Communications of the Association for Information Systems
Volume 36
Article 31
5-2015
Critical Factors of Adopting Enterprise Application
Integration Technology: An Empirical Study on
Larger Hospitals
Wei-Hsi Hung
Department of Information Management, Advanced Institute of Manufacturing with High-Tech Innovations (AIM-HI), National Chung Cheng University, Taiwan, ROC, fhung@mis.ccu.edu.tw
I-Cheng Chang
Department of Accounting, National Dong Hwa University, Taiwan, ROC
David C. Yen
School of Economics and Business, SUNY -Oneonta, USA
Che-Ming Lee
Department of Information Management, National Chung Cheng University, Taiwan, ROC
Follow this and additional works at:
http://aisel.aisnet.org/cais
This material is brought to you by the Journals at AIS Electronic Library (AISeL). It has been accepted for inclusion in Communications of the Association for Information Systems by an authorized administrator of AIS Electronic Library (AISeL). For more information, please contact
elibrary@aisnet.org.
Recommended Citation
Hung, Wei-Hsi; Chang, I-Cheng; Yen, David C.; and Lee, Che-Ming (2015) "Critical Factors of Adopting Enterprise Application Integration Technology: An Empirical Study on Larger Hospitals," Communications of the Association for Information Systems: Vol. 36, Article 31.
Volume 36 Article 31
Critical Factors of Adopting Enterprise Application Integration Technology: An
Empirical Study on Larger Hospitals
Wei-Hsi Hung
Department of Information Management, Advanced Institute of Manufacturing with High-Tech Innovations (AIM-HI), National Chung Cheng University, Taiwan, ROC
fhung@mis.ccu.edu.tw
I-Cheng Chang
Department of Accounting, National Dong Hwa University, Taiwan, ROC icc@mial.ndhu.edu.tw
David C. Yen (Point of Contact)
School of Economics and Business, SUNY -Oneonta, USA David.yen@oneonta.edu
Che-Ming Lee
Department of Information Management, National Chung Cheng University, Taiwan, ROC
As hospitals extend their service scope, they adopt more information systems. These systems are implemented in different timelines and the interfaces of databases become varied. Frequently, the exchange of information between various systems requires additional coordination or even manual input for unifying data. To embrace automation, the solution is to adopt enterprise application integration (EAI) technology, the middleware, to convert data from among various information systems to enable an efficient flow of data in the hospital. In this paper, we discuss and verify the impact factors on the integration levels of EAI by surveying larger hospitals above the regional level in Taiwan and testing a proposed research model. The findings of this study show that information technology infrastructure, hospital size, external pressure, internal pressure, and external support significantly affect the EAI level.
Keywords: Enterprise Application Integration, Hospital Information Systems, Integration Level, Hospital.
Volume 36, Article 31, pp. 619-641, May 2015 The manuscript was received 26/10/2013 and was with the authors 11 months for 3 revisions.
Critical Factors of Adopting Enterprise Application Integration Technology: An
Empirical Study on Larger Hospitals
Virhe. Määritä Aloitus-välilehdessä Title, jota haluat käyttää tähän
kirjoitettavaan tekstiin.
620
Volume 36 Article 31
I. INTRODUCTION
Since medical and healthcare institutions are often complex, multi-functional, and information intensive, integrating management information systems is critical in ensuring that the correct information can be stored and accessed real time (Stefanou & Revanoglou, 2006). Previous studies have suggested that ERP (enterprise resource planning) is applicable and adaptable to the medical industry (Paré & Sicotte, 2001; Stefanou & Revanoglou, 2006; Trimmer, Lela, & Wiggins, 2002). However, ERP is usually deemed to be an expensive and complicated solution, and not every hospital has an adequate budget to completely replace an old decentralized system with a universal ERP system. Consequently, a better solution is to employ the enterprise application integration (EAI) technology (Stal, 2002; Özkarabacak, Çevik, & Gökşen, 2014), which is a type of middleware for interchanging data among the various systems available in hospitals.
Contemporary healthcare information systems (HIS) in hospitals are integrated by several heterogeneous systems (Lenz & Kuhn, 2001). In Taiwan since national health insurance was implemented, hospitals have had to rely more heavily on information systems and technologies to exchange documents and financial data with various public agencies, which resulted in HIS’s spread across the entire country. In general, 98.7 percent of hospitals are using information systems and 93% of them are using them for clinical services (Hwang, She, & Liu, 2008). Most of Taiwan’s hospitals have developed their own systems, and 44.3 percent possess different sub-systems that have been developed using various programming languages or with a different version of the same programming language (particularly in the lower-level hospitals) (Hsu & Pan, 2007). Due to the variance between system structures, data formats, and exchange mechanisms, hospitals often find it difficult to unify systems both internally and externally (Hsiao, Lien, Kang, & Kuo, 2007). Thus, hospitals tend to adopt EAI technology to integrate different systems and to increase the operational efficiency of the information provision. For example, EAI is useful for integrating systems at primary and secondary care levels to ensure that users from the various parties can use an integrated system from a unified gateway (Khoumbati, Themistocleous, & Irani, 2006).
Schmidt (2000) argues that, if a hospital could reach the highest level of EAI (for example, external integration), it would be able to exchange patient data externally, which would, in turn, reduce the waste of medical resources, integrate with upstream medicine and pharmaceutical suppliers to increase inventory turnover, and reduce inventory and procuring personnel costs. Otherwise, insufficient IS integration in hospitals my result in numerous care and medical errors. Moreover, missing hard copy films and diagnosed information may occur without an effective EAI, and this certainly causes delays to clinicians’ decision making processes (Khoumbati et al., 2006). Although EAI is an ongoing technology, it has been widely adopted in several sectors, but its adoption in healthcare is scant (Mantzana, Themistocleous, Irani, & Khoumbati, 2008). Moreover, discussions on what factors influence hospital to reach a high level of EAI are rare in this subject area. One previous study has indicated that healthcare actors play an important role in the EAI-adoption process (Mantzana et al., 2008). However, these actors, such as clinicians and nurses, may resist the adoption of IS. Consequently, serious problems can arise, such as poor communication and insufficient educational training, which can cause projects to fail (Mantzana et al., 2008).
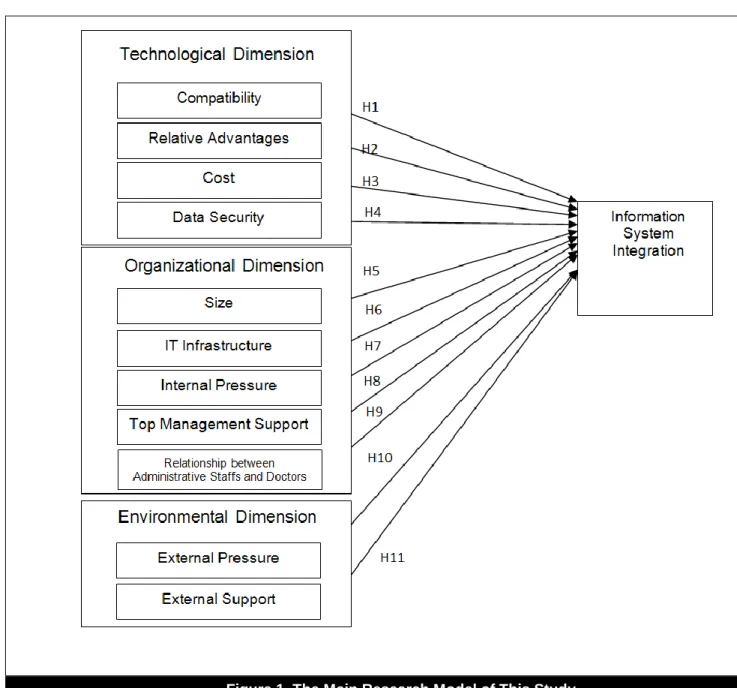
To understand the factors affecting hospital EAI, we employ the innovation diffusion theory and the viewpoints of the technological, organizational, and environmental dimensions (TOE) as Tornatzky, Fleischer, and Chakrabarti (1990) propose. Although the TOE framework has been used in a variety of IT-adoption areas (Gu, Cao, & Duan, 2012; Kuan & Chau, 2001; Lertwongsatien & Wongpinunwatana, 2003; Zhu, Kraemer, & Xu, 2003; Zhu, Wang, & Chen, 2010), it may not be applicable to the healthcare environment. For example, the majority of data in a hospital’s information system needs tailored protection; consequently, better data security features or functions should be carefully considered when adopting EAI technology. Moreover, conflicts between clinical doctors and administrative staff often occur when determining the right information technology to adopt in a hospital; therefore, these associated factors need to be taken into account. In this paper, we analyze the key factors affecting the integration of EAI in terms of the technological, organizational, and environmental dimensions.
