C A S E R E P O R T
Open Access
A penetrating atherosclerotic ulcer rupture
in the ascending aorta with
hemopericardium: a case report
Yuan-Hao Liu
1, Hung-Yen Ke
2, Yi-Chang Lin
2,4*and Chien-Sung Tsai
2,3Abstract
Background: Acute aortic syndrome, including classic aortic dissection, intramural aortic hematoma, and penetrating atherosclerotic ulcer (PAU), is a term used to describe a group of conditions with similar clinical symptoms, but with different pathophysiological mechanisms. PAU is a lesion that penetrates the internal elastic lamina through the media. It is usually located in the descending aorta and rarely observed in the ascending aorta. Case presentation: A 76-year-old man with a history of essential hypertension was brought to the emergency department (ED) because of a sudden-onset chest pain at rest. He had not been taking his medication as ordered. His vital signs in the ED were a blood pressure of 82/60 mmHg, heart rate of 158 beats per min, respiratory rate of 22 breaths per min, and a body temperature of 37.2 °C. An electrocardiogram did not show an ST segment elevation, and cardiac enzymes were within normal limits. No widening mediastinum was found on chest radiography, but a large pericardial effusion with an impending cardiac tamponade was revealed on
echocardiography. The diagnosis of PAU rupture in the ascending aorta with hemopericardium was made with chest computed tomography. An emergent sternotomy and ascending aorta reconstruction were performed. A ruptured ulcerative plaque through the intima to the adventitia without flap dissection in the ascending aorta was confirmed. The patient was discharged 18 days after the operation.
Conclusions: Although PAU in the ascending aorta is uncommon, it is commonly lethal when it ruptures. With the current advances in endovascular techniques and devices, endovascular repair of PAU in the ascending aorta is currently recommended only for high-risk patients unsuitable for open repair. However, we anticipate that endovascular repair may become feasible in patients with PAU in the ascending aorta in the future.
Keywords: Acute aortic syndrome, Penetrating atherosclerotic ulcer, Ascending aorta, Endovascular repair, Case report
Background
Acute aortic syndrome (AAS), including classic aortic dissection, intramural aortic hematoma, and penetrating atherosclerotic ulcer (PAU), is a term used to describe a group of conditions with similar clinical symptoms, but with different pathophysiological mechanisms. PAU was first described by Shennan et al. [1] in 1934, but was first
shown to be a separate clinical and pathological entity by Stanson et al. [2] in 1986. It is an ulcerating athero-sclerotic lesion that disrupts the internal elastic lamina and is associated with hematoma formation within the aortic wall. In the initial stage, atheromatous ulcers de-velop in patients with advanced atherosclerosis; lesions are usually asymptomatic and confined to the intimal layer. In the second stage, the lesion progresses to a deep atheromatous ulcer that penetrates through the elastic lamina into the media. Hematoma formation may extend along the media, resulting in either a “double-barreled” or “thrombosed” aortic dissection. In some cases, hematoma extension causes stretching of the weakened aortic wall, leading to the formation of a saccular aortic
* Correspondence:m860630@mail.ndmctsgh.edu.tw
2Division of Cardiovascular Surgery, Department of Surgery, Tri-Service
General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China
4Department of Biological Science and Technology, National Chiao Tung
University, Hsinchu, Taiwan, Republic of China
Full list of author information is available at the end of the article
© 2016 The Author(s). Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Liu et al. Journal of Cardiothoracic Surgery (2016) 11:103 DOI 10.1186/s13019-016-0502-3
aneurysm [3]. Generally, patients become PAU symp-tomatic in the second stage, with the main symptom being severe, acute chest pain that radiates to the inter-scapular area; this is initially difficult to differentiate from a classic acute aortic dissection or intramural aor-tic hematoma. A chest spiral computed tomography (CT) scan provides a short examination time and high quality two- and three-dimensional image reconstruction to help us identify the type of AAS. Occasionally, some patients exhibit several or all of these lesions, indicative of the existence of a link between them. In such cases, it is difficult to know which was the initiating event [4].
