(J Formos Med Assoc 2002;101:322–8) Key words: earthquake physical illness psychologic distress resource loss
Departments of Social Medicine, 1Nursing Science, 2Family Medicine, and 3Internal Medicine, College of Medicine and Hospital, National Taiwan University, Taipei.
Received: 20 August 2001. Revised: 31 October 2001. Accepted: 5 February 2002.
Reprint requests and correspondence to: Dr. Tai-Yuan Chiu, Department of Social Medicine, National Taiwan University College of Medicine, 7 Chung-Shan South Road, Taipei, Taiwan.
ORIGINAL ARTICLES
E
FFECTS
OF
A
M
AJOR
E
ARTHQUAKE
ON
THE
S
TATUS
OF
P
RE
-
EXISTING
P
HYSICAL
I
LLNESS
AND
L
EVELS
OF
P
SYCHOSOCIAL
D
ISTRESS
IN
C
OMMUNITY
I
NHABITANTS
Tai-Yuan Chiu, Wen-Yu Hu,1 Bee-Horng Lue, Ching-Yu Chen,2 and Bor-Shen Hsieh3
A major earthquake struck central Taiwan on Septem-ber 21, 1999, causing a tremendous amount of damage including 2,494 deaths and 618 severe injuries. Lu-Gu community is located near the epicenter of the
Background and Purpose: A major earthquake struck central Taiwan on September 21, 1999, causing a tremendous amount of damage in a very short time. This study surveyed the changes in the status of pre-existing physical illness and levels of psychosocial distress in a community after this earthquake.
Methods: One hundred and thirty inhabitants of Lu-Gu who were more than 40 years old were surveyed in June 2000, 9 months after the earthquake. A medical team in the disaster area carried out personal interviews using a self-report questionnaire. The questionnaire included demographic characteristics, common physical illnesses, and psychologic distress and resource loss measures.
Results: Subjects reported more rapidly declining visual acuity (11.5%) and worse upper respiratory (7.7%) and gastrointestinal tract symptoms (3.8%) after the earthquake. The mean value of the psychologic distress scores was significantly higher than before the earthquake (12.16 ± 3.28 vs 10.75 ± 2.63; p < 0.01). Women and the elderly had higher psychologic distress scores. Subjects had considerable loss in financial resources, including home contents, adequate food, and sentimental possessions, (3.57 ± 3.94, assessed using a resource loss measure on a 0–3 Likert scale with a possible range of 0–12). Women, the elderly, those who lived alone, and those with severe damage to their homes reported more loss than others in personal resources such as "feeling that my life is peaceful", "personal health", and "sense of optimism", but not in financial resources or interpersonal resources such as companionship, intimacy with at least one friend, and support from co-workers.
Conclusions: There was an increased level of psychologic distress and financial burden among community members 9 months after the earthquake. The findings of this study suggest the need to strengthen community-based health care systems in disaster-prone areas, so that they can provide continuous care, especially related to the psychosocial impacts of these events.
earthquake. Buildings, the traffic system, the environment, and the economy of this community were severely affected. In particular, a number of people faced physical and mental difficulties and loss of
resources. It is the responsibility of health care profes-sionals to deal with earthquake-related health prob-lems in disaster areas [1].
Previous studies reported that health problems that occurred after a severe disaster are usually complicated and most likely to have middle- and long-term conse-quences such as stress-related physical symptoms and psychologic effects [2, 3]. Other studies showed that a number of groups such as the elderly are particularly vulnerable to the long-term consequences of disaster [4, 5]. Five physicians, seven district nurses, and other health professionals were providing community health care in Lu-Gu at the time of the earthquake. Several weeks after the earthquake, most of the medical rescue teams left the disaster area. The community health care professionals had to take care of most of the health problems of the inhabitants. Knowledge of the effects of disaster on health status and its consequences in community inhabitants is important for these professionals. However, few studies in Taiwan have investigated disaster-related health problems.
The purposes of this study were to determine the changes in the status of pre-existing physical illness and to assess the levels of psychosocial distress in a commu-nity after the September 21, 1999, earthquake and to investigate the correlations of these findings with the demographic characteristics of subjects.
S
ubjects and Methods
Subjects
We used a purposive method to select four villages from the 13 villages in Lu-Gu. A personal interview with a self-report questionnaire was conducted with inhab-itants more than 40 years old who came to health centers for regular yearly health check-ups in June 2000, 9 months after the earthquake. Altogether, 130 people were recruited and completed the interview.
