Contents lists available atScienceDirect
Resuscitation
j o u r n a l h o m e p a g e :w w w . e l s e v i e r . c o m / l o c a t e / r e s u s c i t a t i o n
Clinical paper
Post-resuscitative clinical features in the first hour after achieving sustained
ROSC predict the duration of survival in children with non-traumatic
out-of-hospital cardiac arrest
夽
Yan-Ren Lin
a,c,∗, Chao-Jui Li
b, Tung-Kung Wu
c, Yu-Jun Chang
d,f, Shih-Chang Lai
a,c, Tzu-An Liu
g,
Ming-Hau Hsiao
a, Chu-Chung Chou
a,e, Chin-Fu Chang
aaDepartment of Emergency Medicine, Changhua Christian Hospital, Changhua, Taiwan
bDepartment of Emergency Medicine, Chang Gung Memorial Hospital, Kaohsiung Medical Center, Chang Gung University College of Medicine, Kaohsiung, Taiwan cDepartment of Biological Science and Technology and Institute of Biochemical Engineering, National Chiao Tung University, Hsinchu, Taiwan
dEpidemiology and Biostatistics Center, Changhua Christian Hospital, Changhua, Taiwan eInstitute of Medicine, Chungshan Medical University, Taichung, Taiwan
fInstitute of Environmental Medicine, China Medical University, Taichung, Taiwan
gInstitute of Cellular and System Medicine, National Health Research Institutes, Zhunan, Miaoli County, Taiwan
a r t i c l e i n f o
Article history:
Received 31 August 2009
Received in revised form 6 January 2010 Accepted 10 January 2010
Keywords:
Out-of-hospital cardiac arrest Return of spontaneous circulation Post-resuscitative
Cardiac output Children
a b s t r a c t
Aim of the study: Although sustained return of spontaneous circulation (ROSC) can be initially established after resuscitation from non-traumatic out-of-hospital cardiac arrest (OHCA) in some children, many of the children lose spontaneous circulation during hospital stay and do not survive to discharge. The aim of this study was to determine the clinical features during the first hour after ROSC that may predict survival to hospital discharge.
Methods: We retrospectively evaluated the medical records of 228 children who presented to the emer-gency department without spontaneous circulation following non-traumatic OHCA during the period January 1996 to December 2008. Among these children, 80 achieved sustained ROSC for at least 20 min. The post-resuscitative clinical features during the first hour after achieving sustained ROSC that correlated with survival, median duration of survival, and death were analyzed.
Results: Among the 80 children who achieved sustained ROSC for at least 20 min, 28 survived to hospital discharge and 6 had good neurologic outcomes (PCPC scale = 1 or 2). Post-resuscitative clinical features associated with survival included sinus cardiac rhythm (p = 0.012), normal heart rate (p = 0.008), normal blood pressure (p < 0.001), urine output > 1 ml/kg/h (p = 0.002), normal skin color (p = 0.016), lack of car-diopulmonary resuscitation (CPR)-induced rib fracture (p = 0.044), initial Glasgow Coma Scale score > 7 (p < 0.001), and duration of in-hospital CPR≤ 10 min (p < 0.001). Furthermore, these variables were also significantly associated with the duration of survival (all p < 0.05).
Conclusions: The most important predictors of survival to hospital discharge in children with OHCA who achieve sustained ROSC are a normal heart rate, normal blood pressure, and an initial urine out-put > 1 ml/kg/h.
© 2010 Elsevier Ireland Ltd. All rights reserved.
1. Introduction
Pediatric out-of-hospital cardiac arrest (OHCA) is rare and the rate of survival is very low.1–6 Although sustained return
of spontaneous circulation (ROSC) can be initially established
夽 A Spanish translated version of the abstract of this article appears as Appendix in the final online version atdoi:10.1016/j.resuscitation.2010.01.006.
∗ Corresponding author at: Department of Emergency Medicine, Changhua Chris-tian Hospital, 135 Nanshsiao Street, Changhua 500, Taiwan.
Tel.: +886 4 7238595x1374; fax: +886 4 7289233. E-mail address:h6213.lac@gmail.com(Y.-R. Lin).
after resuscitation from non-traumatic OHCA in up to 35% of children, the rate of survival to hospital discharge is only 6–12%, and only 2–4% of those children have good neurologic outcome.1,2 Some studies have shown that survival of
chil-dren with OHCA is associated with factors in the pre-hospital resuscitation period, such as whether the arrest was witnessed, initial cardiac rhythm, and bystander resuscitation.7–9 The
post-resuscitative clinical features that may be predictive of survival and duration of survival in children, however, have not been well addressed.
