行政院國家科學委員會專題研究計畫 成果報告
皮質醇同型受體表現對於急性淋巴型白血病化療反應之影
響及其對策
計畫類別: 個別型計畫 計畫編號: NSC93-2314-B-002-206- 執行期間: 93 年 08 月 01 日至 94 年 07 月 31 日 執行單位: 國立臺灣大學醫學院小兒科 計畫主持人: 林凱信 共同主持人: 盧孟佑 報告類型: 精簡報告 處理方式: 本計畫可公開查詢中 華 民 國 94 年 10 月 30 日
行政院國家科學委員會
專題研究計畫研究成果報告
*********************************** *計畫名稱
* *
皮質醇同型受體表現對於急性淋巴型白血病化療反應及其對策
* ** ***********************************
計畫編號:NSC 93-2314-B-002-206
研 究 期 間 :九十三年八月一日至九十四年七月底止
執 行 單 位:臺大醫院小兒部
中華民國 94 年 10 月 30 日
一、中文摘要 急性淋巴性白血病是兒童癌症中最常見的惡性疾病,需要進行多重藥物的化 學治療,其中皮質醇是急性淋巴性白血病化學治療藥物中的一個重要的基本藥 物。根據以往的報告,對皮質醇單獨治療反應不佳的病人,常伴隨有引導期化療 失敗和預後不好。但皮質醇如何影響治療成績的機制則還不清楚。皮質醇受體的 表現在許多研究報告中被證實與皮質醇的感受性有關,其中皮質醇同型受體 GRα、GRβ 被證實與皮質醇的作用與拮抗作用相關。本實驗收集了 35 位新發病 急性淋巴性白血病病童的骨髓檢體,利用real time PCR 方法定量其白血病細胞 的GRα、GRβ 量。發現各危險群的急性淋巴性白血病童的 GRα、GRβ 量與比率 並無差異。比較臨床上對皮質醇單獨治療反應、引導期化療反應、復發,發現 GRα、GRβ、GRα/GRβ 量高低對臨床治療反應的指標均無影響,這顯示皮質醇 同型受體可能不是影響治療成績的主要機制。 關鍵詞: 急性淋巴性白血病、皮質醇同型受體
Abstract
Acute leukemia is the most common childhood malignancy worldwide, and acute lymphoblastic leukemia (ALL) comprises the majority of pediatric leukemia. It is well known that the overall prognosis is dependent on the appropriate risk-specific chemotherapy. Glucocorticoids (GC) have long been the cornerstone of ALL
chemotherapy. A better in vivo response to the initial 7 day prednisolone monotherapy had correlated to a significantly higher probability of both complete remission and long-term event free survival (EFS). Unsatisfactory response to GC has led to the failure of remission induction, and their survival is adversely affected. Glucocorticoid receptor(GR) expression has long been correlated with GC sensitivity in numerous experimental systems. Previous studies have suggested that GR-β is a dominant negative inhibitor, and down-regulation of GR-α or up-regulation of GR-β could result in GC resistance. Our aim is to determine which mRNA transcript is the one which accounts for GC resistance.
We collected 35 bone marrow samples from fresh ALL patients. Our results show the relative expression of GRα、GRβ、GRα/GRβ shows no difference in the 3 risk groups. The relative expression of GRα、GRβ、GRα/GRβ shows no difference between the PGR and PPR patients of the 3 risk groups. Furthermore, when they were divided into two groups ( high and low) according to the median value of the
GRα/GRβ ratio. The prednisolone response, induction remission rate and relapse rate show no difference in the two groups.
二、計畫緣由與目的:
Acute leukemia is the most common childhood malignancy worldwide, and acute lymphoblastic leukemia (ALL) comprises the majority of pediatric leukemia. It is well known that the overall prognosis is dependent on the appropriate risk-specific
chemotherapy.
