3610 words
Early improvement predicts outcome of major depressive patients treated
with electroconvulsive therapy
Ching-Hua Lin, M.D., Ph.D.1,2; Wei-Cheng Yang, M.D. 1; Ming-Chao Chen, M.D.1, 2;
Hsien-Yuan Lane, M.D., Ph.D.3,4
1Kaohsiung Municipal Kai-Syuan Psychiatric Hospital, Kaohsiung, Taiwan
2 Department of Psychiatry, School of Medicine, College of Medicine, Kaohsiung
Medical University, Kaohsiung, Taiwan
3Department of Psychiatry, China Medical University Hospital, Taichung, Taiwan 4Institute of Clinical Medical Science, China Medical University, Taichung, Taiwan
Running Title: Early improvement predicts acute ECT outcomes
Corresponding author: Hsien-Yuan Lane, M.D., Ph.D., Department of Psychiatry, China Medical University Hospital (Taiwan), No. 2, Yuh-Der Road, Taichung, Taiwan 404
Tel.: (+886) 921-067-260 Fax: (+886) 4-2236-1042 E-mail: hylane@gmail.com
Abstract
predicts final response and remission for patients with major depressive
disorder (MDD) receiving electroconvulsive therapy (ECT). MDD
inpatients (N=130) requiring ECT were recruited. ECT was generally
performed for a maximum of 12 sessions. Symptom severity was assessed
using the 17-item Hamilton Depression Rating Scale (HAMD-17) before
ECT, after every 3 ECT sessions, and after the last ECT. Early improvement
was defined as a reduction in the HAMD-17 score by at least 20%, 25%, or
30% after 3 and 6 ECT sessions. Response was defined as 60% HAMD-17
score reduction, while remission was defined as an endpoint HAMD-17
score of ≦7. Receiver operating characteristic (ROC) curves were used to
determine whether 3 or 6 ECT sessions had better discriminative capacity.
Sensitivity, specificity and predictive values were calculated for the different
definitions of early improvement. Of the 105 patients entering the analysis,
85.7% (n = 90) and 70.5% (n = 74) were classified as responders and
remitters, respectively. Early improvement after 6 ECT sessions showed
better discriminative capacity, with areas under the ROC curve at least 0.8.
It had high sensitivity and high negative predictive value for all cutoffs in
predicting response and remission. High response and remission rates were
observed. Final response and remission could be predicted by early
improvement after 6 ECT sessions. Patients without early improvement
were unlikely to reach response and remission.
Keywords: major depressive disorder; electroconvulsive therapy; early improvement;
sensitivity; negative predictive value
1. Introduction
Electroconvulsive therapy (ECT) is the most effective short-term treatment for patients with severe or treatment-resistant depression, with 70%–90% of those treated showing improvement (APA, 2010; Group, 2003; Kho et al., 2003; Pagnin et al.,
2004).
The clinical variables and biological markers associated with ECT response have been studied extensively. These predictors include psychosis (Birkenhager et al., 2003; Petrides et al., 2001), a history of medication resistance (Dombrovski et al., 2005; Prudic et al., 1996), duration of the depressive episode (Dombrovski et al., 2005; Haq et al., 2015; Medda et al., 2014), melancholic features (Fink et al., 2007), age (O'Connor et al., 2001), polarity of mood disorder (Sienaert et al., 2009), and brain-derived neurotrophic factor (Brunoni et al., 2014; Lin et al., 2013). However, consistent and reliable predictors remain to be found (Antunes et al., 2009).
Some researchers investigating the relationship between early antidepressant effects of ECT and final outcomes have revealed positive results. For example, Rich et al. (Rich et al., 1984) evaluated response rates in 66 depressed patients, and found that the greatest reduction in Hamilton Depression Rating Scale (HAMD) (Hamilton, 1960) scores took place after the first ECT session, with rapid reduction of HAMD scores during the first 4 ECT sessions, followed by limited further improvements thereafter. Post et al. (Post et al., 1987) studied 8 drug free depressed patients.
Improvement was already noteworthy by days 1 and 3, with 50% improvement by the end of week 1 and nearly maximal improvement at about 2 weeks. Rodger et al. (Rodger et al., 1994) reported on 11 depressed patients treated with 5-6 ECT sessions.
The degree of improvement after three treatments of ECT was six times greater than the improvement that occurred over the remainder of the course. Segman et al. (Segman et al., 1995) found that symptom improvement, defined as ≥ 30%
improvement in HAMD scores after 6 bilateral ECT sessions, correctly identified 33 of 34 final responders and 11 of 13 non-responders. They found that 42.7% of the overall improvement of the responders had occurred by 4-8 sessions of ECT. Patients who had derived no or very little therapeutic effect by the 6th ECT were unlikely to benefit from further treatments, while those who showed an early onset of effect should continue treatment up to 12 ECT sessions. A study by the Consortium for Research in ECT (Husain et al., 2004) indicated that more than half of patients treated with ECT showed improvement after 3 sessions, and 65% achieved remission after 10 sessions. They also found that a 30% improvement in symptoms after 6 sessions could predict final remission. Tsuchiyama et al. (Tsuchiyama et al., 2005) reported that response by session 3 of ECT predicted long-term efficacy in relieving depression. However, interpretation of these finding is restricted by the small sample sizes (8-66 subjects) for most studies (Post et al., 1987; Rich et al., 1984; Rodger et al., 1994; Segman et al., 1995; Tsuchiyama et al., 2005), a retrospective study (Rodger et al., 1994), or utilizing symptom improvement from different numbers of ECT sessions to predict outcomes.