Here we present a rare case of AAS in which echocar-diography revealed hemopericardium and cardiac tam-ponade without obvious false lumen in the ascending aorta. Chest CT showed a ruptured PAU in the ascend-ing aorta. An emergent sternotomy and ascendascend-ing aorta reconstruction were immediately performed. The clinical presentation and management is discussed below. Case presentation
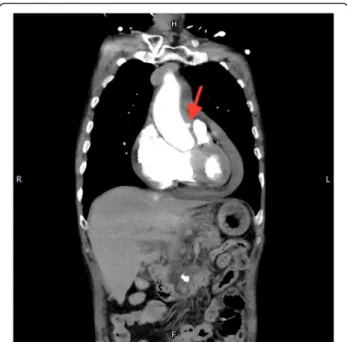
A 76-year-old man with a history of essential hyperten-sion, who had not been taking his medications before this admission, presented to the emergency department (ED) because of a sudden chest pain at rest. His vital signs in the ED were a blood pressure of 82/60 mmHg, heart rate of 158 beats per min, respiratory rate of 22 breaths per min, and a body temperature of 37.2 °C. Electrocardio-gram did not show an ST segment elevation, and cardiac enzymes were within normal limits. No widening medias-tinum was found on chest radiography, but echocardiog-raphy revealed a large pericardial effusion with impending cardiac tamponade. Ruptured PAU of the ascending aorta with hemopericardium was diagnosed with chest CT scan (Figs. 1 and 2). A ruptured ulcer plaque through the in-tima to the adventitia without flap dissection in the as-cending aorta was confirmed. An emergent sternotomy and ascending aorta reconstruction were performed. The postoperative recovery was uneventful, and the patient was discharged 18 days after the operation.
Discussion
PAU tends to occur in elderly men with hypertension, tobacco use, and coronary artery disease [5]. This lesion may precipitate intramural hemorrhage, aortic aneurysm, pseudoaneurysm, or even aortic dissection. PAU usually involves the descending aorta, and although rare in the ascending aorta, it is commonly lethal [6] when it ruptures. Coady et al. [6] demonstrated that the rate of aortic rupture is markedly higher for intramural hematoma (35 %) and PAU (42 %) than for aortic dissection (type A 7.5 %, type B 4.1 %). PAU is frequently asymptomatic and is almost al-ways incidentally diagnosed. The initial clinical appearance of PAU is similar to that of a classic aortic dissection.
Differentiating PAU from the other AAS entities as well as acute pulmonary embolism and acute myocardial infarction is important. We can differentiate between all of these dis-eases in the ED based on patient history, physical examin-ation, electrocardiography, cardiac biomarkers, D-dimers, transthoracic echocardiography, transesophageal echocardi-ography, chest radiechocardi-ography, CT scan, and magnetic reson-ance imaging. As CT scan provides a quick and high quality two- and three-dimensional image reconstruction, it
Fig. 1 A protruding spot (PAU) in the ascending aorta, coronal view (red arrow)
Fig. 2 A protruding spot (PAU) in the ascending aorta, axial view (red arrow)
is the best method for diagnosing PAU, which appears as a focal, contrast-filled outpouching with jagged margins that extends beyond the expected aortic wall boundaries, usually associated with severe underlying atheromatous disease [5]. Although PAU has a high risk of aortic rupture, some authors believe that immediate surgical treatment is not always required because the disease may have a benign course. In the study by Harris et al. [7], few patients devel-oped aortic dissection or aortic rupture during follow-up. Besides, these authors emphasized that compared with the risk of acute aortic rupture, most patients with PAU were at a higher risk from surgical intervention because of their advanced age and poor general health. Moreover, surgical repair of the descending thoracic aorta is frequently associ-ated with complications such as respiratory disease, renal insufficiency, or spinal ischemia. Based on these reasons, patients with PAU involving the descending aorta can ini-tially be treated conservatively with aggressive medical ther-apy and close observation, similar to a descending aortic dissection [8]. Surgery becomes necessary when there are signs of expansion of intramural hematoma (IMH), rupture into the pericardial or pleural cavity, intractable chest pain, and hemodynamic instability. Besides, patients with a PAU must be followed up, particularly during the first month after the onset of AAS [2]. However, for patients with PAU in the ascending aorta, even asymptomatic patients, surgi-cal intervention is recommended as soon as possible be-cause they are at a high risk of evolving into a classic type A aortic dissection, type A IMH, or acute ascending aorta rupture with cardiac tamponade. Owing to improvement of endovascular techniques and advancement of devices, thor-acic endovascular aortic repair (TEVAR) has become the first-line approach for aortic diseases because of its high technical success rate (96.4 %–98.3 %) and low morbidity and mortality rates [9, 10]. TEVAR has been proved to yield excellent short-term and mid-term results in PAU of the descending aorta and has been the first line of management when intervention is indicated. However, TEVAR of PAU in the ascending aorta is rare as PAU is usually found in-cidentally in asymptomatic patients and is complicated with aortic dissection, IMH, or acute aortic rupture in AAS patients. A conventional open repair is still the first consideration in most of these cases. Endovascular therapy of the ascending aorta is frequently used as a “rescue tool” outside of its intended indication. How-ever, several studies have confirmed the safety and feasibility of endovascular repair of the ascending aorta for high-risk patients unsuitable for open repair [11, 12]. Most recently, Khoynezhad et al. [13] designed an FDA-approved physician-sponsored investigational device ex-emption study to investigate the outcome of endovascular repair of the ascending aorta. They demonstrated positive remodeling of the excluded aortic segments similar to sur-veillance studies involving the descending aorta. Although
only six patients were enrolled in the study and only one of them was indicated due to an ascending PAU, we anticipate that endovascular repair may be feasible in patients with PAU in the ascending aorta in the future. Conclusion
PAU is frequently asymptomatic and is diagnosed rather incidentally. While a PAU in the ascending aorta is un-common, it is commonly lethal when it ruptures. Gener-ally, PAU in the descending aorta is conservatively treated with aggressive medical therapy and close observation similar to a descending aortic dissection. We recommend treating PAU in the ascending aorta with an aggressive surgical intervention. A traditional operative procedure involves a sternotomy and ascending aorta reconstruction. However, with the advances in endovascular techniques and devices, endovascular repair of PAU in the descending aorta has been the first line of management when inter-vention is indicated. Although endovascular repair of PAU in the ascending aorta is employed for high-risk patients who are currently unsuitable for open repair, we anticipate that endovascular repair may be feasible in patients with PAU in the ascending aorta in the future.
