A
l though hyperlipidemia has been rec og nized as a ma jor risk fac tor of car dio vas cu lar dis eases for de -cades, the ben e fit of lipid low er ing was dem on strated late in 1994 by a large, ran dom ized clin i cal trial.1 De spite the clin i cal and eco nomic sig nif i cance as so ci ated with the antilipemic drugs, lit tle was known about their uti li -za tion at the na tional level.2,3 Among the mem ber coun tries of the OECD (Or gani sa tion for Eco nomic Co -operation and De vel op ment), only seven coun tries had data based on na tional phar ma ceu ti cal sales in 1998.4Since 1995, a Na tional Health In sur ance (NHI) pro gram cov er ing nearly all pop u la tion has been im ple mented in Tai wan. With the avail abil ity of lon gi tu di nal med i ca tion data of in di vid ual pa tients within the NHI, we had the op -por tu nity of study ing not only the na tional con sump tion of antilipemic drugs, but also the prev a lence of anti -lipemic drug use in this coun try.
In this cur rent study, we sur veyed the out pa tient dataset of the NHI claims from a 50,000-person co hort in the cal en dar year 2000. Be side cal cu lat ing the age- and J Chin Med Assoc
2003;66:39-45 Tzeng-Ji Chen1,3 Shing-Jong Lin2,4 Liang-Kung Chen1,3 Shinn-Jang Hwang1,3 Li-Fang Chou5 1
De part ment of Fam ily Med i cine; 2
Di vi sion of Car di ol ogy, De part ment of Med i cine, Tai pei Vet erans Gen eral Hos pi tal; and
3
Di vi sion of Fam ily Med i cine; 4
In sti tute of Clin i cal Med i cine, Na tional Yang-Ming Uni ver sity School of Med i cine; and
5 De part ment of Pub lic Fi nance, Na tional Chengchi Uni ver sity, Tai pei, Tai wan, R.O.C.
Key Words antilipemic agents; drug uti li za tion;
na tional health pro grams; pharmacoepidemiology; prev a lence
Prev a lence of Antilipemic Drug Use in
Tai wan: Anal y sis of a Sam pling Co hort
within the Na tional Health In sur ance
Back ground. Hyperlipidemia is a ma jor risk fac tor of car dio vas cu lar dis eases. We
in ves ti gated the uti li za tion of antilipemic drugs at the out pa tient sec tor within the Na -tional Health In sur ance in Tai wan.
Methods. We ob tained the first co hort (n = 50,000) dataset from the Na tional Health
In sur ance Re search Da ta base and an a lyzed the out pa tient claim files of the co hort in 2000. The antilipemic drugs were de fined as the drug items be long ing to the group C10 (se rum lipid re duc ing agents) of the An a tom i cal Ther a peu tic Chem i cal clas si fi -ca tion sys tem.
Re sults. Among the co hort with 46,614 el i gi ble peo ple, 760 pa tients had ever re
-ceived antilipemic drugs (prev a lence: 1.6%). The group 60 - 69 years of age had the great est age-specific prev a lence (7.2%), fol lowed by the group over 70 years of age (6.0%). There were more male than fe male pa tients, but fe male pa tients out num bered male pa tients be fore the age of 49 years. The antilipemic drugs had been pre scribed 3,850 times to tally with 70,272 de fined daily doses (DDDs). On an av er age, a pa tient with antilipemic ther apy re ceived 5.1 (± 4.5) pre scrip tions of antilipemic drugs in one year and a pre scrip tion con tained 18.3 (± 11.5) DDDs. We mea sured 4.1 DDDs per 1,000 in hab it ants per day for all antilipemic drug use in 2000. The statins and fibrates pre dom i nated the antilipemic drug use. While gemfibrozil was most pop u lar in re spect of re cip i ents and pre scrip tion items, simvastatin had the larg est amount of use in unit of DDDs. Di a be tes mellitus co-existed in 37.8% of the pa tients with antilipemic ther apy and the stan dard ized mor bid ity ra tio (SMR) was 3.34. The other con com i tant dis eases in cluded es sen tial hy per ten sion (rate: 48.8%, SMR: 2.40) and other heart dis ease (rate: 30.7%, SMR: 2.36).