A number of recent studies defined early improvement by symptom reductions of ≥20%, ≥25%, or ≥30% in the early course of acute treatment (mostly at week 1 or 2) for patients with major psychiatric disorders (Correll et al., 2013; Henkel et al., 2009; Kemp et al., 2011a; Kemp et al., 2011b; Leucht et al., 2008; Machado-Vieira et al., 2013; O'Gorman et al., 2011; Szegedi et al., 2009; Szegedi et al., 2003; Vermeiden et al., 2015). These cutoff points are generally applied to represent a clinically
meaningful change after treatment (Szegedi et al., 2003). These studies found that early improvement is a sensitive predictor of final response and remission for
depressed patients treated with antidepressants or psychotherapy, for bipolar patients treated with mood stabilizers or other psychotropic agents, or for schizophrenic patients treated with antipsychotics. Patients who do not achieve early improvement usually have little chance to meet response or remission goals. Based on these clinical prediction models, psychiatrists can decide when it is appropriate to change treatment strategies for a patient without early improvement.
From a clinical perspective, psychiatrists, patients, and their families need to know from the onset of action of ECT. It is clinically critical to determine whether final non-response or non-remission can be accurately predicted at an early stage of treatment. We hypothesized that: 1) early improvement after 3 or 6 ECT sessions would be a sensitive predictor of final response and remission (sensitivity), and that:
2) patients who did not show early improvement would be unlikely to respond or remit at the end of ECT (negative predictive value).
The aim of this study was to extend the results by Segman et al. (Segman et al., 1995) and the Consortium for Research in ECT (Husain et al., 2004), which stated that a 30% improvement in depressive symptoms after 6 ECT sessions could predict final outcomes.
2. Experimental procedures
2.1. Patients
Han Chinese inpatients with major depressive episode (MDE) requiring ECT were recruited from the Inpatient Psychiatric Unit of Kai-Syuan Psychiatric Hospital, a major psychiatric center in Taiwan, between January 2008 and October 2013. Inclusion criteria were that the patients: 1) were aged 18 years or more, 2) satisfied DSM-IV-TR (APA, 2000) criteria for major depressive disorder, confirmed using the Structured Clinical Interview for DSM-IV Axis I (SCID-I) (APA, 1994), 3) had a 17-item Hamilton Rating Scale for Depression (HAMD-17) (Hamilton, 1960) ≥18, and a Clinical Global Impression of Severity (CGI-S) (Guy, 1976) ≥4 at baseline, 4) had given written informed consent, and 5) had not undergone ECT within the past 6 months. Exclusion criteria included those patients who had histories of schizophrenia or other psychotic disorders, schizoaffective disorders, or bipolar disorder. Patients
with neurological illnesses or serious medical conditions that limited the use of ECT were also excluded.
The study was approved by the Kai-Syuan Psychiatric Hospital’s institutional review board and the current revision of the Declaration of Helsinki. This study was registered on Clinical.trials.gov (Identifier number: NCT02032576).
2.2. ECT Protocol
The practice of ECT was based on the American Psychiatric Association Task Force on ECT (APA, 2001). All subjects and their past medical histories, physical and neurological examinations, blood and urine tests, chest X-ray, electrocardiogram (ECG), and electroencephalography (EEG) were evaluated to determine the patients’ general medical conditions prior to undergoing ECT. Psychotropic agents, including antidepressants, antipsychotics, and mood stabilizers, were discontinued for at least 3 days before initiating ECT, and patients remained medication free until completion of post ECT assessments. During the course of treatment, psychiatrists had the option of adding anxiolytic or sedative-hypnotic medications according to clinical necessity. For our ECT protocol, anesthesia was induced by thiopental or thiamylal, both at doses of 1.5 -2.0 mg/kg i.v.. Neuromuscular blockade was induced by succinylcholine at a dosage of 0.5-1.0 mg/kg i.v.. ECT was performed using the Thymatron System IV machine (Somatics, Inc., Lake Bluff, IL, USA) with a bipolar brief pulse square
wave. Subjects were treated with standard bilateral ECT via two stimulus electrodes placed on the left and right frontotemporal scalp. Physiological monitoring during ECT included an electromyogram (EMG), an EEG, an ECG, and a pulse oximetry. The stimulus parameters of ECT were as follows: a pulse width of 0.5 ms, a
frequency of 60 Hz, and a constant current of 0.9 A. Stimulus intensity was first set up according to the patient’s age and gender (Abrams and Swartz, 2002; Petrides and Fink, 1996). Seizure duration, measured by an EEG, was considered effective when it lasted at least 25 seconds (Coffey et al., 1995; Sackeim et al., 1987). If the seizure duration was inadequate, the procedure was repeated with a higher stimulus dosage. Treatment was given two or three times a week, with all ECTs conducted in the morning. The number of ECT sessions was determined on the basis of clinical judgment until a therapeutic response was obtained. The therapeutic response was considered when remission state (i.e., HAMD-17 score of ≤ 7) or a plateau in
improvement had been reached (APA, 2001). If the response was inadequate, further ECT sessions were added by the treating physiatrist. The maximum number of ECT sessions was 12.
2.3. Outcome measures
Symptom severity was assessed at baseline, after every 3 ECT sessions, and after the final ECT by independent raters (board-certified psychiatrists) using HAMD-17.
To allow time to recover from ECT’s acute cognitive side effects, this assessment was conducted 24-48 hours after treatment. HAMD-17 scores range from 0 to 52, with higher scores indicating more severe depression. The intra-class correlation coefficient (ICC) of reliability was 0.95 between the raters. Side effects following ECT, including memory impairment, headache, and nausea, either observed by the psychiatrist at each visit or reported spontaneously by the patient were recorded.
