通訊作者:龔佩珍
通訊地址:41354台中市霧峰區柳豐路500號 E-mail:ptkung@seed.net.tw
電話:04-23329255
Changes in Quality of Life at Five-year
Follow-up and Factors Associated with
Receiving a Thoracoscopic Sympathectomy
for Hyperhidrosis Patients
Chung-Yu Lai
1,Wen-Chen Tsai
2,Pei-Tseng Kung
3,
Ching-Yuan Cheng
4,Hsin-Yuan Fang
5Department of Surgery,Thoracic Surgery Division,Cheng-Ching General Hospital1
Department of Health Services Administration,China Medical University2
Department of Healthcare Administration,Asia University3
Department of Surgery,Thoracic Surgery Division,Changhua Christian Hospital4
Department of Surgery,Thoracic Surgery Division,China Medical University Hospital5
Abstract
Objective
Our aim was to explore long-term changes in the quality of life and the factors that influenced patients with upper limb hyperhidrosis to undergo thoracoscopic sympathectomy surgery to reduce sweating.
Methods
A cross-sectional study was conducted with a structured questionnaire in order to determine the perceived quality of life and decision about surgery. A total of 528 patients with hyperhidrosis were recruited from a medical center in Taiwan. The impact of hyperhidrosis on quality of life with or without undergoing thoracoscopic sympathectomy surgery was evaluated. The factors influencing the patient's decision to receive surgery were examined with multivariate logistic regression analysis.
Results
The impact of the symptom of hyperhidrosis on patients’ quality of life was 7.21 points (1-10 points) on average for patients who chose surgery and 4.89 points for patients who did not. The impact of hyperhidrosis on quality of life was reduced from 7.21 to 5.22 for post-operative patients 5 years after the surgery. Approximately 90% of these patients had symptoms of compensatory sweating after surgery and 72% of these had severe symptoms. Factors significantly influencing
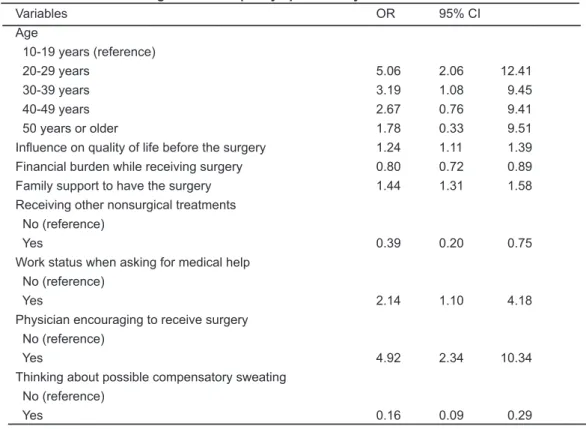
patients’ decisions to have a surgery included age (OR:1.78-5.06), the effect of pre-operative symptoms on the quality of life (OR:1.24; 95%CI:1.11-1.39), the financial burden of surgery (OR:0.80; 95%CI:0.72-0.89), family support (OR:1.44; 95%CI:1.31-1.58), effectiveness of nonsurgical treatments (OR:0.39; 95%CI:0.20-0.75), work status at the time of seeking medical help (OR:2.14; 95%CI:1.10-4.18), physician's opinion (OR:4.92; 95%CI:2.34-10.34), and concerns about postoperative compensatory sweating (OR:0.16; 95%CI:0.09-0.29).
Conclusions
Patients with hyperhidrosis who underwent surgical t herap y had improved quality of lif e, al t hough compensatory sweating could be severe and was a major concern. Physician attitude played an important role in patients’ decisions about surgical therapy.
Keywords
: hyperhidrosis, quality of life, thoracoscopic sympathectomy, compensatory sweatingsympathectomy.
Materials and Methods
Study subjects and data source
The present study was an observational and cross-sectional study, and was conducted on 872 patients with upper limb hyperhidrosis at a medical center in the central region of Taiwan between 2000 and 2006. All patients were mailed a letter and the questionnaire to ask for participating in this study. Patients were interviewed by telephone, and a structured questionnaire was used. This study was approved by the hospital's Ethics Committee (IRB No. HP070043), and the informed content for interview was obtained from the participative patients. A total of 528 patients were interviewed successfully, with a response rate of 60.6%. Among these subjects, 402 subjects (77%) were found to have received thoracoscopic T2 sympathectomy or sympathetic block. Average time after the surgery was 5.4 years when the subjects received this survey.
