Developing and validating a Chinese instrument
to measure lower urinary tract symptoms
among employed women in Taiwan
Yuan-Mei Liao, PhD, RNMolly C. Dougherty, PhD, RN, FAAN Alice R. Boyington, PhD, RN
Mary R. Lynn, PhD, RN
Mary H. Palmer, PhD, RN, FAAN
Lower urinary tract symptoms (LUTS), including urinary incontinence, negatively affect women’s quality of life. Employed women are particularly prone to expe-riencing the negative aspects of LUTS due to their irregular access to toilet facilities. In Taiwan, about 70% of women 25– 44 years of age are employed, yet little research on LUTS in the workplace has been conducted. In this article, the development of a Chi-nese instrument for estimating prevalence of LUTS and identifying factors related to LUTS among employed women is discussed. After instrument-generation and translations, content validity of the instrument was as-sessed and found to be satisfactory. Following a pilot test, psychometric testing of the instrument (which included test-retest reliability and internal consistency) was con-ducted. Test-retest reliability for the majority of the items and internal consistency for the construct LUTS were adequate. Based on initial psychometric testing, the authors suggest the instrument is appropriate for use with women in Taiwan. Additional testing is recommended before being used with other populations.
L
ower urinary tract symptoms (LUTS) are a health concern of particular relevance to women because the prevalence rates are higher than the rates for men.1– 4 Lower urinary tract symptoms can be dividedinto 3 main symptom groups: (1) storage (increased daytime urinary frequency, nocturia, urgency, and urinary incontinence [UI]), (2) voiding (slow stream, splitting or spraying, intermittent stream, hesitancy, straining, and terminal dribble), and (3) post-micturition (feeling of incomplete emptying and post-micturition dribble).5
These symptoms have widespread human and social implications, and cause physical discomfort, shame, and loss of self-confidence that can negatively affect a woman’s quality of life (QOL).6 – 8
The prevalence rates of LUTS for women, which range from 28%– 69%, have been reported for Austra-lia, Denmark, and the United Kingdom.2,3,6,7,9 Stimu-lated by the International Continence Society (ICS), a large body of research on UI from Europe and North America has been reported. For⬎ 40 years, research on LUTS focused on UI, nocturia, and overactive blad-der.10 The prevalence of UI was estimated to be
20 –30% for young adult women, 30 – 40% for middle-aged women, and 30 –50% for elderly women.1 One national survey conducted in the US (N⫽ 5,204; 52.6% female) demonstrated that 31% and 19.6% of the subjects experienced⬎ 1–2 void(s)/night, respectively.11Stewart and colleagues reported that the prevalence of overac-tive bladder among women was around 16.5% in the US.12 In the past 10 years, interest about other LUTS has increased. However, notably lacking are interna-tional studies on LUTS, particularly those on the prevalence of LUTS in women living in Asia.
A better understanding of LUTS is needed to de-velop approaches to manage LUTS. Very little research has addressed the role that the workplace has in women’s experiences with LUTS, although research from the US indicates that this is an important area of investigation.13–16Almost 70% of nurses/nursing
assis-tants avoid urinary elimination during their work shift.17Employed women are not only exposed to the general risk factors for LUTS, but also to risk factors such as inadequacy of bathroom breaks or toilet facil-ities from their work environments. Infrequent voiders
Yuan-Mei Liao is an Assistant Professor at the College of Nursing,
Taipei Medical University, Taipei, Taiwan.
Molly C. Dougherty is a Professor at the School of Nursing, University
of North Carolina at Chapel Hill.
Alice R. Boyington is Director of Nursing Research and Education at
H. Lee Moffit Cancer & Research Institute, Tampa, FL.
Mary R. Lynn is an Associate Professor at the School of Nursing,
University of North Carolina at Chapel Hill.
Mary H. Palmer is a Professor at the School of Nursing, University of
North Carolina at Chapel Hill.
Reprint requests: Miss Yuan-Mei Liao, Taipei Medical University, College of Nursing, 250 Wu-Hsing Street, Taipei, Taiwan110.
E-mail: ymliao@tmu.edu.tw Nurs Outlook 2006;54:353-361.
0029-6554/06/$–see front matter
Copyright © 2006 Mosby, Inc. All rights reserved. doi:10.1016/j.outlook.2006.09.003
(eg, “nurse’s bladder,” and “teacher’s bladder”) who have developed the habit of holding their urine for prolonged periods of time and voiding only a few times each day, are predisposed to urine stasis, voiding dysfunction, and infections.4
In Taiwan, about half of the adult women are employed and about 70% of women 25– 44 years of age are working.18Traditionally, women bear more respon-sibility and obligation of taking care of the elderly and children in their family than men.19 Employed women perform more than one role at a time, and these multiple roles reduce the time they allot for personal health promotion, which may lead to their treating LUTS as a minor concern. Symptoms such as urgency and fre-quency are not only bothersome but may also lead to urinary incontinence without appropriate management, LUTS may develop into a severe condition and increase the cost for managing LUTS.