This paper is organized as follows: in Section 2, we review the literature with a focus on HIS, EAI, and the innovation diffusion theory. In Section 3, we cover the research method and design. In Section 4, we analyze the data, and, in Section 5, we present the results. Finally, in Section 6, we conclude the study.
Volume 36 Article 31
621
II. LITERATURE REVIEW
Hospital Information Systems
The information systems used in hospitals are collectively known as “hospital information systems” or “hospital management information systems” (Chang, Hwang, Hung, Kuo, & Yen, 2009). With the increasingly popular applications of information technology, HIS’s functions have been expanded to support several medical care-related activities. Thus, more medical-related subsystems have been developed and are currently in use (Sultan et al., 2014).
Early HIS were mainly used to process administrative activities such as registration, pricing, and accounting to save labor resources and improve work efficiency. Most of the present HIS are used to automate hospital processes to speed up work procedures, enhance data processing capabilities, and reduce labor costs. The main supporting tasks include registration and reservations, input from doctors, report transmissions, fee rating and pricing, drug package printing, bed management, healthcare reporting, and inventory management (Stefanou & Revanoglou, 2006). HIS simplify the working process and ensure complete data (Chang et al., 2009).
Lenz and Kuhn (2001) state that most HIS are composed of many heterogeneous systems. A typical system comprises enterprise application components that can support commercial and material data processing, including the components needed to enable the hospital to fully care for its patients. Other issues, including economic management, legal, and other hospital needs are taken into consideration in developing HIS. Özogul, Karsak and Tolga (2009) argue that HIS can provide hospitals with functions in five categories: strategic executive service, resource and supply chain planning, medical care support (care support), patient management, and enterprise management.
Enterprise Application Integration (EAI)
Definition of EAIMany researchers have defined EAI as an integration of data and business processes (Linthicum, 2000; Lublinsky, 2001). It is generally regarded as a middleware and interface engine for integrating such multiple application systems as older versions, legacy, and isolated enterprise-wide systems (Bahli & Ji, 2007; Frantz, Corchuelo, & Molina-Jiménez, 2012). EAI has embraced certain system integration approaches, such as middleware, service-oriented architecture (SOA), and data warehouses. More specifically, middleware and SOA offer business process integration solutions to an entity. SOA is one of the main approaches applied in/to enterprise application integration (Lu & Zhang, 2009). In fact, its approach is based on well-defined standards (Iqbal, Shah, James, & Cichowicz, 2013). Further, the systems provide surface integration, which can be achieved using SOA but only at a syntactic level. The semantic detail of the underlying data cannot be supported with this kind of integration. Further, middleware such as Web services could be used to increase semantic integration (Iqbal et al., 2013). On the other hand, data warehousing systems can be regarded as integral for making decisions (Lee, Siau, & Hong, 2003). Bahli and Ji (2007) argue that the system integration is not only suitable for small systems but also applicable to the enterprise systems with scattered business applications. Such application systems can operate on different platforms or with different database systems by accessing different interfaces that share the same data (McKeen & Smith, 2002). For these aforementioned reasons, EAI integrates the existing information systems to make the business processes smoother and display information in a unified format to support the administrative and management decision making (Mendoza, Pérez, & Grimán, 2006). Moreover, Khoumbati, Themistocleous, Irani, and Mantzana (2008) state that applying EAI to the integration of a healthcare organization mainly includes the integrating caring systems internally and externally. To this end, it allows users and patients at different access points to operate through an integrated engine.
According to Lee et al. (2003), the difference between ERP and EAI is that implementing ERP is promotion oriented and bottom-up because it starts with the most primitive element of the business process. Individuals in the organization cannot select individual business processes in the new system but must accept the ERP standard business process. However, the pull-oriented EAI plans and integrates the original scattered application programs and business processes. As an alternative or value-added technology, EAI takes less energy compared to the automated integration procedure of ERP. Since EAI implementation is a bottom-up approach, it fits into business procedures. Although it takes time to plan business procedures, its implementation is relatively easy and it receives less resistance compared to ERP. According to a survey, the cost of implementing EAI is only 10 to 60 percent of the cost of implementing ERP (Lee et al., 2003).
622
Volume 36 Article 31
EAI Models
Many past studies have proposed different operational models of EAI. Some scholars have divided EAI into organizations’ internal and external parts (Bahli & Ji, 2007). In a contrast, Themistocleous and Irani (2002) suggest dividing application integration into vertical and horizontal integration. They further categorize vertical integration into enterprise intranet and Internet B2C integration and horizontal integration into external extension EAI and virtual EAI. Themistocleous and Irani (2000) suggest several ways for evaluating the integration that include: four integration levels (connectivity, transmission, conversion and process automation), a loose or close integration of products and tool products, the integration of customized systems or package systems, and internal or interorganizational integration.
McKeen and Smith (2002) propose several management strategies for EAI implementation, such as EAI strategy, the careful selection of the EAI tools, an integrated design, and the establishment of cooperation between the enterprise and the trading partners. According to Wijnhoven, Spil, Stegwee, and Fa’s (2006) literature review, information technology integration has three different objectives: complete, partial, and co-existing integration. Factors Affecting EAI
Many past studies on innovation adoption and technological integration have pointed out that a variety of factors affect the adoption of different innovative technologies in an organization. Wijnhoven et al. (2006) propose that information technology integration is related to: (1) information systems, such as databases and procedural functions; (2) information technology frameworks, such as data network, operating systems, hardware, and information technological capabilities; and (3) information technology factors, such as the user application process, information technology managers, information technology coordination capabilities, and educational levels. Bahli and Ji (2007) divide the factors that promote EAI adoption into seven perspectives: information technology, business demand, innovation demand, competitive position, economies of scale, environmental, and the perspective of the guiding principles of the highest management.
Themistocleous (2004) provides a framework to explain the factors affecting the adoption of EAI by enterprises for transactions such as interest, the information technology framework, the cost, external and internal pressure, and precision information technology. Khoumbati et al. (2006) use their theoretical framework to explain that it is applicable to medical organizations because these organizations have lower information technology budgets compared to other general industries. Hospitals spend about two percent of their total expenditure on information technology, while organizations in other industries spend about 10 percent of their total expenditure (Lang, 2003). Therefore, medical organizations have greater limitations when adopting information technology. This framework also affects the decision making factors on EAI adoption, such as interest, obstacles, and cost.
EAI Level
Various models have been proposed to categorize the EAI degrees (Li, Huang, Yen, Shih, & Hsueh, 2013). Linthicum (2000) divide EAI into four levels: data, application interface, method, and user interface integration. Schmidt (2000) also divide EAI into four levels: point-to-point, structural, procedural, and external integration. Moreover, Lublinsky (2001) divide it into three levels: data, information, and procedure; they argue that procedural integration is the most complex, most expensive, and most robust one. McKeen and Smith (2002) categorize EAI into such levels as data, application, procedure, and inter-organizational integration. Kamal (2011) proposes that EAI could the support integration at the following four levels: data, procedure, knowledge management, and application integration. More specifically, the level of data integration includes connectivity, transportation, and translation; the level of procedural integration integrates business procedures by using the data integration level; the knowledge management integration level can share, exchange, and upgrade knowledge; and the application integration level integrates the knowledge obtained from the application systems at the procedural integration level.
