ADOPTING THE HEALTHCARE FAILURE MODE AND EFFECT ANALYSIS
TO IMPROVE THE BLOOD TRANSFUSION PROCESSES
Chao-Ton Su
1,*, Chia-Jen Chou
1, Sheng-Hui Hung
2, Pa-Chun Wang
2,3,41 Department of Industrial Engineering and Engineering Management, National Tsing Hua University, Hsinchu 30013,
Taiwan, R.O.C.
*Corresponding author. Email: ctsu@mx.nthu.edu.tw
2 Quality Management Center, Cathay General Hospital, Taipei 10630, Taiwan, R.O.C.
3 Fu Jen Catholic University School of Medicine, Taipei County 24205, Taiwan, R.O.C.
4 Department of Public Health, China Medical University, Taichung 40402, Taiwan, R.O.C.
The aim of this study is to conduct the healthcare failure mode and effects analysis (HFMEA) to evaluate the risky and vulnerable blood transfusion process. By implementing HFMEA, the research hospital plans to develop a safer blood transfusion system that is capable of detecting potentially hazardous events in advance. In this case, eight possible failure modes were identified in total. Regarding the severity and frequency, seven failure modes were identified to have hazard scores higher which are than 8. Five actions were undertaken to eliminate the potential risk processes. After the completion of HFMEA improvement, from the end of July, 2008 to December 2009, two adverse events occurred during the blood transfusion processes and the error rate is 0.012%. The HFMEA proves to be feasible and effective to predict and prevent potentially risky transfusion processes. We have successfully introduced information technology to improve the whole blood transfusion process.
Key Words:
healthcare failure mode and effect analysis (HFMEA), blood transfusion, hazard score.1. INTRODUCTION
Reducing medical errors for a given healthcare process is critical to patient safety. Traditionally, risk assessment methods in healthcare have analyzed adverse events individually. However, risk-evaluated approaches should reflect healthcare operations, which are usually composed of sequential procedures. In other words, a systematic and process-driven programming of risk prevention is necessary for every healthcare provider. Many studies have illustrated the necessities to introduce risk analysis method in preventing the medical error ((Bonnabry et al., 2006); (Bonan et al., 2009)).
Healthcare Failure Mode and Effect Analysis (HFMEA) is a novel technology used to evaluate healthcare processes proactively. HFMEA was first introduced by the Department of Veterans Affairs (VA) System and developed by the National Center for Patient Safety (NCPS) in the United States. HFMEA is a hybrid risk evaluation system that combines the ideas behind Failure Mode and Effect Analysis (FMEA), Hazard Analysis and Critical Control Point (HACCP), and the VA’s root cause analysis (RCA) program. An interdisciplinary team, process and subprocess flow drawing, identification of
failure mode and its cause, a hazard scoring matrix, and a decision tree to determine system weakness are usually included in HFMEA. Currently, the HFMEA method is encouraged by the American Society for Healthcare Risk Management for hospitals in the United States (Gilcheist et al., 2008).
Clinical researches have identified blood transfusion as a significant risky process (Klein, 2001; Rawn, 2008). Errors in blood transfusion result in immediate and long-term negative outcomes including the increase chance of death rates, stroke, renal failure, myocardial infraction, and infection, among others. Therefore, reducing the risks of blood transfusion is a major patient safety issue for all hospitals. The blood transfusion process is setting on top of the list for process analysis, since the process affects a large number of patients and the procedure is complex in nature (Burgmeier, 2002). Linden et al. (2002) indicated that the blood transfusion is a complicated system involving the hospital blood bank, patient floor, emergency department, operating room, transfusionist, and transporter. A more comprehensive and risk proactive analysis of the blood transfusion process is necessary to improve patient safety.
A series of transfusion-related adverse events take place in the research hospital have urged the Patient Safety Committee to take decisive actions to prevent harmful medical errors resulted from transfusion-related processes. An efficient risk prevention method was anticipated to reduce the number of adverse blood transfusion events at the research hospital. The aim of this study is to conduct the HFMEA to evaluate the risky and vulnerable blood transfusion process. By implementing HFMEA, the research hospital plans to develop a safer blood transfusion system that is capable of detecting potentially hazardous events in advance.