Several questionnaires developed to assess LUTS lacked estimates of reliability and validity2,6,9and none addressed assessment of LUTS in employment settings. The Bristol Female Lower Urinary Tract Symptoms (BFLUTS) questionnaire is a valid instrument currently available.7,20However, post-micturition symptoms and questions to assess the role of workplace were not included in the BFLUTS questionnaire. Therefore, a valid and reliable instrument to measure LUTS for em-ployed women was needed. Available generic instruments developed to assess LUTS were not sensitive to factors related to LUTS in working environments.2,6,7,9,20 Previ-ous research indicated that LUTS often can be effec-tively managed with behavioral strategies.21,22 Ap-proaches to the assessment of LUTS in workplaces are needed to support the introduction of behavioral strat-egies to manage LUTS. The purpose of this study was to develop and test an instrument for estimating prev-alence of LUTS and to identify factors related to LUTS among employed women in Taiwan.
METHODS
Instrument development included 3 phases: (1) concep-tual framework generation, (2) instrument generation, and (3) psychometric testing.
Conceptual Framework Generation
The conceptual framework for the Taiwan Teacher Bladder Survey (TTBS) was based on the concepts in Palmer’s Continence Promotion Model and evidence in the literature. Palmer’s model supports an interdiscipli-nary approach to managing UI.23 It includes multiple causative and associated factors located external to the urinary tract as well as cognitive and functional char-acteristics of the individual. Because UI is one of the prevalent LUTS among women,1–3,6 and the factors associated with LUTS are similar to the factors associ-ated with UI,1,9,24 –29 Palmer’s Continence Promotion Model was used to develop the conceptual framework
for the TTBS (Figure 1). In the conceptual framework of the TTBS, 3 constructs (individual characteristics, personal habits, and work-related factors) were concep-tualized as explaining the presence of LUTS, the fourth construct.
Individual characteristics were conceptualized as biologic factors and obstetric/gynecologic factors. Bio-logic factors were seen as rooted in the history of the individual in a broad sense. Age was computed using the individual’s year of birth. Body Mass Index (BMI⫽ kg/m2) was used as an index for judging the body weight and the amount of body fat. Family history of LUTS was defined as a family member among individ-uals’ first-degree relatives (ie, mothers, sisters, daugh-ters) who have or had the experiences of LUTS. Biologic factors exist; they may or may not be modifi-able. Obstetric/gynecologic factors are consequences of events such as pregnancy or surgery that affect the function of the genitourinary system and were not seen as modifiable. Vaginal delivery and surgery were de-fined as the presence or absence of a history of vaginal delivery and obstetric and/or gynecological surgery, respectively. Pregnancy referred to women who were in the state of being pregnant. Parity referred to total number of childbirths.
The personal habits construct was conceptualized as being within the control of the individual. Fluid intake was related to LUTS through the production, storage of urine, and voiding because the amount of urine pro-duced and stored is directly related to fluid intake.27 Bladder habits were conceptualized as individuals’ behaviors of delaying urination and restricting hydra-tion. Individuals who frequently performed these be-haviors were conceptualized as individuals with poor bladder habits. Life-style factors were individuals’ hab-its of caffeine consumption and smoking. Caffeine consumption was conceptualized as affecting urine
stor-Figure 1. Conceptual Framework of the Taiwan Teacher
age and voiding because it is a bladder irritant and is associated with LUTS. Smoking was conceptualized as affecting LUTS because smokers often have a chronic cough, which is related to UI, particularly stress UI.
Within the construct work-related factors, associa-tions between some environmental factors and job conditions were evaluated. Environment factors in-clude: (1) adequacy of bathroom breaks, (2) adequacy of toilet facilities, and (3) availability of relief persons. These 3 factors are conceptualized as contributing to a prolonged voiding interval, which is related to large volume urine storage and contributes to symptoms of urgency and stress UI.4 Job conditions were concep-tualized as (1) amount (length of time) of standing, (2) frequency of straining to lift, and (3) job control. Amount of standing at work was related to LUTS by problems with urine storage related to the gravitational pull on the pelvic organs including the bladder. Strain-ing to lift heavy objects was conceptualized to relate to LUTS in a similar way. When women strain to lift heavy objects in the presence of high parity and vaginal delivery, anatomic and physiologic changes occur and contribute to the downward movement of the bladder and urethra and to stress UI. Job control was concep-tualized as high when the individual has the opportunity to toilet whenever she chooses. Low job control is conceptualized as contributing to abnormal voiding amounts, specifically large volume voids that usually result from a prolonged voiding interval.