Glucocorticoids (GC) have long been the cornerstone of ALL chemotherapy, and it exerts anti-leukemic action via apoptosis induction and/or cell cycle arrest. Although widely used in numerous diseases from ALL to asthma, much is to be discovered about the mechanism how glucocorticoid works.
GC induced partial and complete responses in 80% of initial ALL (iALL) patients, but the response rate decreased dramatically to 35% in relapsed ALL (rALL).
Unsatisfactory response to GC has led to the failure of remission induction in both groups of patients, and their survival is adversely affected. Furthermore, a better in vivo response to the initial 7 day prednisolone monotherapy had correlated to a significantly higher probability of both complete remission and long-term event free survival (EFS).1
Any alteration from the pre-receptor phase such as mdr-1 gene overexpression to the execution phase like caspase activation could lead to resistance to glucocorticoid. After numerous studies in the past decades, most evidences have pointed to a pivotal role of glucocorticoid receptor (GR).
At the receptor level, GC resistance could occur either quantitatively or qualitatively. As for the latter, nuclear translocation and ligand binding affinity/stability (either primary or secondarily modified) could all be possible. It has been demonstrated that there was no correlation between the extent of nuclear translocation of the activated GR and the clinical response to GC in ALL.2
GR expression have long been correlated with GC sensitivity in numerous experimental systems,3,4 and there is evidence that basal GR levels in certain
childhood ALL predicted the in vivo response to single agent GC before combination CT.5 An in vitro drug sensitivity assay, the MTT assay, showed a positive association of in vitro GC sensitivity to long-term outcome in a small group of patients.6 Although there is a strong correlation between GR concentration and GC sensitivity in cell line experiments, in vivo studies yielded contradictory results.7,8,9 One large clinical study
on 546 ALL patients with long term follow up has concluded that the expression level of GR protein was an important and independent prognostic factor, but only in pre-B and early pre-B ALL.8 Sequential comparison of GR levels in iALL and rALL has also been performed, and no significant difference was found.10
GR expression could be either up- or down-regulated by the presence of GC, depending on cell type. In a T-cell lineage ALL (T-ALL) cell line model, there was up-regulation of GR after in vitro exposure to dexamethasone.11 It is well known that T-ALL is more resistant to chemotherapy, and although it is not necessarily
attributable to GR, no good explanation has been found so far.
Promoter preference and alternative splicing of GR mRNA result in different
transcripts, and there are at least five different GR protein isoforms. Previous studies have suggested that GR-β is a dominant negative inhibitor, and down-regulation of GR-α or up-regulation of GR-β could result in GC resistance.12 In the only study to date, decreased GR α/β ratio in T-ALL may be one of the mechanisms for the reduced GC sensitivity.13 However, the role of GR-β as a major determinant in GC resistance is not substantiated by other studies,14 and overexpression of GR-β has failed to repress the transcriptional activation by GR-α in a transfection model.15
We here propose that the answer to the aforementioned controversy may be that it is the successful positive auto-induction of GR protein (but not the basal level) which is required for the GC-induced apoptosis. This would explain the discordance observed between basal GR levels and clinical responses. The discrepancy in inducible GR expression might be mediated through alterative promoter use, or different mRNA transcripts.
Alternatively, the relative level of certain protein isoform(s) to that of GR-α may affect the responsiveness to GC without altering the amount of total GR, though the precise regulatory mechanism is also unknown. The protein expression may be controlled by the relative (or absolute) amount of different mRNAs transcripts, supported by a recent in vivo study on multiple myeloma and other hematological malignancies.24 Some evidence has shown that to trigger an irreversible process of apoptosis, certain amount of GR (per cell) must be achieved, but the cutoff level varied greatly between studies, ranging from 4000 to 16000 receptors/cell.2,16 This discrepancy may be explained by isoform expression as well.
group of NF-kB regulated proteins.17 No studies to date have been published that investigate the link between IAP expression and GC resistance. Here we will use IAPs as an index of a cell’s anti-apoptotic function. Presumably only when the GC-induced apoptotic signal exceeds the anti-apoptotic signal does a cell initiates the irreversible cell death.