Procedure
The survey was conducted using a structured self-report questionnaire and the data were obtained by personal interview. Interviews were carried out by a medical team, which consisted of two physicians, one teacher from National Taiwan University College of Medicine and Hospital, one primary care physician, and two district nurses from the Lu-Gu government health station. All of the interviewers had received a thorough explanation and training about the purposes, instruments, and methodology of this study before the conduction of the survey. An inter-interviewer consis-tency of not less than 0.90 was determined and
in-formed consent was obtained from subjects before the interview. All data obtained in the interviews were reviewed for possible errors in discussion at a daily team meeting.
Instruments
A structured self-report questionnaire consisting of four parts was administered to all subjects. The four parts of the questionnaire included questions on de-mographic characteristics, common physical illnesses, a psychologic distress measure developed by Freedy et al and Ishikawa et al [6–8], and a resource loss measure developed from the resources model proposed by Hobfoll [7, 9]. The psychologic distress and resource loss measures were translated into Chinese and back-translated into English for language adaptation by the investigators. The entire four-part questionnaire was tested for content validity by a panel comprising two physicians, two nurses, and one psychologist, all of whom were experienced in the care of victims in this disaster. A pilot study employing 10 lay persons further confirmed the questionnaire’s content validity and ease of application.
Demographic characteristics assessed by the ques-tionnaire included gender, age, living arrangement, degree of housing damage (none, a little, or partial or complete destruction), and activities of daily life. Com-mon pre-existing physical illnesses at the time of the earthquake that were assessed included hypertension, diabetes mellitus, heart disease, arthritis, and respira-tory tract problems. The findings of this portion of the questionnaire were confirmed by review of previous health records. The self-perception of subjects on the change in status of these pre-existing illnesses (worse or better after the earthquake) was also elicited. Re-ported physical illnesses and symptoms were confirmed in discussions at the daily team meeting during the survey period.
The psychologic distress measure consisted of nine brief questions (difficulty sleeping, frightening thoughts, hopelessness, temper outbursts, palpitation, irritability, depressed affect, worrying, feeling critical toward others). This measure was used to evaluate psychologic distress on a 1 to 3 Likert scale (1 = none, 2 = minor distress, 3 = major distress) before and after the earthquake. Subjects recalled their psychologic condition before the earthquake. The reliability analy-sis of this Chinese version measurement showed a Cronbach’s alpha value of 0.83 for our sample.
The resource loss measure included 17 items. Par-ticipants were asked to rate the extent of loss for each resource since the earthquake on a 0 to 3 Likert scale (0 = no loss to 3 = major loss). An exploratory factor analysis was also used to analyze the Chinese version of the resource loss measurement for construct validity
and this process extracted three factors, which were personal resources ("feeling valuable to others", "fam-ily stability", free time, "feeling that I am accomplishing goals", "sense of optimism", "sense of humor", "feeling that I have control over my life", "feeling that my life is peaceful", "motivation to get things done", "personal health"), financial resources (home contents, senti-mental possessions, clothing, adequate food), and in-terpersonal resources (intimacy with at least one friend, support from co-workers, companionship). The Cronbach’s alpha values of these three factors were 0.82, 0.82, and 0.90, respectively. The alpha value for all 17 items was 0.83 for this study sample.
Statistical analysis
Data management and statistical analysis were performed using SPSS 8.0 statistical software (SPSS Inc, Chicago, IL, USA). A frequency distribution was used to describe the demographic data and the distri-bution of each variable. Mean values and standard deviations were used to analyze the severity of each variable in the psychologic distress and resource loss measures. Paired t-test was used to compare the severity of psychologic distress between the pre-earthquake and post-earthquake stages. Finally, one way ANOVA and Scheffe’s test were used to compare the difference between the severities of psychologic distress or re-source loss and the demographic characteristics of subjects by gender, age, living arrangement, and hous-ing damage. A p value of less than 0.05 was considered statistically significant.