The construct LUTS referred to the lower urinary tract symptoms that individuals may experience at 3 phases (urine storage, urine voiding, and post-micturition). The definitions for UI, increased daytime urinary frequency, urgency, intermittent stream, weak urinary stream, and hesitancy used in the TTBS were based on the stan-dardization report proposed by the ICS.5Nocturia was defined as the complaint that the individual has to wake at nightⱖ 2 times to void because this definition was commonly used in previous studies.2,3,7 Incomplete emptying was defined as the sensation that urine is left in the bladder after micturition.30
Background Research for the TTBS
The initial research that provided the basis for the instrument developed came from a study of the pres-ence of LUTS among public school teachers in North Carolina (unpublished observations).13Items in the North Carolina Teachers Bladder Survey (NC TBS) were de-rived from the literature and previous research.31–34The NC TBS was the only instrument that covered the majority of the constructs for developing the TTBS, which was based on the items in the NC TBS and evidence in the literature.
The NC TBS included 75 items plus 5 items about teachers’ experiences on the usage of the Internet. The NC TBS was refined with studies of content validity, pilot testing, and test-retest reliability testing. Content
validity of the NC TBS was determined and quantified by the index of content validity (CVI).35 Fifty-one items related to the study constructs (bladder habits, bladder symptoms, continence-related health, fluid in-take habits, and work environment) were sent for review by 8 experts. Content validity of the NC TBS was established with the CVI values for all the 51 items reaching .88.13Modifications were made based on the suggestions provided by the participants in the pilot study (N ⫽ 31). Of the 75 items on the revised NC TBS, 63 items were evaluated for agreement across a 1-week time period (n⫽ 44). Twelve items related to fluid intake habits on usual school day/days off and demographics that were not considered adequate for test-retest assessment were not sent for testing. The overall average percent agreement was 85% (SD ⫽ 11.78, range 55–100%) across the 63 items which resulted in an adequate test-retest reliability.13
Instrument Generation and Psychometric Testing
The process of instrument generation and psychometric testing of the TTBS involved 7 steps: (1) development of the TTBS; (2) instrument translation; (3) content validity testing; (4) human subjects (ethical) review; (5) pilot testing; (6) test-retest reliability testing; and (7) testing the internal consistency of the LUTS con-struct.
Development of the TTBS
Twenty-eight items in the NC TBS that were not associated with the aims of developing the TTBS were eliminated, including the items related to the usage of the Internet (5 items), bother resulting from different types of LUTS (5 items), school environment (4 items) (ie, time to report to and leave school, stress and problems that came from scheduling bathroom breaks), teachers’ individual characteristics (13 items) (ie, eth-nicity, teaching experience, the use of oral contracep-tives, menstrual periods, sexual activity, career status, and household income) and teachers’ fluid intake habits on days off (1 item). One item addressing the symptom “increased daytime urinary frequency” was added be-cause it is a common LUTS according to the standard-ization report proposed by the ICS.5 Fifteen items related to the frequency and duration for different types of LUTS were added because it is recommended that such information be collected in all epidemiological studies for LUTS.1 Because bladder pain and bashful bladder were not common LUTS,2,3,6,9these questions were eliminated. However, one item addressing any other LUTS that employed women may experience was added. For burning during urination and itching or burning in the vaginal area, 2 items that addressed teachers’ current experiences were added. The reason of adding these 2 items was to exclude LUTS (ie, UI, frequency, urgency) that might result from urinary tract
infections (UTIs).27 One item that addressed bother resulting from any type of LUTS was added. The item that addressed teachers’ help-seeking behavior was retained.
Five items related to family history of LUTS, teach-ers’ neurologic conditions, amount (length of time) of standing at work, frequency of straining to lift heavy objects at work, and amount of control over jobs were added because these conditions/experiences might be associated with LUTS.4,14,15 Three items about teach-ers’ health-related conditions (diabetes mellitus, chronic cough, and chronic constipation) and one item about teachers’ habits of performing regular exercise were retained because these conditions might be associated with LUTS.9,36Five items about the duration of teach-ers’ health-related conditions including teachteach-ers’ neu-rologic conditions and habits of performing regular exercise were added to acquire more information on these conditions. The first draft of the English TTBS that included 79 items to collect information about LUTS and UTI, individual characteristics, personal habits, and work-related factors was generated.
The first draft was reviewed by a measurement expert, Teresa Edwards, Assistant Director for Survey Research at the Odum Institute for Research in Social Science, University of North Carolina at Chapel Hill. Based on the expert’s recommendations, some modifi-cations were made on items and response options. For example, the last response option for the frequency of symptom “increased daytime urinary frequency” was modified from “every day and/or night” to “every day.” Modifications were also made on the format of the first-draft TTBS to improve ease of response.