2.
REAL-LIFE EXAMPLE
2.1. Setting
The research was conducted in the Cathay General Hospital, a 600-bed, university-affiliated, tertiary referral acute care medical center located in downtown Taipei, Taiwan. The study was approved by the IRB of the Cathay General Hospital.
2.2. Composition of the HFMEA team
Led by the Vice Director of the Clinical Laboratory Department, a multi-disciplinary team was organized following the guidelines of HFMEA as described in the U.S. Department of Veterans Affairs’ HFMEA toolkit (Derosier et al., 2002). The team consists of 10 members from 6 departments, including the quality management center, information technology department, nursing department, clinical laboratory department, blood transfusion committee, and dispatch center, worked under the supervision of 2 external process engineers from the National Tsing Hua University.
2.3. Time Period
This study was divided into three stages, namely, planning, execution, and follow-up. A one and a half hour meeting was held per month. A total of 12 meetings require more than 180 man-hours.
1. Planning phase (from July, 2007 to August, 2007)
addition, the multidisciplinary team was also organized during this phase. 2. Execution phase (from September, 2007 to June, 2008)
This phase focused on drawing a detailed blood transfusion process, constructing the failure modes and identifying their causes, determining hazard scores, deciding on recommendation actions, and recognizing responsible departments.
3. Follow-up phase (from July, 2008 to December, 2009)
The blood transfusion error rate is the most critical index proving the effectiveness of the HFMEA project. The blood transfusion committee worked continuously to monitor the error rate and to make sure that its trend was stable.
2.4. HFMEA Procedure
The HFMEA procedure used to examine potential failures in the blood transfusion was adopted from the HFMEA guidelines (Derosier et al., 2002). More application of detailed HFMEA procedure could be found in ((Esmail et al., 2005); (Linkin et al., 2005); (Van Tilburg et al., 2006); (Habraken et al., 2009)). Followings are the key steps description of the HFMEA process:
Step 1. Define the HFMEA topic. Step 2. Assemble the team.
Step 3. Graphically describe the process Step 4. Conduct a hazard analysis. Step 5. Actions and outcome measures
2.5. Process description
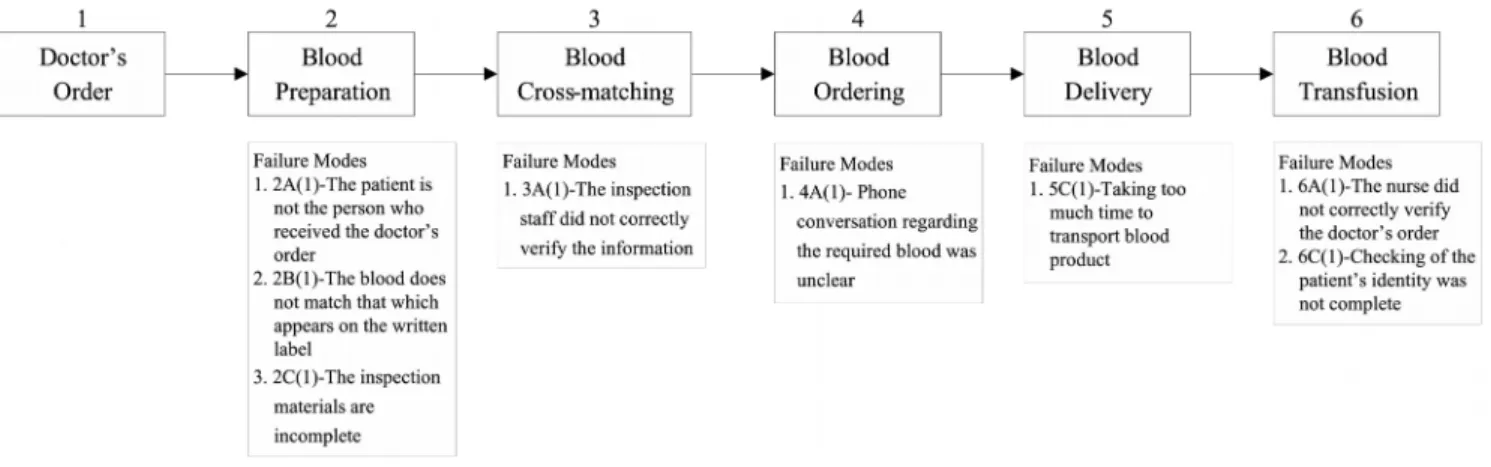
The process of blood transfusion was divided into six main phases: doctor’s order (prescription), blood preparation, cross-matching, blood ordering, blood delivery, and blood transfusion. Figure 1 illustrates the detailed steps of blood transfusion.