Early improvement was defined as a reduction in HAMD-17 score of at least 20%, 25%, or 30% and was assessed after 3 and 6 ECT sessions. Because most of the patients with severe depression would show some response to ECT, response was defined as a reduction of 60% or more in the total HAMD-17 score (Heijnen et al., 2010; Mulder et al., 2003; Sackeim et al., 2000) rather than a reduction of 50% or more (i.e., the traditional criteria). Remission was defined as an endpoint HAMD-17 score of ≤ 7. Treatment “completers” were those who had showed a therapeutic response or those who completed the maximum of 12 ECT sessions.
2.4. Statistical analyses
To decrease the bias from drop-out data, analysis was on a modified intent-to-treat basis for subjects who received at least 6 sessions of ECT and had at least 2 post-baseline assessments.
end of the ECT course were compared in terms of demographic and clinical variables, including gender, medications before ECT, treatment-resistant depression
(Dombrovski et al., 2005; Rasmussen et al., 2007), age, age at onset, duration of current episode (Dombrovski et al., 2005; Haq et al., 2015; Medda et al., 2014), duration of illness (Altamura et al., 2015), number of previous episodes, baseline CGI-S score, baseline HAMD-17 score, side effects, and percentages of improvement in HAMD-17 after 3 and 6 ECT sessions. Medications before ECT were classified as add-on therapy (i.e., an antidepressant augmenting with lithium, methylphenidate, or atypical antipsychotics or combing with a second antidepressant) and monotherapy (i.e. only an antidepressant). Treatment-resistant depression was defined as a lack of response to 2 or more antidepressant treatment with adequate doses and duration (Souery et al., 1999). Age at onset was regarded as age at the first major depressive episode. Duration of illness was defined as the time after the onset to the first major depressive episode (Breitborde et al., 2009) to the day of ECT.
Second, if percentage of improvement in HAMD-17 after 3 and 6 ECT sessions were significant predictors of response/remission, they were entered into a receiver operating characteristic (ROC) curve. The ROC curve was used to identify the number of ECT sessions (e.g., 3 or 6 ECT sessions) that best predicted final response or remission. The area under the ROC curve (AUC) was used to quantify the ability or
accuracy of the test in identifying responders from non-responders, or remitters from non-remitters. In practice, AUC≥0.8 indicates a good discriminative capacity (Hosmer and Lemeshow, 1999; Weinstein, 1980). Since this study sought to obtain practical cutoffs with good discriminative capacity, we focused on AUC≥0.8.
Sensitivity (true positive rate = the proportion of final responders or remitters who were correctly classified as early improvers), specificity (true negative rate = the proportion of final non-responders or non-remitters who were correctly classified as early non-improvers), false positive rate (100%-specificity), false negative rate (100%-sensitivity), positive predictive value (PPV = the proportion of early improvers who finally responded or remitted), and negative predictive value (NPV = the
proportion of early non-improvers who finally did not respond or remit) was calculated for the different definitions of early improvement.
All data were processed by SPSS version 17.0 for Windows (SPSS Inc., Chicago, IL, USA) and MedCalc (MedCalc Software, Belgium). Pearson Chi-square test or Fisher’s exact test was used to compare categorical variables; independent t-test was for continuous variables. All tests were two-tailed, and significance was defined as an alpha of less than 0.05.
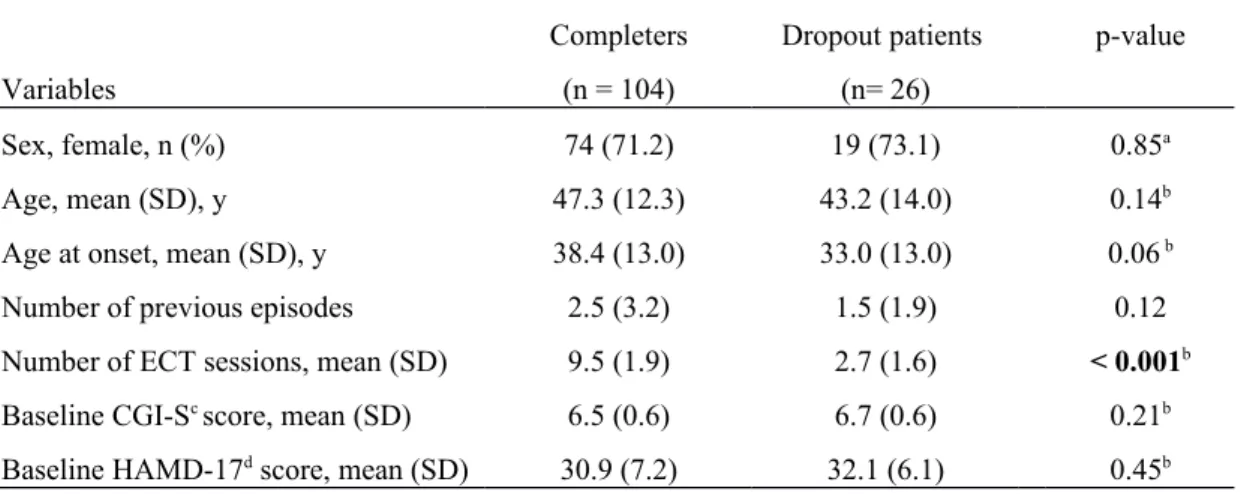
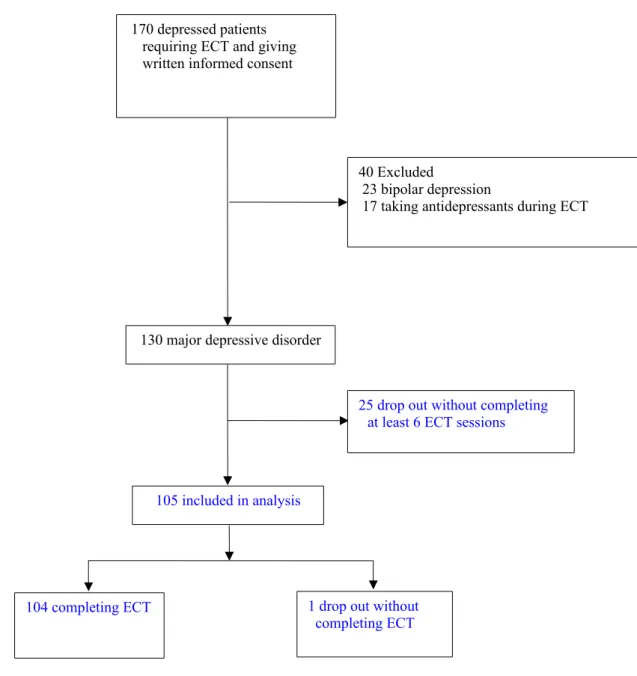
3.1. Patients
The participant selection process is shown in Figure 1. A total of 130 acutely ill inpatients with major depressive disorder (MDD) were enrolled. A total of 130 acutely ill inpatients with major depressive disorder (MDD) were enrolled. Twenty-five of the 130 patients who did not receive at least 6 sessions of ECT were excluded. The remaining 105 patients receiving at least 6 sessions of ECT were included in analysis. One of the 105 discontinued ECT prematurely; the remainder (n = 104) completed the course of ECT. The completers (n = 104) and the dropout patients (n = 26 [25 + 1]) were comparable for sex, age, age at onset, number of previous episodes, baseline CGI-S scores, and baseline HAMD-17 scores (Table 1). Reasons for
