行政院國家科學委員會專題研究計畫 成果報告
細胞趨化性激素在抵抗肺組織胞漿菌炎之保護效性
計畫類別: 個別型計畫 計畫編號: NSC93-2320-B-002-076- 執行期間: 93 年 08 月 01 日至 94 年 07 月 31 日 執行單位: 國立臺灣大學醫學院免疫學研究所 計畫主持人: 伍安怡 報告類型: 精簡報告 處理方式: 本計畫可公開查詢中 華 民 國 94 年 10 月 31 日
中文摘要
在宿主防禦及黏膜免疫反應中 T 細胞扮演重要角色。在呼吸道感染中,T 細胞被活化並在肺臟周圍淋巴結增生,分化的 T 細胞由淋巴結移至肺臟以執行 功能。本實驗室的研究發現,組織胞漿菌肺部感染之小鼠引發第一型 T 細胞反 應,並在感染之肺部形成有細胞浸潤的肉芽腫。研究曾指出 IP-10 蛋白質表現 在肺結核病人的呼吸道。因 IP-10 及其他干擾素 γ 可誘導之細胞趨化素 Mig 和 I-TAC 對於吸引活化 T 細胞,尤其是 Th-1 細胞,扮演重要角色,我們假設在 活化的 Th-1 細胞上表現之 CXCR3 在肺部感染模式中指導分化的 T 細胞由 肺臟周圍淋巴結遷移至肺臟。 我們利用組織胞漿菌肺部感染模式來研究與 Th-1 相關之細胞趨化素的表 現情形。同時利用 CXCR3-/- 小鼠來研究活化的 Th-1 細胞及其他免疫細胞由淋 巴結至器官的遷移。我們的研究發現,肺部感染組織胞漿菌後病菌的清除並未受 到 CXCR3 缺乏而有明顯影響。然而在 CXCR3 缺乏小鼠中,在肺臟周圍淋巴 結中的 NK 細胞數目明顯減少,顯示肺部感染時 NK 細胞由周圍淋巴結遷移至 肺臟是與 CXCR3 有關的。在全身性感染中,去除 CXCR3 配體 IP-10 及 CCR5 配體 RANTES 的小鼠分別在感染第 7 天及第 14 天有較高的病菌負荷 量。這些研究結果顯示,IP-10 參與和 NK 細胞相關之早期組織胞漿菌炎,而 RANTES 對於感染晚期與活化 T 細胞遷移吸引相關之病菌清除有貢獻。Abstract
In respiratiory infections, activated T cells are recruited into the lungs where they exert effector functions. The T cells are activated and expand in the lung-associated lymph nodes following a respiratory infection. The differentiated T cells migrate from the lymph nodes to the lung. Our study showed that mouse with pulmonary histoplasmosis mount a type 1 T cell response, and granuloma was formed in infected lungs with infiltrating cells. The expression of IP-10 protein is reported in the airway of tuberculosis patients. Since IP-10 and other IFN-γ inducible chemokines, Mig and I-TAC are important in the recruitment of activated T cells, especially Th-1 cells, we hypothesize that CXCR3 expression on activated Th1 cells in the pulmonary infection model directs the migration of differentiated T cell from lung-associated lymph nodes to the lung.
Using pulmonary histoplasmosis animal model, we studied the kinetics of the expression of Th1-associated chemokines in the infection. In addition, CXCR3 -/-mice were used to study trafficking of activated Th1 T cells as well as other immune cells from lymph node to their target organ. We found that fungal clearance in pulmonary histoplasmosis is not significantly affected by CXCR3 deficiency. However, in CXCR3-deficient mice, the number of NK cells is reduced in the draining lymph node of lungs, indicating that NK cell migration to the lymph node in pulmonary infection is CXCR3-dependent. In systemic infection, depletion of CXCR3 ligand IP-10 and CCR5 ligand RANTES in wild type mice increased the fungal burdens at day 7 and day 14, respectively, after infection. The results indicate that IP-10 is involved in the early phase of histoplasmosis when NK cells are involved in host defense while RANTES contributes to the later phase of infection when activated T cells are recruited for fungal clearance.
Introduction
Chemokines are small proteins that mediate the recruitment and activation of leucocytes and other cells during immune response. The characteristic of chemokines is redundancy and binding promiscuity between many ligands and receptors. A single chemokine may bind to several receptors, whereas a single chemokine receptor may transduce signals for several chemokines. A number of chemokine receptors have been shown to be associated with the Th1 and Th2 phenotypes (1). CCR5 and CXCR3 are associated with Th1 phenotype, while CCR3, CCR4, CCR8 are associated with the Th2 phenotype.