Step1: Doctor’s Order
The doctor first checks the patient information and gives professional order, which includes the blood transfusion request form, blood testing form, blood product, and blood quantity. Then the nurse double checks the blood product, blood quantity, and the patient’s ID per doctor’s order. The nurse then brings the essential items to the location of the patient. Step 2: Blood Preparation
Before extracting the blood, two nurses double check the information of the identity of the patient. These pieces of information include the name, ID, date of birth, medical record number, and blood type at the bedside. The information is provided by the patient himself or can be seen on his bracelet. Next, the nurses write the bed number, date, name, blood type, and the name of the transfusionist on the blank label. The nurses then confirm and append to the blood transfusion request form. Before preparing to send for the cross-matching operation, the blood transfusion request form, blood testing sheet, and specimen should be completed. Finally, the request form is sent to the blood bank by air shoot (urgent dispatch) or transporter.
Step 3: Blood Cross-matching
The blood bank staff will sign for the specimen receipt and reconfirm the data, which includes the blood transfusion request form, blood testing form, and basic information on the patient’s specimen. The inspection staff will then sign the blood testing form and print out the receipt of signature label. The blood transfusion request form, specimen label, and signature label are then rechecked before the cross-matching operation is performed. If the required data are correct, the cross-matching operation will be implemented. Given the results, the nurses will verify whether those results match the blood type of the patient. The nurse will then double check the blood transfusion request form, specimen label, the receipt of signature label, and the cross-matching results.
For the cross-matching report to be issued, the verification of the signature label and the information about the patient should be accomplished first. The nurses will then enter the inspection report into the laboratory information system (LIS); the LIS will check if the inspection results indeed match the blood type of the patient. In addition, the nurses will enter information on the required blood into the computer. The blood preparation operation is completed.
Step 4: Blood Ordering
The unit requiring blood gives a notice to the blood bank by telephone and issues a blood release form to the dispatch center by air shooter. The blood bank staff will key in the patient’s medical record number that was provided by the nursing staffs into the LIS. Next, the blood bank staff confirms the patient’s name and blood type with the nurses. The blood bank staff then keys in the information, which includes the bed number, blood product, and blood quantity into the computer according to the provided information. Finally, the blood bank staff will prepare the blood and cross check again, after that, the nurses will scan the bar code on the blood pack into the computer, and the LIS will automatically verify the blood product, blood type, blood quantity, and print out the blood release form. After the dispatch center receives the blood release form, the staff will verify the blood product, the bed number, blood type, and the patient’s medical record number. Next, the courier will prepare to transport the blood.
Step 5: Blood Product Delivery
transfusion request form. The blood bank staff then puts the blood into the thermal insulation package. Next, the courier brings the receipt of signature form and the blood release form, which had been charged to transport the blood. Before the blood is taken, the blood bank staff will verify the blood release form, blood transfusion request form, receipt of signature form, and the data on the plastic bag. Finally, the escort takes the blood product to the unit requiring blood.
Step 6: Blood Transfusion
Before transfusing the blood, the nurses not only check whether the blood appears strange (that is, if there is clotting, bubbling, breakage, or discoloration), but also verify the doctor’s order, blood type, quantity, and blood transfusion request form. Next, the nurses then warm up the blood under 37˚ C for 10-20 minutes, if necessary, to check the patient’s bed number, blood type, and patient name on the blood bag. The nurses double check the patient’s identity which included name, ID, birth date, and blood type at the bedside. The blood transfusion is then performed. The procedure begins with the exhaustion of the cannula, followed by determining the size of the needle tip (the drip speed depends on the patient’s situation). The last step is the change of the cannula based on the time or actual situation. During the transfusion, the nurses will observe the condition of the patient and record patient’s response. After giving the feedback on the performed procedure, the whole process is considered completed.