EAI can be also divided into inter-organizational and intra-organizational application integrations (Themistocleous & Irani, 2000; Themistocleous & Irani, 2002; Raghupathi & Umar, 2009). Raghupathi and Tan (2008) argue that classifying internal and external integration may be suitable for medical organizations. They define internal integration as the integration of systems or technologies in the organization, and external integration as the integration of systems or technologies by the interface and related computer systems outside an organization. Many scholars have proposed that inter-organizational integration is a part of EAI or as the highest level of application integration (Linthicum, 2000; McKeen & Smith, 2002). Based on above-mentioned models, we categorize the EAI degrees into five levels: 0 (no integration), 1 (point-to-point integration), 2 (structural integration), 3 (procedural integration), and 4 (external integration).
Volume 36 Article 31
623
Theory of Innovation Diffusion
The concept of innovation diffusion has been applied to many innovation-related issues including innovative ideas, products, and innovative information systems (Chen, Gillenson, & Sherrell, 2002; Karahanna, Straub, & Chervany, 1999; Kim & Ammeter, 2014; Oliveira, Thomas, & Espadanal, 2014; Taylor & Todd, 1995; Wu & Wang, 2005). The innovation diffusion theory emphasizes that an organization strives to diffuse information technology to each user community, which is also true of the implementation of an information system in an organization (Cooper & Zmud, 1990). The innovation diffusion theory was first used to discuss the factors regarding the implementation of information technology in organizations, and it was then extended to discussing the factors affecting the diffusion of information technology in organizations (Premkumar, Ramamurthy, & Nilakanta, 1994; Johnson, Zheng, & Padman, 2014).
Tornatzky and Klein (1982) conducted an empirical study related to innovation diffusion. Their findings show that compatibility and complexity were significantly related to user acceptance of innovative technology. They also summarize the follow-up literature on innovation diffusion, and their findings reveal that researchers used compatibility, complexity, and relative advantages most among the original innovation diffusion factors while they did not commonly use observability and verifiability.
Rogers (1995) proposes two viewpoints: adoption and diffusion. The adoption viewpoint mainly uses the social or organizational characteristics to measure factors causing innovation adoption, while the diffusion viewpoint is used to understand the factors creating innovation diffusion and what factors may result in a wide acceptance of an innovation. Rogers (1995) also discusses the factors affecting the adoption of innovative technology by organizations in terms of three dimensions: the organization’s leader characteristics, its internal structural characteristics, and its external characteristics. A group of researchers have justified that the technological, organizational, and environmental (TOE) framework can be employed to identify some important factors regarding the implementation of an information system (Chang et al., 2009; Chau & Tam, 1997; Hung, Hung, Tsai, & Jiang, 2010; Jackson, Yi, & Park, 2013; Kuan & Chau, 2001; Zhu et al., 2003). Such a framework would simultaneously take internal and external environments into account; both also play critical roles in exploring the influential power of adopting the innovative IT.
In this study, we explore what factors affect the integration of EAI and the level of such integration. We base our study on the innovation diffusion model that Rogers (1995) proposes, and, because we focus on organizational and technological situations, we adopt the TOE framework to help identify the key factors affecting the level of EAI.
III. RESEARCH METHOD AND DESIGN
In this study, we develop a model based on research done by Khoumbati et al. (2006), who used the qualitative method to identify the factors that should be considered in implementing information system integration in hospitals. In addition to exploring factors in the TOE dimensions, we empirically discuss the impact from these factors on implementing information system integration in hospitals. Figure 1 illustrates the study’s main research model.
624
Volume 36 Article 31
Research Hypotheses
Past studies have found that, when innovative technology is incompatible with users’ existing values and jobs in an organization, obstacles to its adoption will arise (Chung & Snyder, 2000). In other words, once the technology is compatible with existing systems and working norms, the organization will tend to adopt it (Premkumar & Roberts, 1999; Rogers, 1995). When a hospital integrates a new information system that is more compatible with it, the cost and difficulty level of the integration will be relatively lower. In other words, when the information system can be integrated relatively easily, there will be an increased willingness to seek it. Therefore, we propose:
H1: The more compatibility the existing systems have in a hospital, the higher level of EAI that will result. Rogers (1995) regards the relative advantages of innovation technology as certain levels of advantages perceived by using new information technology as compared to the original technology. The organization can benefit from bigger organizational interests by using new technology rather than maintaining the status quo (Premkumar & Roberts, 1999). The relative advantages of an innovation can affect an organization’s intention towards adopting it (Chong, Ooi, Lin, & Raman, 2009; Premkumar & Ramamurthy, 1995; Thong, 1999). A hospital’s adoption of innovative technology can enhance the quality of medical services and help the hospital gain a competitive advantage (Hung et al., 2010). When the hospital believes that integrating EAI with other hospitals and even with government can bring more significant benefits and enhance its overall competitiveness, it is more likely to consider integrating more kinds of information systems (Khoumbati et al., 2006). Therefore, we propose:
Volume 36 Article 31
625 H2: The more relative advantages a hospital gains from integrating the existing systems, the higher level of
EAI that will result.
Organizations expect that the benefits derived from a new technology will equal or exceed the cost of implementing it (Premkumar & Roberts, 1999). Organizations, therefore, assess new technologies’ costs and benefits before adopting them (Premkumar & Roberts, 1999). Tornatzky and Klein (1982) point out that lower costs can make adopting new technology easier. However, excessively high costs or an inability to raise financial resources will make an organization unwilling to adopt new information technology (Teo, Lin, & Lai, 2009). If the EAI’s costs are lower, the cost-benefit ratio will be higher, and it will be easier for a hospital to integrate the information system at a high level. Therefore, we propose:
H3: The lower cost a hospital spends on integrating the existing systems, the higher level of EAI that will result.
Hospitals adopting new technology can gain many benefits, but, at the same time, security and privacy issues must be considered in order to comply with the basic principles of medical ethics and social expectations (Meingast, Roosta, & Sastry, 2006). Therefore, the privacy of patient information may become an increasingly important issue. Meingast et al. (2006) also point out that Internet and wireless transmissions may increase risks to data security and privacy. The more the information is shared, the higher the potential for abuse. This might make hospitals less inclined to consider integration. Therefore, we propose:
H4: The more a hospital emphasizes data security, the lower the degree of EAI that will result.
Thong (1999) suggests that small enterprises have more restrictions, such as limited resources. These restrictions often lead to various unique limitations. Lind, Zmud, and Fischer (1989) and Teo et al. (2009) infer that large enterprises have a greater potential for adopting an information system when they have larger-scale operations. Bigger hospitals include more departments and more information systems and have greater demands to integrate scattered information systems (Khoumbati et al., 2008); they also have fewer restrictions in resources, and EAI is more likely to be an economy of scale that ultimately results in a higher level of system integration (Hung et al., 2010). Hence, we propose:
H5: Larger hospitals have a higher level of EAI.
A basic information technology infrastructure is one of the necessary conditions for adopting new technology (Applegate, McKenney, & McFarlan, 1999). Grimson et al. (2000) point out that, in medical organizations, the segmented pieces of infrastructure without integration can impede the hospital’s provision of better medical care. In other words, the higher the level of information technology infrastructure an organization/hospital has, the higher the probability that they will successfully integrate new technology. Thus, the hospital will be more likely to integrate organizational systems and will make the EAI at a higher level. Therefore, we propose:
H6: The higher level of information technology infrastructure a hospital has, the higher level of EAI that will result.
In the current environment, medical negligence may incur great damage to a hospital. EAI can provide better medical care and avoid medical errors (Khoumbati et al., 2006). Information technology infrastructure prior to integration may not adequately allow doctors to access patient data scattered throughout various systems, which makes it difficult for the hospital to provide excellent medical services (Khoumbati et al., 2008). If a hospital faces demands to provide better medical services from its internal environment, it will be more motivated towards an information system integration because a higher level of integration can satisfy a wider variety of demands (Khoumbati et al., 2006). Therefore, we propose:
H7: The more internal pressure a hospital faces for integrating the existing systems, the higher level of EAI that will result.