Con clu sions. Statins were the lead ing antilipemic drugs in Tai wan. The us ers of
antilipemic drugs were more likely to have con com i tant di a be tes mellitus, hy per ten -sion and heart dis ease.
Re ceived: June 22, 2002. Ac cepted: October 22, 2002.
Cor re spon dence to: Shing-Jong Lin, MD, Di vi sion of Car di ol ogy, Tai pei Vet erans Gen eral Hos pi tal, 201, Sec. 2, Shih-Pai Road, Tai pei 112, Tai wan.
sex-specific prev a lence of antilipemic drug use and the con sump tion of sin gle antilipemic drugs in Tai wan, we in ves ti gated the health con di tions of the pa tients with antilipemic ther apy by eval u at ing their con com i tant dis -eases.
METHODS Data sources
We ob tained the first co hort dataset from the Na -tional Health In sur ance Re search Da ta base (NHIRD; http://www.nhri.org.tw/nhird/). The co hort in cluded 50,000 peo ple ran domly sam pled from 23,753,407 peo -ple who had ever been in sured un der the NHI since 1995. The dataset in cluded all in sur ance claims of these 50,000 peo ple from 1996 to 2000. The pur pose of the NHIRD and the struc ture of the NHI claim files had been de -scribed in de tails in our pre vi ous study.5
In the cur rent study, we an a lyzed only the out pa -tient visit and or der files of the co hort dataset in 2000 (R01_CD2000.DAT, and R01_OO2000.DAT). These files con tained the claims of out pa tient (in clud ing emer -gency) vis its to clin ics of West ern med i cine, den tistry and tra di tional Chi nese med i cine. Be sides, we ob tained a com plete file of 21,146 ap proved drug items of West ern med i cine in Tai wan from the web site of the Bu reau of Na tional Health In sur ance (BNHI; http://www.nhi.gov.tw/; ac cessed May 25th, 2001). The BNHI also of fered a list of ATC (the An a tom i cal Ther a peu tic Chem i cal clas si fi -ca tion sys tem) codes (4th level) for each drug item.6 We added the 5th level cod ing for the rel e vant drug items and found their De fined Daily Dose (DDD), re spec tively.6
Study de sign
The antilipemic drugs de fined in our study in cluded all drug items be long ing to the group C10 (se rum lipid re duc ing agents) of the ATC clas si fi ca tion sys tem. The C10 group had only one 3rdlevel sub group C10A (cho -les terol- and triglyceride re duc ers) with five 4th-level sub groups: C10AA (HMG CoA reductase in hib i tors), C10AB (fibrates), C10AC (bile acid sequestrants), C10AD (nic o tinic acid and de riv a tives), and C10AX (other cho -les terol- and triglyceride re duc ers). Totally, 145 items of
antilipemic drugs have been reg is tered in the NHI drug file since 1995.
We first iden ti fied the or der re cords with pre scrip -tions of antilipemic drugs in the R01_OO2000.DAT and then found their as so ci ated visit re cords in the R01_CD2000.DAT. These re cords were ex tracted for fur ther anal y ses. Be cause the bile acid sequestrants, es -pe cially cholestyramine, were not solely used in treat ing hyperlipidemia, we ex cluded their re cords with out a re lated di ag no sis, i.e. 272 as the first three dig its of di ag -nos tic codes in ICD-9-CM (In ter na tional Clas si fi ca tion of Dis eases, 9th Re vi sion, Clin i cal Mod i fi ca tion). In a visit re cord, up to three di ag no ses were coded ac cord ing to the ICD-9-CM.
The use of antilipemic drugs among the co hort was strat i fied by the re cip i ents’ age/sex to de ter mine the prev a lence. We also strat i fied the pre scrip tions of anti -lipemic drugs by their chem i cal sub stances (ATC 5th level) and cal cu lated the num ber of re cip i ents, the num -ber of pre scribed items, and the to tal pre scribed amount in unit of DDDs in each main in gre di ent. Be sides, the num bers of DDDs per 1,000 in hab it ants per day were cal cu lated to re flect the pro por tion of the Tai wan ese pop -u la tion treated daily with each kind of antilipemic dr-ugs at the out pa tient sec tor.