Questionnaire content and reliability and validity T h e q u e s t i o n n a i r e u s e d w a s b a s e d o n t h e questionnaire designed by Milanez de Campos [9]. The questions were translated into Chinese and the theory of reasoned action (TRA) was also applied to the questionnaire items in order to ensure its reliability and validity [13]. Moreover, the questionnaire was reviewed and revised according to 5 physicians’ and experts’ professional opinions and suggestions. This assured the content validity of the questionnaire. Additionally, the Cronbach's α coefficient of QoL of patients with or without thoracoscopic sympathectomy was 0.973, indicating that the consistency of the questionnaire content was high. The questionnaire included content regarding perceived QoL, health care experience (the patient received thoracoscopic sympathectomy or nonsurgical treatments, if other family members had similar symptoms, work status when asking for medical help, if physicians encouraged the patient to have the surgery and explained the problem of compensatory sweating in details, and if the patient concerned about compensatory sweating before the surgery), and basic demographics
Introduction
Hyperhidrosis occurs in every race with an incidence of 0.6% to 2.8% [1,2], and 12.5% to 65% of patients with hyperhidrosis have a family history of hyperhidrosis [3,4]. The treatment of hyperhidrosis is divided into medical therapy and surgical therapy. Medical therapy is effective for only a short period and has significant side effects, therefore it is not useful for long-term treatment. The most effective treatment for upper limb hyperhidrosis is thoracoscopic sympathectomy [5]. Despite different surgical methods [6-8], the success rate of thoracoscopic sympathectomy is between 95% and 99% [9]. However, severe compensatory sweating might happen after the surgery, which cannot be predicted through pre-operative evaluation. Additionally, the severity and prognosis of compensatory sweating is unpredictable [10,11].
In Taiwan, many patients with hyperhidrosis have received thoracoscopic sympathectomy, and thus the number of patients with severe compensatory sweating is significant. Due to this reason, on January 1, 2006 the Bureau of National Health Insurance, Taiwan, stipulated that patients with hyperhidrosis who want to receive thoracoscopic sympathectomy must be at least 20 years old and should be reviewed before the surgery in order to be paid by the National Health Insurance.
However, the number of patients with upper limb hyperhidrosis receiving the surgery has been declining. The reason for this decline is not known. Previous studies have performed quantitative assessments of the quality of life (QoL) before and after the surgery on patients with hyperhidrosis, and the satisfaction degree for thoracoscopic sympathectomy decreased with the passage of time due to recurrence within 12 months [12], but there are no long-term follow-up results. The present study aimed to investigate the relevant factors influencing the acceptance of thoracoscopic sympathectomy by patients with upper limb hyperhidrosis, and to further compare differences in the QoL between patients with and without thoracoscopic sympathectomy. Moreover, we also sought to obtain long-term postoperative results of patients with upper limb hyperhidrosis receiving thoracoscopic
(age, gender, educational level, marital status, monthly family income). A relative score showing the severity of influence on QoL based on different living conditions was given on a scale of 0 to 10. Zero indicated that hyperhidrosis did not influence the QoL at all, and 10 indicated that hyperhidrosis had a very severe impact on the QoL.
Statistical analysis
The Chi-square test and independent t-test were used to analyze differences between the patients who received and who did not receive thoracoscopic sympathectomy. Multivariate logistic regression was used to analyze significant related factors which influenced the patients with hyperhidrosis undergoing thoracoscopic sympathectomy, and stepwise approach was used to screen all relative variables. The dependent variable was if the patients received thoracoscopic sympathectomy or not, and the independent variables included demographic factors, medical factors, self-reported severity of the symptom, changes in quality of life, and influences of family, friends or media. A p value < 0.05 was considered to indicate statistical significance.