Instrument Translation
The translation/back translation process used for the TTBS was modified from the process recommended by the International Quality of Life Assessment (IQOLA) project in translating a health survey.37The process of translation and back translation was used to achieve semantic and conceptual equivalence between the Chinese version TTBS and the English version TTBS. The translation/back translation process involved 3 steps: (1) two bilingual experts whose native language was Chinese translated the English TTBS into Chinese, (2) another 2 bilingual experts whose native language was English translated the Chinese version TTBS back into English, and (3) the 2 English version TTBSs were compared to the original English version TTBS by an expert whose native language was English to assess semantic and conceptual equivalence. Two criteria were emphasized during the translation/back translation pro-cess: (1) the translation should replicate the original as closely as possible in capturing the closest possible meaning, and (2) the translation should be sensitive to cultural adaptation on items that were difficult to translate.37,38
Content Validity Testing
Content validity of the Chinese version TTBS was determined and quantified using a Content Validity Index (CVI).35 Nine experts (3 female elementary
school teachers, 2 urologists, 2 women’s health special-ists, and 2 experienced nurses) whose native language was traditional Chinese were invited to review content validity of the Chinese version TTBS. The grade system used a 4-point scale proposed by Lynn.35 Of the 79
items in the TTBS, 54 were sent to experts for evalu-ation. Twenty-three of the remaining items related to individual characteristics were excluded from evalua-tion because these items were focused on describing the participants and were not specific to the aims of developing the TTBS. Finally, one item each about the bother resulting from any LUTS and about teachers’ help-seeking behaviors was also excluded because these items were not directly relevant to the aims of developing the TTBS.
Pilot Testing
Institutional review board (IRB) approval from the School of Nursing, University of North Carolina at Chapel Hill was obtained for psychometric testing with human subjects. To maximize clarity of the content of the TTBS, a pilot study was conducted. The aims of conducting a pilot study were to obtain feedback from participants on possible problem areas on the TTBS and to identify possible problems in the data collection process. In addition to the content of the TTBS (79 items), 2 questions addressing the problems that might occur during the process of completing the survey and suggestions for any item were added. An item about the time the respondent spent on completing the survey was added also.
Advertisements for participation in a study to help with the development of an instrument were posted on the bulletin boards at 3 elementary schools outside of Taipei city. Thirty female elementary school teachers were invited to complete the TTBS. Informed consent letters, surveys, and incentives (10 US dollars) were provided. The informed consent letter stated that by completing the TTBS, the participants gave permission that their data would be used in the aggregate. A sealed box was left in each school’s academic office. Teachers were instructed to return their completed surveys to the sealed box within 1 week. The principal investigator then collected the box after 1 week of the survey distribution to assure confidentiality.
Test-Retest Reliability Testing
An advertisement for the test-retest study was posted on a bulletin board in one elementary school outside of Taipei city. Thirty schoolteachers were invited to com-plete the TTBS twice at a 10-day interval. The process of the test-retest study was similar to the process carried out in the pilot study except that the same process was
carried out twice. An extra cover page was added to the TTBS. Participants were requested to leave some per-sonal information (ie, numbers of brothers, sisters, and month of birth) on the extra cover page in order to help with the correct matching of their first responses to their second ones. This is similar to the procedure recom-mended by Damrosch for creating anonymous codes for linking over time measures without having the partici-pants provide identifiable codes or linkages.39 Individ-ual characteristics (ie, body height, parity) collected from the surveys were used to insure correct matching also.
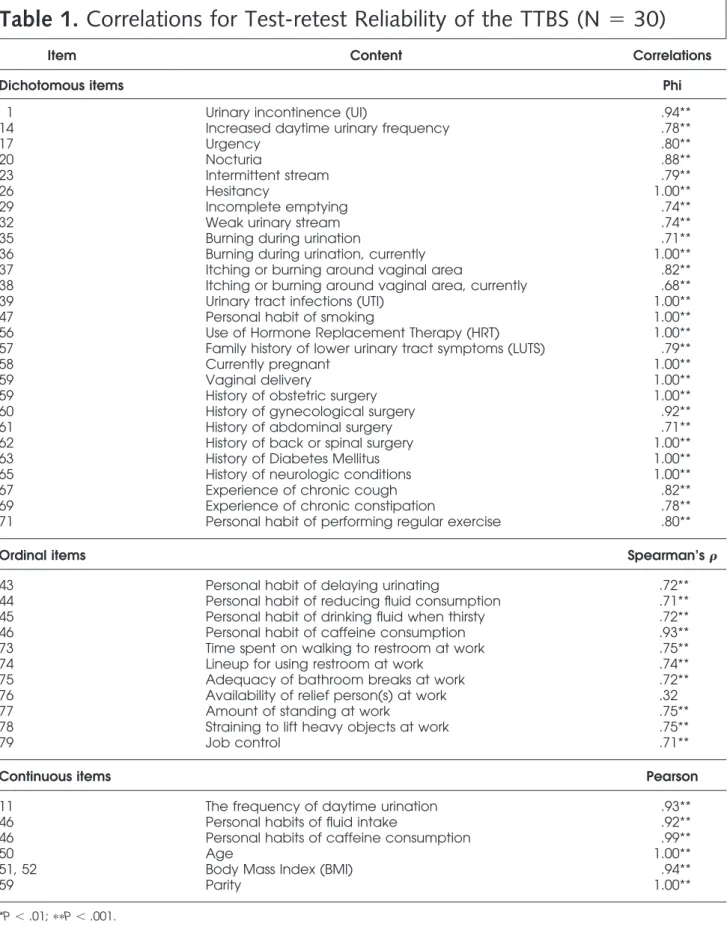
Of the 79 items in the TTBS, 41 items were considered relevant for test-retest assessment. Test-retest reliability for items about the presence of LUTS and UTIs (14 items), individual characteristics (14 items), personal habits (6 items), and work-related factors (7 items) were assessed. Thirty-eight items about the frequency and duration of LUTS (26 items), bother resulting from any type of LUTS (1 item), and teachers’ help-seeking behaviors (1 item), duration of smoking habits and number of cigarettes consumed (2 items), individual characteristics (3 items) (ie, mar-ital status, teaching years and teaching grads), and durations of some health conditions and performing regular exercise (5 items) were excluded from test-retest assessment because these items were not related to the major constructs of the TTBS.