Hyperlipidemia usu ally coexisted with other dis eases. To cal cu late the fre quency of con com i tant dis eases in the pa tients re ceiv ing antilipemic drugs, we ex -tracted the iden ti fi ca tion num bers of these pa tients and found out all of their visit re cords and di ag no ses, not lim -ited to the re cords with pre scrip tions of antilipemic drugs. Be cause more than 12,000 codes in the 9CM had dif fi cul ties in anal y sis, we adopted the group -ing sys tem de vel oped by the Na tional Cen ter of Health Sta tis tics of the United States for use with the data of the Na tional Am bu la tory Med i cal Care Sur vey (NAMCS) and the Na tional Hos pi tal Am bu la tory Med i cal Care Sur vey (NHAMCS).7 All of the orig i nal ICD-9-CM codes were re clas si fied into 22 main cat e go ries and 194 groups. Be side cal cu lat ing the crude rates of ma jor con -com i tant dis eases in the pa tients re ceiv ing antilipemic drugs, we also com puted the stan dard ized mor bid ity ra -tios (SMR) (the in di rect method of rate ad just ment) to elim i nate the con found ing ef fect from age fac tor.8
Data pro cess ing and sta tis ti cal anal y sis
The da ta base soft ware of Microsoft SQL Server 2000 was used for data link age and cal cu la tion. For the age- and sex-specific prev a lence, the de nom i na tors were those peo ple who were still in sured un der the NHI in 2000. Among the 50,000 peo ple of the sam pling co hort, 46,614 were still in sured in 2000. In cal cu lat ing the num -bers of DDDs per 1,000 in hab it ants per day for each kind of antilipemic drugs, the to tal num bers of DDDs from the co hort were at first di vided by 46,614 (peo ple in sured un der the NHI at the end of 2000) and 366 (days in year 2000), and then mul ti plied by 1,000 (in hab it ants). In cal -cu lat ing the SMR, the stan dard pop u la tion was also the co hort. The prev a lence rates and SMRs were dis played with 95% con fi dence in ter vals.9
RE SULTS
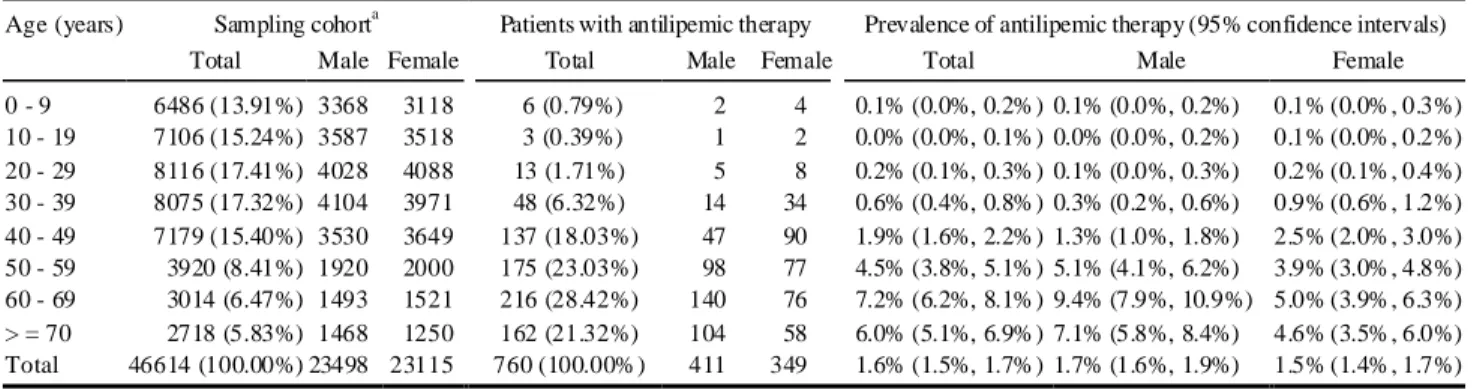
Among the co hort with 46,614 peo ple who were still in sured un der the NIH in 2000, only 41,333 (88.7%) peo -ple had the out pa tient visit of West ern med i cine within the NHI dur ing the whole year. Antilipemic drugs had been ever pre scribed to 760 peo ple (Ta ble 1). The to tal prev a lence of antilipemic drug use was 1.6% (95% CI: 1.5% to 1.7%). Nearly a half of the pa tients with anti -lipemic ther apy were more than 60 years of age. The age-specific prev a lence rate jumped af ter the age of 40 years and was the high est in the age group of 60-69 years (7.2%). The prev a lence rate in the age group over 70 years was higher than that in the age group of 50 - 60 years (6.0% vs. 4.5%). The trend of agespecific prev a
-lence rates was sim i lar in both sexes. Al though the to tal num ber of pa tients with antilipemic ther apy was larger in male than that in fe male, the fe male pa tients still out -num bered the male pa tients be fore the age of 49 years.
