Increased Risk of Dementia in Patients with Chronic Obstructive Pulmonary Disease
Kuang-Ming Liao, MD, MS,1,2 Chung-Han Ho, PhD3,4 Shian-Chin Ko5 and Chung-Yi Li,
PhD6,7
1. Department of Internal Medicine, Chi Mei Medical Center, Chiali, Tainan, Taiwan 2. Institute of Clinical Pharmacy and Pharmaceutical Sciences, National Cheng Kung University, Tainan, Taiwan
3. Department of Medical Research, Chi Mei Medical Center, Tainan, Taiwan
4. Department of Hospital and Health Care Administration, Chia Nan University of Pharmacy and Science, Tainan, Taiwan
5. Department of Chest Medicine, Chi Mei Medical Center, Tainan, Taiwan
6. Department of Public Health, College of Medicine, National Cheng Kung University, Tainan, Taiwan
7. Department of Public Health, College of Public Health, China Medical University, Taichung, Taiwan
Kuang-Ming LIAO: abc8870@yahoo.com.tw Chung-Han Ho: ho.c.hank@gmail.com Shian-Chin Ko: sc.ko@msa.hinet.net Chung-Yi Li: cyli99@mail.ncku.edu.tw
Corresponding author: Chung-Yi Li
Address: No. 138, Shengli Rd., North Dist., Tainan City 704, Taiwan (R.O.C.) Telephone number: + +886-6-2353535 ext.5862 or 5863
Fax number: +886-6-2359033 Email: cyli99@mail.ncku.edu.tw
Abbreviations: COPD = chronic obstructive pulmonary disease; AD = Alzheimer’s disease PD = Parkinson’s disease; NHI = National Health Insurance; NHIRD = National Health Insurance Research Database; IRR = incidence rate ratio; HR = hazard ration; CI = confidence interval; OR = odds ratio.
Kuang-Ming Liao: reviewing the literature and drafting the manuscript; Chung-Han Ho: acquiring and analyzing the data; Shian-Chin Ko: interpretation of the data; Chung-Yi Li: revising the manuscript. All authors have read and approved the final manuscript being submitted.
Abstract
Background: Neurodegenerative disease in patients with chronic obstructive pulmonary
disease (COPD) was observed. We aim to clarify the risk of dementia in patients with COPD.
Methods: The study used claims data from Taiwan’s National Health Insurance Research
Database. Subjects were those who received a discharge diagnosis of COPD between January 1, 2002 and December 31, 2011. Only the first hospitalization was enrolled, and the index date was the first day of admission. Patients younger than 40 years or those with a history of Alzheimer’s disease (AD) or Parkinson’s disease (PD) before the index date were excluded. The patients with COPD were then followed until receiving a diagnosis of AD or PD, death, or the end of the study. Control subjects were selected from hospitalized patients without a history of COPD, AD or PD and were matched according to age (±3 years), gender and the year of admission at a 2:1 ratio. The comorbidities were measured from 1 year before the index date based on the ICD-9-CM codes.
Results: The study included 8,640 patients with COPD and a mean age of 68.76 (± 10.74 )
years. The adjusted hazard ratio of developing dementia (AD or PD) was 1.74 (95% confidence interval = 1.55-1.96) in patients with COPD compared with patients without COPD after adjusting for age, gender and comorbidities.
Conclusions: This nationwide cohort study demonstrates that the risk of dementia, including
AD and PD, is significantly increased in patients with COPD compared with individuals in the general population.
Keywords: Alzheimer’s disease; chronic obstructive pulmonary disease; dementia; National
Introduction
Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory disease characterized by airflow restriction.1 Many studies have showed that cognitive function is
impaired in patients with COPD with or without hypoxemia.2,3 Cerebral disturbance is noted
in patients with COPD and may be related to hypoxia in the brain.3
Dementia is a broad category of brain diseases. The most common type of dementia is Alzheimer's disease (AD) and Parkinson's disease (PD) is the second most common neurodegenerative disorder, 4 after Alzheimer's disease. Other types include vascular
dementia, dementia with Lewy bodies, frontotemporal dementia, Creutzfeldt-Jakob disease, normal pressure hydrocephalus, Huntington's Disease and mixed dementia.