Chong et al. (2009) indicate that support from high-level managers is an important factor in successfully adopting innovative technology because these individuals have the power to make decisions to provide sufficient resources (Premkumar & Roberts, 1999). Rizzoni (1991) and Premkumar and Roberts (1999) indicate that, in small enterprises, high-level managers are generally its owners and are the major decision makers; therefore, they are the important personnel who determine the enterprise’s attitudes and direction. When the level of support from top-level managers is high, their influence on the hospital will be higher, and the allocated organizational resources will be
626
Volume 36 Article 31
greater, which will make it easier for the hospital to integrate information systems, leading to a higher level of EAI. Therefore, we propose:
H8: The more top management support a hospital provides for integrating the existing systems, the higher level of EAI that will result.
In the medical industry, the relationship between the administrative staff and the doctors is extremely important (Khoumbati et al., 2006), particularly in terms of improving contemporary medical services (Davies, Hodges, & Rundall, 2003). Malvey (1981) also mention that problems with integrating HIS can be caused by conflicts between clinical doctors and administrative staff. These conflicts are a huge obstacle to integrating HIS (Khoumbati et al., 2008; Kim & Michelman, 1990). Better relationships between administrative staff and doctors represent fewer conflicts and fewer obstacles to integrating HIS. In this case, it is easier to make integrations among the information systems and the integration level will be higher. Therefore, we propose:
H9: The better relationships between administrative staff and doctors, the higher level of EAI that will result. Hospitals face external pressures in adopting innovative technologies in the form of governments’ committing to provide better medical care and closer cooperation with hospital partners technologies (Khoumbati et al., 2008). Competition increases environmental uncertainty and the demands for and the adoption of innovative technology (Chong et al., 2009; Ettlie, 1983; Ettlie & Bridges, 1982; Wang, Wan, Burke, Bazzoli, & Lin, 2005). Higher government demands for providing medical services will result in greater external pressure on hospitals, creating higher environmental uncertainty due to a fiercer competitive environment. Under such circumstances, a higher level of information system integration is necessary in order to respond to various external pressures (Khoumbati et al., 2006). Therefore, we propose:
H10: The more external pressure a hospital faces for integrating the existing systems, the higher level of EAI that will result.
When employees lack EAI-related skills, organizations look for suppliers or external advisors to help solve integration-related problems (Khoumbati et al., 2006). If an organization believes there is sufficient supplier support or third party support for adopting new technology, it will be willing to attempt to use it (Premkumar & Roberts, 1999). In addition, the outsourcing and growth of third party support will have a significant impact on whether the hospital adopts new technology (Premkumar & Roberts, 1999). In terms of information system integration, the more external support the hospital has, the easier it will be able to solve problems relating to systems integration; consequently, this will help in achieving a higher level of it. Therefore, we propose:
H11: The more external support a hospital receives for integrating the existing systems, the higher level of EAI that will result.
Sampling and Survey Instrument
Our research subjects were hospitals above the regional level as categorized by the Department of Health in Taiwan. We sampled subjects from across Taiwan in all government-assessed hospitals (462 in total) since they are considered to be high-quality hospitals. We particularly surveyed the administrative directors or the information commissioners in those hospitals.
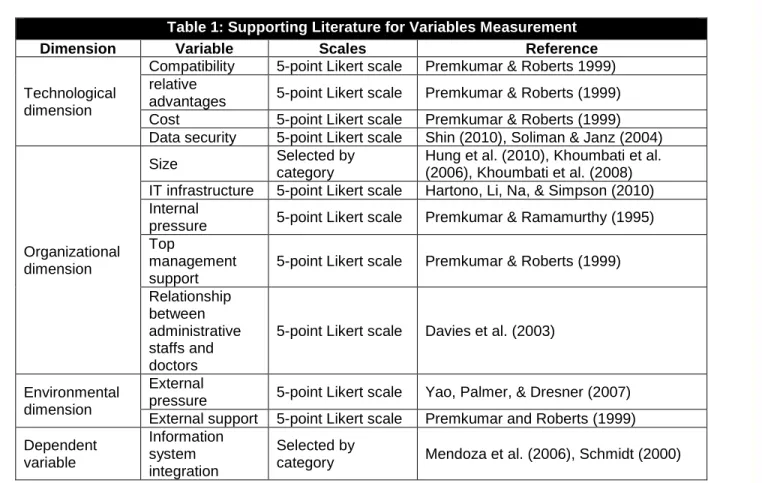
The survey questionnaire was based on a closed questionnaire design. According to our research purposes and research framework, we divided the questionnaire into three major parts. The first part concerned basic information regarding the respondent and the hospital. The second part concerned the information system integration level status quo as regarded by the hospital. The third part concerned the factors affecting the EAI. In the third part, we added EAI characteristics according to the suggestions from experts and scholars, and the characteristics of all levels of information system integration from Mendoza et al (2006) to help the respondents fill in the questionnaire. Table 1 illustrates the variable measurement methods of this study. A panel of three experts in the information management field reviewed the draft questionnaire to confirm the content and make semantic modifications if necessary. Afterwards, we invited five high-level managers from the information technology departments in various hospitals to review the questionnaire again as a pilot test to make sure that the content was not ambiguous or redundant and that the expressions were easy to understand for persons with more technical backgrounds. After this process, we distributed the questionnaire to respondents via (physical) mail.
Volume 36 Article 31
627
Table 1: Supporting Literature for Variables Measurement
Dimension Variable Scales Reference
Technological dimension
Compatibility 5-point Likert scale Premkumar & Roberts 1999) relative
advantages 5-point Likert scale Premkumar & Roberts (1999) Cost 5-point Likert scale Premkumar & Roberts (1999) Data security 5-point Likert scale Shin (2010), Soliman & Janz (2004)
Organizational dimension
Size Selected by
category
Hung et al. (2010), Khoumbati et al. (2006), Khoumbati et al. (2008) IT infrastructure 5-point Likert scale Hartono, Li, Na, & Simpson (2010) Internal
pressure 5-point Likert scale Premkumar & Ramamurthy (1995) Top
management support
5-point Likert scale Premkumar & Roberts (1999) Relationship
between administrative staffs and doctors
5-point Likert scale Davies et al. (2003)
Environmental dimension
External
pressure 5-point Likert scale Yao, Palmer, & Dresner (2007) External support 5-point Likert scale Premkumar and Roberts (1999) Dependent variable Information system integration Selected by
category Mendoza et al. (2006), Schmidt (2000)
IV. RESULTS
Questionnaire Collection
The study’s subjects were the directors from the information departments in the hospitals publicly listed above the regional level. In 2011, we distributed 462 questionnaires and collected a total of 100 copies for a return rate of 21.42 percent. After deleting 12 invalid samples (deemed so because of incomplete answers), we had 88 valid questionnaires for a return rate of 19.04 percent.
Following MacCallum, Widaman, Zhang, and Hong (1999), there is no magic number for determining how large a survey study’s sample should be. However, we believe that the sample size in our study is sufficient for conducting the statistical analysis. To gather the data, we sent the questionnaire to all government-assessed hospitals in the country and the response rate was relatively high for such an organizational-level survey. According Barrett and Kline (1981), our ratio of sample and questionnaire items may fit into the satisfactory range for a sufficient sample. Furthermore, as the literature review section shows, the model is theoretically based. As such, the sample size in this study is statistically sufficient for an analysis.