R
esults
Demographic characteristics
A total of 130 subjects were included in the study, 72 men (55.4%) and 58 women (44.6%), with a mean age of 64.5 ± 9.9 years, and 63 (48.5%) aged 40 to 65 years and 67 aged more than 65 years. Most subjects lived with their families (93.1%). Nearly half (49.2%) of their houses had only a little damage. However, one-quarter (23.9%) of subjects could not stay in their houses, which were damaged beyond repair. Fortunately, only a tiny percentage (3.1%) had family members who suffered severe injures or died in the earthquake.
Self-reported changes in pre-existing physical
illness
Almost all subjects (99.2 %) had normal activities of daily life at the time of the interview. The pre-existing physical illnesses of the subjects before the earthquake
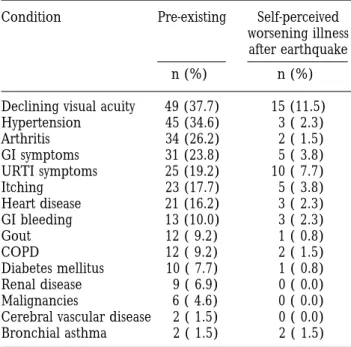
were similar to those reported in other rural communi-ties in Taiwan [10]. Table 1 shows that declining visual acuity and hypertension were the two most common health problems in subjects before the earthquake. However, declining visual acuity (11.5%), upper respi-ratory tract symptoms (7.7%), gastrointestinal tract symptoms (3.8%) and itching of the skin (3.8%) were perceived to have become worse after the earthquake in some people.
Change in psychologic distress
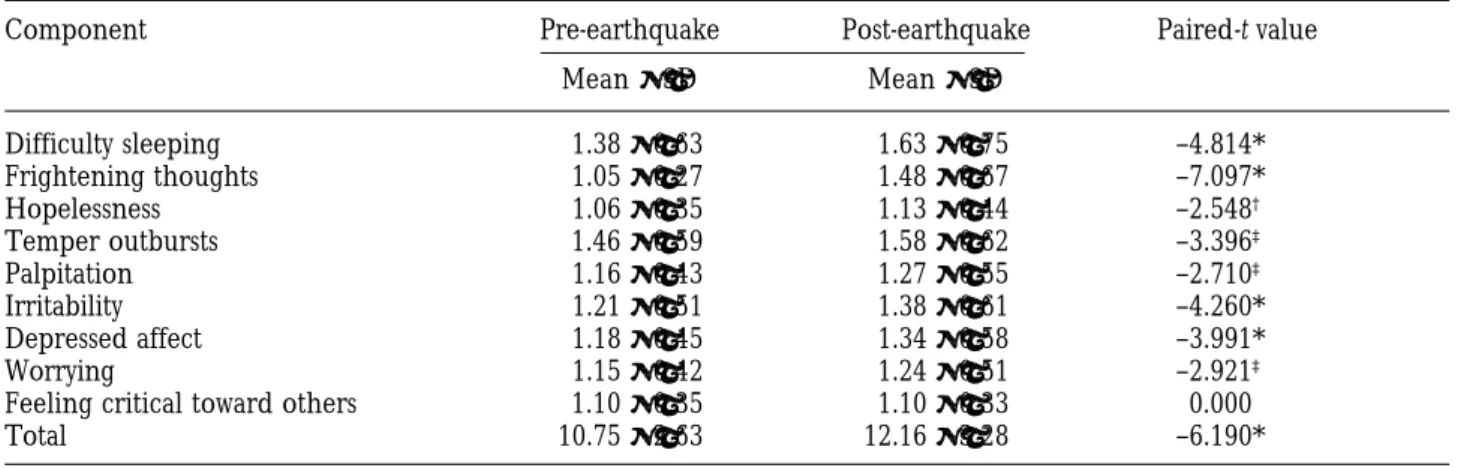
The mean score of the psychologic distress measure 9 months after the earthquake was significantly higher than that before the earthquake (12.16 ± 3.28 vs 10.75
± 2.63; p < 0.01). All components except feeling critical toward others had significantly higher mean scores after the earthquake than before (Table 2).
The items with higher psychologic distress scores at the time of interview were difficulty sleeping, temper outbursts, and frightening thoughts. Hopelessness, feeling critical, and worrying were experienced less frequently. Anxiety states in the inhabitants could be noted from these results.