Cytokines and inflammatory may play an important role in promoting the degenerative processes involved in a wide variety of cognitive disorders, including AD and PD. In many disease, inflammation is a marker of tissue damage, and may either occur after tissue damage in neurodegenerative diseases or serve as a marker of an immunological response.5 COPD is
a systemic inflammatory disease, and inflammation and cytokines may contribute to neuron damage and result in neurodegenerative disorders. Patients with COPD may have a higher risk of becoming AD or PD compared with that found in the general population. There has been only one nationwide retrospective cohort study,6 which indicated that PD risk is
increased in patients with COPD compared with those without COPD.
However, there has been no description in the literature of a relationship between COPD and dementia. We thereby aim to clarify the risk of developing AD or PD in patients with COPD using the nationwide database in Taiwan. Patinets with COPD without previous history of AD or PD and older than 40 years of age will be included in the study. Our study highlighted the important role of dementia in association with the patients with COPD in a wide range of conditions and irrespective of sex.
Methods
Source of Database
Taiwan launched a single-payer NHI program in March 1995. More than 99% of citizens are enrolled in the program. The NHI Research Database (NHIRD) is a medical claims database that was established and is used for research purposes. There are patients’ demographic characteristics, disease diagnoses, prescription records, and medical expenditures in the claim data. Approximately 99% of the total population in Taiwan is enrolled in the NHI Program.7 In this study, we retrieved our study sample from 1 million
beneficiaries randomly sampled from all beneficiaries registered in 2000. All medical claims from January 1, 1997 to December 31, 2011 for those 1 million beneficiaries are available. Before the NHIRD released database to the researchers, the confidential data for individuals were scrambled and encrypted and informed consent forms were therefore waived by the Institutional Review Board.
Study design
This is a retrospective cohort design in which the eligible study subjects were patients who received a discharge diagnosis of COPD (ICD-9-CM codes: 490-492, 496) during a
hospitalization between January 1, 2002 and December 31, 2011. Only the first
hospitalization was enrolled. Control subjects were selected from hospitalized patients without COPD, AD or PD and were matched according to age (based on year of birth), gender and the year of admission at a 2:1 ratio. All patients with COPD were then considered if the first admission for COPD occurred between January 1, 2002 and December 31, 2011. The first date of admission is the index date. Patients younger than 40 years and those with a history of PD (ICD-9-CM = 332) or AD (ICD-9-CM = 331) before the index date were excluded. Patients in the study cohort were then followed to the end of 2011 to investigate the incidence of AD or PD. Comorbidities were evaluated from 1 year before the index day according to ICD-9-CM codes in outpatient and inpatient departments.
Statistical analysis
During the statistical analysis, we first described the demographic characteristics and comorbidities of the study patients. Student’s t-test was used to estimate the mean difference of the continuous variables, and Pearson’s Chi-square was applied to the categorical
variables. The incidence rate of dementia (AD or PD) was evaluated as the number of the patients with COPD and dementia divided by the total person-years, yielding rates per 10,000 person-years of observation. The incidence rate ratios (IRRs) of dementia were estimated under Poisson regression. Cox’s proportional hazard regression model with adjustment for potential confounders was used to assess the risk of dementia. The potential confounders included age, gender, urbanization, coronary artery disease, stroke, hyperlipidemia,
hypertension, diabetes, and head injury. Subjects who did not present AD or PD before the end of study period (i.e., December 31, 2011) were considered censored. We also performed Kaplan-Meier analysis to compare the cumulative incidence of dementia (AD or PD) in the patients with COPD and those without COPD. A P value of <0.05 was considered
statistically significant. All statistical analyses were performed using the Statistical Analysis Software (SAS) System, version 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
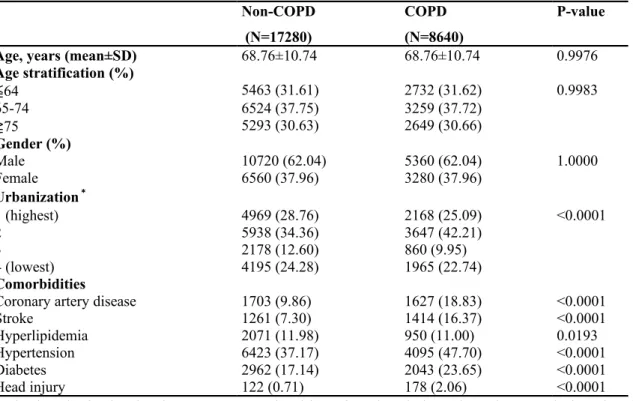
The cohort comprised 8,640 patients with COPD with first hospitalization records from 2002 to 2010. The mean age and corresponding standard deviation (SD) of the study population was 68.76 (± 10.74) years, and males were predominant (62.04%). More than 68% of patients were older than 65 years. Table 1 shows the distributions of demographic characteristics and cormobidities among the 8,640 patients with COPD.