In the out pa tient claims of the co hort in 2000, there were 74 dif fer ent drug items of antilipemic drugs with 18 main in gre di ents. Al though atorvastatin (C10AA05) has been avail able within the NHI since No vem ber 2000, it did not ap pear in our co hort dataset. The antilipemic drugs had been pre scribed to tally 3,850 times with 70,272 DDDs (Ta ble 2). On an av er age, a pa tient with anti lipemic ther apy re ceived 5.1 (SD 4.5) pre scrip tions of anti -lipemic drugs in one year, where a pre scrip tion con tained 18.3 (SD 11.5) DDDs. Be sides, we mea sured 4.1 DDDs per 1,000 in hab it ants per day for all antilipemic drug use in 2000. The statins and fibrates pre dom i nated the anti -lipemic drug use. While gemfibrozil was most pop u lar in re spect of re cip i ents and pre scrip tion items, simvastatin had the larg est amount of use in unit of DDDs.
In 2000, the co hort in our study had 657,038 vis its where 901,977 di ag nos tic codes with 6,335 dis tinct di ag -no ses had been spec i fied. The 760 pa tients with antilipemic ther apy had 24,240 vis its where 44,320 di ag -nos tic codes with 1,752 dis tinct di ag no ses had been spec i fied. Ta ble 3 lists the top 12 di ag no sis groups that were most fre quently ob served in the pa tients with antilipemic ther apy. In or der to il lus trate the SMRs, the fre quen cies of these di ag no ses among the co hort were also dis played. Di a be tes mellitus co-existed in 37.8% of the pa tients with antilipemic ther apy and the SMR was 3.34 (95% CI: 2.61 to 4.17). The other sig nif i cant con -com i tant dis eases in cluded other en do crine nu tri tional
Table 1. Age-sex distribution of the sampling cohort, and patients receiving the antilipemic therapy
Sampling cohorta Patients with antilipemic therapy Prevalence of antilipemic therapy (95% confidence intervals) Age (years)
Total Male Female Total Male Female Total Male Female
0 - 9 6486 (13.91%) 3368 3118 6 (0.79%) 2 4 0.1% (0.0%, 0.2%) 0.1% (0.0%, 0.2%) 0.1% (0.0%, 0.3%) 10 - 19 7106 (15.24%) 3587 3518 3 (0.39%) 1 2 0.0% (0.0%, 0.1%) 0.0% (0.0%, 0.2%) 0.1% (0.0%, 0.2%) 20 - 29 8116 (17.41%) 4028 4088 13 (1.71%) 5 8 0.2% (0.1%, 0.3%) 0.1% (0.0%, 0.3%) 0.2% (0.1%, 0.4%) 30 - 39 8075 (17.32%) 4104 3971 48 (6.32%) 14 34 0.6% (0.4%, 0.8%) 0.3% (0.2%, 0.6%) 0.9% (0.6%, 1.2%) 40 - 49 7179 (15.40%) 3530 3649 137 (18.03%) 47 90 1.9% (1.6%, 2.2%) 1.3% (1.0%, 1.8%) 2.5% (2.0%, 3.0%) 50 - 59 3920 (8.41%) 1920 2000 175 (23.03%) 98 77 4.5% (3.8%, 5.1%) 5.1% (4.1%, 6.2%) 3.9% (3.0%, 4.8%) 60 - 69 3014 (6.47%) 1493 1521 216 (28.42%) 140 76 7.2% (6.2%, 8.1%) 9.4% (7.9%, 10.9%) 5.0% (3.9%, 6.3%) > = 70 2718 (5.83%) 1468 1250 162 (21.32%) 104 58 6.0% (5.1%, 6.9%) 7.1% (5.8%, 8.4%) 4.6% (3.5%, 6.0%) Total 46614 (100.00%) 23498 23115 760 (100.00%) 411 349 1.6% (1.5%, 1.7%) 1.7% (1.6%, 1.9%) 1.5% (1.4%, 1.7%) a
and met a bolic dis eases im mu nity dis or ders (rate: 25.1%, SMR: 3.01), es sen tial hy per ten sion (rate: 48.8%, SMR: 2.40), and other heart dis ease (rate: 30.7%, SMR: 2.36).