Testing the Internal Consistency of the LUTS Construct
Twenty-six elementary schools were selected from the 152 elementary schools in Taipei. After the approv-als for conducting the main study from the selected schools were acquired, a second-stage simple random sampling of 20 female teachers in each school was conducted. A total of 520 surveys were distributed to the 26 elementary schools. Because 68 out of the 520 selected teachers refused to answer the surveys, 68 teachers were randomly selected as substitutes in the schools where the 68 original selected teachers were employed. The process of the main study was similar to that of the pilot study.
STATISTICAL ANALYSIS
Statistical Analysis System (SAS) for Windows was used to conduct the data analysis. Simple frequency distributions and repeated inspection were used to verify the data. Descriptive statistics were used to display the distributions of participants’ individual characteristics.
The standard for evaluating content validity was based on the standard proposed by Lynn35for the CVI (at least 7 out of 9 experts must agree that the item is content-valid by giving the item a grade of 3 or 4 points). For evaluating test-retest reliability, Phi, Spear-man, and Pearson correlations were calculated for the
nominal, ordinal, and continuous variables, respec-tively. Reliability coefficients ⱖ .70 were considered satisfactory.40,41 For testing the internal consistency, Kuder-Richardson Formula 21 (KR-21) was used to test the construct LUTS including items about LUTS with and without items about UTI. For a newly developed instrument, the value of KR-21ⱖ .70 was considered adequate.42
FINDINGS
Instrument Translation
The Chinese translations captured the content of the original TTBS with appropriate adaptation to the cul-tural context. The back translations only differed a little from the original English version. The expert confirmed the conceptual equivalence among the 3 English ver-sions. Because no specific problem was identified during the translation/back translation process, no mod-ification was made on the first Chinese version TTBS.
Content Validity Testing
Nine experts graded all 54 items as either 3 or 4 points; the CVI for all 54 items was 1.00. The content validity for the first Chinese version TTBS was estab-lished.
Pilot Testing
Of the 30 participants, 23 (76.7%) were 31–50 years of age (Mean ⫽ 39.20, SD ⫽ 7.99), the majority of them were married (n⫽ 25; 83.3%) and had a normal BMI (n⫽ 17; 56.7%). Twelve (40.0%) participants had never given birth. Of the other 18 participants who had given birth, 15 (50.0%) had given birth twice and 11 (39.2%) had experienced vaginal birth. The average time spent on completing the TTBS was 19 minutes (range ⫽ 10–35). Participants did not report any specific problem on the process of completing the TTBS.
Item 46 (teachers’ fluid intake and caffeine con-sumption) was modified based on the written com-ments. Several schoolteachers expressed that they had trouble answering the item on the types of tea beverages they usually consumed. Instead of drinking a specific type of tea, they drank different kinds of tea every day. Based on the information collected from 3 supermarkets at Taipei and from participants’ comments, changes were made on the tea with caffeine category. Four different categories (fully fermented, re-fermented, lightly fer-mented, and unfermented) were added based on different caffeine content in each category.43Two subcategories were added to the coffee with caffeine category, instant coffee and brewed coffee or coffee made by dip method.43
Test-Retest Reliability Testing
Of the group involved in test-retest reliability testing (n⫽ 30), 25 (83.3%) were 31–50 years of age (Mean ⫽
44.50, SD⫽ 6.71), the majority of them were married (n ⫽ 26; 86.7%) and had a normal BMI (n ⫽ 20; 66.7%). Five (16.6%) participants had never given birth. Of the other 25 participants who had given birth, 21 (70.0%) had given birth twice and 21 (70.0%) had experienced vaginal birth.
Correlation values for the majority of the 41 items exceeded the criterion set at .70 and were judged adequate; two items (items 38 and 76) designed for assessing teachers’ current experiences of itching or burning around vaginal area and the availability of relief persons at schools received a value ⬍ .70 (Table 1).
Because the correlation value for item 38 was slightly less than the criterion of .70 (Phi ⫽ .68), this item was not modified. In regard to item 76 (Spear-man’s ⫽ .32), some teachers noted that no relief persons were available at their schools. Other teachers indicated that no need existed for such persons. At some schools, student teachers that are senior students at colleges or universities may be available as relief persons. However, in general, relief persons are not available in elementary schools in Taiwan. The item about the availability of relief persons was retained and another item about the need of relief persons’ existence was added. The item “How often do you believe that the existence of a relief person is necessary?” with 4 response options (never, sometimes, usually, and al-ways) was added to the TTBS. The final Chinese version TTBS was generated and included 80 items.