dropping out during the acute phase of ECT included adverse events (n = 13),
premature discharge or withdrawal of consent (n = 11), protocol violation (n = 1), and upper respiratory tract infection (n = 1). The most common adverse events were complaints of pain (n = 6), confusion or memory problems (n = 2), hypoxia after ECT (n = 3), and high frequency of ventricular premature contraction lasting for long duration observed after ECT (n = 2).
3.2. Response/Remission
Of the 105 patients who entered the analysis, 85.7% (n = 90) and 70.5% (n = 74) of the subjects were classified as responders and remitters at the end of the ECT course,
respectively. Responders and non-responders did not differ in sex, medications before ECT, treatment-resistant depression, age, age at onset, duration of current episode, duration of illness, number of previous episodes, number of ECT session, baseline CGI-S scores, baseline HAMD-17 scores, headache, and nausea/vomiting. However, non-responders experienced greater rate of memory impairment than responders during the trial period (p = 0.04). There were no significant differences in sex,
medications before ECT, treatment-resistant depression, age, age at onset, duration of current episode, duration of illness, number of previous episodes, baseline CGI-S scores, baseline HAMD-17 scores, and side effects between the remitters and non-remitters except non-non-remitters received more number of ECT sessions than non-remitters (p = 0.03). Percentages of improvement in HAMD-17 after 3 and 6 ECT sessions were significant predictors of final response and remission (Table 3).
3.3. Area under the ROC curves (AUC)
Percentages of improvement in HAMD-17 after 3 and 6 ECT sessions were entered into ROC curves to determine the number of ECT sessions that could best predict final response and remission. AUCs after 6 ECT sessions (AUCs ≥ 0.8) had good discriminative capacities, and were larger than those after 3 ECT sessions (AUCs < 0.8), regardless of final response or remission as outcome measures (Table 4). Given these results, all subsequent analyses were based on early improvement after 6 ECT
sessions.
3.4. Predictive value of early improvement
The sensitivity, specificity, false positive, false negative, positive and negative predictive values of early improvements across 3 different cutoff points (i.e., the 20%, 25%, and 30% improvements) after 6 ECT sessions, predicting final response and remission, are shown in Table 5.
Early improvement was a very sensitive (but not very specific) predictor of final response and remission. A high percentage of patients without early improvement finally became non-responders and non-remitters (i.e., high NPV values). However, a number of patients who had shown early improvement did not become final
responders or remitters, reflecting limited specificity.
4. Discussion
Our first major finding is that high rates of final response (85.7%) and remission (70.5%) were observed for patients with severe depression treated with bilateral ECT. Whether or not the treatment-resistant depression predicts poor ECT outcome remains no consistent findings (Rasmussen et al., 2007). The response rates (i.e., at least a 50% reduction in symptoms reduction) reported from Western countries for patients receiving ECT as a first line treatment andfor patients with treatment-resistant depression are 80-90% and 50-60%, respectively (Kennedy et al., 2009; Petrides et
al., 2001; Prudic et al., 1996). If we redefined response as a 50% HAMD-17 score reduction rather than 60%, our new response rate is 91.4% (= 96/105). It was higher than those from Western countries. The possible reasons may come from bilateral ECT use and from different race/ethnicity. For example, our response rate was comparable to those (85.7-94.4%) of two Chinese studies for patients with treatment-resistant depression receiving bilateral ECT (Tang et al., 2012). Unfortunately, ECT usage in Asian countries is much lower than in Western countries, data for
comparison are limited (Swartz, 2009).
