INTRODUCTION
In 1980, Mitrofanoff described a method of achieving continent urinary diversion by surgically closing the bladder neck and creating a continent catheterizable stoma from the appendixxNz
. The principles behind the procedure are use of a narrow, supple conduit, which, when brought out to the skin asa catheterizable stoma, will provide continence by acting as a flap-valve and attachment of the
conduit to a low-pressure urine storage reservoir by an antireflux mechanism. Early experience in the pediatric population focused on use of the appendix as the efferent limb, while bladder served as the reservoirxOz
. Further developments have demonstrated that any segment of bowel can be tapered and implanted to achieve continencexPz
. Recently, the Mitrofanoff procedure was applied in those bladder cancer patients who undergoing radical cystectomy and continent urinary diversion
The Use of The Appendix or Tapered Ileal Segment as a
Continent Cathererizable Efferent Limb of
Urinary Reservior
Kuan-Chou Chen
NWing-Ming Lai
OYi-Kuang Chen
PHan-Sun Chiang
NIQI*
Background and Purpose:We report our functional results of ileal continent reservoir, which utilized the modified Mitrofanoff procedure as the continence mechanism in 5 invasive bladder cancer patients post radical cystectomy. Methods: Five invasive bladder cancer patients accepted radical cystectomy with ileal continent reservoir formation and follow-up ranged from 28 to 99 months (mean 53). Three patients accepted modified appendix and two accepted the ileal segment tapering as the continent catheterizable efferent limb. One patient died of metastatic bladder cancer 28 months postoperatively. Results: During the mean follow-up of 53 months, all the 5 patients were satisfied with the ease of performing self-catheterization through the umbilical stoma. Urodynamic evaluations revealed low pressure reservoir and stable sphincter tone without urine leakage. None of patients had stoma stenosis or appendix perforation, catheterization interval increased from 3 to 5 hours as reservoir capacity developed. Conclusion: The appendix or tapered ileal segment seem to be the satisfactory structure for the creation of a continent catheterizable conduit and the placement of stoma in the umbilicus proves to be advantageous in enhancing the patient's body image and quality of life. (FJJM 2005; 3 (2) : 69-74 )
Key words: continent urinary diversion, ileum, appendix, radical cystectomy
Department of Urology, Taipei Medical University Hospital, Taipei, TaiwanN Mercy Sex Counseling & Therapy Center, Taipei, TaiwanO Taipei County San Chung Hospital, , Taipei, TaiwanP College of Medicine, Fu Jen Catholic University, Taipei, TaiwanQ
Submitted April, 22, 2005; final version accepted May, 29, 2005. * Correspondence author: hansun@mails.fju.edu.tw
formation, and the use of the umbilicus as a stomal site preserves normal body image and thus does not interfere with quality of lifexQz. We report our functional results of continent urinary diversion made by ileum, and using the modified Mitrofanoff procedure for the continence mechanism in 5 invasivebladdercancerpatientspostradicalcystectomy.
METHODS
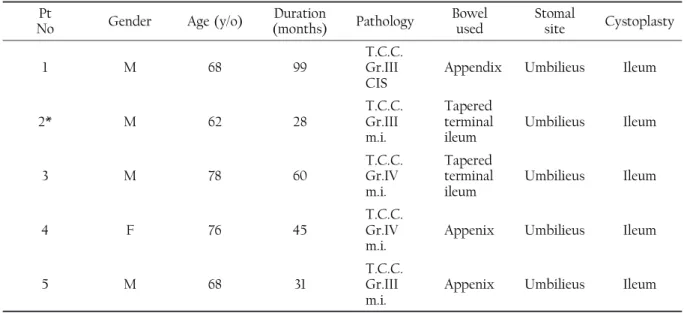
Five invasive bladder cancer patients accepted radical cystectomy with ileal continent reservoir formation and follow-up ranged from 28 to 99 months (mean 53). Three patients accepted modified appendix and two accepted the ileal segment tapering as the continent catheterizable efferent limb. One patient died of metastatic bladder ca ncer 28 months postoperatively (Table 1).