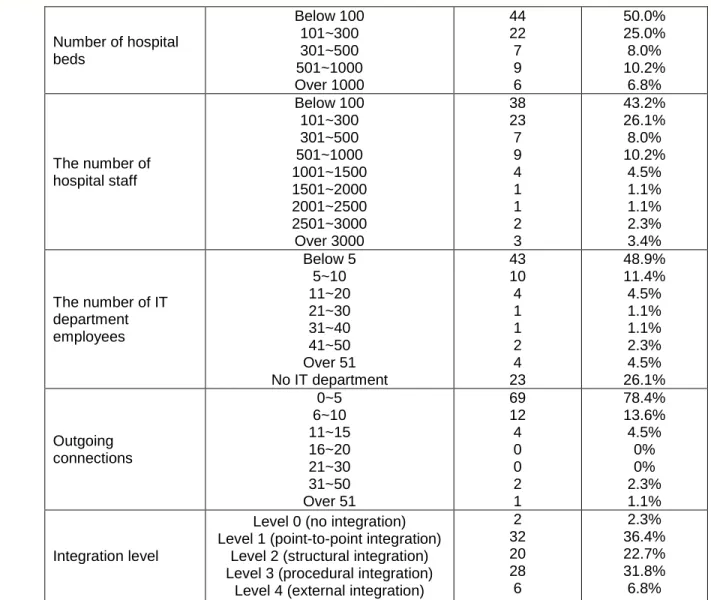
We used the SPSS 19 software program to preliminarily analyze the data. The results show that that 26 percent of the hospitals had no information technology department. The highest integration level in the hospitals occurred in point-to-point integration (36.4%), followed by structural integration (22.7%) and procedural integration (31.8%). Table 2 illustrates the hospitals’ background information.
Table 2: Demographic Results
Data Category Frequency Percentage
Hospital level Medical center Regional hospitals District hospitals 4 16 68 4.5% 18.2% 77.3%
628 Volume 36 Article 31 Number of hospital beds Below 100 101~300 301~500 501~1000 Over 1000 44 22 7 9 6 50.0% 25.0% 8.0% 10.2% 6.8% The number of hospital staff Below 100 101~300 301~500 501~1000 1001~1500 1501~2000 2001~2500 2501~3000 Over 3000 38 23 7 9 4 1 1 2 3 43.2% 26.1% 8.0% 10.2% 4.5% 1.1% 1.1% 2.3% 3.4% The number of IT department employees Below 5 5~10 11~20 21~30 31~40 41~50 Over 51 No IT department 43 10 4 1 1 2 4 23 48.9% 11.4% 4.5% 1.1% 1.1% 2.3% 4.5% 26.1% Outgoing connections 0~5 6~10 11~15 16~20 21~30 31~50 Over 51 69 12 4 0 0 2 1 78.4% 13.6% 4.5% 0% 0% 2.3% 1.1% Integration level
Level 0 (no integration) Level 1 (point-to-point integration)
Level 2 (structural integration) Level 3 (procedural integration)
Level 4 (external integration)
2 32 20 28 6 2.3% 36.4% 22.7% 31.8% 6.8%
Reliability and Validity Tests
In this study, we used Cronbach’s α to measure reliability. Cuieford (1965) suggests that a Cronbach’s α value above 0.7 suggests high reliability. A value in the range of 0.35 to 0.7 stands for a medium level of reliability, and a value below 0.35 stands for low reliability. Table 3 illustrates the original reliability results. The reliability levels of integration costs and data security were relatively lower before we deleted some question items.
Table 3: Results of Reliability Test
Variables Number of items Means Cronbach’s α
Compatibility (CP) 3 3.731 0.701
Relative advantages (RA) 4 3.849 0.806
Cost (CO) 4 3.347 0.424
Data security (DS) 5 3.482 0.615
Size (SI) 1 1.990 1.000
IT infrastructure (II) 6 3.205 0.940
Internal pressure (IP) 7 3.911 0.862
Top management support (TS) 4 3.509 0.914
Relationship between administrative staff and doctors (AD)
7 3.646 0.772
External pressure (EP) 4 3.347 0.813
External support (ES) 5 3.114 0.861
We developed the questionnaire’s theoretical basis from the literature; therefore, it has a considerable level of face validity. After we completed the draft, we had experts in the information management field review it and modify the
Volume 36 Article 31
629 content and semantics where required.. Then, we invited five senior information managers with practical experience
in hospitals to ensure the questionnaire’s content quality and, thus, improve content validity.
We took advantage of the principal component analysis and employs the varimax of the orthogonal rotation to process factors and clarify the meanings of various factors. Before factor analysis, the correlation of the variable observation values should be observed. We employed the Kaiser-Meyer-Olkin (KMO) measure and the Bartlett test to examine the appropriateness of the correlation coefficients. Hair, Anderson, Tatham, and Black (1998) point out that, if the value of KMO is smaller than 0.5, it is unsuitable for factor analysis. The analysis results of the test showed that the KMO values of the three dimensions in this study were all above 0.6.
We deleted questionable items that could not converge into a single variable and that had a factor loading below 0.6. These items included RA1, CO1, DS1, DS2 and DS5. In terms of the organizational dimension, the deleted question items included AD4, AD6, AD7, IP1, and IP3. In the environmental dimensions, we deleted ES1 because it fell into the EP variable. Table 4 shows the factor analysis after the deletion process.
Table 4: Results of the Factor Analysis
II TS ES IP AD RA EP CP DS CO II4 .846 II5 .810 II3 .802 II2 .800 II1 .795 II6 .768 TS1 .815 TS2 .760 TS4 .724 TS3 .711 ES5 .880 ES4 .855 ES3 .843 ES2 .832 IP6 .822 IP5 .672 IP4 .667 IP7 .654 IP2 .623 AD2 .820 AD3 .645 AD5 .644 AD1 .623 AD6 .602 RA2 .767 RA3 .731 RA4 .623 EP1 .735 EP3 .618 EP2 .614 EP4 .608 CP2 .789 CP3 .649 CP1 .648 DS3 .845 DS4 .838 CO4 .737 CO3 .720 CO2 .616
630
Volume 36 Article 31
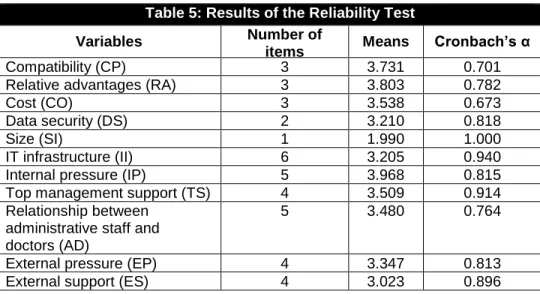
After deleting the unsuitable questions in the various dimensions, we conducted a reliability analysis to produce the results shown in Table 5. The Cronbach’s α values of the CO and DS variables were 0.673 and 0.818, respectively.
Table 5: Results of the Reliability Test Variables Number of
items Means Cronbach’s α
Compatibility (CP) 3 3.731 0.701
Relative advantages (RA) 3 3.803 0.782
Cost (CO) 3 3.538 0.673
Data security (DS) 2 3.210 0.818
Size (SI) 1 1.990 1.000
IT infrastructure (II) 6 3.205 0.940
Internal pressure (IP) 5 3.968 0.815
Top management support (TS) 4 3.509 0.914
Relationship between administrative staff and doctors (AD)
5 3.480 0.764
External pressure (EP) 4 3.347 0.813
External support (ES) 4 3.023 0.896
Normality Test
The normality test can be conducted by distributing skewness Kurtosis values. At the 0.01 significant level, if the values of skewness and Kurtosis are in the range of the normality boundary values |±2.58|, the data distribution belongs to normality (Hair et al., 1998). The values of skewness and Kurtosis of all the variables in this study were in the range of |±2.58|, which suggests that the variables in this study were of normal distribution.
Variance Homoscedasticity Test
We used Levene’s test for testing variance homoscedasticity. When the tested p-value is above 0.01, the research model is consistent with the basic assumption of variance homoscedasticity. The p-values of all variables in this study were above 0.01, which suggests that the assumption of variance homoscedasticity is true.