The aim of this study was to determine the clinical features dur-ing the first hour after ROSC that may predict survival in children with non-traumatic OHCA.
0300-9572/$ – see front matter © 2010 Elsevier Ireland Ltd. All rights reserved. doi:10.1016/j.resuscitation.2010.01.006
2. Methods
2.1. Study design
Children aged≤ 18 years who presented to the emergency department (ED) of either the Chang Gung Memorial Hospital or the Changhua Christian Hospital with OHCA of non-traumatic ori-gin during the period January 1996–December 2008 were included in this study. Patient characteristics and post-resuscitative clini-cal features that may be associated with the outcomes of children with OHCA were analyzed retrospectively. The study protocol was approved by the Institutional Review Boards of both hospitals. 2.2. Study setting and population
We retrospectively reviewed the medical records of 238 chil-dren aged≤ 18 years with non-traumatic OHCA who presented to the ED at the Chang Gung Memorial Hospital (CGMH) in southern Taiwan or the Changhua Christian Hospital (CCH) in central Taiwan. The CGMH is a 2500-bed medical center covering a population of 1,700,000 individuals, among whom 330,000 are children. The inci-dence of pediatric OHCA at that institution is 4.7/100,000. The CCH is a 2000-bed medical center covering a population of 1,500,000 individuals, among whom 330,000 are children. The incidence of pediatric OHCA at that institution is 4.5/100,000. Among the 238 children, 10 were brought to the CGMH (n = 4) or the CCH (n = 6)
without resuscitation attempts because of “do not resuscitate” orders and were declared dead on arrival. Data on these children were excluded from the analysis. Therefore, the study population comprised 228 children. All of the OHCA children were obtained from the database for tracking arrest without missing cases. None of the patients had spontaneous circulation upon arrival at the ED. The organization of local public emergency medical systems and the training of EMS personnel are similar in both southern and cen-tral Taiwan. Pre-hospital basic life support (BLS) provided by EMS personnel included chest compression, use of automated external defibrillator, and use of non-invasive ventilation, such as a Bag-Valve-Mask. The decision to stop resuscitation was made only by ED physicians after a detailed clinical assessment indicated that achieving successful resuscitation was not possible.
Patients in this study were divided into 8 major groups based on the possible etiology of the OHCA: (1) sudden infant death syndrome; (2) infections (including upper and lower respiratory tract infection, urinary tract infection, deep neck infection, and infective colitis); (3) cardiovascular diseases (including myocardi-tis, heart failure, and congenital heart diseases); (4) neurological disease (including status epilepticus, spontaneous intracranial hemorrhage, and hydrocephalus); (5) asphyxia (caused by acute or chronic respiratory failure, food bolus or foreign body airway obstruction); (6) malignancy; (7) intoxication (drug or substance overdose); and (8) idiopathic causes. Classification of etiology was based on a detailed history, clinical assessment, laboratory
investi-Table 1
Patient characteristics and factors associated with sustained ROSC in non-traumatic OHCA children.
Non-traumatic OHCA children (n = 228) No. (%) Sustained ROSC
Yes (n = 80) No (n = 148) p-value
Age (mean± SD) (y/o) 4.82± 5.42
Newborn 29 (12.7) 14 15 0.622 Infant 85 (37.3) 25 60 Toddler 36 (15.9) 16 20 Preschool 20 (8.7) 8 12 School 23 (10.3) 9 14 Adolescence 35 (15.1) 8 27 Sex Boy 123 (54) 47 76 0.289 Girl 105 (46) 33 72
Place of cardiac arresta
Home 185 (81) 55 130 0.011
Outside the home 43 (19) 25 18
Witnessed arresta
Yes 148 (64.9) 66 82 0.002
No 80 (35.1) 14 66
The period from scene to hospitala(min) 28.12± 19.54 (11)b 20.67± 13.23 34.28± 20.57 <0.001
Pre-hospital BLS durationa(mean± SD) (min) 14.10± 12.67 (9)b 10.22± 5.82 19.98± 16.61 0.005
Etiology
Sudden infant death syndrome 43 (19) 10 33 0.583
Infections 31 (13.5) 13 18 Cardiovascular diseases 23 (10.3) 10 13 Neurological diseases 29 (12.7) 14 15 Asphyxia 60 (26.2) 20 40 Malignancy 23 (10.3) 8 15 Intoxication 5 (2.4) 1 4 Idiopathic 14 (5.6) 4 10
Initial cardiac rhythma
Asystole 152 (66.7) 38 114 <0.001
PEA 42 (18.3) 18 24
VFc 34 (15.1) 24 10
Body weight (mean± SD) (kg) 17.51± 13.16 (12)b 16.24± 14.76 17.22± 15.69 0.824
In-hospital CPR durationa(mean± SD) (min) 33.36± 17.12 13.39± 8.56 38.57± 21.88 <0.001 aFactors associated with achieving sustained ROSC in the ED.