Table 3 shows the relationships between subject characteristics and psychologic distress. Women and subjects older than 60 years had higher scores in psychologic distress, although this difference was not statistically significant. Although the psychologic dis-tress score was lower in subjects who lived with family
Table 1. Physical illness before the earthquake and self-perceived conditions after the earthquake (N = 130) Condition Pre-existing Self-perceived
worsening illness after earthquake
n (%) n (%)
Declining visual acuity 49 (37.7) 15 (11.5)
Hypertension 45 (34.6) 3 ( 2.3) Arthritis 34 (26.2) 2 ( 1.5) GI symptoms 31 (23.8) 5 ( 3.8) URTI symptoms 25 (19.2) 10 ( 7.7) Itching 23 (17.7) 5 ( 3.8) Heart disease 21 (16.2) 3 ( 2.3) GI bleeding 13 (10.0) 3 ( 2.3) Gout 12 ( 9.2) 1 ( 0.8) COPD 12 ( 9.2) 2 ( 1.5) Diabetes mellitus 10 ( 7.7) 1 ( 0.8) Renal disease 9 ( 6.9) 0 ( 0.0) Malignancies 6 ( 4.6) 0 ( 0.0)
Cerebral vascular disease 2 ( 1.5) 0 ( 0.0) Bronchial asthma 2 ( 1.5) 2 ( 1.5) GI = gastrointestinal tract; URTI = upper respiratory tract infection; COPD = chronic obstructive pulmonary disease.
Table 2. Psychologic distress scores before and 9 months after the earthquake (N = 130)
Component Pre-earthquake Post-earthquake Paired-t value
Mean ± SD Mean ± SD Difficulty sleeping 1.38± 0.63 1.63± 0.75 –4.814* Frightening thoughts 1.05± 0.27 1.48± 0.67 –7.097* Hopelessness 1.06± 0.35 1.13± 0.44 –2.548† Temper outbursts 1.46± 0.59 1.58± 0.62 –3.396‡ Palpitation 1.16± 0.43 1.27± 0.55 –2.710‡ Irritability 1.21± 0.51 1.38± 0.61 –4.260* Depressed affect 1.18± 0.45 1.34± 0.58 –3.991* Worrying 1.15± 0.42 1.24± 0.51 –2.921‡
Feeling critical toward others 1.10± 0.35 1.10± 0.33 0.000
Total 10.75± 2.63 12.16± 3.28 –6.190*
*p < 0.001; †p < 0.05; ‡p < 0.01; SD = standard deviation.
members before the earthquake (10.71 ± 2.50 vs. 11.38 ± 4.40), the change in psychologic distress of these sub-jects was still significant (12.14 ± 3.24 vs 10.71 ± 2.5; p < 0.01), which indicated a similar impact of the disaster on those who lived alone or with their family. The results also showed significant change in psychologic distress in those who had housing damage. Moreover, subjects who could not return to their homes because of complete housing destruction by the earthquake suffered more psychologic distress than those who could return without housing damage, although this difference was not statistically significant on Scheffe’s test (mean difference, 2.41; 95% confidence interval (95%CI), 5.72–0.89).
Table 3. Relationships between psychologic distress scores and subject characteristics (N = 130)
Characteristics Psychologic distress score
Pre-earthquake Post-earthquake Paired t-value
Mean ± SD (F) Mean ± SD (F) Gender Male (n = 72) 10.72 ± 3.03 (0.02) 11.76 ± 3.27 (2.39) –4.46* Female (n = 58) 10.79 ± 2.05 12.66 ± 3.26 –4.50* Age (yr) 40–60 (n = 37) 10.70 ± 2.34 (0.65) 11.89 ± 3.19 (0.26) –3.26† > 60 (n = 93) 10.68 ± 2.56 12.21 ± 3.24 –5.27* Living arrangement Alone (n = 8) 11.38 ± 4.40 (2.41) 12.12 ± 4.19 (0.37) –1.43 With family (n = 122) 10.71 ± 2.50 12.14 ± 3.24 –5.94* Housing damage None (n = 35) 10.74 ± 2.87 (0.42) 11.28 ± 2.99 (1.81) –1.33 Little (n = 64) 10.97 ± 2.61 12.47 ± 3.26 –5.75* Partial (n = 21) 10.28 ± 1.52 11.95 ± 2.84 –2.44‡ Complete (n = 10) 10.42 ± 3.75 13.70 ± 4.72 –2.70‡
SD = standard deviation. Comparisons of psychologic distress score pre- and post-earthquake: paired-t test. Gender, age, living arrangement, housing damage, and psychologic distress score: one way ANOVA and Scheffe’s test. *p < 0.001; †p < 0.05; ‡p < 0.01.