Multicollinearity Test
The Pearson correlation matrix can examine the multicollinearity of variables. Hair et al. (1998) state that independent variables often have the phenomenon of multicollinearity. If the correlation coefficient of any two independent variables is above 0.9, there is a high level of multicollinearity between the two variables. Table 6 shows that the correlation coefficient of any two variables was below 0.9, which suggests that this study’s variables had no serious multicollinearity.
Table 6: Results of the Correlation Coefficient
II TS ES IP AD RA EP CP DS CO
IT infrastructure (II) 1 Top management
support (TS)
.593 1
External support (ES) .057 .066 1
Internal pressure (IP) .339 .362 .081 1 Relationship between
administrative staff and doctors (AD)
.317 .516 .124 .179 1
Relative advantages (RA)
.289 .252 .118 .524 .098 1
External pressure (EP) .575 .602 .169 .403 .482 .325 1
Compatibility (CP) .478 .472 .122 .307 .273 .357 .393 1
Data security (DS) .049 .233 .019 -.017 .165 -.040 -.029 .037 1 Cost (CO) -.235 -.088 .193 .188 .067 .024 .076 -.162 -.193 1
Volume 36 Article 31
631
Independence of the Error Terms
We used Durbin-Watson statistics to test the independence of the error terms. When the Durbin-Watson value is nearly 2, the error terms are independent. The statistical value of the Durbin-Watson value in this study was close to 2, which suggests the error terms’ independence.
Regression Analysis
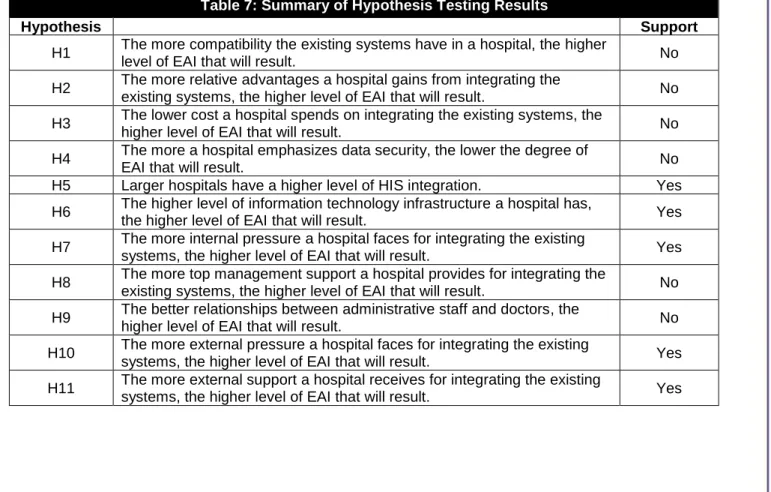
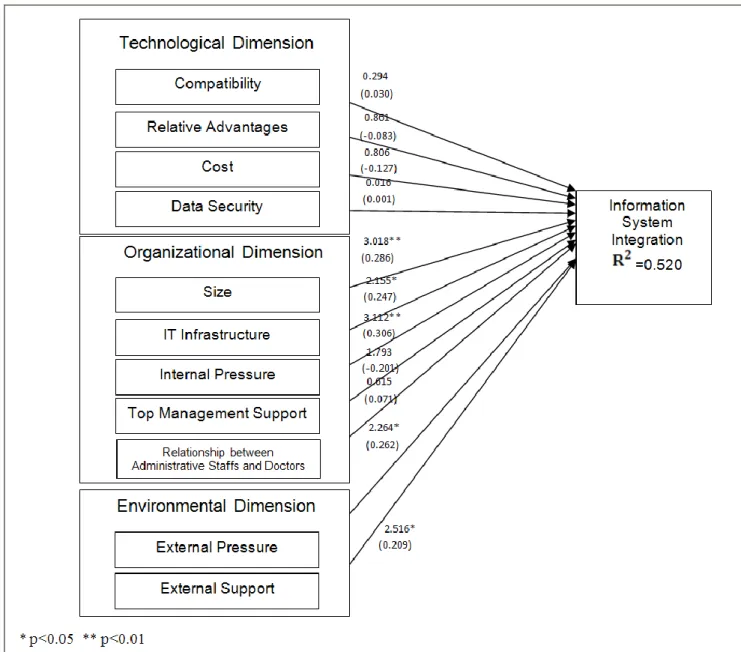
We adopted partial linear squares and smartPLS 2.0 to examine the key factors in the technological, organizational, and environmental dimensions that affect EAI integration levels. In addition, we analyzed the material relationships among the variables and assessed the model’s explanatory power. We used PLS because it is suitable for models with the small and medium-sized samples (Chin, 2001). PLS increases the explanatory variance without the need for a larger sample size (because we had 88 valid samples, PLS was suitable). We used the bootstrapping approach to estimate the path coefficient and then estimated it by using the 500 times re-sampling method that Chin (2001) proposes. Figure 2 shows the results, and Table 7 summarizes the hypothesis results.
Multivariate Analysis of Variance
We used the Multivariate Analysis of Variance (MANOVA) method to check whether hospitals at different information system integration levels had different impacting factors on their EAI level. In terms of the MANOVA homogeneity test results, the BOX M value was 160.246. The F statistic after conversion from the BOX M value was 0.949 and the significance testing p-value was 0.648. These results are not at the significance level, which means that 11 variables at four integration levels did not violate the MANOVA’s homogeneity assumptions.
Furthermore, the Wilks' Lambda (p-value = 0.01) was below 0.05 at the significance level, which suggests that at least one of 11 variables significantly varied at different integration levels.
Table 7: Summary of Hypothesis Testing Results
Hypothesis Support
H1 The more compatibility the existing systems have in a hospital, the higher
level of EAI that will result. No
H2 The more relative advantages a hospital gains from integrating the
existing systems, the higher level of EAI that will result. No H3 The lower cost a hospital spends on integrating the existing systems, the
higher level of EAI that will result. No
H4 The more a hospital emphasizes data security, the lower the degree of
EAI that will result. No
H5 Larger hospitals have a higher level of HIS integration. Yes H6 The higher level of information technology infrastructure a hospital has,
the higher level of EAI that will result. Yes
H7 The more internal pressure a hospital faces for integrating the existing
systems, the higher level of EAI that will result. Yes H8 The more top management support a hospital provides for integrating the
existing systems, the higher level of EAI that will result. No H9 The better relationships between administrative staff and doctors, the
higher level of EAI that will result. No
H10 The more external pressure a hospital faces for integrating the existing
systems, the higher level of EAI that will result. Yes H11 The more external support a hospital receives for integrating the existing
632
Volume 36 Article 31
Figure 2. The Structural Model Path Analysis Diagram
Table 8 illustrates the results of the effect items among subjects; namely, the univariate analysis results of the 11 variables for different levels of integration. It indicates that all variables except for the AD (relationship between administrative personnel and doctors), DS (data security), and CO (integration cost) reached the significance level (p value = 0.05). In other words, the remaining eight variables affected inter-level relationships in EAI.