bNumber of patients with missing information. c VF includes patients with pulseless VT.
gations, and radiological examinations. Etiologies that were unclear were classified as idiopathic causes. In addition, children were also divided into 6 groups according to age: newborn (<1 month), infant (1–12 months), toddler (>12 months to 3 years), preschool (>3–5 years), school age (>5–12 years), and adolescent (>12–18 years). 2.3. Study protocol
Information relating to the pre-hospital phase of resuscitation and BLS, including location of cardiac arrest and the duration of pre-hospital CPR, was obtained from public EMS records and witness statements. Children with OHCA received in-hospital resuscitation according to the advanced pediatric life support (APLS) protocol in both centers. The protocols adhered to the pediatric Utstein reporting system.6 In this study, in-hospital CPR was defined as
resuscitation attempts performed in the ED. All treatments and decisions regarding the termination of resuscitation efforts were made at the discretion of the treating physician. Data on patient characteristics gathered from ED patient charts included initial vital signs, age, sex, initial cardiac rhythm on presentation to the ED, duration of in-hospital CPR, body weight, body temperature (mea-sured by an infrared ear thermometer), medications administered during CPR, the duration of in-hospital CPR, and clinical features during the post-resuscitation phase. In this study, the initial cardiac
rhythm on presentation to the ED was obtained from electrocardio-graphic monitor that had been recorded immediately upon arrival. The rhythms included ventricular fibrillation (VF), pulseless ven-tricular tachycardia, pulseless electrical activity (PEA), and asystole. In this study, VF includes patients with pulseless ventricular tachy-cardia. Sustained ROSC was defined as that which resulted in at least 20 min of ROSC.10
The duration of survival was defined as the period from the time the patient achieved sustained ROSC in the ED to death or discharge from hospital. The following post-resuscitative clinical features evaluated in this study had been monitored and recorded by ED physicians or nurses every 10–15 min during the first hour after children had achieved spontaneous circulation: (1) cardiac rhythm (sinus, ventricular, and junctional rhythms) and heart rate (normal, tachycardia, bradycardia). Ventricular rhythm included ventricular pre-mature contractions and idioventricular rhythm. These data were obtained from electrocardiograms. The domi-nant cardiac rhythm and heart rate during the post-resuscitative period in each child were chosen for analysis; (2) mean arterial blood pressure (MAP). In this study, normal blood pressure was defined in children with MAP values within the normal range for children of the same age; hypertension was defined in children with MAP values that were higher than the normal range for chil-dren of the same age; and hypotension was defined as MAP values
that were lower than the normal range for children of the same age. In patients with large variations in blood pressure readings, the dominant blood pressure was used for analysis; (3) skin color of the face and trunk (normal, pale, cyanotic); (4) urine output (>1, 1–0.5, <0.5 ml/kg/h) and color of urine (straw-yellow, dark, blood-tinged). These data were recorded from the urine drained from urinary catheters that had been inserted immediately after patients had achieved sustained ROSC. Urine drained from urinary catheters during catheterization was regarded as residual urine and was not considered post-resuscitative urine output. The color of the urine was determined after the initial urine had been dis-carded; (4) presence of rib fracture. The diagnosis of fracture was made by ED physicians or radiologists based on radiographic evi-dence on portable chest X-ray images that had been obtained in all children immediately after they had achieved sustained ROSC. Old rib fractures and those associated with possible child abuse were not included in this study; (5) the initial Glasgow Coma Scale (GCS) (>7, 7–4, 3). All verbal scores were graded as 1 because all patients had an artificial airway. The highest score during the first 1-h interval after achieving sustained ROSC was chosen for analy-sis; and (6) body temperature. Moreover, the mean blood pressures and heart rates were reported respectively in 4 time periods during their ED stay (≤15, 16–30, 31–45, 46–60 min) for analyzing the car-diac output in children who survived to discharge and in children who did not survive to discharge. The mean value would be chosen
when children who had more than one measured data in one time period.
The total amount of fluid (including crystalloid fluid, colloid fluid, and blood products) administered during in-hospital CPR (from the time patients arrived at the ED until they achieved sus-tained ROSC) was recorded and categorized as >61, 60–41, 40–21 and≤20 ml/kg.