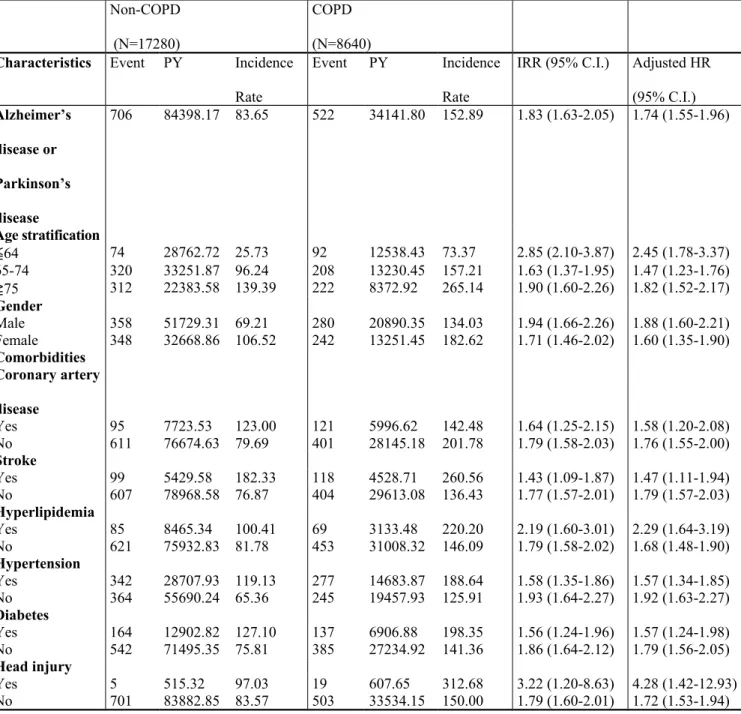
In this cohort, patients with COPD had a higher prevalence of coronary artery disease, stroke, hypertension, diabetes and head injury. The incidence rate of dementia (AD or PD) (per 10,000 person-years) and adjusted hazard ration (HR) between the patients with COPD and patients without COPD are present in Table 2. Patients with COPD had higher overall incidence rate of dementia than in the non-COPD group (152.89 vs. 83.65 per 10,000 person-years), with an IRR of 1.83 (95% confidence interval (CI) =1 .63-2.05). The adjusted HR of dementia in patients with COPD is 1.74 (95% CI = 1.55-1.96) compared with patients without COPD after adjusting for age, gender, coronary artery disease, stroke,
hyperlipidemia, hypertension, diabetes and head injury.
The incidence of dementia was higher in patients with COPD than in those without COPD, and the incidence rate of dementia increased with age in patients with and without COPD. Patients with COPD had a higher risk of dementia than did patients without COPD among patients younger than 65 years, with an IRR of 2.85 (95% CI = 2.10-3.87) and an adjusted HR of 2.45 (95% CI = 1.78-3.37). Among subjects older than 75 years of age, patients with COPD had a higher risk of dementia than did the patients without COPD, with an IRR of 1.90 (95% CI = 1.60-2.26) and an adjusted HR of 1.82 (95% CI = 1.52-2.17).
The incidence rate of dementia was higher in female patients with COPD than male patients with COPD (182.62 vs. 134.03 per 10,000 person-years).The adjusted HR of dementia observed in male patients with COPD in comparison with male patients without COPD was 1.88 (95% CI = 1.60-2.21). The adjusted HR of dementia observed in female patients with COPD in comparison with female patients without COPD was 1.60 (95% CI = 1.35-1.90).
Table 3 shows the incidence of dementia stratified by age, gender and medical conditions. The risk of dementia was significantly greater in male patients with COPD who were younger than 65 years of age, with IRR = 3.82 (95% CI = 2.55-5.71) and adjusted HR = 3.46 (95% CI = 2.27-5.25) compared with patients without COPD who were younger than 65 years of age.