2.6. Evaluation
Because of the implementation of HFMEA, there has been only two adverse events occurred in the blood transfusion process through 2009. Those action plans will be proliferated to the entire Cathay Healthcare System hospitals, including the Cathay General Hospital, Sijhih Branch, Hsinchu Branch, and the Cathay Neihu Clinic in order to ensure the safety of all patients. There are additional benefits for the implementation of this HFMEA project. The data collected through the PDA system, such as blood transport time, blood injection time, and blood returned rate proved to be useful in evaluating the efficiency of the blood transfusion process. The users (the satisfaction was 34.7%) felt the improvements were helpful in the handling of their daily work.
3.
RESULTS
Data Collection
The period allotted for data collection was from 2005 to 2009. A total of 58,933 blood transfusion processes were performed during this investigation (13,261 in 2005, 12,013 in 2006, 11,306 in 2007, 10,795 in 2008 and 11,558 in 2009). The number of adverse events in these blood transfusion procedure was 19 (4 in 2005, 2 in 2006, 11 in 2007, 0 in 2008 and 2 in 2009) for a defect rate of almost 0.032%.
3.2. Failure Modes and Analysis of Causes
The HFMEA team analyzed the blood transfusion process in detail. It was able to identify eight possible failure modes (see Figure 2). In addition, the team analyzed the severity and probability of each failure mode and determined the relevant recommendation actions. Table 1 illustrates the deployment of the decision tree to determine whether the recommended
actions are necessary or not.
Figure 2. Failure Modes of Blood Transfusion ProcesS
By brainstorming, the team summarized that there were 18 possible causes that could result in these eight failure modes. In addition, the analyzed results of the decision tree showed that there were nine possible causes that needed to be addressed. The team decided to submit six of recommendation actions to hospital management for approval. Finally, five out of the six recommendation actions were selected for initial implementation of improvement campaigns.
Table 1. HFMEA Analysis of the Blood Transfusion Process
HFMEA Step 4 – Hazard Analysis HFMEA Step 5- Identify Actions and Outcomes
Failure Modes:
First evaluation failure mode before determining potential causes Potential Causes Se ve ri ty Pr ob ab ili ty H az ar d Sc or e S in gl e Po in t W ea kn es s? E xi st in g C on tr ol M ea su re ? D et ec ta bl e? Pr oc ee d? Action Type (Control, Accept, Eliminate) or Rationale for Stopping Action Outcomes Measure Pe rs on R es po ns ib le
2A(1) The patient is not the person who received the doctor’s order C at . O cc . 12 N N Yes 2A(1) a
The patient was inarticulate M
i. U n. 2 Y N Y No 2A(1) b
The nurses did not listen well M
i. U n. 2 N No 2A (1) c
The nurse did not see the contents of bracelet well
C
a.
O
c.
12 N N Yes Control
1. Enforcement of nurse education training 2. Ask the nurse to do thorough verification
of vital information The incorrect rate of identifying patient Nurse department 2A(1) d
The identifications in the bracelet were not clear
C
a.
R
e.
4 Y N Y No
2B(1) The blood does not match the description on the label of tube
C
a.
F
r. 16 N N Yes
a
label to the tube
1. They labeled the wrong test tube
2. They attached the wrong blood requisite form 3. They wrote incorrect data on
the label
Eliminate
procedure (SOP) of blood transfusion 2. Retraining the nurses
3. Verify the patient’s bracelet, blood testing form, and preparation of blood transfusion label through the PDA
rate of label department 2. Blood transfusion committee 3. Medical information center 2B(1) b
The nurses poured the blood into the wrong test tube
C a. O c. 12 N N Yes Control & Eliminate
Same as above Same as above Same as above
2C(1) The inspection materials are incomplete
M
o.