Results
Descriptive analysis and bivariate analysis
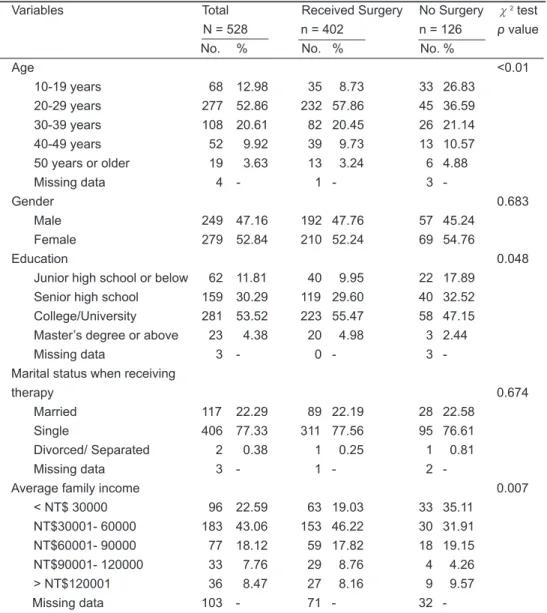
In Table 1, a total of 249 out of 528 subjects were male (47.16%). The subjects' ages are between 11 and 63 years old, and average age was 28.7 years. The average age of the patients receiving surgery was 28.69 years and that of the patients not receiving surgery was 27.42 years. When the age was older, the number of patients receiving thoracoscopic sympathectomy decreased. The highest proportion of patients receiving thoracoscopic sympathectomy had a college/university degree (55.47%). Table 2 indicates how the hyperhidrosis influences QoL in terms of different environments, movements, emotions, dressing, and leisure time. The subjects receiving surgery had average 7.21 points before surgery in terms of the severity of the impact on overall QoL, whereas those not receiving surgery had 4.89 on average. The impact on overall OoL significantly reduced from
7.21 to 5.22 after receiving surgery (p< 0.05), indicating that receiving sympathectomy could increase the hyperhidrosis patients’QoL. The top three items that most influenced both patients after receiving surgery and those not receiving surgery were‘in a closed or extremely hot environment (7.27 vs. 6.76 points)’and 'feel nervous (6.53 vs. 6.37 points)’, and the third item was‘wearing sandals or barefoot (5.89 points)’for the patients with surgery but it was‘holding someone’s hands (6.11 points)’for the patients without surgery instead.
The independent t-test was used to compare each item between patients after receiving surgery and those not receiving surgery (Table 2). In general, patients after receiving surgery still had higher average scores on symptoms influencing QoL, especially for items such as ‘wearing sandals or barefoot’,‘the appearance of wearing colorful clothes’,and‘while resting’(p< 0.05). Generally, regardless of receiving or not receiving the surgery, most patients had more than 6 points on items of‘in a closed or an extremely hot environment’and ‘feeling nervous’.
Moreover, the living conditions of the patients who received or did not receive surgery were compared. The result showed that‘the need of explanation for an embarrassing situation caused by hyperhidrosis’ had a higher level of influence on patients receiving surgery (p
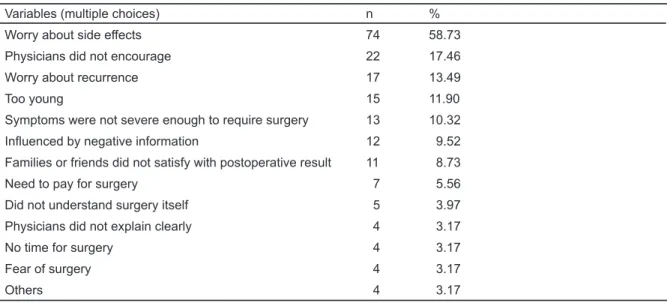
< 0.05). As for financial burden and family support for the surgery, there was a significant difference between these two groups. In terms of financial burden, the patients receiving the surgery had 1.56 points and the patients not receiving the surgery had 3.02 points (p< 0.05), in which the higher score means having a higher financial burden for the surgery. In terms of family support, the scores were 7.52 and 3.80 (p< 0.05), respectively, which means the patients with a surgery had a higher family supports. The reasons of not receiving sympathectomy were analyzed (Table 3), and the result showed that most patients did not chose thoracoscopic sympathectomy because of concerning about side effects (58.73%). Other reasons included physicians not encouraging to
perform the surgery (17.46%), worrying about recurrence (13.49%), too young (11.90%), or symptoms being not severe (10.32%).