Among patients age 75 and older, the adjusted HR of dementia was 2.05 (95% CI = 1.53-2.75) in male patients with COPD and 1.76 (95% CI = 1.41-2.20) in female patients with COPD compared with patients without COPD. Among patients with comorbidities who were younger than 65 years of age, the adjusted HR of dementia was 2.19 (95% CI = 1.42-3.39) in patients with COPD compared with patients without COPD.
Figure 1 shows the cumulative incidence of dementia in patients with COPD and those without COPD. The incidence of dementia (log-rank test, P<0.0001) was significantly difference in patients with COPD than in those without COPD.
Discussion Study strength
This is the first study to employ a nationwide, population-based, follow-up study design to explore the relationship between COPD and dementia. The overall incidence rate of dementia was 152.89 per 10,000 person-years and 74% higher in the patients with COPD than in the patients without COPD and an adjusted HR of 1.74 after adjusting for age, gender and medical comorbidities. COPD cohort had a higher risk of developing dementia than did non- COPD cohort.
Association between COPD and dementia
A population-based study used self-administered questionnaire in Eastern Finland8
showed that COPD (HR 1.85, 95% CI 1.05 – 3.28), asthma (HR 1.88, 95% CI 0.77 – 4.63) and both pulmonary diseases combined (HR 1.94, 95% CI 1.16 – 3.27) increased the risk of cognitive impairment. We have found similar results in our study and our diagnosis of COPD is made by a physician. The physician-diagnosed COPD were more accurate than the
information was inquired in the self-administered questionnaire. Another population-based cohort study found that COPD significantly increased the risk for mild cognitive impairment by 83% (hazard ratio, 1.83 [95% CI, 1.04-3.23]).9 They defined COPD as physician
diagnosed and did not base the definition of spirometry. The definition was similar in our study and pulmonary function test was also not available in our database. However, previous studies have shown that mild COPD is underdiagnosed in the population and physician-diagnosed COPD may overdiagnose COPD without the pulmonary function data.10-12 A
retrospective study revealed that the odds ratio (OR) for cognitive impairment was almost 2 times higher in patients with COPD than in those without COPD. The study also used
physician-diagnosed COPD cases identified by using the data source and followed by the electronic medical record review and not by spirometry.
Risk factors of dementia
Patients with COPD age older than 75 years had a higher incidence rate of dementia than did patients with COPD who were younger than 65 years of age. Age is a risk factor for dementia not only in the general population but also in the COPD patient population.
The comorbidity-specific incidence rate of dementia was higher in both the patients with and without COPD. Head trauma is one of the risk of PD and has been related to the pathogenesis of PD. The results of meta-analysis and system review show that a history of head trauma is implicated in developing PD.13Otherwise, there has been a identification of
the relationship between head injury and AD. Research has linked head injury to a greater risk of developing of AD;14 an animal study revealed that traumatic brain injury can hasten
the occurrence of extracellular Aβ aggregation in mice;15 and epidemiological studies show
that 30% of patients with brain injury have Aβ plaques and this is the mechanism of AD.16
Thus, head injury play an important role in the etiology of dementia. In our study, patients with COPD had a higher risk of dementia (adjusted HR: 4.28, 95% CI: 1.42-12.93) compared with the non-COPD cohort among individuals with a head injury.
Patients with COPD but without diabetes had a 79% high-risk of dementia in comparison with patients without COPD or diabetes. Patients with COPD and diabetes only had a 57% high-risk of dementia in comparison with patients without COPD but with diabetes. The relatioship between patients with PD and diabetes remains controversial.17 One study
demonstrated that diabetes may have a greater risk of developing AD.18 Another study found
that diabetes did not add to the risk of AD in a population study; however, diabetes may play an important role in developing AD in the absence of other known major AD risk factors.19 In
the study, patients with COPD and diabetes did not add to the risk of developing dementia compared with patients with COPD without diabetes, and this result was similar to that of a previous database study.6 It can be seen that the incidence of dementia increases with age in
patients with or without COPD. Among patients with COPD who were younger than 65 years of age, the adjusted HR of dementia is 2.45 compared with patients without COPD. Among patients with COPD who reach age 75 and over, the adjusted HR of dementia is 1.82 compared with patients without COPD. COPD increases the risk of developing dementia in younger populations (under 65 years old); this effect was observed in the male population but was not found in the female population after age stratification.
