A Review for Information Systems to Support Outpatient Asthma Health
Management
I-Jou
Chen
, Hung-Wen
Chiu
Graduate Institute of Biomedical Informatics, Taipei Medical University, Taipei, Taiwan
*hwchiu@tmu.edu.tw
Abstract
Mobile or web technologies for supporting asthma self-management may improve patient–doctor communication and patient self-efficacy. People of all ages in countries throughout the world are affected by asthma, and this disease is a significant burden not only in terms of the health care system but also because it results in loss of productivity and reduced participation in family life. Recent evidence suggests that interactive Internet-based asthma monitoring improves asthma control. This paper will explore the application of various mobile and web-based asthma management systems, with a goal of developing an integrated information management platform for asthma patients. Keywords: asthma, chronic disease management, telecare, mobile technology
1. Introduction
Asthma is one of the most common chronic diseases. The World Health Organization (WHO) estimates that about 300 million people have asthma worldwide, and the asthma population is expected to increase to 1 billion people by 2025[1]. According to the Taiwan Department of Health, about 503,000 people were plagued by asthma in that country in 2005[2]. The compound annual growth rate (CAGR) of asthma mortality was 2.28% in Asia-Pacific countries from 1999 to 2006. Thus, the mortality rates for asthma have been increasing steadily over the past decades[3-5].
Asthma is a significant burden not only in terms of the health care system but it also results in a loss of productivity and reduced participation in family life.
To reduce the prevalence of asthma, it is necessary to actively promote health education and knowledge of correct drug use. Both the National Institutes of Health (NIH) [6] and the Global Initiative for Asthma (GINA) [1] have recommended guidelines for asthma diagnosis and patient management. These guidelines suggest that asthma is better controlled by identifying and reducing exposure to risk factors, developing good patient–doctor partnerships, and following medication instructions. The most important activities to reduce the occurrence of asthma are (1) adherence to a self-management plan; (2) patient compliance with written doctor’s instructions and daily recording of symptoms; and (3) maintaining a written history of drug use, allergies, lung function, and frequency of visits to the hospital.
Traditionally, asthma patients record their peak flow meter readings and symptom scores in paper diaries, and therefore physicians cannot review patient information in real time and cannot give real-time recommendations. However, in recent years, telemedicine applications have been developed to help asthma patients self-manage their disease and record their conditions and changes in external factors (e.g., the environment) and internal factors (e.g., allergies). These information systems have advantages and disadvantages, and the aim of this paper is to explore the application of these various systems with a goal of developing an integrated information management platform for asthma patients.
2. Background
2.1. The Global Initiative for Asthma
The Global Initiative for Asthma (GINA) project was initiated in 1993, in collaboration with the National Heart, Lung and Blood Institute (NHLBI), the National Institutes of Health USA (NIH), and the World Health Organization (WHO). Its goal is to produce recommendations for asthma management based on the best scientific information available. GINA holds a World Asthma Day on the first Tuesday in May of each year to promote worldwide asthma awareness.
Taiwan began issuing guidelines for asthma treatment in 1995, and the latest version of these guidelines is the 2006 edition[7].
2.2 Definition of Asthma
The NHLBI defines asthma as a chronic inflammatory disorder of the airways, which can either naturally resolve or be treated to restore it to normalcy. According to GINA 2008 guidelines, this inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness, and cough, particularly at night and early morning. GINA also states that common risk factors for asthma symptoms include exposure to allergens, exercise, and strong emotional expressions [8-13].
2.3 Diagnosing Asthma
Asthma cannot be diagnosed with a single examination. A physician will need to take into consideration the patient’s medical history, physical examination findings, and lung function data to assess whether the patient has asthma.
2.4 Monitoring Asthma
Peak expiratory flow (PEF) measurements can be an important aid in both diagnosing and monitoring asthma. Measurements of lung function provide an assessment of the severity, reversibility, and variability of airflow limitation, and help confirm the diagnosis of asthma. The GINA asthma treatment guidelines cite the degree of variation in daily PEF values from morning to evening as a means of monitoring and assessing a patient’s status and response to therapy.
The Taiwan Association of Asthma Education recommends the Asthma Control Test (ACT) to assess asthma symptoms. This patient-based, monthly five-item health survey is designed to identify a patient’s degree of disease control. This test benefits patients who occasionally forget to use their peak flow meter, or in cases where the peak flow meter cannot monitor night coughs; however, the ACT is intended to supplement, not replace, the peak flow meter. The NHLBI began promoting ACT assessment in 2003 and GINA recognized ACT assessment of asthma control in 2006. The United States, Canada, Australia, and other countries currently use the ACT [7].