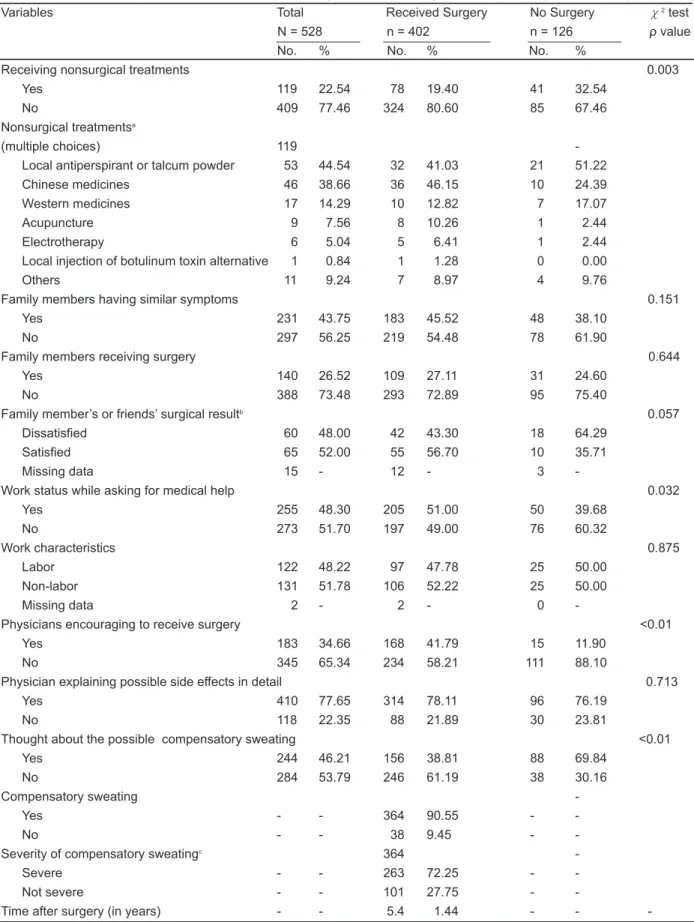
Table 4 shows the analysis of the patients' health care experiences. Approximately 32.5% of the patients who did not receive thoracoscopic sympathectomy tried nonsurgical treatments. For nonsurgical treatments, most patients used antiperspirant (44.54%) and Chinese medicine (38.66%), and only a few patients considered using acupuncture (7.56%), electrotherapy (5.04%), or local injection of botulinum toxin (0.84%) as an alternative. There was somewhat difference in‘family member's or friend's surgical results’between these two groups. The surgery group had more family members or friends with satisfied in the results of surgery than those without surgery group but the statistical significance is at border line (p=0.057). Moreover,‘work status while asking for medical help’was also a factor influencing the decision to undergo the surgery. A higher proportion (51.00%) of patients who received sympathectomy had a job, but work characteristic was not an influencing factor. With regard to physicians’attitudes, most physicians (65.34%) did not encourage the patients to receive thoracoscopic sympathectomy when the patients asked for medical help. However, we found that the surgery group had a significantly higher percentage (41.79%) in physicians encouraging to receive the surgery than those without surgery group (p< 0.05). Most physicians (77.65%) explained the side effects that might occur after the surgery for two groups in detail. There was a statistical significance in‘if patients had thought about the severity of compensatory sweating after seeing the doctor’between these two groups (p
< 0.05). Only 38.81% of the patients who received the surgery had thought about compensatory sweating, while 69.84% of the patients without surgery had thought about compensatory sweating. The present study further analyzed the incidence and the severity of compensatory sweating caused by sympathectomy. The results of average 5-year postoperative follow-up showed that 90.55% of the patients had compensatory sweating, and
72.25% of them had severe symptoms. It means that more than 60% of the patients who received thoracoscopic sympathectomy had severe compensatory sweating.
Logistic regression analysis was used to analyze the factors influencing receiving or not receiving sympathectomy. Table 5 shows the significant factors, including‘age’,‘influence on QoL before the surgery’,‘financial burden of receiving the surgery’, ‘level of family support to have the surgery’,‘if patients had received other non-surgical treatments’, ‘work status while asking for medical help’,‘if physicians encouraged to receive the surgery’,and‘if patients thought about compensatory sweating’(p< 0.05). Moreover, the probability of having sympathectomy was 5.06 times higher in patients 20-29 years of age than in patients 10-19 years of age (95% CI: 2.06-12.41). When controlling for other influencing factors, the probability of receiving sympathectomy increased by 1.24 times as every unit impact increasing on pre-operative QoL (95% CI: 1.11-1.39). When other influencing factors were kept the same, the probability of receiving sympathectomy decreased 20% as every unit increased in financial burden (95% CI: 0.72-0.89). When the level of family support in having sympathectomy increased one unit, the probability of having the surgery increased by 1.44 times (95% CI: 1.31-1.58). If the patient had a job when seeking medical help, their probability of receiving the surgery increased by 2.14 times (95% CI: 1.10-4.18). When physicians encouraged the patients to receive the surgery, the probability of receiving the surgery increased by 4.92 times (95% CI: 2.34-10.34). When the patients thought about the severity of compensatory sweating, their probability of receiving the surgery would reduce to 0.16 times (95% CI: 0.09-0.29). Overall, except for age, when physicians encouraged patients to receive surgery, the patient's willingness to have the surgery increased most. However, if the patient carefully considered the severity of compensatory sweating, the proportion of patients receiving the surgery decreased most.
