Detection, Diagnosis, and Treatment of Early Breast
Cancer Requires Creative Interdisciplinary Teamwork
László Tabár,* Tony Hsiu-Hsi Chen,
†Amy Min-Fang Yen,
†and Peter B. Dean
‡The development of modern breast imaging methods has resulted in a paradigm shift in our approach to diagnosing and treating breast cancer. Regular mammography screening can bring about a profound change in the spectrum of the disease since it shifts the balance of breast cancers from mainly palpable to mainly impalpable cases, most of which are still localized to the breast. Interdisciplinary breast centers provide the environment for devel-oping and sustaining the expertise and renewed commitment necessary to meet the challenge of detecting and defining preclinical breast cancer, and also tailoring the treat-ment accordingly. A consensus decision made by the specialists at a pretreattreat-ment planning conference is in the best interests of the breast cancer patient. Treatment will be more appropriate when early cancers are divided into groups with significantly different progno-sis. This is a significant challenge for the breast team.
Semin Breast Dis 8:4-9 © 2005 Elsevier Inc. All rights reserved. KEYWORDS breast diseases, mammography, patient care team
Paradigm Shift in Emphasis
from Late-Stage Therapy to
Early-Stage Diagnosis
and Therapy
For centuries, women have brought their palpable breast tu-mors to the attention of their physicians, by which time these tumors were mostly far advanced. Physicians caring for breast cancer patients have been treating tumors that measured 3 cm and larger, when the majority of these cancers were poorly dif-ferentiated and over 40% were disseminated. The frequently accompanying systemic disease often led to a poor outcome.
The development of modern breast imaging methods has resulted in a paradigm shift in our approach to diagnosing and treating breast cancer. Earlier diagnosis allows treatment to be initiated years earlier in the course of the disease—a situation that previous generations were seldom able to accomplish. Reg-ular mammography screening can bring about a profound change in the spectrum of the disease since it shifts the balance of breast cancers from mainly palpable to mainly impalpable
cases, most of which are still localized to the breast. Thanks to early detection, invasive cancers 1 to 14 mm in size will com-prise about 50% of the cases, when only about 20% of them are poorly differentiated and only 10% to 15% are node positive. We are experiencing a paradigm shift in controlling the disease, since preventing advanced cancer by arresting the disease pro-cess is becoming our main goal. Thus a modern, well-function-ing, interdisciplinary breast center will manage a large number of in situ carcinoma cases and invasive breast cancers that are predominantly⬍15 mm in size.
The success of the randomized controlled trials (RCTs) in demonstrating a significant decrease in mortality from breast cancer has given us convincing evidence that this disease is not systemic from its inception; instead, it is a progressive disease where detection and treatment in the early phase accomplishes a significant improvement in outcome. It is clear today that the treatment methods which fail in advanced stage disease have a proven life-saving capability when applied years earlier in the course of the disease. This leads to the inescapable conclusion that patient outcome will depend more on the time point in the course of the disease when therapy is initiated, and less on the particular therapeutic regimen chosen.1-3
A New Era in the Diagnosis and
Treatment of Breast Cancer
The significant improvement in the spectrum of tumor char-acteristics has brought a revolutionary new opportunity for
*Department of Mammography, Falun Central Hospital, Falun, Sweden. †Institute of Preventive Medicine, National Taiwan University, Taipei,
Tai-wan.
‡University of Turku Faculty of Medicine, Turku, Finland.
Address reprint requests to Dr. Laszlo Tabar, Falun Central Hospital, De-partment of Mammography, Falun 79182, Sweden. E-mail: laszlo@ mammographic.org
4 1092-4450/05/$-see front matter © 2005 Elsevier Inc. All rights reserved. doi:10.1053/j.sembd.2006.03.006
all health care professionals involved in the diagnosis and treatment of breast cancer patients. In a modern breast cen-ter, the representatives of all specialties are obliged to revise their diagnostic and therapeutic approaches to the disease. A new way of thinking and a renewed commitment are re-quired—not an easy task. Obviously, it is difficult to justify treatment guidelines for screen-detected breast cancers that are based on trials of palpable, clinically detected breast can-cers.
