2012/7/13
1
Effects of Implant-Abutment Connection
Design on Peri-Implant Bone Level
Purpose
To investigate the effects of external, internal, and
Mores taper implant-abutment connections on
peri-implant bone levels prior to and after loading of dental
implant,
by
conducting
a
clinical
analysis
and
comparison.
Materials & Methods
Digitized, standardized, and classified the periapical x-ray data were collected from China Medical University Hospital Dental Department during the period of 2002 to 2010. The software of Image J (NIH, Bethesda, MD, USA) were used to measure the bone loss (bone level change;difference of vertical bone defect; △VBD) prior to and after the loading of dental implants.
Implants used in this study:
Three types of implant systems were placed at the bone level..
1.External hex connection: Branemark (Brånemark System
TMMK IV TiUnite®, Nobel Biocare, Sweden)
2.Internal octagon connection: Cowellmedi (Sub. Atlas Cowellmedi Co., Busan, South Korea)
3.Morse taper connection: ANKYLOS (Ankylos®plus Implant,
Friadent, Mannheim, Germany)
Table 1. Average age at time of placement
Results
Conclusions
Ming‐I Lin; Heng‐Li Huang; Jui‐Ting Hsu; Yen‐Wen Shen; Lih‐Jyh
Fuh
School of Dentistry, China Medical University, Taichung, Taiwan.
91 Hsueh‐Shih Road, Taichung 40402, Taiwan, R.O.C.
Table 2. Time schedule of the study
T0–T1 : biological phase T1–T2 : Loading phase I T1–T3 : Loading phase II
The study protocol was reviewed and approved by the Institutional Review Board (IRB) of China Medical University Hospital (CMUH).CMUH IRB No.:DMR101-IRB-1-078.
a. Observe the bone loss of these three types of implant systems during the period of biological phase( 4 months after surgery T0-T1) .
b. Observe the bone loss of these three types of implant systems during the periods of loading phase I ( 3 months after loading T1-T2 ) and loading phase II ( 6 months after loading T1-T3 ).
MG :micro-gap
BICP :Bone to implant contact point
PBL :peri bone level VBD :the distance between
MG and BICP ΔVBD :bone loss(bone level
change)
Fig 1. Definition of reference point for measureing bone loss
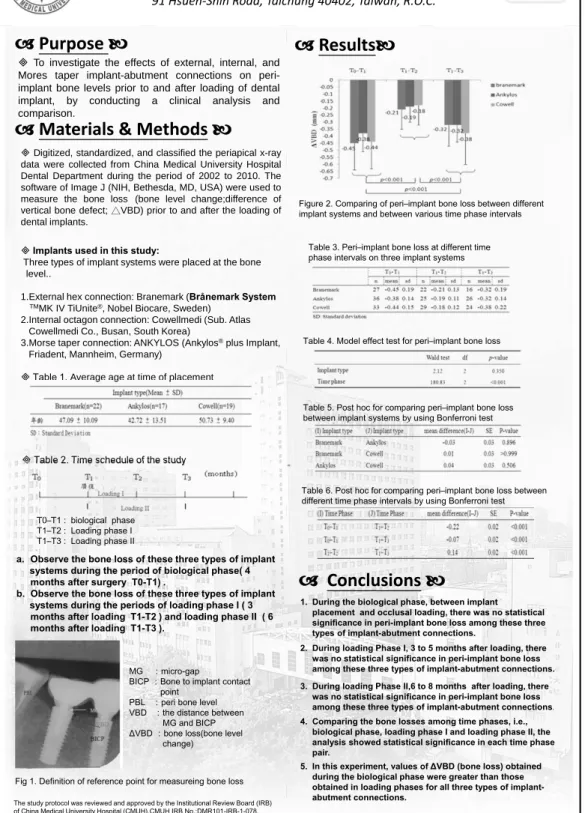
Figure 2. Comparing of peri–implant bone loss between different implant systems and between various time phase intervals
Table 3. Peri–implant bone loss at different time phase intervals on three implant systems
Table 4. Model effect test for peri–implant bone loss
Table 5. Post hoc for comparing peri–implant bone loss between implant systems by using Bonferroni test
Table 6. Post hoc for comparing peri–implant bone loss between different time phase intervals by using Bonferroni test
1. During the biological phase, between implant placement and occlusal loading, there was no statistical significance in peri-implant bone loss among these three types of implant-abutment connections.
2. During loading Phase I, 3 to 5 months after loading, there was no statistical significance in peri-implant bone loss among these three types of implant-abutment connections. 3. During loading Phase II,6 to 8 months after loading, there
was no statistical significance in peri-implant bone loss
among these three types of implant-abutment connections.
4. Comparing the bone losses among time phases, i.e., biological phase, loading phase I and loading phase II, the analysis showed statistical significance in each time phase pair.
5. In this experiment, values of ΔVBD (bone loss) obtained during the biological phase were greater than those obtained in loading phases for all three types of implant-abutment connections.