related to a patient's personal characteristics and attitude. With regard to work, hyperhidrosis caused problems for patients who had a job; so this group of patients was more willing to receive the surgery. In terms of physicians’attitude, the present study found that the majority of physicians did not encourage the patients to receive sympathectomy. It can be seen that the patients had a sympathectomy primarily based on their personal willingness and physician's advice was only a secondary consideration. In terms of the consideration of compensatory sweating, most patients who cared about the possibility of compensatory sweating would not receive thoracoscopic sympathectomy. Thoracoscopic sympathectomy is the only way to eradicate hyperhidrosis with a high success rate and a low recurrence rate. However, once compensatory sweating occurs, it is permanent, and many patients might regret having had the surgery. The results of 5-year postoperative follow-up showed that 90% of the patients had compensatory sweating, and 70% of them felt their sweating was severe. This result is far more serious than those reported in other articles [14-17]. The possible reasons for this might be that the subjects recruited in the present study included patients with excessive palmar and axillary sweating. The choice of sympathetic ganglion location can affect the incidence of severe compensatory sweating. Moreover, average follow-up time of the present study was 5.4 years; the incidence and the severity of compensatory sweating may further increase with more time.
The results of logistic regression analysis showed that physician's encouragement to have the surgery was the most significant influencing factor (OR= 4.92). However, in the analysis of reasons for not receiving the surgery, the factor of‘physicians did not encourage’ was ranked the second. This might be because physicians realized that the incidence of severe postoperative compensatory sweating was high, and there was no acceptable treatment for it.
A l t h o u g h m o s t p a t i e n t s d e c i d e d t o h a v e a sympathectomy primarily based on personal willingness, physician's suggestions enhanced their willingness.
Discussion
In the present study, 231 out of 528 patients’ families (43.75%) had similar symptoms, which is consistent with the results of previous reports showing that 12.5% to 65% of hyperhidrosis patients have a family history of hyperhidrosis [7,9]. The present study analyzed the factors in terms of different scenarios which influence quality of life. It is generally believed that living conditions that are seriously affected by hyperhidrosis will be more of an influence on a patient's willingness to have thoracoscopic sympathectomy. The results revealed that after the patients had received the surgery, the patient group with surgery still felt significantly higher influence than those without surgery on‘wearing sandals or barefoot’,‘the appearance of wearing colorful clothes’,and‘having leisure activities’.Although the influencing level on QoL decreased from 7.21 points before surgery to 5.22 points after surgery, it was still higher than the average score of 4.89 in the patients who did not receive surgery. It could be thought that the hyperhidrosis patients’QoL was indeed improved by thoracoscopic sympathectomy; however, the situation was not better than what the patients might expect. This result is consistent with the study results by Milanez (2003), but the differences in influencing levels on QoL between these two studies cannot be compared [4].
The present study found that the reasons why the hyperhidrosis patients did not receive thoracoscopic sympathectomy. Most of the patients (58.73%) did not choose thoracoscopic sympathectomy because of concern of side effects. In addition to self-reported symptoms and objective influencing levels on QoL, subjective perception is also one of the important influencing factors, which is in accordance with the theory of reasoned action (TRA) presented by Fishbein & Ajzen [13].
In this study, the differences in health care experiences between the patients who received and who did not receive surgery were also compared. A higher proportion of patients without thoracoscopic sympathectomy tried nonsurgical treatments, especially antiperspirant and Chinese medicine. This is more
However, the major concern for patients in deciding to have the surgery or not is the side effect of compensatory sweating. Although the success rate of sympathectomy is high, patients need to consider the risks of anesthesia and adhesions. Moreover, complications such as hemothorax and pneumothorax could occur. Therefore, both physicians and hyperhidrosis patients need to evaluate, explain, and communicate carefully, and then choose an appropriate treatment. According to the Bureau of National Health Insurance database in Taiwan, we further analyzed the data and found the number of Taiwanese with upper limb hyperhidrosis receiving thoracoscopic sympathectomy decreased from 347 per million people in 2000 to 16 per million people in 2006. It seems to reflect that both hyperhidrosis patients and physicians
did not satisfy with the quality of life after the surgery of thoracoscopic sympathectomy over time.