Our goal should be to maximize the benefits and minimize the risks by avoiding the extremes of undertreatment and overtreatment as well as the extremes of underdiagnosis and overdiagnosis. Interdisciplinary breast centers provide the environment for developing and sustaining the expertise and renewed commitment necessary to meet the challenge of de-tecting and defining preclinical breast cancer, and also tailor-ing the treatment accordtailor-ingly.
The use of modern imaging methods has provided us with a large series of early breast cancer cases which have now been followed for more than 20 years. Restricting our atten-tion to all DCIS cases and invasive tumors measuring⬍15 mm in size can provide valuable information regarding the suitability of various therapeutic regimens for achieving ex-cellent long-term survival while simultaneously avoiding overtreatment.4-7
Interdisciplinary
Breast Centers Need
Histopathologic Methods
Matching Modern
Imaging Methods
The introduction of large-scale, population-based mammog-raphy screening added a new dimension to the traditional interaction between pathologists and radiologists. The mam-mographic, ultrasound, and MRI examination of the breast provides an excellent overview of the whole breast, showing the relative proportions of all the different tissues within the breast. The conventional microscopic examination of breast specimens employs a resolution far superior to that of the mammogram, but the only tissue examined is that contained within the 4-m-thick tissue specimen obtained from a small paraffin block. Progress in histologic–mammographic corre-lation can be best made by examining a histology specimen at greater length, width, and depth.
The subgross, 3-D histology technique serves to bridge the gap that separates the pathologist from the radiologist, bring-ing them to a common ground for a better understandbring-ing of breast morphology. Combining the large section (10 ⫻ 8-cm) histology technique with the subgross, 3-D method makes a precise correlation with the imaging methods possi-ble. This comprehensive correlative approach helps the screening radiologist learn how to better select cases for fur-ther workup. These improvements in communication be-tween the members of the diagnostic team will serve to opti-mize the sensitivity and specificity of breast cancer diagnosis.
There are manifold advantages of microscopic examina-tion of a large, contiguous tissue sample on a glass measuring 8⫻ 10 cm, advantages which affect all of the subspecialties involved. These include, among others, the benefit of micro-scopic examination of an area measuring 60 to 80 cm2instead of no more than 5 cm2 using conventional histology. This results in a better evaluation of the extent of breast diseases, especially certain subtypes of breast cancer, such as invasive lobular cancer, multifocal tumors, and different types of DCIS. The margins can be assessed more accurately, again providing a significant impact on further treatment planning. Large section histology provides a better way to compare histology with mammography, breast ultrasound, and MRI images of the breast, furnishing continuous feedback to the radiologist and accelerating the learning curve, improving diagnosis and interdisciplinary communication. The end re-sult is better patient care through more appropriate treatment planning with fewer recurrences.8,9
A Consensus
Decision Made by
the Specialists at a
Pretreatment Planning
Conference Is in the
Best Interests of the
Breast Cancer Patient
Late stage breast cancer tends to follow a fairly uniform clin-ical course, regardless of the particular histologclin-ical type. This has contributed to the belief that breast cancer is a uniform disease entity, for which a uniform treatment plan has been followed for most of the 20th century. However, during the past two to three decades, among women who have regularly attended mammography screening, the majority of breast cancers have been diagnosed in the nonpalpable preclinical phase. Since the heterogeneous nature of breast cancer is more apparent in earlier stages, the approaches to diagnosis and therapy have necessarily become more complex. Effec-tive patient management in this new era has required the development of subspecialty areas within the fields of clinical pathology, radiology, surgery, and oncology. Thus, the re-sponsibility for diagnosis and treatment decisions has been distributed among several specialties. The specialists work-ing in interdisciplinary breast centers can effectively meet the challenges arising as a result of mammography screening.