DIS CUS SION
The in sur ance claims data from the NHI in Tai wan are in valu able to the re search of pharmacoepidemiology. The uti li za tion of antilipemic drugs is one of the good ex am ples be cause nearly all of these drugs have unique in -di ca tion and the pre scrip tion of them has been un der rigid re stric tions based on the rec og nized guide lines, e.g. the sec ond re port of the Na tional Cho les terol Ed u ca tion
Pro gram Ex pert Panel on De tec tion, Eval u a tion, and Treat ment of High Blood Cho les terol in Adults.10 Al -though the prev a lence of antilipemic drug use might be sig nif i cantly lower than the prev a lence of hyperlipi demia among the pop u la tion, the trend and other anal y -ses would help to iden tify the key points of pub lic health and med i cal in ter ven tions.
The Chi nese in Tai wan are known to have low in ci -dence of cor o nary ar tery dis ease and low prev a lence of hyperlipidemia in in ter na tional com par i son.11 But it re -mains un known whether the prev a lence of pa tients with antilipemic ther apy in Tai wan is also low cor re spond -ingly. The in ter na tional com par i son of drug uti li za tions is usu ally more dy namic than that of dis ease ep i de mi ol -Table 2. Distribution of antilipemic drug prescriptions by main ingredients
ATCacoding Group/ingredient name
No of recipients No of antilipemic drug items Total DDDsbof antilipemic drugs DDDs per 1,000 inhabitants per day
C10AA HMG CoA reductase inhibitors 422 1,934 40,552 2.4
C10AA01 Simvastatin 170 753 19,115 1.1 C10AA02 Lovastatin 134 475 8,634 0.5 C10AA03 Pravastatin 70 348 4,963 0.3 C10AA04 Fluvastatin 88 358 7,840 0.5 C10AB Fibrates 395 1,700 24,850 1.5 C10AB01 Clofibrate 12 49 247 0.0 C10AB02 Bezafibrate 80 347 5,123 0.3
C10AB03 Aluminium clofibrate 1 4 90 0.0
C10AB04 Gemfibrozil 260 1,017 14,648 0.9
C10AB05 Fenofibrate 33 90 2,285 0.1
C10AB06 Simfibrate 1 1 2 0.0
C10AB09 Etofibrate 39 192 2,455 0.1
C10AC Bile acid sequestrants 7 26 337 0.0
C10AC01 Cholestyramine 4 20 189 0.0
C10AC03 Detaxtran 3 6 148 0.0
C10AD Nicotinic acid and derivatives 34 172 4,384 0.3
C10AD01 Niceritrol 2 16 148 0.0
C10AD03 Nicofuranose 5 15 262 0.0
C10AD06 Acipimox 21 113 3,311 0.2
C10AD- Nicomol 6 28 663 0.0
C10AX Other cholesterol and triglyceride reducers 6 18 148 0.0
C10AX02 Probucol 6 18 148 0.0
Total 760c 3,850 70,272 4.1
a
ATC = Anatomical Therapeutic Chemical classification system. b
DDD = defined daily dose. c
ogy. For ex am ple, the Fin land and other Nordic coun tries had slightly lower prev a lence of antilipemic drug us ers and fewer DDDs/1,000 in hab it ants/day in early 1990s than Tai wan in 2000.2,3 How ever, the antilipemic drug use in those coun tries in creased 6- to 8-fold from 1994 to 2000, mostly due to statins.4 Fur ther study is needed to in ves ti gate whether the strict re stric tions within the NHI in Tai wan, e.g. man da tory blood anal y sis in three-month in ter vals, dis cour age the antilipemic drug use and hin der the dif fu sion of newer in no va tions.