Neurologic outcomes of children who survived to discharge were evaluated according to the Pediatric Cerebral Performance Category (PCPC) scale before cardiac arrest (baseline), at the time of discharge from the hospital, and at follow-up. The PCPC scale range from 1 (no disability) to 5 (coma or vegetative state). In this study, survivors were divided into 3 groups based on neurologic outcome: (1) good neurologic outcome (PCPC scale = 1 or 2); (2) neurologic outcome unchanged from baseline (no deterioration in PCPC scale categories); and (3) poor neurologic outcome (PCPC scale≥ 3). 2.4. Data analysis
Descriptive analyses of independent variables (age, sex, etiolo-gies of OHCA, pre-hospital information, duration of in-hospital CPR, medication dosage, post-resuscitative clinical features, and dura-tion of survival) are reported as percentages or mean± standard deviation (SD). Factors that may be associated with sustained ROSC and survival were analyzed by the by Mann–Whitney U
Table 2
Association between post-resuscitative clinical features during the first hour after achieving sustained ROSC and survival. Children who achieved sustained ROSC (n = 80)
Survived to discharge p-value
Success (n = 28) Failure (n = 52) Type of cardiac rhythma
Sinus rhythm 22 23 0.012
Ventricular rhythm 4 21
Junction rhythm 2 8
Hear ratea
Normal heart rate 13 10 0.008
Tachycardia 13 25
Bradycardia 2 17
Blood pressurea
Normal blood pressure 11 8 ≤0.001
Hypertension 13 11 Hypotension 4 33 Urine outputa >1 ml/kg/h 13 8 0.002 1–0.5 ml/kg/h 12 21 <0.5 ml/kg/h 3 23
CPR-induced rib fracturea
Yes 2 13 0.044 No 26 39 Color of urine Straw-yellow 11 27 0.531 Dark 11 15 Blood-tinged 6 10 Color of skina Normal 13 13 0.016 Pale 12 18 Cyanotic 3 21 Initial GCSa >7 13 2 <0.001 7–4 9 30 3 6 20
Number of epinephrine injections (mean± SD) 4.92± 3.76 9.46± 5.83 0.582
Epinephrine total dose (mean± SD) (mg/kg) 0.32± 0.25 0.42± 0.41 0.884
Body temperature (mean± SD) (◦C) 35.87± 2.15 34.77± 1.78 0.952
Duration of in-hospital CPRa(mean± SD) (min) 9.57± 13.63 14.37± 12.76 <0.001 aFactors associated with survival.
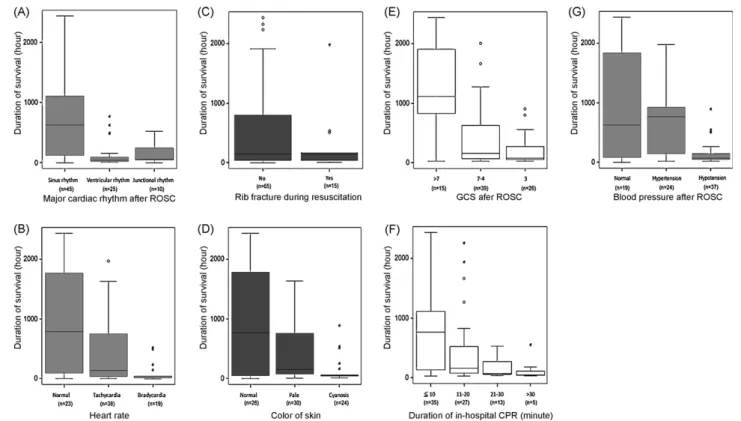
Fig. 2. Post-resuscitative clinical features in the first hour after achieving sustained ROSC associated the durations of survival in non-traumatic OHCA children. (A) The major type of cardiac rhythm; (B) heart rate; (C) rib fracture caused by CPR; (D) the color of skin; (E) initial GCS; (F) the duration of in-hospital CPR; (G) the blood pressure (analyzed by non-parametric test and all p < 0.05).
test, Fisher’s exact test, or Chi-Square test. Relationships between post-resuscitative clinical features of patients and duration of sur-vival were analyzed by a non-parametric test (Mann–Whitney U test or Kruskal–Wallis test) and the results are reported as a box plot. Multiple logistic regression analysis was used to analyze the relationship between survival and rib fracture after adjusting for duration of CPR. A p-value < 0.05 was considered to be statistically significant. All analyses were performed using SPSS software ver-sion 15.0 (SPSS Inc., Chicago, IL).