Responders had shorter observed value of duration of current episode (15.1 20.5 vs. 19.3 19.9) and observed value of duration of illness (8.0 7.0 vs. 12.0 8.3) than non-responders. Similarly, remitters had shorter observed value of duration of current episode (15.021.4 vs. 17.518.1) and observed value of duration of illness (8.06.6 vs. 9.88.6) than non-remitters (Table 3). Two time-related variables (i.e., duration of current episode and duration of illness) cannot predict response or
remission significantly. According to statistical theory, using continuous variables as outcome measure is more precise than using dichotomized outcomes (e.g.,
response/non-response or remission/non-remission) (Ragland, 1992; Streiner, 2002; Taylor et al., 2006). If outcome was defined as HAMD-17 score change after ECT, HAMD-17 score change (-24.2 8.7) was related to duration of current episode (r
=0.215, p=0.028) and duration of illness (r = 0.193, p=0.048) analyzed by Pearson’s correlation. It means that the longer the duration of current episode or duration of illness, the less the symptomatic improvement after ECT. Therefore, the potential variables affecting ECT outcomes require further exploration in future studies.
As early as 3 ECT sessions, responders or remitters had significantly greater percentage of symptom improvement than non-responders or non-remitters (see Table 3). However, we did not further analyze their predictive values due to inadequate discriminative capacities (i.e., AUCs<0.8) (see Table 4). The second finding is that early improvement after 6 ECT sessions predicted final response or remission with high sensitivity and high NPV. High NPV means that the absence of early
improvement after 6 sessions with ECT is unlikely to lead to final response or remission. This finding was consistent with reports by Segman et al. (Segman et al., 1995) and by the Consortium for Research in ECT (Husain et al., 2004), which stated that early improvement after 6 ECT sessions would predict final remission. A study by Daly et al. (Daly et al., 2001) also found that an average of 6 ECT sessions is needed to reach initial response. Actually, the 6th session of ECT has commonly been regarded as the usual session for treatment evaluation in ECT textbooks (APA, 2001; Kellner, 2012; Mankad, 2010; Waite and Easton, 2013).
multiple medications or other interventions, but is generally regarded as the treatment of last resort. High sensitivity of early improvement in predicting final response or remission denoted that false-negative rates were low. These low false negative rates could prevent premature discontinuation of ECT for patients who would finally achieve response/remission.
We found that 20.0-26.7% of non-responders and 12.9-16.1% of non-remitters (i.e., low specificity shown in Table 5) at the end point were correctly identified as early improvers after 6 ECT sessions. We also found that 60.0-75.0% of early non-improvers after 6 ECT sessions were also non-responders at the end point, and that 80.0-100.0% of early non-improvers after 6 ECT sessions were non-remitters at the end of ECT course (i.e., high NPV in Table 5). Early improvement with high sensitivity was not necessarily associated with a favorable final response/remission, which means that early improvement was not specific for final response/remission. High negative predictive values indicate that those patients who did not show
improvement after 6 ECT sessions had a minimal chance of achieving final response and remission. Choosing 20%, 25%, or 30% cutoff points for the definition of early improvement after 6 ECT sessions produced comparable results (Table 5). A higher cutoff level (e.g., 30%) tended to decrease sensitivity and increase specificity.
utilization of early improvement to predict final response or remission from
pharmacotherapy and psychotherapy to ECT. Therefore, the presence or absence of early improvement could help psychiatrists decide earlier whether ECT techniques should be adjusted. Second, a maximum number of 12 ECT sessions was generally necessary to avoid undertreatment. In clinical practice, most patients require 6 to 12 treatments (APA, 2001, 2010; Kellner, 2012). A patient who has had poor response after 12 treatments is unlikely to have a favorable response to ECT later (Waite and Easton, 2013). Additionally, the advantages of administering concomitant
antidepressants during the ECT are still controversial (Baghai et al., 2006; Lauritzen et al., 1996; Mayur et al., 2000). Antidepressants were discontinued during the ECT course in the present study to decrease possible confounding of the ECT’s efficacy.
However, our findings should be interpreted with caution due to certain
limitations. First, this was an uncontrolled, open-label study. Second, the sample size was relatively low. The present results should be replicated in independent studies with larger sample sizes. Third, all participants were treated with bilateral ECT. Whether the present findings can be extrapolated to those treated with right unilateral ECT requires additional study. Fourth, according to the study protocol, symptom severity was assessed every 3 ECT sessions. If symptom severity was assessed every 1 or 2 ECT sessions, early improvement by the 4th or 5th ECT sessions might have
been observed. Finally, whether response to ECT differs between bipolar depression and unipolar depression is still inconclusive (Dierckx et al., 2012). Whether our results can be generalized to bipolar depression remains uncertain.
In conclusion, efficacy, tolerability, and acceptability are vital for patients receiving ECT. The clinical value of this study is that early non-improvement after 6 ECT sessions is unlikely to lead to final response or remission if ECT is continued, and its technique remains unchanged (APA, 2001).
References
Abrams, R., Swartz, C.M., 2002. ECT Instruction Manual for the Thymatron TM System IV. 7th ed. Lake Bluff, Illinois, USA: Somatics Ins.
Altamura, A.C., Serati, M., Buoli, M., 2015. Is duration of illness really influencing outcome in major psychoses? Nordic journal of psychiatry 69, 403-417.
Antunes, P.B., Rosa, M.A., Belmonte-de-Abreu, P.S., Lobato, M.I., Fleck, M.P., 2009. [Electroconvulsive therapy in major depression: current aspects]. Rev Bras Psiquiatr 31 Suppl 1, S26-33.