A Brief Introduction Of The Continent Catheterizable Conduit Formation:
After achieving a low-pressure ileal reservoir, the ureter-bladder anastomosis was performed using Le Duc-Camey antireflux method. When the continent catheterizable conduit was constructed by using appendix, the mesoappendix was excised from the distal 2.5-3 cm to allow the fashioning of an adequate submucosal tunnel(Fig 1), and the distal 1 cm was tailored also to allow the formation of a 0.5 cm nipple valve(Fig 2). Antirefluxing connection between the conduit and the reservoir were performed by burying the nipple valve into the lumen of the reservoir with six to eight simple extracorporeal knots(Fig 3), and then the limb was correctly positioned and embedded under the seromucosal layer with a 14Fr. catheter in situ to avoid kinking(Fig 4).The appendico-umblical stoma was created as an oval anastomosis using a V-shaped flap of the umbilical funnel(Fig 5 ). To construct the continent catheterizable conduit by
Table 1. Basic data, bowel segment used and stoma site in the 5 patients
Pt
No Gender Age (y/o) (months)Duration Pathology Bowelused Stomalsite Cystoplasty
1 M 68 99 T.C.C.Gr.III
CIS Appendix Umbilieus Ileum
2* M 62 28 T.C.C.Gr.III
m.i.
Tapered terminal
ileum Umbilieus Ileum
3 M 78 60 T.C.C.Gr.IV
m.i.
Tapered terminal
ileum Umbilieus Ileum
4 F 76 45 T.C.C.Gr.IV
m.i. Appenix Umbilieus Ileum
5 M 68 31 T.C.C.Gr.III
m.i. Appenix Umbilieus Ileum
CIS, carcinoma in situ; m.i., muscle invasion
using tapered ileum segment, a 10-12 cm ileum segment that just distal to the 70 cm ileum segment used for reservoir formation was isolated and tapered to 14 Fr. in diameter. The mesentery was excised from the distal 2.5-3 cm to allow the fashioning of an adequate submucosal tunnel, and the distal 1 cm was tailored also to allow the formation of a 0.5 cm nipple valve. Antirefluxing connection between the conduit and the reservoir were performed by burying the nipple valve into the lumen of the reservoir with six to eight simple extracorporeal knots, and then the limb was correctly positioned and embedded under the seromucosal layer with a 14Fr. catheter in situ to avoid kinking. The conduit-umblical stoma was created as an oval anastomosis using a V-shaped flap of the umbilical funnel.
RESULTS
During the mean follow-up of 53 months, 1 patient died of metastatic bladder cancer, but all the 5 patients were satisfied with the ease of performing self-catheterization throughthe umbilical stoma. Urodynamicevaluations revealed low pressure
Fig 2. The distal 1 cm appendix was tailored to
allow the formation of a 0.5 cm nipple valve.
Fig 1. The mesoappendix was excised from the distal 2.5-3 cm to allow the fashioning of an adequate submucosal tunnel.
Fig 3. Antirefluxing connection between the
conduit and the reservoir were performed by burying the nipple valve into the lumen of the reservoir with six to eight simple extracorporeal knots.
Fig 4. The limb was correctly positioned and
embedded under the seromucosal layer with a14Fr. catheter in situ to avoid kinking.
Fig 5. The appendico-umblical stoma was created
as an oval anastomosis using a V-shaped flap of the umbilical funnel.
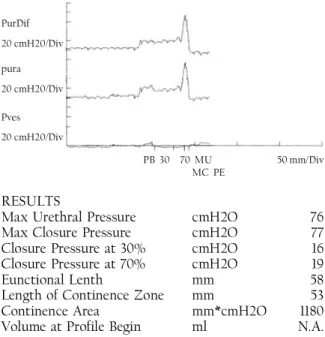
reservoir with capacity 550-650 c.c. and stable sphinctertonewithouturineleakage,therepresentative urodynamic data is shown in Fig 6 with the maximum closure pressure of 77cmH2O in pressure profiles. None of patients had stoma stenosis or appendix perforation, catheterization interval increased from 3 to 5 hours as reservoir capacity developed. None of patients had suffered from ureterovesicle(UV) junction stenosis or UV reflux on follow-up image studies. The patient No 5 who had impaired renal function(serum creatinine:3.2mg/ dl) preoperatively suffered from hypokalemia and progressive renal function impairment(serum creatinine elevated to 4.3mg/dl) during the postoperative OPD follow-up even no evidences of urine retention or incomplete reservoir empty, and these physiological disorders settled down after regular oral potassium supplement.
DISCUSSION
Our study reports a continence rate of 100% by using the modified appendix or tapered ileal segment to create continent catheterizable conduits, with the same satisfactory results as reported by Dr. BissadaxRz
in 1993, and the easy clean intermittent catheterization to be achieved in all patients.