Testing the Internal Consistency of the LUTS Construct
For the internal consistency analysis, of a total 471 completed surveys, 445 were usable and 26 were excluded for analysis because of item non-response. Of the 445 participants, 389 (87.5%) were 26 –50 years of age (Mean⫽ 38.93, SD ⫽ 8.56), the majority of them were married (n⫽ 295; 66.3%) and had a normal BMI (n ⫽ 350; 78.8%). One hundred and eighty-eight women (42.8%) had given birth twice, 185 (43.7%) had experienced vaginal births, and 142 (32.5%) had under-gone gynecological surgery. Values of internal consis-tency for the construct LUTS were calculated with (.72) and without (.71) the items about UTI and exceeding the criterion of .70 and were considered as adequate.
DISCUSSION
Despite concerns about wording problems of some items and response options, overall the translation/back translation process resulted in a Chinese language TTBS determined to be equivalent to the original English TTBS. The systematic and scientific process used to translate the instrument made the international, cross-cultural study possible.
Items and response options in the TTBS were easily understood because attention had been paid to the
educational level, culture, and idiomatic preference of potential subject groups. The panel of experts was diverse, representing opinions that might come from subjects, clinicians, and academics. In the future, con-struct validity of measures of LUTS can be assessed if there is a “gold standard” for the assessment of LUTS44,45 or a definitive determination of whether a woman does (or does not) have LUTS as a discreet entity. At this time, choosing the criterion for future validation studies should be done cautiously. In addi-tion to the use of urodynamics, which are considered to be the best diagnostic tool in assessment of lower urinary tract function,46 using extra assessment meth-ods such as history-taking and voiding diaries to con-firm the validity of the construct LUTS may be suitable approaches to consider in construct validity testing.
For test-retest reliability, the TTBS produced stable results over a 10-day interval. The interval between 2 contacts met the general recommendation of an interval of approximately 1–2 weeks between 2 administra-tions.40Using a 10-day interval avoided the participants undergoing real changes in the characteristics under study and limited carry-over, or memory effects. The adequate value on the internal consistency reliability for the construct LUTS supports the internal consistency of the participants’ responses to the TTBS items.
LIMITATIONS
Because the construct LUTS has not been well-investigated, measurement of this construct is in its infancy. No “gold standard” or established criterion measurement for the assessment of LUTS,44,45personal habits or work-related factors that contribute to the devel-opment of LUTS is available which limits the feasibility of carrying out further validity testing. The assessment of construct validity of the Chinese version TTBS will commence as the conceptual and measurement work in this area advances. Despite this limitation, the content validity foundation of the Chinese version TTBS is a solid foundation for further validity work.
A limitation of the test-retest study is that the participants were volunteers and it is possible that these teachers remembered their initial responses because they knew that they would complete the survey again when they enrolled in the test-retest study. Recruiting a large sample and informing the enrolled participants that they might be randomly selected to complete the survey for a second time would be a preferred approach for future test-retest assessments. Calculations of the internal consistency for the constructs personal habits and work environment in the TTBS were not feasible because the response options varied across the different questions.
CONCLUSION
The lack of a specific instrument for measuring LUTS among employed women, coupled with an increasing
Table 1. Correlations for Test-retest Reliability of the TTBS (N
⫽ 30)
Item Content Correlations
Dichotomous items Phi
1 Urinary incontinence (UI) .94**
14 Increased daytime urinary frequency .78**
17 Urgency .80**
20 Nocturia .88**
23 Intermittent stream .79**
26 Hesitancy 1.00**
29 Incomplete emptying .74**
32 Weak urinary stream .74**
35 Burning during urination .71**
36 Burning during urination, currently 1.00**
37 Itching or burning around vaginal area .82**
38 Itching or burning around vaginal area, currently .68**
39 Urinary tract infections (UTI) 1.00**
47 Personal habit of smoking 1.00**
56 Use of Hormone Replacement Therapy (HRT) 1.00**
57 Family history of lower urinary tract symptoms (LUTS) .79**
58 Currently pregnant 1.00**
59 Vaginal delivery 1.00**
59 History of obstetric surgery 1.00**
60 History of gynecological surgery .92**
61 History of abdominal surgery .71**
62 History of back or spinal surgery 1.00**
63 History of Diabetes Mellitus 1.00**
65 History of neurologic conditions 1.00**
67 Experience of chronic cough .82**
69 Experience of chronic constipation .78**
71 Personal habit of performing regular exercise .80**
Ordinal items Spearman’s
43 Personal habit of delaying urinating .72**
44 Personal habit of reducing fluid consumption .71**
45 Personal habit of drinking fluid when thirsty .72**
46 Personal habit of caffeine consumption .93**
73 Time spent on walking to restroom at work .75**
74 Lineup for using restroom at work .74**
75 Adequacy of bathroom breaks at work .72**
76 Availability of relief person(s) at work .32
77 Amount of standing at work .75**
78 Straining to lift heavy objects at work .75**
79 Job control .71**
Continuous items Pearson
11 The frequency of daytime urination .93**
46 Personal habits of fluid intake .92**
46 Personal habits of caffeine consumption .99**
50 Age 1.00**
51, 52 Body Mass Index (BMI) .94**
59 Parity 1.00**
recognition of the effects of work environments on LUTS, provided a stimulus to develop a new measure for LUTS among employed women. Usually, validity of an instrument is not fully established during the initial scale development period. Because validation is a cumulative, ongoing process47and the most success-ful instruments are those for which the authors take long-term responsibility for further refinement,48more research is needed on the TTBS. The Chinese version TTBS and the English version TTBS are available for use from the first author. However, psychometric test-ing for the English version is not currently available.