Recent advances in breast imaging methods, in combina-tion with the use of sophisticated preoperative percutaneous biopsy methods, provide accurate information about the na-ture of the disease, and about most of the prognostic factors, such as tumor size, histologic type, and malignancy grade. This facilitates treatment planning in an unprecedented man-ner, compared with earlier decades. The regular pretreatment planning conference arriving at a consensus decision for the most appropriate therapeutic option for each patient is an important advancement and a powerful tool serving the best interests of the patient. These regular meetings also serve as a
dynamic forum for continuing medical education and re-search into further improvements in patient management.10
Treatment Will Be More
Appropriate When Early
Cancers Are Divided into
Groups with Significantly
Different Prognoses: A
Challenge for the Breast Team
Screening women at regular intervals results in the detection of a large number of in situ and 1- to 14-mm invasive breast cancers. In response, surgical treatment has gradually adopted less radical treatment options tailored to the specific tumor features and disease extent. Additionally, the develop-ment of the sentinel node technique was a great step forward in reducing treatment-related morbidity.
A similar, less extensive use of adjunctive therapeutic reg-imens could decrease the risk of overtreatment of screen de-tected, nonpalpable breast cancers. Beginning with DCIS, Silverstein has carefully documented that radiotherapy fol-lowing complete excision of the disease has not contributed to any improvement in disease-specific survival.11He
con-cludes that: “if there is no difference in breast cancer-specific survival regardless of the treatment and in some subgroups the absolute benefit from radiation therapy is extremely small, it seems reasonable to attempt to develop a system to select patients with DCIS who could be safely treated in the least aggressive way.”
Furthermore, there are accumulating data questioning whether the routine use of radiation following lumpectomy for early stage invasive breast cancer is necessary, or could
possibly even be avoided in selected subgroups of patients. Recently, several different approaches to this problem have been published.
1. Hughes and coworkers, in their C9343 trial, chose women 70 years of age and older with invasive tumors smaller than 20 mm and with ER⫹ or unknown recep-tor status. All women had lumpectomy and were ran-domized to tamoxifen plus radiation therapy or to a tamoxifen-only group. Local recurrence occurred in 4% of the nonirradiated group, whereas there was 1% recurrence in the irradiated group. They concluded that: “lumpectomy plus adjuvant therapy with tamox-ifen alone is a realistic choice for the treatment of women 70 years of age or older who have early, estro-gen receptor-positive breast cancer.”12Indeed, there is
an ever increasing number of early breast cancer cases detected at mammography screening, where postoper-ative radiotherapy offers no demonstrable survival ben-efit, and there is minimal benefit in terms of decreased local recurrence. In these cases, the treatment-related adverse effects, however minor in nature, will be am-plified and the cost/effect ratio will be grossly unbal-anced.
2. Whereas one of the main selection criteria in the Hughes and coworkers trial was patient age, the Leo-nard and coworkers publication13focuses on the
histo-logic tumor type. They have reported the long-term follow-up results of 44 patients withⱕ3 cm pure tu-bular cancers who have undergone complete excision without postoperative irradiation. They concluded that: “breast irradiation could be omitted after conser-vative surgery in older patients with smaller (ⱕ3 cm) tubular, well-differentiated breast cancers.”