Compensatory sweating cannot be prevented or treated, but many studies have suggested that different procedures such as T4 sympathectomy or sympathetic nerve block can reduce the severity of compensatory sweating [2,6]. However, many physicians might be unconvinced by these reports. Further research with different surgical methods is needed, including QoL analysis. Since the outcomes of T2 sympathetic block might not achieve patient expectations and satisfaction, we suggest the T2 sympathetic block surgery should be carefully performed after physicians have complete communication with patients.
Table 1. Sample Patients’ Demographics Information
Variables Total Received Surgery No Surgery χ2 test N = 528 n = 402 n = 126 ρ value
No. % No. % No. %
Age <0.01 10-19 years 68 12.98 35 8.73 33 26.83 20-29 years 277 52.86 232 57.86 45 36.59 30-39 years 108 20.61 82 20.45 26 21.14 40-49 years 52 9.92 39 9.73 13 10.57 50 years or older 19 3.63 13 3.24 6 4.88 Missing data 4 - 1 - 3 - Gender 0.683 Male 249 47.16 192 47.76 57 45.24 Female 279 52.84 210 52.24 69 54.76 Education 0.048
Junior high school or below 62 11.81 40 9.95 22 17.89 Senior high school 159 30.29 119 29.60 40 32.52 College/University 281 53.52 223 55.47 58 47.15 Master’s degree or above 23 4.38 20 4.98 3 2.44 Missing data 3 - 0 - 3 - Marital status when receiving
therapy 0.674
Married 117 22.29 89 22.19 28 22.58
Single 406 77.33 311 77.56 95 76.61
Divorced/ Separated 2 0.38 1 0.25 1 0.81 Missing data 3 - 1 - 2 -
Average family income 0.007
< NT$ 30000 96 22.59 63 19.03 33 35.11 NT$30001- 60000 183 43.06 153 46.22 30 31.91 NT$60001- 90000 77 18.12 59 17.82 18 19.15 NT$90001- 120000 33 7.76 29 8.76 4 4.26 > NT$120001 36 8.47 27 8.16 9 9.57 Missing data 103 - 71 - 32 -
Note: the average age of the patients receiving surgery was 28.69 ± 9.08 years; the average age of the patients not receiving surgery was 27.42 ± 11.72 years.
Table 2. Impact of Hyperhidrosis on Quality of Life and Family’s Supports
Received Surgery No Surgery t-test n = 402 n = 126 ρ value
Mean SD Mean SD
Variables of Quality of Lifea
Influence while in a closed or extremely hot environment 7.27 3.07 6.76 2.91 0.104
Influence when feeling nervous 6.53 3.37 6.37 3.07 0.634
Influence when wearing sandals or barefoot 5.85 3.58 4.66 3.56 0.001
Influence on holding others’ hands 5.69 4.01 6.11 3.53 0.295
Influence on shaking others’ hands 5.45 4.20 5.98 3.62 0.201
Influence on social activities 5.49 3.53 4.88 3.29 0.088
Influence on writing 5.36 3.90 5.07 3.24 0.401
Influence on holding things tightly 5.25 3.78 5.29 3.27 0.901
Influence on knowing new friends or touching others 5.27 3.70 5.17 3.40 0.782
Influence on exercise 5.22 3.51 4.87 3.26 0.308
Influence on hand work 5.19 3.80 4.93 3.08 0.430
Influence on intimate activities 4.99 3.56 4.45 3.23 0.134
Influence when feeling depressed or annoyed 4.92 3.54 4.56 3.43 0.306 Influence on wearing colorful clothes 4.49 3.70 3.33 3.35 0.002 Influence while facing problems or frustration 4.09 3.45 3.99 3.21 0.773
Influence on leisure time 3.57 3.00 2.90 2.62 0.025
Influence when thinking about questions 3.23 2.97 3.00 2.97 0.446 Influence on overall quality of life 5.22 2.46 4.89 2.25 0.181 Influence on quality of life before the surgeryb 7.21 2.52 - -
-Living Conditions and Supports
Cause embarrassing situation and need to explain to othersc 5.50 3.37 4.66 3.39 0.015 People would deliberately evadec 2.65 2.97 2.31 2.89 0.256 Financial burden of receiving surgeryd 1.56 2.38 3.02 3.33 <0.01 Family support to have the surgerye 7.52 2.85 3.80 3.51 <0.01 a 0-10 points represent the influencing level on quality of life. Higher score means the influence is greater.