Our first aim is to determine which mRNA transcript is the one which accounts for
GC resistance. The in vivo response to the 7 days’ prednisolone monotherapy would be the most direct index of GC resistance. Prednisone good response (PGR) was defined as a blast count of less than 1,000/microL and a prednisone poor response (PPR) as a blast count of at least 1,000/microL, both in peripheral smears, after 7 days of oral prednisone (60 mg/m2 per day) and one intrathecal dose of methotrexate.The response .while the result of chemotherapeutic induction, relapse rate will all be traced for comparison. The mRNA which contributes most to the inducible GR protein would most likely be the target of therapeutic manipulation. There is so far no published data linking these splice variants to GC sensitivity in clinical studies. 三、結果與討論
Patient samples:本計畫一年來收集了 35 位新發病急性淋巴性白血病病童的
骨髓檢體,依TPOG ALL 治療計畫分成 standard risk(SR)、high risk(HR)、very high
risk(VHR)三組,病童之診斷和基本資料列在表一。
Quantitative RT-PCR (Reverse Transcription-Polymerase Chain Reaction) by TaqMan Method::Total RNA was extracted from cell pellets of patients’ leukemic blasts, according to manufacturer’s instructions, followed by cDNA synthesis with random hexamers. PCR reactions were performed using the primers : GRα ( forward: 5’-CTATGCATGAAGTGGTTGAAAA-3’; reverse: 5’- TTTCAGCTAACATCT CGGG-3’), generating PCR products of 96bp; GRβ ( forward: 5’-GAAGGAAACT CCAGCCAGAA-3’; reverse: 5’-CCACATAACTTTTCATG CCAGAA-3’),
generating PCR products of 264bp. The TaqMan probes for GRα (5’-CGAGCTGAAGCAGATGCAGGACAAGTAC-3’) and GRβ
(5’-CGAGCTGAAGCAGATGCAGGACAAGTAC) were labeled at 5’ end with reporter dye molecule. The PCR primers and the target probe for GAPDH were purchased from ABI as a kit of TaqMan GAPDH control reagent kit.
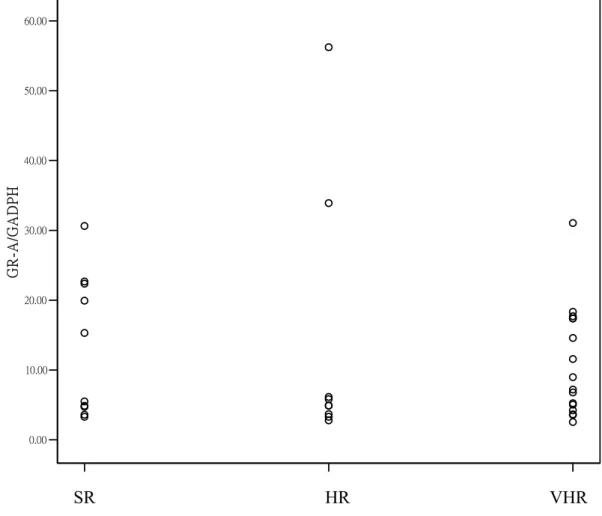
Expression of GR gene in leukemic blasts:Figure 1 shows the relative mRNA levels in primary leukemia blasts from patients. The relative expression of GRα、 GRβ、GRα/GRβ shows no difference in the 3 risk groups.
Expression of GR genes and response of leukemic blasts to prednisolone
poor response patients. The relative expression of GRα、GRβ、GRα/GRβ shows no difference between the PGR and PPR patients of the 3 risk groups.