F
r. 8 N N Yes
HFMEA Step 4 – Hazard Analysis HFMEA Step 5- Identify Actions and Outcomes
Failure Modes:
First evaluation failure mode before determining potential causes Potential Causes Se ve ri ty Pr ob ab il ity H az ar d Sc or e Si ng le P oi nt W ea kn es s? E xi st in g C on tr ol M ea su re ? D et ec ta bl e? Pr oc ee d? Action Type (Control, Accept, Eliminate) or Rationale for Stopping Action Outcomes Measure Pe rs on R es po ns ib le 2C(1) a
The nurses did not verify the data of the specimen and dispatched such to the blood bank M o. F r. 8 N N Yes Eliminate Control
1. Modify the standard operation procedure (SOP) of blood transfusion (double-check and sign)
2. Retraining the nurses
The incorrect rate of checking blood 1. Nursing department 2. Blood transfusion committee
3. Verify the specimen through the PDA before sending it to the blood bank
transfusion data 3. Medical information center 2C(1) b
The nurse did not know that the blood transfusion request form, the blood testing form, and the specimen were all required
M o. R e. 2 N No 2C(1) c
The specimen was losing during the transport M i. U n. 2 N No 2C(1) d
The inspection staff received the specimen but did not notice the incorrectness M i. U n. 2 N No
3A(1) The inspection staff did not correctly verify the information C a. F r. 16 N N Y Eliminate Control
1. Use of PDA to scan blood bag, blood transfusion request form, blood release form before blood is released
2. Printing the label to be stuck on the blood bag Discrepancy rate of specimen and label 1. Blood transfusion committee 2. Blood bank 3. Medical information center 4A(1) Phone conversation
regarding the required blood was unclear
M o. F r. 8 N N Yes 4A(1) a
The unit requiring blood did not clearly articulate the essential information about the required blood
M
o.
F
r. 8 N N Yes Control 1. Cancellation of the order blood by
telephone
2. Ordering blood on-line
Incorrect rate of blood product 1. Blood bank 2. Nursing department 3. Medical
information center
HFMEA Step 4 – Hazard Analysis HFMEA Step 5- Identify Actions and Outcomes
Failure Modes:
First evaluation failure mode before determining potential causes Potential Causes Se ve ri ty Pr ob ab ili ty H az ar d Sc or e S in gl e Po in t W ea kn es s? E xi st in g C on tr ol M ea su re ? D et ec ta bl e? Pr oc ee d? Action Type (Control, Accept, Eliminate) or Rationale for Stopping Action Outcomes Measure Pe rs on R es po ns ib le 4A (1) b
The blood bank staff did not concentrate
M
o. Fr.
8 N N Yes Control
Same as above Incorrect rate
of inspection report
As above
5C(1) Taking too much time to transport blood product
M i. F r. 4 N No 5C(1) a
It took too much time to wait for the elevator
M i. F r. 4 N No 5C(1) b
The nursing staff spent too much time for transporting
M
i.
F
r.
4 N No
6A(1) The nurse did not thoroughly verify the doctor’s order
M
a.
O
c. 9 N N Yes
6A(1) The nurse did not indeed check M
a.
O
c.
a the doctor’s order
procedure (SOP) of blood transfusion (double-check the doctor’s order )
2. Retraining the nurses
verifying doctor’s order
Department
6A(1) b
The nurse was too tired to check the data M a. R e. 3 N No
6C(1) Checking of the patient’s identity was not complete
O a. F r. 16 N N Yes 6C(1) a
The nurses did not follow SOP when they verified the blood transfusion data O a. F r. 16 N N Yes Eliminate Control
1. Modify the standard operation procedure (SOP) of blood transfusion
2. Retraining the nurse
3. Verification the label on the blood bag by the PDA
Incorrect rate of blood transfusion 1. Nursing department 2. Blood transfusion committee 3. Medical information center Ca.: catastrophic; Ma.: major; Mo.: moderate; Mi.: minor; Fr.: frequent; Oc.: occasional; Un.: uncommon; Re.: remote.