b Respondents were the patients who had received the surgery. 0–10 points represent the influencing level on quality of life. Higher score means the greater influencing level.
c 0-10 points represent the frequency of occurrence. Higher score means the frequency of occurrence is more often. d 0-10 points represent the level of financial burden. Higher score means the higher financial burden for surgery. e 0–10 points represents the level of family support. Higher score means the level of family support is higher.
Table 3. Reasons for patients with hyperhidrosis not to receive thoracoscopic sympathectomy (N = 126)
Variables (multiple choices) n %
Worry about side effects 74 58.73
Physicians did not encourage 22 17.46
Worry about recurrence 17 13.49
Too young 15 11.90
Symptoms were not severe enough to require surgery 13 10.32
Influenced by negative information 12 9.52
Families or friends did not satisfy with postoperative result 11 8.73
Need to pay for surgery 7 5.56
Did not understand surgery itself 5 3.97
Physicians did not explain clearly 4 3.17
No time for surgery 4 3.17
Fear of surgery 4 3.17
Table 4. Health Care Experiences of Patients Receiving or Not Receiving Thoracoscopic Sympathectomy
Variables Total Received Surgery No Surgery χ2 test N = 528 n = 402 n = 126 ρ value
No. % No. % No. %
Receiving nonsurgical treatments 0.003
Yes 119 22.54 78 19.40 41 32.54
No 409 77.46 324 80.60 85 67.46
Nonsurgical treatmentsa
(multiple choices) 119
-Local antiperspirant or talcum powder 53 44.54 32 41.03 21 51.22
Chinese medicines 46 38.66 36 46.15 10 24.39
Western medicines 17 14.29 10 12.82 7 17.07
Acupuncture 9 7.56 8 10.26 1 2.44
Electrotherapy 6 5.04 5 6.41 1 2.44 Local injection of botulinum toxin alternative 1 0.84 1 1.28 0 0.00
Others 11 9.24 7 8.97 4 9.76
Family members having similar symptoms 0.151
Yes 231 43.75 183 45.52 48 38.10
No 297 56.25 219 54.48 78 61.90
Family members receiving surgery 0.644
Yes 140 26.52 109 27.11 31 24.60
No 388 73.48 293 72.89 95 75.40
Family member’s or friends’ surgical resultb 0.057
Dissatisfied 60 48.00 42 43.30 18 64.29
Satisfied 65 52.00 55 56.70 10 35.71
Missing data 15 - 12 - 3 -
Work status while asking for medical help 0.032
Yes 255 48.30 205 51.00 50 39.68 No 273 51.70 197 49.00 76 60.32 Work characteristics 0.875 Labor 122 48.22 97 47.78 25 50.00 Non-labor 131 51.78 106 52.22 25 50.00 Missing data 2 - 2 - 0 -
Physicians encouraging to receive surgery <0.01
Yes 183 34.66 168 41.79 15 11.90
No 345 65.34 234 58.21 111 88.10
Physician explaining possible side effects in detail 0.713
Yes 410 77.65 314 78.11 96 76.19
No 118 22.35 88 21.89 30 23.81
Thought about the possible compensatory sweating <0.01
Yes 244 46.21 156 38.81 88 69.84
No 284 53.79 246 61.19 38 30.16
Compensatory sweating
-Yes - - 364 90.55 - -
No - - 38 9.45 - -
Severity of compensatory sweatingc 364
-Severe - - 263 72.25 - -
Not severe - - 101 27.75 - -
Time after surgery (in years) - - 5.4 1.44 - -a Respondents were the patients who had received non-surgical treatments.
b Respondents were the patients whose families or friends had received the surgery. Satisfied included satisfied and very satisfied. Not satisfied included dissatisfied and very dissatisfied.