3. Results
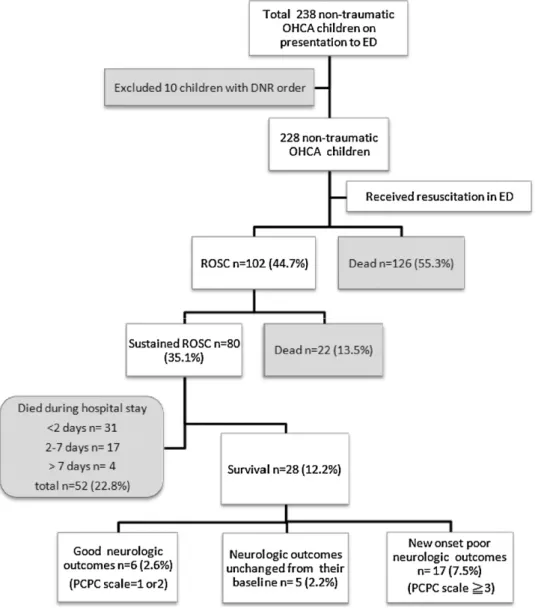
3.1. Patient characteristics and factors related to sustained ROSC Data on 228 children with OHCA of non-traumatic origin were analyzed. Patient characteristics are presented inTable 1. Among the 228 patients, sustained ROSC was achieved in 80 children. The overall mortality rate was 87.8%. A total of 28 patients survived to discharge. Among them, 6 had good neurologic outcomes and 17 had poor neurologic outcomes (Fig. 1). The factors that were positively associated with achieving sustained ROSC in the ED are also shown inTable 1.
3.2. Clinical features during the first hour after achieving sustained ROSC
Among the 80 children who achieved sustained ROSC, only one died in the ED within the first hour. The mean duration of ED stay was 1.62± 0.43 h. During the first hour after achieving sustained ROSC, the major type of cardiac rhythm was sinus rhythm (56.3%) followed by ventricular rhythm (31.3%) and junctional rhythm (12.4%). The most common heart rate was tachycardia (47.5%) fol-lowed by normal heart rate (28.8%) and bradycardia (23.7%). The
most common blood pressure status was hypotension (46.3%). Most of the children (41.3%) had a urine output of 0.5–1 ml/kg/h, and the most common color of urine was straw-yellow. Fifteen (18.8%) children had CPR-induced rib fracture. Thirty (37.5%) children had pale skin color and 24 (30%) were cyanotic after achieving sus-tained ROSC. Most children had an initial GCS score in the range of 4–7 (Table 2). The mean number of epinephrine injections was 6.73± 4.54 and the mean total dose of epinephrine was 0.39 ± 0.27 (mg/kg).
3.3. Likelihood of survival according to clinical features during the first hour after achieving sustained ROSC
Clinical features during the first hour after achieving sustained ROSC that were significantly predictive of survival included cardiac rhythm, heart rate, blood pressure status, urine output, CPR-induced rib fracture, skin color, initial GCS score, and duration of in-hospital CPR (Table 2).
3.4. Associations between clinical features in the first hour after achieving sustained ROSC and the median duration of survival
The duration of survival of the 80 children who achieved sustained ROSC in the ED ranged from 0.4 to 2456 h. The median duration of survival was significantly longer in patients with sinus rhythm than in patients with ventricular or junc-tional rhythm (Fig. 2A) and significantly shorter in patients with bradycardia after sustained ROSC than patients with normal heart rate or tachycardia (Fig. 2B). Children with CPR-induced rib fracture had a shorter median duration of survival than children without rib fracture (Fig. 2C). The mean duration of pre-hospital CPR and total duration of CPR (pre-hospital plus in-hospital) were longer in patients with rib fracture (13.47± 6.62
and 31.34± 18.42 min) than in patients without rib fracture (10.58± 11.73 and 26.42 ± 15.54 min). After adjusting for total duration of CPR, multiple logistic regression analysis revealed that CPR-induced rib fracture was a significant predictor of poor survival (OR: 6.21, 95% CI: 1.17–32.83, p = 0.032). Children with cyanotic skin color during the post-resuscitative period had a significantly shorter median duration of survival than children with pale or nor-mal skin color (Fig. 2D). In addition, children with an initial GCS > 7 had a longer median duration of survival than children with GCS≤ 7 (Fig. 2E).