Furthermore, when they were divided into two groups ( high and low) according to the median value of the GRα/GRβ ratio. The prednisolone response, induction remission rate and relapse rate show no difference in the two groups (table 2). Discussion
Glucocorticoid- sensitivity of leukemic blasts has been demonstrated in some studies to be prognostic factor in childhood ALL. Despite the extensive use of glucocorticoids in treatment for childhood ALL for decades, little is known about the molecular mechanisms of glucocorticoid sensitivity/resistence of leukemic blast. Several slicing variants are generated from the GR gene. GRα is a functionally active receptor, and the GRβmay have a dominant negative effect on GRα. These isoforms were reported to play a role in the occurrence of glucocorticoid resistance in tumor cells. Some studies demonstrated that in vitro glucocorticoid sensitivity of ALL blasts is correlated with the ratio of GRα/GRβ. But our studydid not show any association between the in vivo prednisolone response and the ratio of GRα/GRβ.
四、計畫成果自評:
本計畫收案35 位,追蹤時間約 30 月,其中只有 8 位復發。可能因為個案數
太少、追蹤時間不夠久,導致分析結果不明顯。另外有些檢體因存放年代較久, RNA 的品質較差,無法分析或 real-time PCR 品質不良而放棄。不過就本實驗結 果GC isoform 對 in vivo 的 prednisolone response 不像 in vitro 的 cytotoxic assay
Figure 1 Relative mRNA levels of GRα、GRβ and GRα/GRβ in primary leukemia blasts from ALL patients.
0.00 10.00 20.00 30.00 40.00 50.00 60.00 GR-A/GADPH SR HR VHR
0.00 0.10 0.20 0.30 0.40 0.50 0.60 0.70 GR-B/GAD PH SR HR VHR
0.00 0.01 0.02 0.03 0.04 0.05 0.06 B/A SR HR VHR
Table 1 The basic characteristics of patients Number Age Median [min, max] Gender [M/F] Duration of follow up(mon) Prednisolone response [GPR/PPR] Induction remission Relapse SR 10 4.49 [2.61;9.31] 5/5 42.1 [10.5;57.3] 10/0 10/10 0 HR 9 3.78 [1.59;14.23] 4/5 24.6 [9.5;44.4] 7/2 9/9 3 VHR 16 6.08 [0.72;12.13] 7/9 31.5 [4.7;57.9] 10/5 14/15 6 total 35 4.66 [0.72;14.23] 16/19 31.5 [4.7;57.9] 27/7 33/34 9
Table 2 The prednisolone response, induction remission and relapse rate in the high and low GRα/GRβ groups
Number Prednisolone response [GPR/PPR] Induction remission Relapse High 18 15/3 18/18 6 Low 17 13/4 15/16 3
五、參考文獻
1. Riehm H, et al. Corticosteroid-dependent reduction of leukocyte count in blood as a prognostic factor in acute lymphoblastic leukemia cell in childhood. Klinische Padiatrie 1987;199:151-160. 2. Costlow ME, et al. Glucocorticoid receptor in childhood acute lymphoblastic leukemia. Cancer Research 1982;42:4801-4806.
3. Reichardt HM, et al. Mice with an increased glucocorticoid receptor gene dosage showed enhanced resistance to stress and endotoxic shock. Molecular and Cellular Biology 2000;20:9009-9017. 4. Lippman M, et al. Glucocorticoid binding proteins in human leukaemic lymphoblasts. Nature New Biology 1973;242:157-158.
5. Pui CH, et al. The relationship of blast cell glucocorticoid receptor levels to response to single-agent steroid trial and remission response in children with acute lymphoblastic leukemia. Leukemia Research 1984;8:579-585.
6. Pieters Receptor, et al. Relation of cellular drug resistance to long-term clinical outcome in childhood acute lymphoblastic leukemia. Lancet 1991;338:399.
7. Weiss C, et al. Prognostic significance of glucocorticoid receptor determination in patients with chronic lymphocytic leukemia and immunocytoma: lack of a positive correlation between receptor levels and clinical responsiveness. Leukemia Research 1990;14:327-332.