Mechanisms contributing to dementia
COPD is a chronic and systemic inflammatory disease and the inflammatory markers have been associated with cognitive impairment and dementia.20,21 COPD is also associated with
an increased risk for cardiovascular disease and this one of the mechanisms contributing to dementia.22 The association between COPD and dementia still observed after adjustment for
vascular diseases, suggesting that COPD is an independent predictor of dementia.23
Patients with COPD have a higher chance of developing neuronal damage and the high risk is due to either hypoxia or associated comorbidities.Aging and the low cerebral perfusion are the key pathologic events associated with the development of dementia.9
Impact of dementia on the patients with COPD
In our study, patients with COPD and dementia, the incidence rate of severe sepsis and hospital mortality were higher than the patients with COPD without dementia. Dementia will increase the risk of severe sepsis with an adjusted OR of 1.38 (95% CI: 1.10-1.72) and hospital mortality with an adjusted OR 1.69 (95% CI: 1.18-2.43). Dementia also increased acute respiratory failure after adjusting for the confounding factors. Dementia is associated with an increased risk of adverse reactions, and cause an increase in mortality. Patients with COPD need to avoid smoking, manage health problems including diabetes, blood pressure, high cholesterol and intensive control the COPD to prevent dementia or delay its onset.
Limitations
The limitations of our study a lack of data on smoking status, the performance on a pulmonary function test and COPD severity in the database. The relationship between dementia and COPD severity needs to be further investigated. The present study is a nationwide cohort study, and we believe that the large number of participants and the comprehensive enrollment of patients with COPD in Taiwan ensure that the data are normally distributed and that the results are significant.
Patients with COPD have a high-risk of developing dementia compared with patients without COPD according to a nationwide cohort study, and COPD plays an import role in the development of dementia in male patients younger than 65 years of age.
References
1. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. GOLD Scientific Committee. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic
Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163:1256-1276.
2. Dodd JW, Getov SV, Jones PW. Cognitive function in COPD. Eur Respir J. 2010;35: 913-922.
3. Grant I, Heaton RK, McSweeny AJ, Adams KM, Timms RM. Neuropsychologic findings in hypoxemic chronic obstructive pulmonary disease. Arch Intern Med. 1982;142:1470-1476.
4. Nussbaum RL, Ellis CE. Alzheimer's disease and Parkinson's disease. N Engl J Med. 2003;348:1356-1364.
5. Greig NH, Mattson MP, Perry T, Chan SL, Giordano T, Sambamurti K, Rogers JT, Ovadia H, Lahiri DK. New therapeutic strategies and Drug candidates for
neurodegenerative diseases: p53 and TNF-alpha inhibitors, and GLP-1 receptor agonists. Ann N Y Acad Sci. 2004;1035:290-315.
6. Li CH, Chen WC, Liao WC, Tu CY, Lin CL, Sung FC, Chen CH, Hsu WH. The association between chronic obstructive pulmonary disease and Parkinson's disease: a nationwide population-based retrospective cohort study. Q J M. 2015;108:39-45 7. Chi NF, Chien L-N, Ku H-L, Hu CJ, Chiou HY. Alzheimer disease and risk of stroke:
A population-based cohort study. Neurology. 2013;80:705-717.
8. Rusanen M, Ngandu T, Laatikainen T, Tuomilehto J, Soininen H, Kivipelto M. Chronic obstructive pulmonary disease and asthma and the risk of mild cognitive impairment and dementia: a population based CAIDE study. Curr Alzheimer Res. 2013;10:549-555.
9. Singh B, Mielke MM, Parsaik AK, et al. A prospective study of chronic obstructive pulmonary disease and the risk for mild cognitive impairment. JAMA Neurol. 2014; 71:581-588.
10. Bednarek M, Maciejewski J, Wozniak M, Kuca P, Zielinski J. Prevalence, severity and underdiagnosis of COPD in the primary care setting. Thorax. 2008;63:402-407.