Information about LUTS in teachers, nurses, and other occupations at risk can be collected by using this instrument. Knowledge about LUTS among employed women in Asia will be advanced by use of the Chinese version TTBS. With a better understanding of LUTS, intervention studies that incorporate modifications of personal habits or of the workplace can be designed to foster management of LUTS for employed women.
The authors wish to acknowledge the assistance of all the elementary school teachers who participated in the studies as well as Teresa Edwards, Assistant Director for Survey Research at the Odum Institute for Research in Social Science, University of North Caro-lina at Chapel Hill, and the other experts who were involved in the development of the TTBS.
REFERENCES
1. Hunskaar S, Burgio K, Diokno AC, Herzog AR, Hjalmas K, Lapitan MC. Epidemiology and natural history of urinary incontinence (UI). In: Abrams P, Cardozo L, Khoury S, Wein A, editors. Incontinence. Plymouth, UK: Health Pub-lication Ltd; 2002. p. 165-201.
2. Perry S, Shaw C, Assassa P, Dallosso H, Williams K, Brittain KR, et al. An epidemiological study to establish the prevalence of urinary symptoms and felt need in the community: The Leicestershire MRC Incontinence Study. J Public Health Med 2000;22:427-34.
3. Pinnock CB, Marshall VA. Troublesome lower urinary tract symptoms in the community: a prevalence study. Med J Aust 1997;167:72-5.
4. Wall LL, Norton PA, DeLancey JOL. Practical urogynecol-ogy. Baltimore, MD: Williams & Wilkins; 1993.
5. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmeten U, et al. The standardization of terminology of lower urinary tract function: report from the standardization sub-committee of the International Continence Society. Am J Obstet Gynecol 2002;187:116-26.
6. Moller LA, Lose G, Jorgensen T. The prevalence and bothersomeness of lower urinary tract symptoms in women 40-60 years of age. Acta Obstet Gynecol Scand 2000;79: 298-305.
7. Swithinbank LV, Donovan JL, Heaume JC, Rogers CA, James MC, Yang Q, et al. Urinary symptoms and inconti-nence in women: relationships between occurrence, age, and perceived impact. Br J Gen Pract 1999;49:897-900. 8. Kelleher C. Quality of life and urinary incontinence. In:
Cardozo L, Staskin DJ, editors. Textbook of female urology and urogynaecology. London: Isis Medical Media Ltd; 2001. p. 47-57.
9. Moller LA, Lose G, Jorgensen T. Risk factors for lower urinary tract symptoms in women 40 to 60 years of age. Obstet Gynecol 2000;96:446-51.
10. Palmer MH. Use of health behavior change theories to guide urinary incontinence research. Nurs Res 2004;53:49-55. 11. Coyne KS, Zhou Z, Bhattacharyya SK, Thompson CL,
Dhawan R, Versi E. The prevalence of nocturia and its effect on health-related quality of life and sleep in a community sample in the USA. BJU Int 2003;92:948-54.
12. Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol 2003;20:327-36.
13. Boyington AR, Dougherty MC, Lynn MR, Liao YM, Lin SY. Development and testing of the Teachers Bladder Survey. Unpublished manuscript (under review).
14. Fitzgerald ST, Palmer MH, Kirkland VL, Robinson L. The impact of urinary incontinence in working women: a study in a production facility. Women Health 2002;35:1-17. 15. Palmer MH, Fitzgerald S, Berry SJ, Hart K. Urinary
incon-tinence in working women: an exploratory study. Women Health 1999;29:67-82.
16. Sampselle CM, Palmer MH, Boyington AR, O’Dell KK, Wooldridge L. Prevention of urinary incontinence in adults: population-based strategies. Nurs Res 2004;53:61-7. 17. Bendtsen AL, Andersen JR, Andersen JT. Infrequent voiders
syndrome (nurses bladder): prevalence among nurses and assistant nurses in a surgical ward. Scand J Urol Nephrol 1991;25:201-4.
18. Directorate – General of Budget, Accounting and Statistic, Executive Yuan. Age Labor force participation rates, by year in Taiwan area. 2004. Available at:http://www.stat.gov.tw/ public/data/dgbas04/bc4/yrtable7.xls. Accessed on August 1, 2005.