Table 5. Multivariate Logistic Regression Analysis of the Hyperhidrosis Patients Receiving or not Receiving Thoracoscopic Sympathectomy
Variables OR 95% CI Age 10-19 years (reference) 20-29 years 5.06 2.06 12.41 30-39 years 3.19 1.08 9.45 40-49 years 2.67 0.76 9.41 50 years or older 1.78 0.33 9.51
Influence on quality of life before the surgery 1.24 1.11 1.39 Financial burden while receiving surgery 0.80 0.72 0.89 Family support to have the surgery 1.44 1.31 1.58 Receiving other nonsurgical treatments
No (reference)
Yes 0.39 0.20 0.75
Work status when asking for medical help No (reference)
Yes 2.14 1.10 4.18
Physician encouraging to receive surgery No (reference)
Yes 4.92 2.34 10.34
Thinking about possible compensatory sweating No (reference)
Yes 0.16 0.09 0.29
Note : The dependent variables of the regression model were receiving surgery (n = 402) or not receiving surgery (n = 126) groups. The reference group was the group not receiving surgery.
References
1. Leung AK, Chan PY, Choi MC : Hyperhidrosis. Int J Dermatol 1999;38:561-7.
2. Panhofer P, Zacherl J, Jakesz R, et al. : Improved quality of life after sympathetic block for upper limb hyperhidrosis. Br J Surg 2006;93:582-6.
3. Ro KM, Cantor RM, Lange KL, et al. : Plamar hyperhidrosis: evidence of genetic transmission. J Vasc Surg 2002;35:382-6.
4. De Campos JR, Kauffman P, Werebe Ede C, et al. : Q u a l i t y o f l i f e b e f o r e a n d a f t e r t h o r a c i c sympathectomy: report on 378 operated patients. Ann Thorac Surg 2003;76:886-91.
5. Atkins JL, Butler PE : Hyperhidrosis: a review of c u r r e n t m a n a g e m e n t . P l a s t R e c o n s t r S u r g 2002;110:222-8.
6. Neumayer C, Zacherl J : Experience with limited e n d o s c o p i c t h o r a c i c s y m p a t h e t i c b l o c k f o r hyperhidrosis and facial blushing. Clin Auton Res 2003;13:52-7.
7. Dewey TM, Herbert MA, Hill SL, et al. :
One-year follow-up after thoracoscopic sympathectomy for hyperhidrosis: outcomes and consequences. Ann Thorac Surg 2006;81:1227-33.
8. Hashmonai M, Kopelman D, Assalia A : The treatment of primary hyperhidrosis: a review. Surg Today 2000;30:211-8.
9. Gossot D, Kabiri H, Ciliandro R, et al. : Early complications of thoracic endoscopic sympathectomy. A prospective study of 940 procedures. Ann Thorac Surg 2001;71:1116-19.
10. Kopelman D, Hashmonai M, Ehrenreich M, et al. : Upper dorsal thoracoscopic sympathectomy for palmar hyperhidrosis: improved intermediate-term results. J Vasc Surg 1996;24:194-9.
11. Rajesh YS, Pratap CP, Woodyer AB : Thoracoscopic sympathectomy for palmar hyperhidrosis and Raynaud's phenomenon of the upper limb and excessive facial blushing: a five year experience. Postgrad Med J 2002;78:682-4.
12. Rodríguez PM, Freixinet JL, Hussein M, , et al. : Si de e ffe cts, com plications and outcome of
thoracoscopic sympathectomy for palmar and axillary hyperhidrosis in 406 patients. Eur J Cardiothorac Surg 2008;34:514-19.
13. Fishbein M, Ajzen I : Belief, attitude, intention, and behavior: An introduction to theory and research. Reading, MA: Addison-Wesley, 1975.
14. Adar R, Kurchin A : Palmar hyperhidrosis and its surgical treatment: a report of 100 cases. Ann Surg 1977;186:34-41.
15. Lin TS, Kuo SJ, Chou MC : Uniportal endoscopic thoracic sympathectomy for treatment of palmar and axillary hyperhidrosis:analysis of 2000 cases. Neurosurgery 2002;51:84-7.
16. Doolabh N, Horswell S, Williams M, et al. : Thoracoscopic sympathectomy for hyperhidrosis: i n d i c a t i o n s a n d r e s u l t s. A n n T h o r a c S u r g 2004;77:410-14.
17. Ureña A, Ramos R, Masuet C, et al. : An assessment of plantar hyperhidrosis after endoscopic thoracic s y m p a t h i c o l y s i s. E u r J C a r d i o t h o r a c S u r g 2009;36:360-63.