The fo cus of pharmacoepidemiology study of anti -lipemic drugs in the lit er a ture could be sum ma rized into the fol low ing as pects: age-, sex-, dis ease-, phy si specific drug use, and out come anal y sis.12-21 Some of these in ves ti ga tions could be also re peated in Tai wan with the cur rent NHIRD datasets, but the other could not be done be cause of the in her ent lim i ta tions of the NHI claims data.
For ex am ple, hyperlipidemia, hy per ten sion and hy per glycemia (socalled 3H) are known to have a clus ter ing ten dency. Using SMRs to com pare the pa tients re ceiv ing antilipemic ther apy with the sam pling pop u la -tion in comorbidity, our study showed that those pa tients in Tai wan did have con com i tant di a be tes mellitus and es -sen tial hy per ten sion more fre quently. In the fu ture we
would per form an other study to know what per cent age of pa tients with di a be tes mellitus or es sen tial hy per ten sion also re ceive antilipemic ther apy.
As to the vari a tions of phy si cians in man ag ing hyperlipidemia or pre scrib ing the antilipemic drugs, the NHIRD did not sup ply datasets sam pled ac cord ing to con sult ing phy si cians. The datasets in our cur rent study and other avail able datasets with sys tem atic sam pling from all vis its could only of fer ag gre gate sta tis tics of the phy si cian spe cial ties, not of in di vid ual phy si cians.
A se ri ous draw back of the NHI claims is the ab sence of lab o ra tory data, let alone other clin i cal and so cio eco -nomic in for ma tion. Fur ther more, the pri vacy pol icy of the BNHI and NHIRD has en crypted the pa tients’ per sonal iden ti fi ca tion num bers (PID). Al though the en -crypted PIDs re main con sis tent in all the NHIRD datasets, they can not be linked to other out side da ta bases, e.g. the mor tal ity da ta base of the De part ment of Health. Be sides, the re search ers are for bid den to iden tify the pa tients for dis ease con fir ma tion and fol lowups. That is, the out -come anal y sis and the study on the ap pro pri ate ness (over- and undertreatment) of antilipemic drug use are not fea si ble with the NHI claims.22-25
To the best of our knowl edge, our cur rent study might be one of the first in ves ti ga tions con cern ing the Table 3. Frequency of concomitant diseases in the patients with antilipemic therapy
Diagnosis grouping Sampling cohort
(n = 46,614)
Patients with antilipemic therapy (n = 760)
No. of patients
with a diagnosis Rate
No. of patients
with a diagnosis Rate SMRa(95% CIb) Other acute respiratory infections 30,562 65.6% 526 69.2% 1.14 (0.95, 1.35)
Essential hypertension 3,011 6.5% 371 48.8% 2.40 (1.94, 2.92)
Other diseases of the digestive system 10,466 22.5% 362 47.6% 1.55 (1.25, 1.89) Diseases of the teeth and supporting structures 15,949 34.2% 294 38.7% 1.23 (0.96, 1.53)
Diabetes mellitus 1,796 3.9% 287 37.8% 3.34 (2.61, 4.17)
Other heart disease 2,019 4.3% 233 30.7% 2.36 (1.80, 3.02)
Conjunctivitis 8,432 18.1% 218 28.7% 1.27 (0.95, 1.64)
Other symptoms/signs and ill-defined conditions 4,656 10.0% 202 26.6% 1.63 (1.21, 2.12)
Other dorsopathies 3,921 8.4% 196 25.8% 1.46 (1.08, 1.91)
Acute bronchitis and bronchiolitis 10,106 21.7% 193 25.4% 1.25 (0.92, 1.63) Other endocrine nutritional and metabolic