Resource loss
Table 4 shows the mean value of the 17 items in the resource loss measure. In terms of personal resources, the loss in the items of feeling that my life is peaceful, sense of optimism, and personal health was higher than others. Meanwhile, home contents in financial resources showed greater loss than other items. The loss of interpersonal resources, however, was not remarkable.
Comparing resource loss scores with demographic characteristics of subjects, we found that women, the elderly, those who lived alone, and those with severe housing damage reported higher loss of personal re-sources than other groups. However, only housing
Table 4. Scores of loss as measured by the 17-item resource loss measure 9 months after the earthquake (N = 130)
Items Mean ± SD Range
Personal resources 2.82 ± 5.47 0.00–30.00 Feeling valuable to others 0.02 ± 0.26
Family stability 0.24 ± 0.80
Free time 0.02 ± 0.45
Feeling that I am accomplishing 0.34 ± 0.94 goals
Sense of optimism 0.37 ± 0.97
Sense of humor 0.26 ± 0.83
Feeling that I have control over 0.27 ± 0.82 my life
Feeling that my life is peaceful 0.50 ± 1.09 Motivation to get things done 0.31 ± 0.91 Personal health 0.44 ± 1.04 Financial resources 3.57 ± 3.94 0.00–12.00 Home contents 1.53 ± 1.38 Sentimental possessions 0.68 ± 1.18 Clothing 0.58 ± 1.10 Adequate food 0.78 ± 1.25 Interpersonal resources 0.35 ± 1.50 0.00–9.00 Intimacy with at least one friend 0.12 ± 0.54
Support from co-workers 0.08 ± 0.48
Companionship 0.15 ± 0.62
Total 6.73 ± 7.62 0.00–51.00
SD = standard deviation.
damage showed a significant group difference on Scheffe’s test, namely, subjects who could not return to their homes because of housing destruction had higher scores of personal resource loss than those with no
damage (mean difference, 7.00; 95%CI, 12.23–1.77) or a little damage (mean difference, 6.11; 95%CI: 11.06–1.15). The results showed that housing damage was responsible for significant group differences in interpersonal resource loss on Scheffe’s test, which indicated that subjects who were unable to return to their homes due to partial housing damage had more social resource loss than those with no damage (mean difference, 1.19; 95%CI, 2.30–0.08) or only a little damage (mean difference, 1.33; 95%CI, 2.34–0.32) (Table 5).
D
iscussion
Although increased incidences and severities of some illnesses such as cardiovascular disease, cerebrovascu-lar disease, and gastrointestinal bleeding have been reported after a severe disaster [11–15], few subjects in this study complained of these problems. However, some subjects complained of more rapidly declining visual acuity and worsening upper respiratory and gastrointestinal tract symptoms. These illnesses may be related to the changes in life style and health activities caused by the earthquake [16]. Concerns and further investigation on these changes in life style and health activities related to physical fitness and immune func-tion after the earthquake would be worthwhile.
Posttraumatic stress disorder and psychologic dis-tress were emphasized in previous studies on disasters [17–19]. Although the extent of psychologic stress may
Table 5. Relationship between resource loss scores and subject characteristics (N = 130)
Characteristics Resource loss
Personal resources Financial resources Interpersonal resources
Mean ± SD (F) Mean ± SD (F) Mean ± SD (F)
Gender Male (n = 72) 2.43 ± 5.31 (0.80) 3.00 ± 3.37 (3.43) 0.43 ± 1.69 (0.51) Female (n = 58) 3.29 ± 5.68 4.28 ± 4.48 0.24 ± 1.26 Age (yr) 40–60 (n = 37) 2.27 ± 4.71 (0.43) 4.05 ± 4.05 (0.58) 0.22 ± 1.03 (0.43) > 60 (n = 93) 2.47 ± 5.70 3.47 ± 3.93 0.41 ± 1.68 Living arrangement Alone (n = 8) 4.50 ± 6.80 (0.58) 2.38 ± 2.67 (0.82) 0.00 ± 0.00 (0.26) With family (n = 122) 2.68 ± 5.40 3.68 ± 4.01 0.37 ± 1.55 Housing damage None (n = 35) 1.20 ± 2.84 (6.65)* 2.80 ± 4.87 (2.37) 0.14 ± 0.60 (6.13)† Little (n = 64) 2.09 ± 4.58 3.50 ± 3.67 0.00 ± 0.00 Partial (n = 21) 5.14 ± 7.32 3.66 ± 2.87 1.33 ± 2.87 Complete (n = 10) 8.20 ± 8.62 6.50 ± 2.88 0.20 ± 2.90
SD = standard deviation. Gender, age, living arrangement, housing damage, and resource loss scores: one way ANOVA and Scheffe’s test. *p < 0.001; †p < 0.01.
