issue.6The discrepancy may be explained by cultural differences. It is worth mentioning that students who had family members who died of cancer had a higher level of belief for the state-ment on ANH. With personal experience, students tended to believe that ANH is not beneficial to terminal patients.
Some studies in Taiwan have revealed that most medical professionals and families feel that it is ethically acceptable to use sedation in termi-nal cancer patients for refractory symptoms;17,18 however, the participants had a relatively low level of belief in this issue prior to the curriculum. This may have been because of unfamiliarity with palliative sedative therapy. Increasing knowledge and clinical experience about palliative sedative therapy will help students to make an appropriate decision for the patient.
As the four common ethical decision-making issues crucially influence the quality of care in hospices,19it is important for physicians to have positive beliefs and adequate skills to deal with them. The study also explored the underlying factors that contribute to the improvement of ethical beliefs, which would be helpful in de-signing a better curriculum for end-of-life care. Knowledge scores, improvement from before to after the curriculum, and personal characteristics were not related to ethical-belief improvement.
As a result, improvement in ethical beliefs may have occurred because of the total effect of the curriculum. Some factors were not identified by the evaluation instrument in the present study, such as clinical role model observation and in-teraction with patients.
Certain caveats should be mentioned in rela-tion to the present study. The participants partic-ipated voluntarily and there was no control group, thus maturation and selection bias have to be con-sidered. The evaluation was limited to the 1-week curriculum design period. A longitudinal study would allow for a better understanding of the in-formation retention pattern of the knowledge and beliefs relating to ethical decision-making in the subsequent years of medical training, including residency and clinical practice.
The combination of lectures by interdiscipli-nary staff, bedside patient care, and interactive discussion is an effective curriculum to improve medical students’ knowledge and beliefs about ethical decision-making with regard to end-of-life care. Clinical management of symptoms, especially pain control, and the issue of ANH should be emphasized in undergraduate curricula throughout residency training.
Acknowledgments
The authors are indebted to the faculty of the Department of Family Medicine, National Taiwan University Hospital, for their full support in conducting this study.
References
1. Billings JA, Block S. Palliative care in undergraduate medical education. Status report and future directions.
JAMA 1997;278:733–8.
2. Charlton R, Ford E. Education needs in palliative care.
Fam Pract 1995;12:70–4.
3. Dickinson GE. A quarter century of end-of-life issues in U.S. medical schools. Death Stud 2002;26:635–46.
4. Field D, Wee B. Preparation for palliative care: teaching about death, dying and bereavement in UK medical schools 2000–2001. Med Educ 2002;36:561–7.
5. Magnani JW, Minor MA, Aldrich JM. Care at the end of life: a novel curriculum module implemented by medical students. Acad Med 2002;77:292–8.
6. Porter-Williamson K, Von Gunten CF, Garman K. Improv-ing knowledge in palliative medicine with a required hos-pice rotation for third-year medical students. Acad Med 2004;79:777–82.
7. Spiegel MJ, Meier DE, Goldhirsch S, et al. Assessing the outcome of a palliative care educational initiative. J Palliat
Med 2002;5:343–52.
8. Ross MM, McDonald B, McGuinness J. The palliative care quiz for nursing (PCQN): the development of an instru-ment to measure nurses’ knowledge of palliative care.
J Adv Nurs 1996;23:126–37.
9. Meekin SA, Klein JE, Fleischman AR, et al. Development of a palliative education assessment tool for medical stu-dent education. Acad Med 2000;75:986–92.
10. Von Gunten CF, Twaddle M, Preodor M. Evidence of im-proved knowledge and skills after an elective rotation in a hospice and palliative care program for internal medicine residents. Am J Hosp Palliat Care 2005;22:195–203. 11. Ogle KS, Mavis B, Rohrer J. Graduating medical students’
competencies and educational experiences in palliative care. J Pain Symptom Manage 1997;14:280–5.
12. Hu WY, Chiu TY, Dai YT, et al. Nurses’ willingness and the predictors of willingness to provide palliative care in rural communities of Taiwan. J Pain Symptom Manage 2003; 26:760–8.
13. Liu WJ, Hu WY, Chiu YF. Factors that influence physicians in providing palliative care in rural communities in Taiwan.
Support Care Cancer 2005;13:781–9.
14. Leung KK, Chiu TY, Chen CY. The influence of awareness of terminal condition on spiritual well-being in terminal cancer patients. J Pain Symptom Manage 2006;31:449–56. 15. Hu WY, Chiu TY, Cheng YR, et al. Why Taiwanese hospice patients want to stay in hospital: health-care professionals’ beliefs and solutions. Support Care Cancer 2004;12:285–92. 16. Chiu TY, Hu WY, Chuang RB. Terminal cancer patients’ wishes and influencing factors toward the provision of ar-tificial nutrition and hydration in Taiwan. J Pain Symptom
Manage 2004;27:206–14.
17. Chiu TY, Hu WY, Lue BH, et al. Sedation for refractory symptoms of terminal cancer patients in Taiwan. J Pain
Symptom Manage 2001;21:467–72.
18. Hu WY, Chiu TY, Cheng SY, et al. Morphine for dyspnea control in terminal cancer patients: is it appropriate in Taiwan? J Pain Symptom Manage 2004;28:356–63. 19. Chiu TY, Hu WY, Cheng SY, et al. Ethical dilemmas in
palliative care: a study in Taiwan. J Med Ethics 2000;26: 353–7.