DSM-IV. American Psychiatric Press, Washington, DC.
APA, 2000. Diagnostic and statistical manual of mental disorders : DSM-IV-TR, 4th ed., text revision. ed. American Psychiatric Association, Washington, DC.
APA, 2001. The practice of electroconvulsive therapy : recommendations for
treatment, training, and privileging : a task force report of the American Psychiatric Association, 2nd ed. ed. American Psychiatric Association, Washington, D.C.
APA, 2010. Practice guideline for the treatment of patients with major depressive disorder (Third Edition). American Psychiatric Association. Am. J. Psychiatry, 1-152. Baghai, T.C., Marcuse, A., Brosch, M., Schule, C., Eser, D., Nothdurfter, C., Steng, Y., Noack, I., Pietschmann, K., Moller, H.J., Rupprecht, R., 2006. The influence of concomitant antidepressant medication on safety, tolerability and clinical effectiveness of electroconvulsive therapy. World J. Biol. Psychiatry 7, 82-90.
Birkenhager, T.K., Pluijms, E.M., Lucius, S.A., 2003. ECT response in delusional versus non-delusional depressed inpatients. J. Affect. Disord. 74, 191-195.
Breitborde, N.J., Srihari, V.H., Woods, S.W., 2009. Review of the operational definition for first-episode psychosis. Early intervention in psychiatry 3, 259-265.
Brunoni, A.R., Baeken, C., Machado-Vieira, R., Gattaz, W.F., Vanderhasselt, M.A., 2014. BDNF blood levels after electroconvulsive therapy in patients with mood disorders: a systematic review and meta-analysis. World J. Biol. Psychiatry 15, 411-418.
Coffey, C.E., Lucke, J., Weiner, R.D., Krystal, A.D., Aque, M., 1995. Seizure threshold in electroconvulsive therapy: I. Initial seizure threshold. Biol. Psychiatry 37, 713-720. Correll, C.U., Zhao, J., Carson, W., Marcus, R., McQuade, R., Forbes, R.A., Mankoski, R., 2013. Early antipsychotic response to aripiprazole in adolescents with
schizophrenia: predictive value for clinical outcomes. J. Am. Acad. Child Adolesc. Psychiatry 52, 689-698 e683.
Daly, J.J., Prudic, J., Devanand, D.P., Nobler, M.S., Lisanby, S.H., Peyser, S., Roose, S.P., Sackeim, H.A., 2001. ECT in bipolar and unipolar depression: differences in speed of response. Bipolar disorders 3, 95-104.
Dierckx, B., Heijnen, W.T., van den Broek, W.W., Birkenhager, T.K., 2012. Efficacy of electroconvulsive therapy in bipolar versus unipolar major depression: a meta-analysis. Bipolar disorders 14, 146-150.
Dombrovski, A.Y., Mulsant, B.H., Haskett, R.F., Prudic, J., Begley, A.E., Sackeim, H.A., 2005. Predictors of remission after electroconvulsive therapy in unipolar major depression. J. Clin. Psychiatry 66, 1043-1049.
Fink, M., Rush, A.J., Knapp, R., Rasmussen, K., Mueller, M., Rummans, T.A., O'Connor, K., Husain, M., Biggs, M., Bailine, S., Kellner, C.H., Consortium for Research in,
a CORE publication. J. ECT 23, 139-146.
Group, U.E.R., 2003. Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet 361, 799-808.
Guy, W., 1976. ECDEU Assessment manual for psychopharmacology. DHEW Publication 76338, Washington DC.
Hamilton, M., 1960. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56-62.
Haq, A.U., Sitzmann, A.F., Goldman, M.L., Maixner, D.F., Mickey, B.J., 2015. Response of depression to electroconvulsive therapy: a meta-analysis of clinical predictors. J. Clin. Psychiatry 76, 1374-1384.
Heijnen, W.T., Birkenhager, T.K., Wierdsma, A.I., van den Broek, W.W., 2010. Antidepressant pharmacotherapy failure and response to subsequent
electroconvulsive therapy: a meta-analysis. J. Clin. Psychopharmacol. 30, 616-619. Henkel, V., Seemuller, F., Obermeier, M., Adli, M., Bauer, M., Mundt, C., Brieger, P., Laux, G., Bender, W., Heuser, I., Zeiler, J., Gaebel, W., Mayr, A., Moller, H.J., Riedel, M., 2009. Does early improvement triggered by antidepressants predict
response/remission? Analysis of data from a naturalistic study on a large sample of inpatients with major depression. J. Affect. Disord. 115, 439-449.
Hosmer, D.W., Lemeshow, S., 1999. Applied logistic regression, 2nd ed. John Wiley & Sons, New York.
Husain, M.M., Rush, A.J., Fink, M., Knapp, R., Petrides, G., Rummans, T., Biggs, M.M., O'Connor, K., Rasmussen, K., Litle, M., Zhao, W., Bernstein, H.J., Smith, G., Mueller, M., McClintock, S.M., Bailine, S.H., Kellner, C.H., 2004. Speed of response and
remission in major depressive disorder with acute electroconvulsive therapy (ECT): a Consortium for Research in ECT (CORE) report. J. Clin. Psychiatry 65, 485-491.
Kellner, C.H., 2012. Brain stimulation in psychiatry : ECT, DBS, TMS, and other modalities. Cambridge University Press, Cambridge.