IP-10 (CXCL10, IFNγ-induced protein of 10KDa), Mig (CXCL9, monokine induced by IFNγ) and I-TAC (CXCL11, IFN-induced T-cell α-chemoattractant) specifically chemoattract activated T cells and NK cells (2-5). These three chemokines share a common receptor, CXCR3 (4). CXCR3 is expressed on peripheral blood T cells activated in vitro and on a significant fraction of circulating CD4+ and CD8+ T cells. B cells, and NK cells (6). In aerosol Mycobacterium tuberculosis infection, it has been shown that polymorphonuclear neutrophils (PMN) are essential for accurate early granuloma formation (7). The PMN-mediated regulation of granuloma formation depended on chemokine signaling through CXCR3, in particular MIG, since mice with CXCR3 deficiency or Mig neutralization showed impaired early granuloma formation. In addition, it is reported that IFNγ, but not TNFα or IL-1β, strongly induced IP-10, Mig and I-TAC expression in normal human bronchial epithelial cells (NHBEC) (8). It was also reported that IP-10 mRNA was expressed in the bronchial epithelium of tuberculosis patients. These results indicate that IP-10, Mig and I-TAC may play an important role in the recruitment of activated T cells into the lungs where the T cells exert effector function.
Histoplasma capsulatum is a dimorphic fungus. Natural infection results from inhalation of the microconidia. The conidia transform in the lungs and become yeast cells which are taken up and reside primarily within the macrophages. The infected macrophage is not able to clear the residing Histoplasma yeast cells until it is been activated by IFNγ. The activated macrophages can produce anti-microbe molecules such as nitric oxide to inhibit the replication of intracellular yeasts and clear them. Therefore, IFNγ, which is mainly produced by activated CD4 T cells, plays a crucial role in host defense in host defense against histoplasmosis.
Our preliminary study showed that pulmonary histoplasmosis mounted a type 1 T cell response (Fig. 1). Since IP-10 and other IFNγ-inducible chemokines, Mig and I-TAC are important in the recruitment of activated T cells, especially Th1 cells, we therefore asked whether CXCR3 expression on activated Th1 cells in the pulmonary
Histoplasmosis infection model directs the migration of differentiated T cell from lung-associated lymph nodes to the lung. We used CXCR3-deficient mice with the pulmonary histoplasmosis animal model to study how lacking CXCR3 will impact on the trafficking of activated Th1 T cells from lymph node to their target organ.
Results
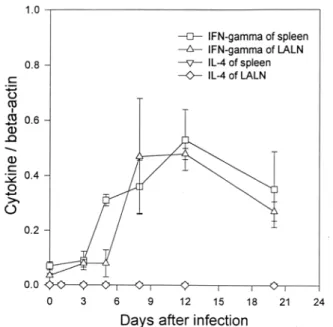
1. Type-1 immune response is induced in pulmonary histoplasmosis. We first determined the cytokine profile in the pulmonary Histoplasma infection. Total RNA was extracted from lymph nodes and spleen of wild type mice intratracheally inoculated with Histoplasma yeast cells. The level of IFNγ and IL-4 mRNA expression is normalized against β-actin expression. Data in Fig. 1 show that IFNγ but not IL-4 was expressed after Histoplasma infection, indicating that type-1 cytokine is induced after Histoplasma infection.
Fig. 1. IFNγ and IL-4 expression in lung-associated lymph nodes and spleen of Histoplasma-infected mice.
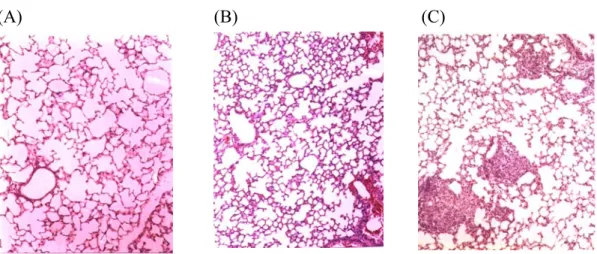
2. Intratracheal inoculation of Histoplasma induces granuloma formation. Next we examined the lung tissues of infected mice. The animals were inoculated intratracheally with Histoplasma yeast cells. Lung tissues were collected at day 12 of infection. Hematoxylin staining in Fig. 2 shows granuloma in infected lungs with infiltrating cells.