3.3. Recommendation Actions
Action plan 1: online blood product ordering system
To reduce transcription errors and mistakes caused by miscommunication on the telephone, our team proposed the improvement action by establishing an online blood product ordering system, which was completed in April, 2008. The blood-requiring unit is asked to send the request of blood products, including blood type and transfusion time through the system. After the request is submitted, the system will simultaneously message the blood bank via personal handyphone system (PHS).
Action plan 2: adhere patient information label on the individual blood product package.
To avoid the blurred identification of the blood product package, the blood bank staff used a water-proof printed, instead of a hand-written patient/blood information sticker, which displays the patient name, blood type, bar code, and date. The printed stickers are placed on both the blood product package and the plastic bag, which is wrapped outside of the package.
Action plan 3: employ a PDA to prevent patient identification error.
This action used a PDA (Team Pad 500G, FUJITSU, Kawasaki, Japan; work on Windows CE, .NET platform.) to match the information on a patient’s wrist band (bracelet bar code) and the sticker on blood product package. Before the transfusion, the nurse uses PDA to confirm patient identification by scanning the patient’s wrist band as well as the sticker on blood product package.
Action plan 4: retrain and test of blood transfusion system users
To be aware of the knowledge and techniques in operating the new blood transfusion process, the blood transfusion committee retrained staff and requested them to be re-qualified. At the end, a total of 490 staff was participated in the new education course and the re-qualification exams showed the understanding of new process were 92.8% for doctors, 95% for nurses, and 97% for blood bank staff.
Action plan 5: revise the standard operation procedures (SOP) of blood transfusion
The blood transfusion committee revised the SOP of blood transfusion process and adopted the latest changes of the whole transfusion processes including the PDA Sentry Robot, the online blood product ordering system, and the use of patient/blood information stickers for the blood product package.
4.
DISSCUSSION
Although HFMEA shows the effectiveness in identifying and preventing the possible adverse events, it still required certain conditions to succeed. Strong support from the top management of the hospital is the most critical term. In addition, the identical faith and language of all related members also direct affect the achievement of the HFMEA project. Last but not least, the skills of implementing HFMEA can be a prerequisite to complete the project.
HFMEA is a valuable method for proactive risk analysis of the blood transfusion process. It helped the research hospital in identifying potential failures in the blood transfusion and in understanding the importance of evaluating the process from a systematic point of view. A systematic view permits a more comprehensive evaluation of the weaknesses and failure modes of the system before any adverse outcomes occur. Despite the extensive investment of money, time, and manpower, the method ensures a safer medical environment for patients and staff. Many researches have illustrated the efficiency of HFMEA and its favorable effect on a variety of medical processes ((Esmail et al.,
2005); (Linkin et al., 2005); (Van Tilburg et al., 2006); (Habraken et al., 2009)).
There may have many opportunities for errors to show at a number of critical points in the blood transfusion chain, starting with the doctor’s order, blood preparation, blood cross-matching, blood ordering, blood delivery, and final blood transfusion. To reduce those opportunities of adverse events in the blood transfusion chain, our team addresses several preventing actions, for example, the online blood product ordering and a PDA sentry robot to identify the patients. Those actions are responded to different researches which discussed the possible error occurring in the blood transfusion process. Stainsby ea al. (2005) indicated that weal links are the critical problem in the blood transfusion chain. Saxena et al. (2004) demonstrated the poorly defined monitoring systems would be the cause of the adverse events. The improvements made over past 1.5 years appear to have been quite effective in preventing transfusion errors and reducing the number of near-misses. The result of this study illustrated the effective of the HFMEA and the contribution of improving the patient safety.
5.
CONCLUSION
HFMEA proves to be an effective methodology to analyze and re-engineer healthcare processes, especially for complex processes that are potentially risky to patient. By using HFMEA in this study we identified several critical failure modes that are likely to threat patient’s safety. We have successfully introduced information technology to improve the whole blood transfusion process.