Kemp, D.E., Ganocy, S.J., Brecher, M., Carlson, B.X., Edwards, S., Eudicone, J.M., Evoniuk, G., Jansen, W., Leon, A.C., Minkwitz, M., Pikalov, A., Stassen, H.H., Szegedi, A., Tohen, M., Van Willigenburg, A.P., Calabrese, J.R., 2011a. Clinical value of early partial symptomatic improvement in the prediction of response and remission during short-term treatment trials in 3369 subjects with bipolar I or II depression. J. Affect. Disord. 130, 171-179.
Kemp, D.E., Johnson, E., Wang, W.V., Tohen, M., Calabrese, J.R., 2011b. Clinical utility of early improvement to predict response or remission in acute mania: focus on olanzapine and risperidone. J. Clin. Psychiatry 72, 1236-1241.
Kennedy, S.H., Milev, R., Giacobbe, P., Ramasubbu, R., Lam, R.W., Parikh, S.V., Patten, S.B., Ravindran, A.V., Canadian Network for, M., Anxiety, T., 2009. Canadian Network
for Mood and Anxiety Treatments (CANMAT) Clinical guidelines for the management of major depressive disorder in adults. IV. Neurostimulation therapies. J. Affect. Disord. 117 Suppl 1, S44-53.
Kho, K.H., van Vreeswijk, M.F., Simpson, S., Zwinderman, A.H., 2003. A meta-analysis of electroconvulsive therapy efficacy in depression. J. ECT 19, 139-147.
Lauritzen, L., Odgaard, K., Clemmesen, L., Lunde, M., Ohrstrom, J., Black, C., Bech, P., 1996. Relapse prevention by means of paroxetine in ECT-treated patients with major depression: a comparison with imipramine and placebo in medium-term
continuation therapy. Acta Psychiatr. Scand. 94, 241-251.
Leucht, S., Shamsi, S.A., Busch, R., Kissling, W., Kane, J.M., 2008. Predicting antipsychotic drug response - replication and extension to six weeks in an international olanzapine study. Schizophr. Res. 101, 312-319.
Lin, C.H., Chen, M.C., Lee, W.K., Chen, C.C., Huang, C.H., Lane, H.Y., 2013.
Electroconvulsive therapy improves clinical manifestation with plasma BDNF levels unchanged in treatment-resistant depression patients. Neuropsychobiology 68, 110-115.
Machado-Vieira, R., Luckenbaugh, D.A., Soeiro-de-Souza, M.G., Marca, G., Henter, I.D., Busnello, J.V., Gattaz, W.F., Zarate, C.A., Jr., 2013. Early improvement with lithium in classic mania and its association with later response. J. Affect. Disord. 144, 160-164.
Mankad, M.V., 2010. Clinical manual of electroconvulsive therapy, 1st ed. American Psychiatric Pub., Washington, DC.
Mayur, P.M., Gangadhar, B.N., Subbakrishna, D.K., Janakiramaiah, N., 2000. Discontinuation of antidepressant drugs during electroconvulsive therapy: a controlled study. J. Affect. Disord. 58, 37-41.
Medda, P., Mauri, M., Toni, C., Mariani, M.G., Rizzato, S., Miniati, M., De Simone, L., Perugi, G., 2014. Predictors of remission in 208 drug-resistant depressive patients treated with electroconvulsive therapy. J. ECT 30, 292-297.
Mulder, R.T., Joyce, P.R., Frampton, C., 2003. Relationships among measures of treatment outcome in depressed patients. J. Affect. Disord. 76, 127-135. O'Connor, M.K., Knapp, R., Husain, M., Rummans, T.A., Petrides, G., Smith, G., Mueller, M., Snyder, K., Bernstein, H., Rush, A.J., Fink, M., Kellner, C., 2001. The influence of age on the response of major depression to electroconvulsive therapy: a C.O.R.E. Report. Am. J. Geriatr. Psychiatry 9, 382-390.
O'Gorman, C., Kapur, S., Kolluri, S., Kane, J., 2011. Early improvement on
antipsychotic treatment as a predictor of subsequent response in schizophrenia: analyses from ziprasidone clinical studies. Hum Psychopharmacol 26, 282-290. Pagnin, D., de Queiroz, V., Pini, S., Cassano, G.B., 2004. Efficacy of ECT in depression:
a meta-analytic review. J. ECT 20, 13-20.
Petrides, G., Fink, M., 1996. The "half-age" stimulation strategy for ECT dosing. Convuls. Ther. 12, 138-146.
Petrides, G., Fink, M., Husain, M.M., Knapp, R.G., Rush, A.J., Mueller, M., Rummans, T.A., O'Connor, K.M., Rasmussen, K.G., Jr., Bernstein, H.J., Biggs, M., Bailine, S.H., Kellner, C.H., 2001. ECT remission rates in psychotic versus nonpsychotic depressed patients: a report from CORE. J. ECT 17, 244-253.
Post, R.M., Uhde, T.W., Rubinow, D.R., Huggins, T., 1987. Differential time course of antidepressant effects after sleep deprivation, ECT, and carbamazepine: clinical and theoretical implications. Psychiatry Res. 22, 11-19.
Prudic, J., Haskett, R.F., Mulsant, B., Malone, K.M., Pettinati, H.M., Stephens, S., Greenberg, R., Rifas, S.L., Sackeim, H.A., 1996. Resistance to antidepressant
medications and short-term clinical response to ECT. Am. J. Psychiatry 153, 985-992. Ragland, D.R., 1992. Dichotomizing continuous outcome variables: dependence of the magnitude of association and statistical power on the cutpoint. Epidemiology 3, 434-440.