decline gradually with the passage of time, some vul-nerable groups such as the elderly or people with severe housing damage may need to be observed closely [20–23]. Even though this study was carried out 9 months after the earthquake, nearly all items in the psychologic stress measurement had significantly higher mean scores than before the earthquake. Although subjects in this study might represent healthier people in the community due to their ability to walk to health centers, they still suffered from high psychologic distress. Hence, extending care to other community residents is important.
Resource loss can be divided into the loss of internal and external resources [9]. Personal resources are inter-nal resources, which may indicate the potential for recon-struction after a disaster. Financial and interpersonal resources are external resources. The extent of loss of external resources may represent the extent of impact of the disaster. In this study, external resources showed recovery within a shorter time after the earthquake than internal resources. Among personal resources items, feel-ing my life is peaceful, sense of optimism, and personal health had greater loss compared to other items. This finding suggests that people developed feelings of insta-bility or inconsistency in their lives after this severe disaster. The results in this study showed little loss in the items of feeling valuable to others, family stability, and free time, which might suggest the presence of good family struc-ture or support in Taiwanese communities. From the viewpoint of personal resources, we found that the extent of loss was not predominant, which suggests that future reconstruction efforts may resolve these problems.
Lu-Gu is a rural community with a population density lower than that of large cities. Although this earthquake severely damaged this community, most people have still been able to live in their existing houses or start construc-tion on a new house in the same place. Family support and social interaction are still strong because the original community is intact. This may explain why the loss of social (interpersonal) resources was not remarkable in this study.
This study revealed that the earthquake caused health problems that continued months after the earthquake. There was an increased level of psycho-logic distress and financial burden 9 months after the earthquake. Community health care professionals, al-though they were also victims of the disaster, still had to lead or participate with multi-professional teams to provide continuous care for the community. In Taiwan, training programs in family and community medicine have been advocated for 20 years and are now available to most community physicians, nurses, and other health care professionals. Emphasis of a bio-psycho-social care model in training for family and community practice might improve the ability of health care professionals
to provide comprehensive care for post-disaster prob-lems in community inhabitants.
In order to provide more efficacious health care to the community in a post-disaster setting, the medical team from National Taiwan University Medical College established a community-based medical rescue and health care system in Lu-Gu.
Almost all the subjects had normal activities of daily life. The inclusion only of subjects who were able to walk from their houses to health centers for health check-ups probably created a selection bias toward healthier community members. Data on pre-disaster morbidity was mainly based on the subject’s memory, which is also a limitation of this study. Rescue and rehabilitation efforts in the disaster area were con-ducted aggressively within several months after the earthquake. It was, thus, difficult to perform a more comprehensive survey in that stage.
In conclusion, only a few physical illnesses were re-ported to have become worse compared to pre-earth-quake levels 9 months after the earthpre-earth-quake. However, significant psychologic distress had developed and still demanded continuous care. Although the loss of finan-cial resources was remarkable, personal resource items, including "feeling that my life is peaceful", "personal health", and "sense of optimism", showed good recovery. Otherwise, the elderly, women, those who lived alone, and those with severe housing damage reported higher levels of psychologic distress and loss of internal resources. Health problems that developed after the earthquake were psychosocial-related and may have long-term consequences. These findings suggest the need to strengthen community-based health care systems in disaster-prone areas so that they can provide regular health evaluation and continuous care, especially related to the psychosocial impacts of these events.
ACKNOWLEDGMENTS: The authors would like to thank Professor Susumu Wakai, Chairman of the Department of International Community Health at the Graduate School of International Health in the University of Tokyo, for his useful comments. We would also like to thank Professors SL Hwang, EC Wu, and MB Lee for their help during the survey, and also Ms CH Teng and YY Pan for their help with manuscript preparation. The authors also gratefully acknowledge the contributions of the resident participants in this study.