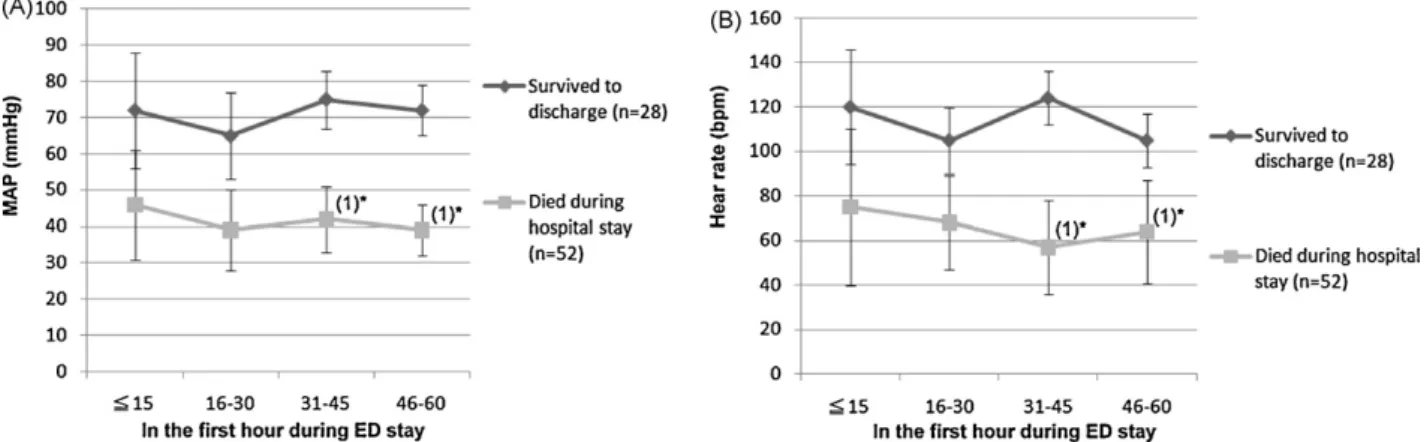
Among the 80 children who achieved sustained ROSC in the ED, 43.8% (n = 35) achieved a return of spontaneous circulation after less than 10 min of in-hospital CPR. Our analysis revealed an inverse correlation between median duration of survival and length of in-hospital CPR (Fig. 2F). In addition, children with post-resuscitative hypotension had a shorter median duration of survival than chil-dren with normal blood pressure or hypertension (Fig. 2G). We also found that children with an initial urine output > 1 ml/kg/h had a longer median duration of survival than children with urine output < 1 ml/kg/h. There was a direct association between the duration of survival and urine output (Fig. 3A) (all p < 0.05). The MAP and heart rate during the first hour after achieving sustained ROSC were significantly higher in children who survived to dis-charge than in children who did not survived to disdis-charge (Fig. 4A and B).
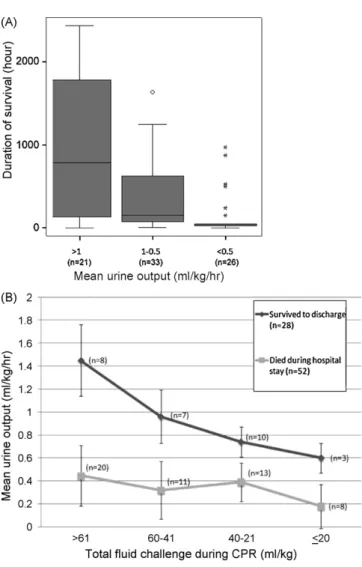
Fig. 3. The urine output in the first hour after achieving sustained ROSC (A) asso-ciated the different durations of survival (p < 0.001) and (B) the initial urine output increased in proportion to the amount of fluid administered during CPR in patients who survived to discharge.
3.5. The relationship between volume of fluid administered during CPR and urine output in children with sustained ROSC
We found that in patients who survived to discharge (n = 28), the initial urine output increased in proportion to the amount of fluid administered during CPR. However, in children who died during hospital stay (n = 52), the initial urine output was very low and the mean urine output was not >0.5 ml/kg/h, even in patients who had received massive fluid challenge during CPR (Fig. 3B).
3.6. Good neurologic outcomes of survivors
All survivors with good neurologic outcomes had sinus rhythm and normal heart rate or tachycardia when spontaneous circula-tion returned. None of them had an initial urine output lower than 0.5 ml/kg/h and none of them had CPR-related chest injuries. In addition, the total duration of CPR (pre-hospital plus in-hospital) was <25 min and the duration of in-hospital CPR was <15 min. With the exception of one child, all children showed deterioration in at least one PCPC scale category.
4. Discussion
Although sustained ROSC can be initially established after resus-citation from non-traumatic OHCA in some children, many of the children lose spontaneous circulation during hospital stay and do not survive to discharge.2It remains challenging for ED physicians
to predict the survival after OHCA in children, especially in children with unstable signs in the post-resuscitative period. In this study, we have analyzed the post-resuscitative clinical features that may predict the chances of survival and the duration of survival.