Abbreviations
AAS, acute aortic syndrome; CXR, chest roentgenogram; ED, emergent department; IMH, intramural hematoma; PAU, penetrating atherosclerotic ulcer; TEVAR, thoracic endovascular aortic repair
Acknowledgements No
Funding No
Availability of data and materials I wish to share my data.
Authors’ contributions
1st author: YHL: 2nd author: HYK: 3rd author: YCL: 4th author: CST. All authors read and approved the final manuscript.
Competing interests No
Consent for publication Not applicable.
Ethics approval and consent to participate Not applicable.
Author details
1Division of Cardiovascular Surgery, Department of Surgery, Kaohsiung
Armed Forces General Hospital, Kaohsiung, Taiwan, Republic of China.
2Division of Cardiovascular Surgery, Department of Surgery, Tri-Service
General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China.3Division of Cardiovascular Surgery, Department of Surgery,
Taoyuan Armed Forces General Hospital, Taoyuan, Taiwan, Republic of China.
4Department of Biological Science and Technology, National Chiao Tung
University, Hsinchu, Taiwan, Republic of China.
Received: 18 April 2016 Accepted: 5 July 2016
References
1. Coady MA et al. Penetrating ulcer of the thoracic aorta: What is it? How do we recognize it? How do we manage it? J Vasc Surg. 1998;27:1006–16. 2. Stanson AW, Kazmier FJ, Hollier LH, et al. Penetrating atherosclerotic ulcers
of the thoracic aorta: natural history and clinicopathologic correlations. Ann Vasc Surg. 1986;1:15–23.
3. Hayashi H, Matsuoka Y, Sakamoto I, et al. Penetrating atherosclerotic ulcer of the aorta: imaging features and disease concept. RadioGraphics. 2000;20: 995–1005.
4. Vilacosta I, Roman JA. Acute aortic syndrome. Heart. 2001;85:365–8. 5. Romero J, Shah A, Korniyenko A. A blind spot in the eye of imaging
technology: penetrating atheromatous ulcer. Hellenic J Cardiol. 2013;54: 322–5.
6. Coady MA, Rizzo JA, Elefteriades JA. Pathologic variants of thoracic aortic dis- sections. Penetrating atherosclerotic ulcers and intramural hematomas. Cardiol Clin. 1999;17:637–57.
7. Harris JA, Bis KG, Glover JL, et al. Penetrating atherosclerotic ulcers of the aorta. J Vasc Surg. 1994;19:90–9.
8. Azeem S. Sheikh, Kamran Ali, Sajjad Mazhar, et al. Acute aortic syndrome. Circulation. 2013;128:1122–1127.
9. Ziza V, Canaud L, Molinari N, et al. Thoracic endovascular aortic repair: A single center’s 15-year experience. J Thorac Cardiovasc Surg. 2016;151(6):1595–603. 10. D’Annoville T, Ozdemir BA, Alric P, et al. Thoracic endovascular aortic repair
for penetrating aortic ulcer: literature review. Ann Thorac Surg. 2016;101(6): 2272–8.
11. Roselli EE, Idrees J, Greenberg RK, et al. Endovascular stent grafting for ascending aorta repair in high-risk patients. J Thorac Cardiovasc Surg. 2015; 149:144–54.
12. Tsilimparis N, Debus ES, Oderich GS, et al. International experience with endovascular therapy of the ascending aorta with a dedicated endograft.
J Vasc Surg. 2016;63(6):1476–82.
13. Khoynezhad A, Donayre CE, Walot I, et al. Feasibility of endovascular repair of ascending aortic pathologies as part of an FDA-approved physician-sponsored investigational device exemption. J Vasc Surg. 2016;63(6):1483–95.
• We accept pre-submission inquiries
• Our selector tool helps you to find the most relevant journal
• We provide round the clock customer support
• Convenient online submission
• Thorough peer review
• Inclusion in PubMed and all major indexing services
• Maximum visibility for your research Submit your manuscript at
www.biomedcentral.com/submit