11. Prieto Centurion V, Huang F, Naureckas ET, et al. Confirmatory spirometry for adults hospitalized with a diagnosis of asthma or chronic obstructive pulmonary disease exacerbation. BMC Pulm Med. 2012;12:73-80.
12. Hnizdo E, Glindmeyer HW, Petsonk EL, Enright P, Buist AS. Case definitions for chronic obstructive pulmonary disease. COPD. 2006;3:95-100
13. Jafari S, Etminan M, Aminzadeh F, Samii A. Head injury and risk of Parkinson disease: a systematic review and meta-analysis. Mov Disord. 2013;28:1222-1229. 14. Sivanandam TM, Thakur MK. Traumatic brain injury: a risk factor for Alzheimer’s
disease. Neurosci Biobehav Rev. 2012;36:1376-1381.
15. Tajiri N, Kellogg SL, Shimizu T, Arendash GW, Borlongan CV. Traumatic brain injury precipitates cognitive impairment and extracellular Aβ aggregation in Alzheimer's disease transgenic mice. PLoS One. 2013;8:e78851.
16. Johnson VE, Stewart W, Smith DH. Traumatic brain injury and amyloid-β pathology: a link to Alzheimer’s disease? Nat Rev Neurosci. 2010;11: 361-370.
17. Schernhammer E, Hansen J, Rugbjerg K, Wermuth L, Ritz B. Diabetes and the risk of developing Parkinson’s disease in Denmark. Diabetes Care. 2011;34:1102-1108. 18. Arvanitakis Z, Wilson RS, Bienias JL, Evans DA, Bennett DA. Diabetes mellitus and
risk of Alzheimer disease and decline in cognitive function. Arch Neurol. 2004;61:661-666.
19. Akomolafe A, Beiser A, Meigs JB et al. Diabetes mellitus and risk of developing Alzheimer disease: results from the Framingham Study. Arch Neurol. 2006;63:1551-1555.
20. Roberts RO, Geda YE, Knopman DS, et al. Association of C-reactive protein with mild cognitive impairment. Alzheimers Dement. 2009;5:398-405.
21. Roberts RO, Geda YE, Knopman DS, et al. Metabolic syndrome, inflammation, and nonamnestic mild cognitive impairment in older persons: a population-based study. Alzheimer Dis Assoc Disord. 2010;24:11-18.
22. Wysocki M, Luo X, Schmeidler J, et al. Hypertension is associated with cognitive decline in elderly people at high risk for dementia. Am J Geriatr Psychiatry.
2012;20:179-187.
23. de la Torre JC. Critical threshold cerebral hypoperfusion causes Alzheimer's disease?
Figure legend
Figure 1. Cumulative incidence of dementia in patients with chronic obstructive pulmonary
Table 1. Demographic characteristics and comorbidities in patients with and without chronic
obstructive pulmonary disease
Non-COPD (N=17280)
COPD (N=8640)
P-value
Age, years (mean±SD) 68.76±10.74 68.76±10.74 0.9976
Age stratification (%) ≦64 5463 (31.61) 2732 (31.62) 0.9983 65-74 6524 (37.75) 3259 (37.72) ≧75 5293 (30.63) 2649 (30.66) Gender (%) Male 10720 (62.04) 5360 (62.04) 1.0000 Female 6560 (37.96) 3280 (37.96) Urbanization* 1 (highest) 4969 (28.76) 2168 (25.09) <0.0001 2 5938 (34.36) 3647 (42.21) 3 2178 (12.60) 860 (9.95) 4 (lowest) 4195 (24.28) 1965 (22.74) Comorbidities
Coronary artery disease 1703 (9.86) 1627 (18.83) <0.0001
Stroke 1261 (7.30) 1414 (16.37) <0.0001
Hyperlipidemia 2071 (11.98) 950 (11.00) 0.0193
Hypertension 6423 (37.17) 4095 (47.70) <0.0001
Diabetes 2962 (17.14) 2043 (23.65) <0.0001
Head injury 122 (0.71) 178 (2.06) <0.0001
*The level of urbanization was categorized into four levels based on the population density of the subject’s area of residence, where ‘1’ was most urbanized and ‘4’ was least urbanized.