3. In addition to patient age and histologic tumor type, we propose the use of mammographic tumor features to improve the efficacy of selecting women with early in-vasive breast cancer for less radical treatment.14
Al-though there are numerous histologic subtypes of inva-sive breast cancer, the mammogram reduces the distinctions to five basic mammographic appearances. The mammographic tumor features of 1- to 14-mm invasive breast cancers can be divided into five basic categories (Fig. 1). In three of them, the type of calcifi-cation determines the category, regardless of the pres-ence or abspres-ence of any associated tumor mass. The calcifications include the casting type (BIRADS “linear, branching”), the crushed stone-like (BIRADS “pleo-morphic”), and the powdery calcifications (BIRADS “amorphous”). The fourth category includes the circu-lar/oval tumor masses without associated calcifications. The fifth and most common group includes the stellate/ spiculated cancers with no associated calcifications. Our database originates from Dalarna County, Sweden, where a population-based mammography screening trial began in 1977. Since October 1977, all breast can-cer cases have been prospectively and consecutively documented with ongoing follow up. A total of 782 cases of invasive breast cancer ranging from 1 to 14 mm in size have been diagnosed between 1977 and 1998 and followed for up to 24 years. This gave us the op-portunity to search for subgroups that had excellent survival while having received less radical treatment. To determine the patient subgroups that could avoid
postoperative irradiation without compromising their long-term outcome, a prospective, randomized therapy trial was performed.15 No difference whatsoever was
seen in disease-specific survival between the irradiation and nonirradiation groups, although there was a signif-icant difference in local recurrence rate. This provides additional evidence that local recurrence in early breast cancer cases does not govern disease-specific survival, although it may serve as a marker.
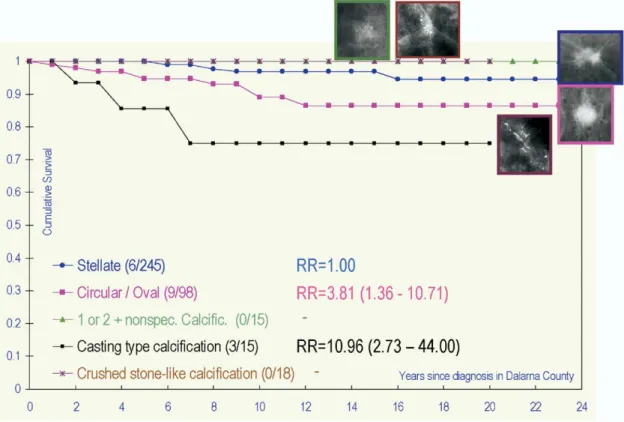
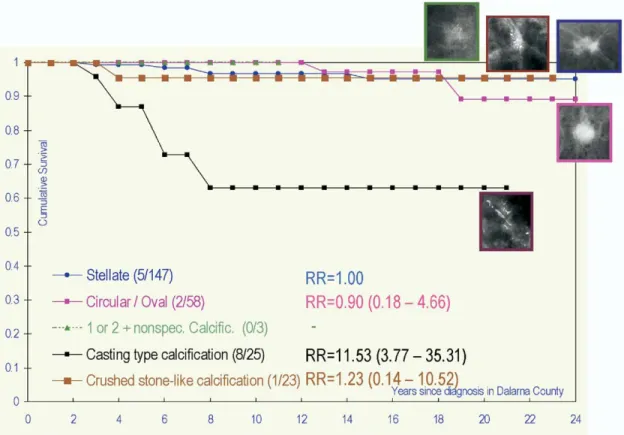
When reviewing the 782-patient material, including cases from the randomized therapy trial, and using the mammo-graphic tumor features to plot the 24-year disease-specific survival curves in the irradiated and nonirradiated groups, a striking similarity emerges (Figs. 2and 3). In both groups, the 1- to 14-mm invasive tumors associated with casting type calcifications have a surprisingly poor outcome regardless of the use of radiotherapy; whereas two other groups (the stel-late tumors without associated calcifications and the pow-dery calcifications) comprising two-thirds of the cases had an excellent 24-year outcome, again regardless of the use of radiotherapy.
Fig. 4shows the long-term outcome by mammographic tumor features for those cases having no information con-cerning postoperative radiotherapy. This figure bears a close resemblance toFigs. 2and3. One can conclude from these results that, once a small subgroup with the poorest progno-sis (ie, cases presenting with casting type calcifications) has been separated, the remaining cases will have excellent
24-Figure 2 Group with postoperative radiotherapy. Cumulative survival of women with 1- to 14-mm invasive breast cancer according to mammographic tumor features. (Color version of figure is available online.)