diseases immunity disorders 1,971 4.2% 191 25.1% 3.01 (2.21, 3.94)
Gastritis and duodenitis 5,174 11.1% 159 20.9% 1.39 (0.99, 1.87)
a
SMR = standardized morbidity ratio. The age adjustment was preformed according to the age structure of the sampling cohort. b
prev a lence of antilipemic drug use among a rep re sen ta -tive pop u la tion in Tai wan. Be cause the pri vate use of the drugs out side the NHI is not in cluded in our datasets and the claims fail to of fer other sig nif i cant data, the tra di tional ep i de mi o log i cal sur veys are still needed to fa cil i -tate the un der stand ing of hyperlipidemia man age ment and antilipemic drug use in Tai wan.26
AC KNOWL EDGE MENTS
This study is based in part on data from the Na tional Health In sur ance Re search Da ta base pro vided by the Bu -reau of Na tional Health In sur ance, De part ment of Health and man aged by Na tional Health Re search In sti tutes in Tai wan. The in ter pre ta tion and con clu sions con tained herein do not rep re sent those of Bu reau of Na tional Health In sur ance, De part ment of Health or Na tional Health Re search In sti tutes.
REF ER ENCES
1. Scan di na vian Simvastatin Sur vival Study Group. Ran dom ised trial of cho les terol low er ing in 4444 pa tients with cor o nary heart dis ease: the Scan di na vian Simvastatin Sur vival Study (4S). Lan cet 1994;344:1383-9.
2. Martikainen J, Klaukka T, Reunanen A, Peura S, Wahlroos H. Re cent trends in the con sump tion of lipid-lowering drugs in Fin land. J Clin Epidemiol 1996;49:1453-7.
3. Magrini N, Einarson T, Vaccheri A, McManus P, Montanaro N, Berg man U. Use of lipid-lowering drugs from 1990 to 1994: an in ter na tional com par i son among Aus tra lia, Fin land, It aly (Emilia Romagna Re gion), Nor way and Swe den. Eur J
Clin Pharmacol 1997;53:185-9.
4. OECD Health Data 2001. Paris: OECD (Or gani sa tion for Eco nomic Co-operation and De vel op ment), 2001.
5. Su TP, Chen TJ, Hwang SJ, Chou LF, Fan AP, Chen YC. Uti li za tion of psychotropic drugs in Tai wan: I. an over view of out -pa tient sec tor in 2000. J Chin Med Assoc 2002;65:378-91. 6. Guide lines for ATC Clas si fi ca tion and DDD As sign ment, 3rd
ed. Oslo: WHO Col lab o rating Cen tre for Drug Sta tis tics Meth od ol ogy, 2000.
7. Schappert SM. Am bu la tory Care Visits to Phy si cian Of fices,
Hos pi tal Out pa tient De part ments, and Emer gency De part ments: United States, 1997 (Vi tal Health Sta tis tics, Se ries 13, No.
143). Hyattsville: Na tional Cen ter for Health Sta tis tics, 1999. 8. Page RM, Cole GE, Timmreck TC. Ba sic Ep i de mi o log i cal
Methods and Biostatistics: A Prac ti cal Guide book. Boston,
Lon don: Jones and Bart lett, 1995.
9. Gardner MJ, Altman DG. Sta tis tics with Con fi dence Con fi -dence In ter vals and Sta tis ti cal Guide lines. Lon don: Brit ish Med i cal Jour nal, 1989.
10. Ex pert Panel on De tec tion, Eval u a tion, and Treat ment of High Blood Cho les terol in Adults. Sum mary of the sec ond re port of the Na tional Cho les terol Ed u ca tion Pro gram (NCEP) Ex pert Panel on De tec tion, Eval u a tion, and Treat ment of High Blood Cho les terol in Adults (Adult Treat ment Panel II). JAMA 1993;269:3015-23.