Table 2. Incidence of dementia in patients with/without chronic obstructive pulmonary disease. Non-COPD (N=17280) COPD (N=8640)
Characteristics Event PY Incidence
Rate
Event PY Incidence Rate
IRR (95% C.I.) Adjusted HR (95% C.I.) Alzheimer’s disease or Parkinson’s disease 706 84398.17 83.65 522 34141.80 152.89 1.83 (1.63-2.05) 1.74 (1.55-1.96) Age stratification ≦64 74 28762.72 25.73 92 12538.43 73.37 2.85 (2.10-3.87) 2.45 (1.78-3.37) 65-74 320 33251.87 96.24 208 13230.45 157.21 1.63 (1.37-1.95) 1.47 (1.23-1.76) ≧75 312 22383.58 139.39 222 8372.92 265.14 1.90 (1.60-2.26) 1.82 (1.52-2.17) Gender Male 358 51729.31 69.21 280 20890.35 134.03 1.94 (1.66-2.26) 1.88 (1.60-2.21) Female 348 32668.86 106.52 242 13251.45 182.62 1.71 (1.46-2.02) 1.60 (1.35-1.90) Comorbidities Coronary artery disease Yes 95 7723.53 123.00 121 5996.62 142.48 1.64 (1.25-2.15) 1.58 (1.20-2.08) No 611 76674.63 79.69 401 28145.18 201.78 1.79 (1.58-2.03) 1.76 (1.55-2.00) Stroke Yes 99 5429.58 182.33 118 4528.71 260.56 1.43 (1.09-1.87) 1.47 (1.11-1.94) No 607 78968.58 76.87 404 29613.08 136.43 1.77 (1.57-2.01) 1.79 (1.57-2.03) Hyperlipidemia Yes 85 8465.34 100.41 69 3133.48 220.20 2.19 (1.60-3.01) 2.29 (1.64-3.19) No 621 75932.83 81.78 453 31008.32 146.09 1.79 (1.58-2.02) 1.68 (1.48-1.90) Hypertension Yes 342 28707.93 119.13 277 14683.87 188.64 1.58 (1.35-1.86) 1.57 (1.34-1.85) No 364 55690.24 65.36 245 19457.93 125.91 1.93 (1.64-2.27) 1.92 (1.63-2.27) Diabetes Yes 164 12902.82 127.10 137 6906.88 198.35 1.56 (1.24-1.96) 1.57 (1.24-1.98) No 542 71495.35 75.81 385 27234.92 141.36 1.86 (1.64-2.12) 1.79 (1.56-2.05) Head injury Yes 5 515.32 97.03 19 607.65 312.68 3.22 (1.20-8.63) 4.28 (1.42-12.93) No 701 83882.85 83.57 503 33534.15 150.00 1.79 (1.60-2.01) 1.72 (1.53-1.94)
Table 3. Incidence of dementia stratified by sex, age and comorbidity, with the hazards ratio
for patients with chronic obstructive pulmonary disease compared with those without chronic obstructive pulmonary disease.
Non-COPD (N=17280) COPD (N=8640)
Characteristics Event PY Incidence
Rate
Event PY Incidence Rate
IRR (95% C.I.) Adjusted HR (95% C.I.) Male ≦64 38 19480.84 19.51 62 8329.31 74.44 3.82 (2.55-5.71) 3.46 (2.27-5.25) 65-74 210 23970.29 87.61 137 9430.56 145.27 1.66 (1.34-2.06) 1.52 (1.22-1.90) ≧75 110 8278.18 132.88 81 3130.48 258.75 1.95 (1.46-2.59) 2.05 (1.53-2.75) Female ≦64 36 9281.88 38.79 30 4209.12 71.27 1.84 (1.13-2.98) 1.50 (0.90-2.49) 65-74 110 9281.57 118.51 71 3799.89 186.85 1.58 (1.17-2.12) 1.36 (0.99-1.86) ≧75 202 14105.40 143.21 141 5242.43 268.96 1.88 (1.51-2.33) 1.76 (1.41-2.20) Comorbidities ≦64 36 8892.28 40.49 57 5788.12 98.48 2.43 (1.60-3.69) 2.19 (1.42-3.39) 65-74 217 16466.22 131.79 148 8063.12 183.55 1.39 (1.13-1.72) 1.28 (1.03-1.58) ≧75 194 12126.27 159.98 159 5843.75 272.09 1.70 (1.38-2.10) 1.66 (1.34-2.07)