Figure 3 Group with no postoperative radiotherapy. Cumulative survival of women with 1- to 14-mm invasive breast cancer according to mammographic tumor features. (Color version of figure is available online.)
Figure 4 Group with no information about postoperative radiotherapy. Cumulative survival of women with 1- to 14-mm invasive breast cancer according to mammographic tumor features. (Color version of figure is available online.)
year disease-specific survival, even if postoperative irradia-tion is not given.
One of the many tasks facing the specialists participating in interdisciplinary breast centers is to discuss, test, and implement new diagnostic and treatment strategies for continuous im-provement of breast cancer care. Recent advances in clinical research may lead to changes in the standard of care, thus breast centers should find them worth discussing. A pertinent subject for discussion includes the various attempts to forgo postoper-ative radiotherapy or other adjunctive therapeutic regimens in selected groups of patients with early breast cancer.
Interdisciplinary breast centers have arisen in response to the need to manage organized screening, make the correct preoperative diagnosis of the abnormalities detected at screening, and provide the most appropriate, individualized treatment for each breast cancer case. As breast cancers are detected in ever-increasing numbers at ever-smaller sizes, new challenges are faced by every member of the breast team. These challenges can only be met by thorough, prospective data collection and its critical evaluation by all the team members. The introduction of large-scale, regular screening has made it possible to study and follow up large numbers of consecutively collected, small breast cancers. This previously unavailable database allows us to further improve the guide-lines for the diagnosis and treatment of breast cancer.
References
1. Smith RA, Duffy SW, Gabe R, et al: The randomized trials of breast cancer screening: what have we learned? Radiol Clin North Am 42:793-806, 2004
2. Duffy SW, Smith RA, Gabe R, et al: Screening for breast cancer. Surg Oncol Clin North Am 14:671-697, 2005
3. Tabar L, Dean PB: Mammography and breast cancer: the new era. Int J Gynaecol Obstet 82:319-326, 2003
4. Tabar L, Dean PB: Breast cancer: a progressive, heterogeneous disease requiring multidisciplinary diagnosis and treatment. J Oncol Manag 3:12-13, 1994
5. Lee ZC, Coleman C, Link J: Developing comprehensive breast centers. Part II. Critical success factors J Oncol Manag 1:6-12, 1992
6. Lee CZ: Comprehensive breast centers: priorities and pitfalls. Breast J 5:319-324, 1999
7. Tabar L, Dean PB, Kaufman CS, et al: A new era in the diagnosis of breast cancer. Surg Oncol Clin North Am 9:233-277, 2000
8. Tot T, Tabar L, Dean PB: The pressing need for better histologic-mam-mographic correlation of the many variations in normal breast anat-omy. Virchows Arch 437:338-344, 2000
9. Tot T, Tabar L, Dean PB: Practical Breast Pathology. Stuttgart, Georg Thieme Verlag, 2002
10. Lee CZ: Oncopolitical issues: obstacles and options for success in a comprehensive breast center. Surg Oncol Clin North Am 9:279-294, 2000
11. Silverstein MJ: An argument against routine use of radiotherapy for ductal carcinoma in situ. Oncology 17:1511-1533, 2003
12. Hughes KS, Schnaper LA, Berry D, et al: Lumpectomy plus tamoxifen with or without irradiation in women 70 years of age or older with early breast cancer. N Engl J Med 351:971-977, 2004
13. Leonard CE, Howell K, Shapiro H, et al: Excision only for tubular carcinoma of the breast. Breast J 11:129-133, 2005
14. Tabar L, Dean PB:Preventing premature death from breast cancer. Eur Oncol Rev, 2005. Available at: http://www.touchbriefings.com/cdps/ cditem.cfm?nid⫽1432&cid⫽5#Contents.Accessed January 10, 2006. 15. Liljegren G: Is postoperative radiotherapy after breast conserving sur-gery always mandatory? A review of randomised controlled trials. Scand J Surg 91:251-254, 2002