11. Pan WH, Chiang BN. Plasma lipid pro files and ep i de mi ol ogy of atherosclerotic dis eases in Tai wan - a unique ex pe ri ence.
Ath ero scle ro sis 1995;118:285-95.
12. Sketris IS, Kephart GC, Hicks VA, Hub bard EJ, Brown MG, Chan dler RF, MacLean DR. Pre scribing pat terns of antilipemic drugs and prev a lence of hy per cho les ter ol emia in the Nova Sco tia pop u la tion more than 65 years old. Ann Pharmacother 1995;29:576-81.
13. Miller M, Byington R, Hunninghake D, Pitt B, Furberg CD. Sex bias and underutilization of lipidlowering ther apy in pa tients with cor o nary ar tery dis ease at ac a demic med i cal cen -ters in the United States and Can ada. Arch In tern Med 2000;160:343-7.
14. Savoie I, Kazanjian A. Uti li za tion of lipid-lowering drugs in men and women: a re flec tion of the re search ev i dence? J Clin
Epidemiol 2002;55:95-101.
15. Massing MW, Sueta CA, Chowdhury M, Biggs DP, Simpson RJ Jr. Lipid man age ment among cor o nary ar tery dis ease pa -tients with di a be tes mellitus or ad vanced age. Am J Cardiol 2001:87:646-9.
16. Jackevicius CA, An der son GM, Leiter L, Tu JV. Use of the statins in pa tients af ter acute myo car dial in farc tion: Does ev i -dence change prac tice. Arch In tern Med 2001;161:183-8. 17. Harder S, Mohr O, Klepzig H. Lipid-lowering treat ment in
cor o nary ar tery dis ease: a sur vey in an am bu la tory out pa tient clinic. Int J Clin Pharmacol Ther 2001;39:534-8.
18. Stafford RS, Blumenthal D, Pasternak RC. Vari a tions in cho -les terol man age ment prac tices of U.S. phy si cians. J Am Coll
Cardiol 1997;29:139-46.
19. Baxter C, Jones R, Corr L. Time trend anal y sis and vari a tions in pre scrib ing lipid low er ing drugs in gen eral prac tice. BMJ 1998;317:1134-5.
20. Packham C, Rob in son J, Mor ris J, Rich ards C, Marks P, Gray D. Statin pre scrib ing in Nottingham gen eral prac tices: a cross-sectional study. J Pub lic Health Med 1999;21:60-4.
21. Pearson TA, Laurora I, Chu H, Kafonek S. The Lipid Treat -ment As sess -ment Pro ject (L-TAP): a multicenter sur vey to eval u ate the per cent ages of dyslipidemic pa tients re ceiv ing lipid-lowering ther apy and achiev ing low-density li po pro tein cho les terol goals. Arch In tern Med 2000;160:459-67. 22. Majumdar SR, Gurwitz JH, Soumerai SB. Undertreatment of
hyperlipidemia in the sec ond ary pre ven tion of cor o nary ar tery dis ease. J Gen In tern Med 1999;14:711-7.
23. Larsen J, Vaccheri A, Andersen M, Montanaro N, Berg man U. Lack of ad her ence to lipidlowering drug treat ment. A com par i son of uti li za tion pat terns in de fined pop u la tions in Funen, Den
-mark and Bo lo gna, It aly. Br J Clin Pharmacol 2000;49: 463-71. 24. Feely J, McGettigan P, Kelly A. Growth in use of statins af ter tri als is not tar geted to most ap pro pri ate pa tients. Clin
Pharmacol Ther 2000;67:438-41.
25. Abookire SA, Karson AS, Fiskio J, Bates DW. Use and mon i tor ing of “statin” lipidlowering drugs com pared with guide -lines. Arch In tern Med 2001;161:53-8.
26. Lee YT, Lin RS, Sung FC, Yang CY, Chien KL, Chen WJ, et
al. ChinShan Com mu nity Car dio vas cu lar Co hort in Tai wan
-base line data and five-year fol low-up mor bid ity and mor tal ity.