19. Chao SY, Roth P. The experience of Taiwanese women caring for parents-in-law. J Adv Nurs 2000;31:631-8. 20. Jackson S, Donovan J, Brookes S, Eckford S, Swithinbank
L, Abrams P. The Bristol Female Lower Urinary Tract Symptoms questionnaire: development and psychometric testing. Br J Urol 1996;77:805-12.
21. Burgio KL. Behavioral treatment options for urinary incon-tinence. Gastroenterology 2004;126:82-9.
22. Tomlinson BU, Dougherty MC, Perdergast JF, Boyington AR, Coffman MA, Pickens SM. Dietary caffeine, fluid intake and urinary incontinence in older rural women. Int Urogynecol J Pelvic Floor Dysfunct 1999;10:22-8. 23. Palmer MH. Interdisciplinary approaches to the treatment of
urinary incontinence in older adults. Top Geriatr Rehabil 2000;16:1-9.
24. Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community-based epidemiological survey of female urinary incontinence: The Norwegian EPINCONT study. J Clin Epidemiol 2000;53:1150-7.
25. Peyrat L, Haillot O, Bruyere F, Boutin JM, Bertrand P, Lanson Y. Prevalence and risk factors of urinary inconti-nence in young and middle-aged women. BJU Int 2002;89: 61-6.
26. Yu HJ, Chie WC, Chiu TY. Prevalence and risk factors of urinary incontinence in community-dwelling women in the Taipei area. J Urol (Taiwan) 1994;5:24-31.
27. Doughty DB. Urinary and fecal incontinence: nursing man-agement. 2nd ed. St. Louis, MO: Mosby Inc; 2000.
28. Arya LA, Myers DL, Jackson ND. Dietary caffeine intake and the risk for detrusor instability: a case-control study. Obstet Gynecol 2000;96:85-9.
29. Hannestad YS, Rortveit G, Daltveit AK, Hunskaar S. Are smoking and other factors associated with female urinary incontinence? The Norwegian EPINCONT Study. BJOG 2003;110:247-54.
30. Khullar V, Cardozo L. History and examination. In: Cardozo L, Staskin DJ, editors. Textbook of female urology and urogyne-cology. London: Isis Medical Media Ltd; 2001. p. 153-65. 31. Hart KJ, Palmer MH, Fitzgerald S. Perceived causes of
urinary incontinence and reporting: a study with working women. Clin Nurs Res 1999;8:84-92.
32. Hunskaar S, Burgio K, Diokno AC, Herzog AR, Hjalmas K, Lapitan MC. Epidemiology and natural history of urinary incontinence in women. Urology 2003;62:16-23.
33. Kirkland VL, Palmer MH, Fitzgerald ST. Incontinence in a manufacturing setting: women’s perceptions and responses. Public Health Nurs 2001;18:312-7.
34. Nygaard I, Linder M. Thirst at work. Int Urogynecol J Pelvic Floor Dysfunct 1997;8:340-3.
35. Lynn MR. Determination and quantification of content validity. Nurs Res 1986;35:382-5.
36. Chiarelli P, Brown W, McElduff P. Leaking urine: preva-lence and associated factors in Australian women. Neurourol Urodyn 1999;18:567-77.
37. Bullinger M, Alonso J, Apolone G, Leplege A, Sullivan M, Wood-Dauphinee S, et al. Translating health status
question-naires and evaluating their quality: the IQOLA project approach. J Clin Epidemiol 1998;51:913-23.
38. Behling O, Law KS. Translating questionnaires and other research instruments: problems and solutions. London: Sage publications; 2000.
39. Damrosch SP. Ensuring anonymity by use of subject-generated identification codes. Res Nurs Health 1986;9:61-3.
40. Pedhazur EJ, Schmelkin LP. Measurement, design, and analysis: An integrated approach. Hillsdale, NJ: Lawrence Erlbaum Associates Publishers; 1991.
41. Polit DF, Beck CT. Nursing reserarch: principle and methods. 7th ed. New York, NY: Lippincott Williams & Wilkins; 2004. 42. Brink PJ, Wood MJ. Advanced design in nursing research.
London: SAGE Publications; 1998.
43. Chao C. Get to know coffee. Newsletter of Mackay Memo-rial Hospital (Taiwan) 2001. Available at: http://www.tpa. edu.tw/department/medical.Accessed April 5, 2004. 44. Fultz NH, Herzog AR. Measuring urinary incontinence in
surveys. Gerontologist 1993;33:708-13.
45. Jackson S. Female urinary—symptom evaluation and diag-nosis. Eur Urol 1997;32:20-4.
46. Gordon D, Groutz A. Evaluation of female lower urinary tract symptoms: overview and update. Curr Opin Obstet Gynecol 2001;13:521-7.
47. DeVellis RF. Scale development: Theory and application. Newbury Park, CA: Sage Publication; 1991.
48. McDowell I, Newell C. Measuring health: A guide to rating scales and questionnaires. New York, NY: Oxford Univer-sity Press; 1996.