Table 8: The Result of Multivariate Analysis of Variance (MANOVA) Independent
variable Dependent variable df
Average sum of squares f-value p-value Integration level Compatibility 4 1.129 3.886 0.006 Relative advantages 4 0.924 2.717 0.035 Cost 4 0.232 0.489 0.743 Data security 4 0.123 0.255 0.906 Size 4 7.248 5.371 0.001 IT infrastructure 4 4.827 9.821 0.000 Internal pressure 4 0.848 4.279 0.003
Top management support 4 1.510 3.617 0.009
Relationship between administrative staff and doctors
Volume 36 Article 31
633
External pressure 4 2.154 8.858 0.000
External support 4 1.681 2.652 0.039
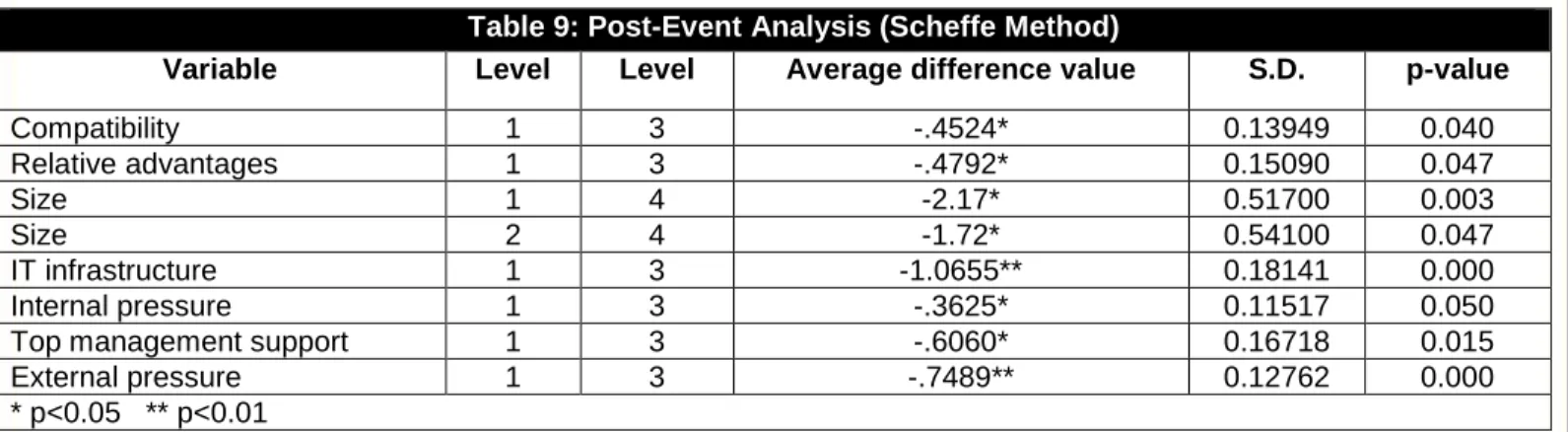
Table 9 illustrates the post-event pairwise comparison, which we conducted by using the univariate Scheffe method. If the differences in the variable averages of the two level groups reached the significance level when the p-value was smaller than 0.05, then the average difference value in the average difference column is marked with the symbol “*”. When the differences reached the significance level when the p-value was smaller than 0.01, the average difference value is marked with the symbol “**”. Table 9 shows only the values that reached significant levels (marked with “*” or “**”). For example, in terms of relative advantages, the result from the sample in level 1 was significantly lower than the result from the sample in level 3. In other words, the factor of relative advantages was decisive when hospitals considered upgrading their integration level from 1 to 3. However, this factor may not be critical when hospital considers upgrading from level 1 to 4, where the factor of size was the only decisive factor. In terms of integration, level 4 may be costly for hospitals since they need to be highly integrated both internally and externally. For this reason, large hospitals may have both the need and the capability (e.g., budget) to embrace the level 4 integration.
Table 9: Post-Event Analysis (Scheffe Method)
Variable Level Level Average difference value S.D. p-value
Compatibility 1 3 -.4524* 0.13949 0.040 Relative advantages 1 3 -.4792* 0.15090 0.047 Size 1 4 -2.17* 0.51700 0.003 Size 2 4 -1.72* 0.54100 0.047 IT infrastructure 1 3 -1.0655** 0.18141 0.000 Internal pressure 1 3 -.3625* 0.11517 0.050
Top management support 1 3 -.6060* 0.16718 0.015
External pressure 1 3 -.7489** 0.12762 0.000
* p<0.05 ** p<0.01
V. DISCUSSION
The Technological Dimension
“Compatibility” has no significant impact on the EAI level. As such, we can infer that, regardless of hospitals’ integration stage, they believed that their current integration met their objectives and that the changes in the integration caused no major problem at all.
We found that “relative advantage” had no significant impact on the EAI level, which is inconsistent with findings obtained from the previous studies. Since hospitals are frequently non-profit organizations, they may pay less attention to the competition in comparison with other kinds of industries. In addition, EAI is already perceived as an essential tool for integrating a variety of applications in hospitals and improving the quality of their information services (Lian, Yen, & Wang, 2014). Therefore, enhancing the competitive advantage may not be considered to be a causal factor for the hospitals to adopt EAI. In other words, they adopt EAI for systems integration despite the fact that the resulting adoption may or may not create a relative advantage over their competitors.
In addition, “cost” did not have a significant impact on the EAI level. One possible reason for this finding may be that the medical service industry spends only one fifth of its operational budget on information technologies compared with other types of industries. In fact, the expenditure of healthcare organizations on information technologies only accounts for 2 percent of the total budget, while other industries spend about 10 percent (Lang, 2003). These numbers may indicate that IT investment in the medical service industry is relatively lower than it is in other industries. When a hospital invests more in EAI, this may cause less long-term financial burden for the hospital. Furthermore, investing in EAI usually costs much less than investing in a new HIS. Thus, while hospitals are used to investing large amounts of money in HIS, investing in EAI seems to be a relative smaller financial concern. Furthermore, when hospitals have implemented more HIS, integrating various kinds of systems becomes an imperative action. As such, for these reasons, the cost of adopting EAI may not be a significant factor.
In the technological dimension, “data security” had no significant impact on the EAI integration level, possibly because the HIS are planned with patients at the core. Therefore, regardless of the integration degree at various levels, data security, particularly patient privacy, is the main concern (Chang et al., 2009). Moreover, users’ behavior on HIS is carefully regulated because only strictly managed accounts can access certain kinds of data. Regardless of the EAI integration level, hospitals take data security seriously.
634
Volume 36 Article 31
The Organizational Dimension
Regarding the organizational dimension, “size” had a significant positive impact on the EAI level. In other words, larger hospitals were more likely to integrate HIS. This finding is consistent with previous studies that show larger hospitals have more distributed systems, have more need to distribute data to various systems, and more need to integrate HIS for better economies of scale (Hung et al., 2010).
”IT infrastructure” also had a significant positive impact on the EAI integration level. This result verifies that a basic information technology infrastructure is one of the necessary conditions to successfully introduce new technologies (Applegate et al., 1999). Hospitals with higher integration levels have better information technology infrastructures, which drive them to integrate HIS.
“Internal pressure” had a significant positive impact on the EAI level. This suggests that hospitals at a higher integration level may perceive internal pressure more significantly compared to hospitals with a low integration level. There is more internal need to speed up the internal data transmission process and to reduce the waiting times of the patients in such hospitals. Therefore, the hospital’s IT department will be required to integrate internal information systems in order to meet the internal needs of the hospital and enhance overall medical service quality. However, “top management support” had no significant impact on the EAI level, possibly because top management will support what is beneficial to the organization in enhancing its competitive edge regardless of the organization or industry. In Taiwan’s healthcare system, hospitals’ top management (such as the president or vice presidents) commonly possess medical degrees and backgrounds/experiences. Therefore, they may not be deeply involved in the information technology-related decisions and fully understand the associated information technology-related issues. Consequently, they may rely heavily on the recommendations and assessment of/from the information technology departments.
“Relationships between administrative staffs and doctors” had no significant impact on EAI levels. We can infer that doctors and administrative personnel have to maintain good relationships regardless of the EAI level. In hospitals, each sub-division has to work and communicate with other divisions seamlessly (e.g., in the case of communicating with medical treatments across various departments) to avoid possible errors.
The Environmental Dimension
In terms of the environmental dimension, “external pressure” had a significant impact on the EAI level. Nolan (1973) notes that the maturity of an organization’s computer systems stems from efficient support for daily operations in order to maintain competitiveness in the industry. If clients complain about long waiting times or complex referral procedures, they are more likely to express dissatisfaction or turn to other hospitals. Hospitals attempt to satisfy patient needs and gain a leading advantage over competitors while retaining patient loyalty, and this often results in adopting EAI. The findings of this study are similar to those of other studies, which suggest that competition increases environmental uncertainties and demands on innovative technology (Chong et al., 2009; Ettlie, 1983; Ettlie & Bridges, 1982; Wang et al., 2005).