Rasmussen, K.G., Mueller, M., Knapp, R.G., Husain, M.M., Rummans, T.A., Sampson, S.M., O'Connor, M.K., Petrides, G., Fink, M., Kellner, C.H., 2007. Antidepressant medication treatment failure does not predict lower remission with ECT for major depressive disorder: a report from the consortium for research in electroconvulsive therapy. J. Clin. Psychiatry 68, 1701-1706.
Rich, C.L., Spiker, D.G., Jewell, S.W., Neil, J.F., Black, N.A., 1984. The efficiency of ECT: I. Response rate in depressive episodes. Psychiatry Res. 11, 167-176.
Rodger, C.R., Scott, A.I., Whalley, L.J., 1994. Is there a delay in the onset of the antidepressant effect of electroconvulsive therapy? Br. J. Psychiatry 164, 106-109. Sackeim, H., Decina, P., Prohovnik, I., Malitz, S., 1987. Seizure threshold in
electroconvulsive therapy. Effects of sex, age, electrode placement, and number of treatments. Arch. Gen. Psychiatry 44, 355-360.
Sackeim, H.A., Prudic, J., Devanand, D.P., Nobler, M.S., Lisanby, S.H., Peyser, S., Fitzsimons, L., Moody, B.J., Clark, J., 2000. A prospective, randomized, double-blind comparison of bilateral and right unilateral electroconvulsive therapy at different stimulus intensities. Arch. Gen. Psychiatry 57, 425-434.
Segman, R.H., Shapira, B., Gorfine, M., Lerer, B., 1995. Onset and time course of antidepressant action: psychopharmacological implications of a controlled trial of electroconvulsive therapy. Psychopharmacology (Berl.) 119, 440-448.
Sienaert, P., Vansteelandt, K., Demyttenaere, K., Peuskens, J., 2009. Ultra-brief pulse ECT in bipolar and unipolar depressive disorder: differences in speed of response. Bipolar disorders 11, 418-424.
Souery, D., Amsterdam, J., de Montigny, C., Lecrubier, Y., Montgomery, S., Lipp, O., Racagni, G., Zohar, J., Mendlewicz, J., 1999. Treatment resistant depression: methodological overview and operational criteria. Eur. Neuropsychopharmacol. 9, 83-91.
Streiner, D.L., 2002. Breaking up is hard to do: the heartbreak of dichotomizing continuous data. Can J Psychiatry 47, 262-266.
Swartz, C., 2009. Electroconvulsive and neuromodulation therapies. Cambridge University Press, Cambridge.
Szegedi, A., Jansen, W.T., van Willigenburg, A.P., van der Meulen, E., Stassen, H.H., Thase, M.E., 2009. Early improvement in the first 2 weeks as a predictor of treatment outcome in patients with major depressive disorder: a meta-analysis including 6562 patients. J. Clin. Psychiatry 70, 344-353.
Szegedi, A., Muller, M.J., Anghelescu, I., Klawe, C., Kohnen, R., Benkert, O., 2003. Early improvement under mirtazapine and paroxetine predicts later stable response and remission with high sensitivity in patients with major depression. J. Clin.
Psychiatry 64, 413-420.
Tang, Y.L., Jiang, W., Ren, Y.P., Ma, X., Cotes, R.O., McDonald, W.M., 2012.
Electroconvulsive therapy in China: clinical practice and research on efficacy. J. ECT 28, 206-212.
Taylor, A.B., West, G.G., Aiken, L.S., 2006. Loss of Power in Logistic, Ordinal Logistic, and Probit Regression When an Outcome Variable Is Coarsely Categorizedy. Educ Psychol Meas 66, 228-239.
Tsuchiyama, K., Nagayama, H., Yamada, K., Isogawa, K., Katsuragi, S., Kiyota, A., 2005. Predicting efficacy of electroconvulsive therapy in major depressive disorder.
Psychiatry Clin. Neurosci. 59, 546-550.
Vermeiden, M., Kamperman, A.M., Vulink, M.E., van den Broek, W.W., Birkenhager, T.K., 2015. Early improvement as a predictor of eventual antidepressant treatment response in severely depressed inpatients. Psychopharmacology (Berl.) 232, 1347-1356.
Waite, J.e., Easton, A.e., 2013. The ECT handbook, Third edition / edited by Jonathan Waite & Andrew Easton. ed.
Table 1. Clinical characteristics between dropout patients and completers Variables Completers (n = 104) Dropout patients (n= 26) p-value Sex, female, n (%) 74 (71.2) 19 (73.1) 0.85a Age, mean (SD), y 47.3 (12.3) 43.2 (14.0) 0.14b
Age at onset, mean (SD), y 38.4 (13.0) 33.0 (13.0) 0.06 b
Number of previous episodes 2.5 (3.2) 1.5 (1.9) 0.12
Number of ECT sessions, mean (SD) 9.5 (1.9) 2.7 (1.6) < 0.001b
Baseline CGI-Sc score, mean (SD) 6.5 (0.6) 6.7 (0.6) 0.21b
Baseline HAMD-17d score, mean (SD) 30.9 (7.2) 32.1 (6.1) 0.45b
Bold, statistically significant
aPearson’s χ2 test bIndependent t test.
cCGI-S = Clinical Global Impression of Severity
Figure 1. Selection of participants for the analysis.
1 drop out without completing ECT
25 drop out without completing at least 6 ECT sessions 130 major depressive disorder
170 depressed patients requiring ECT and giving written informed consent
40Excluded
23 bipolar depression
17 taking antidepressants during ECT
105 included in analysis