(A) (B) (C)
Fig. 2. Granuloma formation in lungs after Histoplasma infection. Lung tissue was collected from normal mouse (A), mouse inoculated intratracheally with heat-killed Histoplasma yeast cells (B) and live yeast cells (C). The tissues were stained with hematoxylin.
3. Fungal clearance in pulmonary infection is not significantly affected by CXCR3 deficiency. Wild type and CXCR3 knockout mice were infected with Histoplasma intratracheally. The fungal counts in the lung tissues were enumerated at different time points. The fungal counts gradually increased after infection in both the wild type and CXCR3-deficient mice (Fig. 3). There was no statistically significant difference between wild type and knockout mice. Interestingly, the maximum fungal loads at day 7 were lower in the CXCR3-deficient mice than in the wild type mice. These data indicate that the ability to clear Histoplasma is not impaired in the CXCR3 knockout mice.
2.5 3.5 4.5 5.5 6.5 Lo g 10 C F U /g l u ng 0 2 4 6 8 10 12 14 16 Days after infection
WT CXCR3 KO
**
**
Fig. 3. The fungal loads at different time points after intratracheal Histoplasma infection. Lungs were harvested at 3, 5, 7, 11 and 15 days after infection and the fungal loads were determined. More than 8 mice were used at each time point (*p<0.05, **p<0.01).
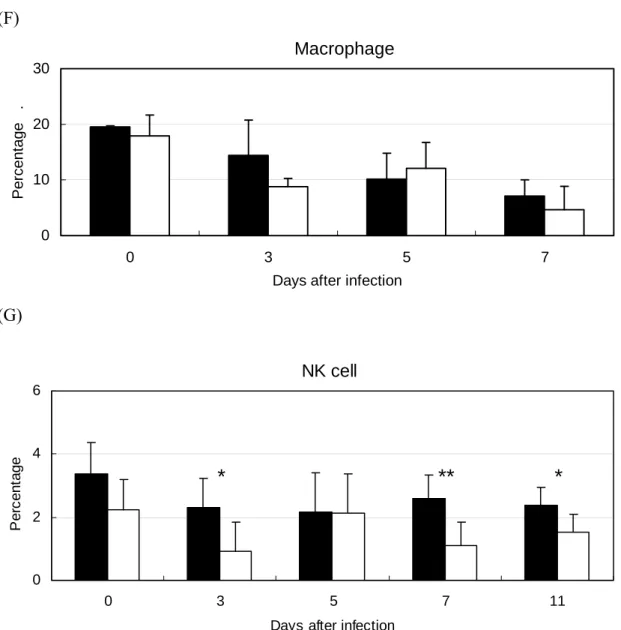
4. NK cells but not lymphocytes in the draining lymph node of Histoplasma-infected CXCR3-deficient mice are reduced. We next examined the cellular composition in the lymph nodes that drain the lungs. Results in Fig. 4 show that the percentage of T cells, B cells, macrophages and dendritic cells in the CXCR3-deficient mice were not significantly different from that in the wild type mice. However, the percentage of NK cells was lower in the CXCR3-deficient mice than that in wild type mice (*p<0.05, **p<0.01), which indicates that CXCR3 is important to NK cell migration to the draining lymph nodes.
T cell
0 50 100
0 3 5 7 11
Days after infection
P er c ent ag e . WT KO (A) (B) CD4 T cell 0 20 40 60 0 3 5 7 11
Days after infection
P
er
c
ent
(C) CD8 T cell 0 10 20 30 0 3 5 7 11
Days after infection
P er c ent age . (D) B cell 0 20 40 60 0 3 5 7 11
Days after infection
P er c ent age . (E) Dendritic cell 0 0.5 1 1.5 0 3 5 7 11
Days after infection
P e rc ent ag e .
Macrophage 0 10 20 30 0 3 5 7
Days after infection
P er c ent age . (F) (G) NK cell 0 2 4 6 0 3 5 7 11
Days after infection
P
er
c
ent
age
*
**
*
Fig. 4. Cell composition of the mediastinal lymph node at different time points after infection. The mediastibal lymph nodes, where the T cells drain to the lungs, were collected at different time points. Lymph nodes were grinded and cells were stained with (A) anti-CD3 (T cells), (B) anti-CD4, (C) anti-CD8, (D) anti-B220 (B cells), (E) anti-CD11c (dendritic cells), (F) anti-Mac1 (macrophages), and (G) anti-panNK (NK cells) antibodies. Cells were acquired and analyzed by flow cytometry. The close symbol represents the wild type mice and the open symbol represents the CXCR3 knockout mice (*p<0.05, **p<0.01).