Previous studies have shown that the initial cardiac rhythm (immediately upon arrival or at the scene) plays an important role in predicting the survival of OHCA children.3,7 In this study, we
found that sinus rhythm in the post-resuscitative period was asso-ciated with survival. Furthermore, we found that children with initial ventricular and junctional rhythm had a shorter duration of survival than children with sinus rhythm. In addition, normal heart rate and tachycardia were both associated with survival. Very few children who presented with bradycardia during the post-resuscitative period survived to discharge and none of them had good neurologic outcomes. Therefore, close monitoring of cardiac rhythm and rate during the post-resuscitation period and provid-ing appropriate management are important after children achieve sustained ROSC.
Although CPR-induced rib fracture is common and has been shown to be associated with poor outcome in adult OHCA patients. Lederer et al. analyzed the autopsy and chest X-ray reports of adult OHCA patients and found that CPR-induced rib fracture occurred in up to 94.7% of cases,11the relationship between rib fracture caused
by CPR and outcome of children with OHCA who achieve sustained ROSC have not been well analyzed. In this study, we found that rib fracture was associated with prolonged CPR duration and children with rib fracture had lower chance to survive than children with-out CPR-induced fracture after adjusting for total duration of CPR. A few studies have reported that CPR-induced rib fracture is not common in pediatric patients.12For example, in a series of 923
chil-dren who received CPR, rib fracture occurred in only 3 patients.13
In our study, however, 15 of the 80 children suffered CPR-induced rib fracture. One of the possible reasons for the higher incidence of rib fracture in our study is resuscitation improperly performed by bystanders. According to the EMS records, 9 children with rib frac-ture had received a precordial thump by a witness to the cardiac arrest before the EMS had arrived.
Fig. 4. The MAP (A) and heart rate (B) which might associate with post-resuscitative cardiac output were all higher in children who survived to discharge than in children who did not survive to discharge in the 4 time points during the first hour of their ED stay. *Number of patients with missing information.
Oxygenation can be assessed by measuring PaO2 levels and by pulse oximetry; however, skin color assessment is a simpler, more rapid method for assessing oxygen delivery, especially in the ED (PaO2need withdraw the blood and pulse oximetry might be affected by incorrect sensor application and movements). Cyanotic skin color during the post-resuscitation period in the ED can be interpreted as a sign of severe hypoxia. In this study, we found that cyanotic skin color was associated with poor survival and shorter duration of survival. In fact, none of the children who survived to discharge with good neurologic outcomes had cyanotic skin color during the post-resuscitation period.
Prolonged CPR has an impact on the ultimate prognosis of chil-dren with non-traumatic OHCA.2,14 In this study, we found that
the duration of in-hospital CPR is a significant predictor of survival. Among the children who initially achieved a sustained ROSC in the ED, those who received in-hospital CPR for more than 20 min had a markedly shorter duration of survival and none of them survived to discharge with good neurologic outcomes.
Studies have shown that urine output is associated with the severity of hypovolemia.15–17However, the association between
the amount of urine output and the prognosis of children with non-traumatic OHCA has not been well addressed. In this study, we found that initial urine output in the first hour after achieving sustained ROSC is associated with the duration of survival. Urine output > 1 ml/kg/h was associated with longer duration of survival. In children who survived to discharge (n = 28), their first hour urine output increased in proportion to the total amount of fluid that had been administered during CPR. In children who died during hospi-tal stay (n = 52), their first hour urine output was not dependent on the amount of fluid that had been administered. The urine out-put in the first hour after achieving sustained ROSC might reflect the initial post-resuscitative hemodynamic status (including rela-tive hypovolemia and the perfusion status of the urinary system). Adequate urine output in the initial post-resuscitation phase can indicate stabilization of hemodynamic status, and, therefore, bet-ter outcome. In fact, the initial urine output was not lower than 0.5 ml/h/kg in any of the children who survived to discharge with good neurologic outcomes. Therefore, patients might be more sta-ble when a balance between fluid input and urine output is reached after achieving sustained ROSC.
Previous studies have demonstrated that the outcomes of OHCA patients could be better if cardiac function returned as soon as possible.18–20We thought that the post-resuscitative blood
pres-sure and heart rate directly associated with the initial cardiac output. Moreover, the end organ perfusion (i.e., urinary system perfusion) which was also associated with cardiac output could be reflected by urine output. Therefore, the initial blood pressure, heart rate and urine output were important clinical features for
primary clinicians to predict the outcomes of OHCA children and monitoring the blood pressure and heart rate should be empha-sized.