8. Kato GJ, et al. High glucocorticoid receptor content of leukemic blasts is a favorable prognostic factor in childhood acute lymphoblastic leukemia. Blood 1993;82(8):2304-2309.
9. Iacobelli S, et al. glucocorticoid receptors predict response to combination chemotherapy in patients with acute lymphoblastic leukemia. Oncology (Basel) 1987;44:13-16.
10. Pui CH, et al. Sequential studies of lymphoblast glucocorticoid receptor levels at diagnosis and relapse in childhood leukemia: an update. Leukemia Research 1986;10:227-29.
11. Tonko M, et al. Gene expression profiles of proliferating vs. G1/G0 arrested human leukemia cells suggest a mechanism for glucocorticoid-induced apoptosis. FASEB 2001;15:693-699.
12. Gagliardo R, et al. Is there a role for glucocorticoid receptor beta in asthma? Respir Res 2001;2:1-4. 13. Longui CA, et al. Low glucocorticoid receptor alpha/beta ratio in T-cell lymphoblastic leukemia. Hormone and Metabolic Research 2000;32:401-406.
14. Csoka M, et al. Glucocorticoid-induced apoptosis and treatment sensitivity in acute lymphoblastic leukemia of children. Pediatric Hematology and Oncology 1997;14:433-442.
15. de Lange, et al. Natural variants of the β isoform of the human glucocorticoid receptor do not alter sensitivity to glucocorticoids. Molecular and Cellular Endocrinology 1999;153:163-168.
16. Mastrangelo R, et al. Clinical implication of glucocorticoid receptor studies in childhood acute lymphoblastic leukemia. Blood 1980;56:1036-1040.
17. Yang Y, et al. Thymocyte apoptosis. Journal of Clinical Immunology. 1999;19:337-349.
18. Barrett TJ, et al. Coordinate regulation of glucocorticoid receptor and c-jun gene expression is cell type-specific and exhibits differential hormonal sensitivity for down- and up-regulation. Biochemistry
1996;35:9746-9753.
19. Ramdas J, et al. Glucocorticoid-induced cell death requires autoinduction of glucocorticoid receptor expression in human leukemic T cells. Cancer Research 1999;59:1378-1385.
20. Pedersen KB, et al. Quantification and glucocorticoid regulation of glucocorticoid receptor transcripts in two human leukemic cell lines. Biochemistry 2003;42:10978-10990.
21. Pardi R, et al. In vivo effects of a single infusion of theophylline on human peripheral blood lymphocytes. Clin Exp Immunol 1984;57:722.
22. Winoto A, et al. Nuclear hormone receptors in T lymphocytes. Cell 2002;109:S57-S66. 23. Haarman EG, et al. In vitro Glucocorticoid resistance in childhood leukemia correlates with receptor affinity determined at 37∘C, but not with affinity determined at room temperature. Leukemia 2002; 16:1882-1884.
24. de Lange P, et al. Expression in hematological malignancies of a glucocorticoid receptor splice variant that augments glucocorticoid receptor-mediated effects in transfected cells. Cancer Research 2001;61:3937-3941.
25. Gametchu B, et al. Correlation of membrane glucocorticoid receptor levels with
glucocorticoid-induced apoptosis competence using mutant leukemic and lymphoma cell lines. J Cell Biochem 2002;87(2):133-146.
![Table 1 The basic characteristics of patients Number Age Median [min, max] Gender[M/F] Duration of follow up(mon) Prednisolone response [GPR/PPR] Induction remission Relapse SR 10 4.49 [2.61;9.31] 5/5 42.1 [10.5;57.3] 10/0 10/10 0 HR 9 3](https://thumb-ap.123doks.com/thumbv2/9libinfo/8839762.238515/12.892.129.798.160.398/characteristics-patients-duration-prednisolone-response-induction-remission-relapse.webp)