R
eferences
1. Huang GS, Yang YL, Chiu TY, et al: The concerns of community residents in the post-disaster reconstruction. Formos J Med 2002;6: (In Press).
2. Katakami Y: Earthquake-induced stress: relationships and trends noticed in health examination data from survivors of the great Hanshin-Awaji earthquake (Jan. 17, 1995). Rinsho Byori 1998;46:599–604.
3. Bland SH, O’Leary ES, Farinaro E, et al: Long-term psychological effects of natural disasters. Psychosom Med 1996;58:18–24.
4. Armenian HK, Melkonian AK, Hovanesian AP: Long term mortality and morbidity related to degree of dam-age following the 1998 earthquake in Armenia. Am J Epidemiol 1998;148:1077–84.
5. Shinfuku N: To be a victim and a survivor of the Great Hanshin-Awaji Earthquake. J Psychosom Res 1999;46:541–8. 6. Freedy JR, Saladin ME, Kilpatrick DG, et al: Understand-ing acute psychological distress followUnderstand-ing natural disaster. J Trauma Stress 1994;7:257–73.
7. Freedy JR, Shaw DL, Jarrell MP, et al: Toward an under-standing of the psychological impact of natural disasters: an application of the conservation resources stress model. J Trauma Stress 1992;5:441–54.
8. Ishikawa Y, Kawabata M, Muraki T: The effects of the Great Hanshin-Awaji Earthquake on the health status and the activities of daily living of the elderly and disabled. Proceedings of the International Symposium on Disaster and Health IPPAO, Manila, Philippines, 1997:241–50. 9. Hobfoll SE: Conservation of resources. A new attempt at
conceptualizing stress. Am Psychol 1989;44:513–24. 10. Chiu TY, Chen CY, Chen CI, et al: A study of community
care at Chinshan Group Practice Center. Chin J Fam Med 1991;1:36–44.
11. Kario K, Matsuo T, Kayaba K, et al: Earthquake-induced cardiovascular disease and related risk factors in focusing on the Great Hanshin-Awaji Earthquake. Am J Epidemiol 1998;8:131–9.
12. Katsouyanni K, Kogevinas M, Trichopoulos D:
Earth-quake-related stress and cardiac mortality. Int J Epidemiol 1986;15:326–30.
13. Suzuki S, Sakamoto S, Miki T, et al: Hanshin-Awaji earthquake and acute myocardial infarction. Lancet 1995;345:981.
14. Trevisan M, Jossa F, Farinaro E, et al: Earthquake and coronary heart disease risk factors: a longitudinal study. Am J Epidemiol 1992;135:632–7.
15. Leor J, Poole WK, Kloner RA: Sudden cardiac death trig-gered by an earthquake. N Engl J Med 1996;334:413–9. 16. Fukuda S, Morimoto K, Mure K, et al: Posttraumatic
stress and change in lifestyle among the Hanshin-Awaji earthquake victims. Prev Med 1999;29:147–51.
17. Liao SC, Lee YJ, Lin SK, et al: Acute stress syndromes in patients at an emergency medical station after a major earthquake. Taiwanese J Psychiatry 2000;14:31–40. 18. Liao SC, Lee MB, Lee YJ, et al: Psychological distress and
its association with psychosocial factors in rescue workers within two months of a major earthquake. J Formos Med Assoc 2002;101:169–76.
19. Sharan P, Chaudhary G, Kavathekar SA, et al: Prelimi-nary report of psychiatric disorders in survivors of a severe earthquake. Am J Psychiatry 1996;153:556–8. 20. Goenjian AK, Najarian LM, Pynoos RS, et al:
Posttrau-matic stress disorder in elderly and younger adults after the 1988 earthquake in Armenia. Am J Psychiatry 1994; 151:895–901.
21. Tanida N: What happened to elderly people in the great Hanshin earthquake. BMJ 1996;313:1133–5.
22. Kato H, Asukai N: Post-traumatic symptoms among younger and elderly evacuees in the early stages follow-ing the 1995 Hanshin-Awaji earthquake in Japan. Acta Psychiatr Scand 1996;93:477–81.
23. Nakamura H: Overview of the Hanshin-Awaji earthquake disaster. Acta Paediatr Jpn 1995;37:713–6.