4.1. Limitations
To our knowledge, children who experience an OHCA but who do not present with neurologic deficits are prime candidates for cardiac resuscitation. In this study, however, only 6 children were discharged with good neurologic outcomes. Therefore, factors asso-ciated with good neurologic outcomes were difficult to analyze. In addition, data from 11 patients were excluded from the analysis of mean duration from scene to hospital and data from 9 patients were excluded from the analysis of mean pre-hospital BLS dura-tion because of missing data. Also, 12 children were excluded from the analysis of mean body weight because of missing data. The ret-rospective nature of this study was also a limitation. In our EDs, children who suffered OHCA and achieved sustained ROSC were quite unstable and would not stay in ED for long time. Therefore, the vital signs of patients will be routinely recorded every 10–15 min. Although, every doctors and nurses were well trained and passed the APLS examinations. There were still potentially some mistakes in recording data.
5. Conclusions
The post-resuscitative clinical features of non-traumatic OHCA children in the first hour after achieving sustained ROSC that can predict survival include sinus rhythm, a normal heart rate, normal blood pressure, and an initial urine output > 1 ml/kg/h.
Conflict of interest statement
There is no conflict of interest related to this study.
References
1. Donoghue AJ, Nadkarni V, Berg RA, et al. Out-of-hospital pediatric cardiac arrest: an epidemiologic review and assessment of current knowledge. Ann Emerg Med 2005;46:512–22.
2. Young KD, Gausche-Hill M, McClung CD, et al. A prospective, population-based study of the epidemiology and outcome of out-of-hospital pediatric cardiopul-monary arrest. Pediatrics 2004;114:157–64.
3. Lin YR, Wu HP, Huang CY, et al. Significant factors in predicting sustained ROSC in paediatric patients with traumatic out-of-hospital cardiac arrest admitted to the emergency department. Resuscitation 2007;74:83–9.
4. Lin YR, Wu HP, Huang CY, et al. Predictors of successful resuscitation in non-trauma dead-on-arrival children. Acta Paediatr Taiwan 2006;47:278–83. 5. Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr
6. Zaritsky A, Nadkarni V, Hazinski MF, et al. Recommended guidelines for uni-form reporting of pediatric advanced life support: the pediatric Utstein style. Circulation 1995;92:2006–20.
7. Atkins DL, Everson-Stewart S, Sears GK, et al. Resuscitation outcomes consor-tium investigators epidemiology and outcomes from out-of-hospital cardiac arrest in children: the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation 2009;119:1484–91.
8. Engdahl J, Axelsson A, Bång A, et al. The epidemiology of cardiac arrest in children and young adults. Resuscitation 2003;58:131–8.
9. Hickey RW, Cohen DM, Strausbaugh S, et al. Pediatric patients requiring CPR in the prehospital setting. Ann Emerg Med 1995;25:495–501.
10. Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resus-citation outcome reports: update and simplification of the Utstein templates for resuscitation registries. A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, Inter American Heart Foundation, Resuscitation Council of Southern Africa). Resuscitation 2004;63:233–49.
11. Lederer W, Mair D, Rabl W, et al. Frequency of rib and sternum fractures associ-ated with out-of-hospital cardiopulmonary resuscitation is underestimassoci-ated by conventional chest X-ray. Resuscitation 2004;60:157–62.
12. Hoke RS, Chamberlain D. Skeletal chest injuries secondary to cardiopulmonary resuscitation. Resuscitation 2004;63:327–38.
13. Maguire S, Mann M, John N, et al. Does cardiopulmonary resuscitation cause rib fractures in children? A systematic review. Child Abuse Negl 2006;30: 739–51.
14. Gillis J, Dickson D, Rieder M, et al. Results of inpatient pediatric resuscitation. Crit Care Med 1986;14:469–71.
15. Shackford SR, Norton CH, Ziegler MG, et al. The effect of hemorrhage and resus-citation on serum levels of immunoreactive atrial natriuretic factor. Ann Surg 1988;207:195–200.
16. McCunn M, Dutton R. End-points of resuscitation how much is enough? Curr Opin Anaesthesiol 2000;13:147–53.
17. Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med 2008;34:17–60.
18. Marcusohn E, Roguin A, Sebbag A, et al. Primary percutaneous coronary inter-vention after out-of-hospital cardiac arrest: patients and outcomes. Isr Med Assoc J 2007;9:257–9.
19. Lettieri C, Savonitto S, De Servi S, et al. Emergency percutaneous coronary inter-vention in patients with ST-elevation myocardial infarction complicated by out-of-hospital cardiac arrest: early and medium-term outcome. Am Heart J 2009;157:569–75.
20. Overlie PA, Walter PD, Hurd II HP, et al. Emergency cardiopulmonary support with circulatory support devices. Cardiology 1994;84:231– 7.