The HFMEA analysis of this study proves that information technology can effectively reduce the human errors. The linkage of the online blood product ordering system with HIS provides immediate access to blood-related patient information to secure the correctness of patient identification. Moreover, the PDA system also can prevent incorrect patient identification at the last step of blood transfusion at bedside.
6.
ACKNOWLEDGEMENT
This project was presented in the 2009 International Society for Quality in Health Care meeting, Dublin, Ireland.
7.
REFERENCES
1. Bonan, B., Martelli, N., Berhoune, M., Marie-Laure, M., Havard, L. and Prognon, P. (2009). The Application of
Hazard Analysis and Critical Control Points and Risk Management in the Preparation of Anti-cancer Drugs. International Journal for Quality in Health Care, 21(1): 44-50.
2. Bonnabry, P., Cingria, L., Ackermann, M., Sadeghipour, F., Bigler, L. and Mach, N. (2006). Use of a Prospective
Risk Analysis Method to Improve the Safety of the Cancer Chemotherapy Process. International Journal for Quality in Health Care, 18(1): 9-16.
3. Burgmeier, J.R.N. (2002). Failure Mode and Effect Analysis: An Application in Reducing Risk in Blood
Transfusion. The Joint Commission Journal on Quality Improvement, 28(6): 331-339.
4. DeRosier, J., Stalhandske, E., Bagian, J.P. and Nudell, T. (2002). Using Health Care Failure Mode and Effect
Journal on Quality Improvement, 28(5): 248-267.
5. Esmail, R., Cummings, C., Dersch, D., Duchscherer, G., Glowa, J., Liggett, G., Hulme, T. and Patient Safety and
Adverse Events Team (2005). Using Healthcare Failure Mode and Effect Analysis Tool to Review the Process of Ordering and Administration Potassium Chloride and Potassium Phosphate. Healthcare Quarterly, 8(Sp): 73-80.
6. Gilcheist, M., Franklin, B.D. and Patel, J.P. (2008). An Outpatient Parenteral Antibiotic Therapy (OPAT) Map to
Identify Risks Associated with an OPAT Service. Journal of Antimicrobial Chemotherapy, 62(1): 177-183.
7. Habraken, M.M.P., Van der Schaaaf, T.W., Leistikow, I.P. and Reijnders-Thijssen, P.M.J (2009). Prospective
Risk Analysis of Health Care Processes: A Systematic Evaluation of the Use of HFMEA(TM) in Dutch Health Care. Ergonomics, 52(7): 809-819.
8. Klein, H.G. (2001). Will Blood Transfusion Ever be Safe Enough? Transfusion Medicine, 11(2): 122-124.
9. Linden, J.V., Wagner, K., Voytovich, A.E. and Sheehan, J. (2002). Transfusion Errors in New York State: An
Analysis of 10 Years’ Experience. Transfusion, 40(10): 1207-1213.
10. Linkin, D.R., Sausman, C., Santos, L., Lyons, C., Fox, C., Aumiller, L., Esterhai, J., Pittman, B. and Lautenbach,
E. (2005). Applicability of Healthcare Failure Mode and Effects Analysis to Healthcare Epidemiology: Evaluation of the Sterilization and Use of Surgical Instruments. Clinical Infectious Diseases, 41(7): 1014-1019.
11. Rawn, J. (2008). The Silent Risks of Blood Transfusion. Current Opinion in Anesthesiology, 21(5): 664-668.
12. Saxena, S., Ramer, L. and Shulmun, I.A. (2004). A Comprehensive Assessment Program to Improve
Blood-administering Practices Using the FOCUS-PDCA Model. Transfusion, 44(9): 1350-1356.
13. Stansby, D., Russell, J., Cohen, H. and Lilleyman, J. (2005). Reducing Adverse Events in Blood Transfusion.
British Journal of Haematology, 131(1): 8-12.
14. Van Tilburg, C.M., Leistikow, I.P., Rademaker, C.M.A., Bierings, M.B. and Van Dijk, A.T.H. (2006). Health
Care Failure Mode and Effect Analysis: A Useful Proactive Risk Analysis in a Pediatric Oncology Ward. Quality and Safety in Health Care, 15(1): 58-63.