Histoplasma infection. Although the ability to clear Histoplasma yeast cells from the lungs was not significantly impaired in CXCR3-deficient mice, we examined the effect of chemokines in systemic histoplasmosis. We used neutralizing antibodies against chemokine IP-10 and RANTES RANTES is the ligand of another type-1 immune response-associated chemokine receptor CCR5. Wild type mice were intravenously infected with Histoplasma. The animals were treated with anti-IP-10 or anti-RANTES antibody every other day starting day 0. The spleens were harvested at different time point after infection and the fungal counts were enumerated. Data in Fig. 5 show that depletion of IP-10 and RANTES increased susceptibility to histoplasmosis. Mice with anti-IP-10 treatment had higher fungal loads than those with untreated control and those with anti-RANTES treatment at day 7 (*p<0.05 and **p<0.01, respectively). However, the fungal load in mice treated with anti-IP-10 was comparable to that in the untreated group, indicating that IP-10 plays a role in early host defense against the pathogen. On the other hand, depleting RANTES increased the fungal counts at day 7. Although the fungal counts declined by day 14, mice with anti-RANTES treatment still had higher Histoplasma counts than the untreated mice.. These results indicate that IP-10 and RANTES both play an important role in host defense against systemic Histoplasma infection. IP-10 is involved in the early stage of infection, whereas RANTES contributed to later time of infection.
3 4 5 6
3 7 14
Days after infection
Lo g10 C F U /g s p le e n untreated anti-RANTES anti-IP-10 ** ** * ** *p<0.05, **p<0.01
Fig. 5. Comparing mice with or without neutralizing antibody treatment for their susceptibility to Histoplasma infection. Spleens were harvested at 3, 7, and 14 days after intravenous infection and the fungal loads were determined. Four mice were used at each treatment and each time point (*p<0.05, **p<0.01).
Reference
1. O'Garra, A., L.M. McEvoy, and A. Zlotnik. 1998. T-cell subsets: chemokine receptors guide the way. Curr Biol 8:R646-649.
2. Farber, J.M. 1997. Mig and IP-10: CXC chemokines that target lymphocytes. J Leukoc Biol 61:246-257.
3. Liao, F., R.L. Rabin, J.R. Yannelli, L.G. Koniaris, P. Vanguri, and J.M. Farber. 1995. Human Mig chemokine: biochemical and functional characterization. J Exp Med 182:1301-1314.
4. Loetscher, M., B. Gerber, P. Loetscher, S.A. Jones, L. Piali, I. Clark-Lewis, M. Baggiolini, and B. Moser. 1996. Chemokine receptor specific for IP10 and mig: structure, function, and expression in activated T-lymphocytes. J Exp Med 184:963-969.
5. Taub, D.D., A.R. Lloyd, K. Conlon, J.M. Wang, J.R. Ortaldo, A. Harada, K. Matsushima, D.J. Kelvin, and J.J. Oppenheim. 1993. Recombinant human interferon-inducible protein 10 is a chemoattractant for human monocytes and T lymphocytes and promotes T cell adhesion to endothelial cells. J Exp Med 177:1809-1814.
6. Qin, S., J.B. Rottman, P. Myers, N. Kassam, M. Weinblatt, M. Loetscher, A.E. Koch, B. Moser, and C.R. Mackay. 1998. The chemokine receptors CXCR3 and CCR5 mark subsets of T cells associated with certain inflammatory reactions. J Clin Invest 101:746-754.
7. Seiler, P., P. Aichele, S. Bandermann, A.E. Hauser, B. Lu, N.P. Gerard, C. Gerard, S. Ehlers, H.J. Mollenkopf, and S.H. Kaufmann. 2003. Early granuloma formation after aerosol Mycobacterium tuberculosis infection is regulated by neutrophils via CXCR3-signaling chemokines. Eur J Immunol 33:2676-2686.
8. Sauty, A., M. Dziejman, R.A. Taha, A.S. Iarossi, K. Neote, E.A. Garcia-Zepeda, Q. Hamid, and A.D. Luster. 1999. The T cell-specific CXC chemokines IP-10, Mig, and I-TAC are expressed by activated human bronchial epithelial cells. J Immunol 162:3549-3558.