The appendix remains the tissue of choice to fashioncatheterizable channels, and the shortcomings derived from its small caliber require using small catheters to empty the reconstructed bladderxSz. We uniquely used 14 Fr. catheter to drain the bladder urine, and it always worked smoothly. Poor bladder emptying and the pooling of mucus may result in an increased incidence of bladder stone formation. Fortunately, there was no bladder stone formation in our patients after long-term follow-up, it maybe due to the careful patient selection before operation, and they had highly motivation and intelligence to deal with the strict regimen of clean intermittent catheterization so as not to jeopardize the entire procedure. Other tubular structures such as tapered small bowel segments have been reported as alternatives when the appendix is unavailablexTz
. Tapered bowel segments have good mobility but the distal portion has poor vascularity. In addition, long bowel segments (between 10 and 12 cm) are neededxSz . Its thick mesentery must be excised from the distal 2.5-3 cm to allow the fashioning of an adequate submucosal tunnel, and invariably part of this segment becomes ischemic, shortening the tunnel and potentially leading to a stricture. The incidence of difficult catheterization, presumably due to the presence of transverse mucosal folds, as well as stomal stenosis, is also higher with this techniquexUz. In our two patients using tapered ileal segments to fashion catheterizable conduits, there were no above complications noticed at present, and it may PurDif 20 cmH20/Div pura 20 cmH20/Div Pves 20 cmH20/Div PB 30 70 MU 50 mm/Div MC PE RESULTS
Max Urethral Pressure cmH2O 76 Max Closure Pressure cmH2O 77 Closure Pressure at 30% cmH2O 16 Closure Pressure at 70% cmH2O 19
Eunctional Lenth mm 58
Length of Continence Zone mm 53 Continence Area mm*cmH2O 1180 Volume at Profile Begin ml N.A.
Fig 6. The representative urodynamic datashowed the maximum closure pressure of 77cmH2O in pressure profiles.
need further follow-up. Stenosis seems to be the weak point of the appendico-umblical stoma, and it is reported to be avoided by creation of an oval anastomosis using a V-shaped flap of the umbilical funnel instead of the original circular anastomosis xVz
. We used oval anastomosis to deal with the appendico-umblical stoma, and no stenosis was detected.
With rising pressure in the urinary reservoir, compression of the nipple valve mechanismincreases, resulting in a higher resistance to leakagexQz. The appendicular pressure profile of our patients showed the abdomenal wall closing the neosphincter pertinently with the patient supine and providing a completely continent, easily catheterized stoma. The conventional approach to Mitrofanoff appendicovesicostomy with continent urinary stoma to the umbilicus is open surgery. In recent years, several investigators have successfully incorporated laparoscopy into the reconstructive procedure to minimize postoperative patient morbidity and improve cosmesisxNMINNz
. With the advent of Laparoscopic surgery, appendix preservation and usingappendixasthecontinentstomalaparoscopically will be unsolicited. Of course, the experience of the surgeon with laparoscopic techniques and the anatomy of the patient need to be carefully considered before using the described technique.
In conclusion, the appendix or tapered ileal segment seem to be the satisfactory structure for the creation of a continent catheterizable conduit and the placement of stoma in the umbilicus proves to be advantageous in enhancing the patient's body image and quality of life.
REFERENCES
1. Keetch DW, Basler JW, Kavoussi LR, et al. Modification of Mitrofanoff principle for continent urinary diversion. Urology 1993;41:507-510. 2. Bihrle R, Adams MC, Foster RS. Adaptations of
the Mitrofanoff principle in adult continent urinary reservoirs.Tech Urol. Summer 1995;1:94-101. 3. Cendron M, Gearhart JP. The Mitrofanoff principle.
Technique and application in continent urinary diversion. Urol Clin North Am 1991;18:615-621. 4. Marino G, Laudi M. Ileal T-pouch as a urinary
continent cutaneous diversion: clinical and urodynamic evaluation. BJU Int 2002;90:47-50. 5. Bissada NK Characteristics and use of the IN situ
appendix as a continent catheterization stoma for continent urinary diversion in adults J Urol 1993;150:151-152.
6. Figueroa TE, Sabogal L, Helal M, et al: The tapered and reimplanted small bowel as a variation of the Mitrofanoff procedure: preliminary results. J Urol 1994;152:73-75,.
7. Castellan MA, Gosalbez R Jr, Labbie A, et al. Clinical applications of the Monti procedure as a continent catheterizable stoma.Urology 1999; 54:152-156.
8. Monti PR, Carvalho Lara R, Dutra MA, et al: New techniques for construction of efferent conduits based on the Mitrofanoff principle. Urology 1997; 49:112-115.
9. Ramirez OM. Abdominoplasty and abdominal wall rehabilitation: a comprehensive approach. Plast Reconstr Surg 2000;105:425-435.
10. Lorenzo JL, Castillo A, Serrano EA, et al: Urodynamically based modification of Mitrofanoff procedure. J Endourol 1997;11:77-81.
11. Hsu TH, Shortliffe LD. Laparoscopic Mitrofanoff appendicovesicostomy.Urology 2004;64: 802-804.