Finally, “external support” also had a significant impact on the EAI level. If organizations believe that sufficient numbers of suppliers or third parties support a new technology, they are more willing to implement it. The penetration of outsourcing and the growth supported by third parties both have a significant impact on new technology (Premkumar & Roberts, 1999).
VI. CONCLUSIONS
In the past, hospitals have developed different types of systems to deal with the operational procedures performed in various departments. Nowadays, hospitals provide more healthcare-related activities, and more information systems have been implemented. Therefore, hospitals are now facing the problem that data cannot be shared easily across different types of systems. EAI seems to be a reasonable solution to this problem. However, there has been limited empirical work on determining what factors influence whether hospitals adopt EAI. In this study, we examined the key factors affecting whether hospitals adopt EAI, particularly in the technological, organizational, and environmental dimensions. The data analysis results show that IT infrastructure, size, external pressure, internal pressure, and external support significantly affected EAI adoption levels. These critical factors provide substantial aid and advice for academics and practitioners. Hospital managers could make appropriate decisions to improve the integration of information systems by referring to these findings. Recently, research that is based on multiple perspectives of adopting innovation clearly deserves academic attention, especially when such a trend has been noticed in hospital studies in recent years. This study extends the body of knowledge and contributes to the provision of better healthcare services. Table 10 summarizes several previous studies that are similar to this one and contrasts their empirical results. These studies were based on the TOE framework or focused on EAI adoption.
Volume 36 Article 31
635 With this study, we uncovered that "hospital size" and "external pressure" were critical factors affecting hospitals’
EAI adoption, and this result is in line with prior studies. In other words, the bigger the hospital is, the more its need for EAI. Similarly, the stronger the competition is, the more the hospital’s willingness to adopt EAI in order to increase efficiency to meet the fierce competition in the market. Results of both "IT infrastructure" and "internal pressure" are confirmed by most of the prior studies. Since EAI in the subject hospitals has the function of integrating internal and fundamental systems, it is of no surprise that these two factors are significant.
One surprising result of this study was with "external support", which has not been tested frequently in the past TOE or EAI studies but has proved to be a significant factor in our research. Because of the existence of various kinds of information systems and/or applications in hospitals, such as systems for medicals records, surgery, websites, and patient relationship management, it is almost impossible for a hospital's IT department to master all the different systems/applications. Thus, hospitals are different from other organizations in the business world and tend to seek IT support from external agencies. The IT department in a hospitals acts as a bridging role between the agencies and the hospital when the hospital is adopting certain kinds of systems/technologies. As such, we can see that "external support" is a decisive factor for EAI adoption in hospitals.
All factors in the technological dimension were insignificant, a finding that is inconsistent with the results of most past TOE and EAI studies. In the real world, hospitals have been trying to integrate all kinds of systems, and, further they generally categorize these integrated systems as HIS (healthcare information systems). Thus, regardless of the technological concerns, hospitals may already be adopting EAI to integrate their existing systems. Not surprisingly, technology-related factors have proved to be insignificant.
As for “top management support”, this study’s results show that it was not a significant factor, a finding also different compared with past studies. Since the EAI techniques focused on in this study are relatively low level, the decision making power is frequently decentralized to a lower level of management. This may be one reason why "top management support" was not a significant factor. Regarding the factor of "relationship between administrative staff and doctor, the result shows that this kind of relationship was not so critical in encouraging hospitals to adopt EAI.
Table 10. Comparison between Current and Prior Studies This study Hung et al. (2010) Lian et al. (2014) Cao, Jones, & Sheng (2014) Khoumbati et al. (2006) Mantzana et al. (2008) Kamal, Hackney, & Ali (2013) Research topic Variable CRM adoption based on TOE Cloud computing based on TOE Hospital RFID based on TOE EAI adoption in healthecare (qualitative study) EAI adoption in healthecare (qualitative study) EAI adoption in local government Technological dimension Relative advantage □ ✓ □ ✓ Compatibility □ ✓ □ ✓ Data security □ ✓ ✓ ✓ ✓ Costs □ □ ✓ ✓ ✓ Organizational dimension Hospital size ✓ ✓ ✓ ✓ ✓
Top management support □ ✓ ✓ ✓
IT infrastructure ✓ ✓ ✓ ✓
Internal pressure ✓ ✓ ✓
Relationship between administrative
staff and doctors
□ ✓ ✓
Environmental dimension
636
Volume 36 Article 31
External support ✓
Note: □: this variable was mentioned in the study; ✓: this variable was statistically significant in the study.
Implications of Research
This study’s findings have the following management implications for hospitals. First, this study identifies five factors that have a significant impact on EAI integration. These provide a guideline for hospitals when considering integrating information systems. Second, because small hospitals face increasing competitive market pressure, they need to invest in and strengthen the construction of their information technology infrastructure to enhance their competitiveness. Moreover, when the EAI level is higher, the diagnostic decision making quality of doctors will also be higher. Enhancing healthcare quality could directly affect patient confidence and their degree of satisfaction with a hospital. Hence, for a hospital’s long-term operational strategy, doctors should be aware of the importance and significance of adopting EAI and demonstrably support it. Finally, the adopting EAI can help to reduce medical malpractice. When carrying out relevant risk control, hospitals should consider adopting EAI.
This study’s findings provide information system suppliers with practical implications. Accordingly, “external support” had a significant impact on the EAI level. Providing explicit and clear explanations of the advantages and benefits of system integration to hospital staff by information system integration service providers will improve the willingness to integrate information systems and further affect the integration level. Technological service providers should also understand the impact factors of EAI based on this study’s findings. It should help them to adjust advertising or promotional activity strategies and provide them with reference information to demonstrate the potential of system integration to hospitals. Since small hospitals are limited in funding, information system suppliers may help them improve the information system integration level in terms of their demands and resources. Finally, since hospitals lack information technology personnel, information system suppliers should provide more technological assistance and hold training courses to reduce resistance from users after system integration.
This study’s finding have the following implications for government authorities. According to the results, “external pressure” significantly affects EAI levels. Because healthcare services are highly relevant to people’s lives, any mistake or omission may lead to irreparable loss. Government authorities should continuously encourage hospitals to upgrade their information system integration levels. This would not only reduce the social costs of medical risks but also ensure the timeliness and accuracy of medical information. In addition, government authorities could periodically hold seminars and invite speakers from hospitals with higher information system integration levels to share their practical experiences and achievements. Hospitals with less IT development could learn more from these events.
Limitations and Future Research
The research subjects in this study were information department supervisors, directors of healthcare organizations, or staff who were responsible for managing information technologies. We made efforts to reach respondents who knew the information systems in the hospitals, but there is no guarantee that all respondents were the best persons. Moreover, we only adopted the survey approach to test the key factors. Future studies could conduct interviews with the relevant directors regarding the differences (e.g., organizational change issues) before and after adopting EAI. Follow-up studies could also compare performances before and after adopting of EAI to examine whether various levels of EAI would result in different kinds of benefits. Future research could also conduct case studies regarding EAI in other countries to learn useful lessons for achieving successful integration under different circumstances. Higher levels of EAI integration may result in higher degrees of interoperability, which has its own key challenges. First, to achieve higher interoperability, entities should completely agree on standards (Brailer, 2005). Secondly, early adopters with the negative network externalities and first-mover disadvantages may find it difficult to synchronize with the behavior of the market (Raghupathi & Tan, 2008). Since we did not include the degree of interoperability in this study, future study could take this issue into account as a new dimension to gain additional insight.
REFERENCES
Editor’s Note: The following reference list contains hyperlinks to World Wide Web pages. Readers who have the ability to access the Web directly from their word processor or are reading the paper on the Web, can gain direct access to these linked references. Readers are warned, however, that:
1. These links existed as of the date of publication but are not guaranteed to be working thereafter.
2. The contents of Web pages may change over time. Where version information is provided in the References, different versions may not contain the information or the conclusions referenced.