2.5 The Goal of Asthma Control
Asthma is a chronic disease; however, as long as patients receive health education, execute their self-management plan, and follow their doctor’s instructions, they can achieve long-term monitoring. The asthma treatment guidelines issued in Taiwan in 2006 have the following objectives: on a daily basis, to have no (or only slight) chronic symptoms—rarely an acute attack; unrestricted activities (including sports); PEF values are close to normal; and there are no drug side effects.
3. Studies Reviewed
Review of the past 10 years of research pertaining to asthma-related telemedicine indicates that its application has gradually increased. With the popularization of Internet applications, people can, through mobile devices or computer transmission, send physiological signals remotely and can also access real-time medical information.
3.1. Web-based Asthma Management Applications
Michael Vedran [14] established a web-based asthma management tool with which patients can, via the Internet, upload their PEF values and allergy history, and the health care provider can, through the platform, review the patient’s level of asthma control. This tool can calculate PEF rate and variability and present them in trend graphs that offer patients a comprehensive view,
enabling them to monitor the progress of their asthma. This system has improved the overall quality and safety levels of health care services provided to patients, owing to the greater efficiency in delivering treatments and reduced delays, omissions, and mistakes. The system has been tested through a preliminary survey in the United Kingdom and Greece.
3.2. Mobile Device Asthma Management Applications
In Korea, Lee [15] developed web-based and mobile device applications for the management of asthma. Based on ASP.NET and a Mobile Toolkit, this system enables an asthma patient to use a pocket PC, a mobile phone, or a desktop computer for reliable, wireless exchange of all relevant information between a doctor and a patient. Studies have shown that mobile devices can increase system utilization by 10–30%, and patients can easily obtain customized instructions according to their daily personal symptoms, PEF values, medications, and activity restrictions.
Similarly, a researcher developed an asthma management software with which a patient uses an electronic peak flow meter linked to a mobile phone with an interactive screen (touch screen) to record current asthma symptoms, which are transmitted to and stored in a server. This asthma tool is easy to use and saves time, and the digital peak flow meter can reduce input errors. Patients are able to view their own PEF values, and mobile devices will draw PEF charts and also provide the day temperature, wind speed, and pollen count to enable patients to improve their awareness of risks of an asthma attack [16].
Hung [17], in cooperation with Taiwan’s mobile company, provides a fee-based mobile asthma management service through which patient PEF values and asthma symptoms can be input to a mobile phone and then transmitted to health care providers. They also built and maintain an asthma web site where users can review their own PEF value charts and observe daily changes in environmental factors in Taiwan. Medical personnel can send treatment recommendations or alerts through messages or e-mails. The tool can provide real-time monitoring and can also reduce waste of medical resources.
3.3 Study of Environmental Impacts on Asthma Chu [18] used the Neural Network Toolbox of the MATLAB software to predict daily exposure to severe environmental factors in the central region of Taiwan. The server of the detecting system collects real-time data from the national network of air quality monitoring stations. In response to a remote query, the server makes the decision whether to send warning messages according to a proposed asthma neural network model; this “asthma inducement decision support system” can provide asthma patients with geographic information about regions that have air pollution. Moreover, the
system provides early warning for patients to avoid possible asthma triggers of air pollution and weather changes.
In 2009, the Taiwan Association of Asthma Education published a report on the impact of temperature, relative humidity, and suspended particulates on asthma. Through its web site, users have access to a daily asthma indicator—a tool that can increase people’s awareness of asthma management options and knowledge of health issues [19].
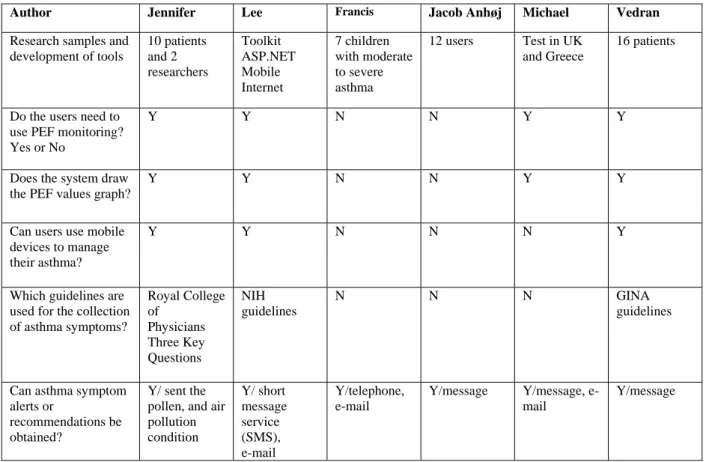
For a comparison of web-based applications for asthma management, see Table 1[14-30].
4. Discussion and Future Work
Although research shows that asthma is one of the world’s most common chronic diseases, studies of web-based and mobile phone asthma management applications have been conducted only recently and availability of such systems is still not commonly known. Although an asthma attack is acute and serious, the symptoms of a mild cough can be easily ignored. In addition, asthma inducement includes many factors, and the lack of integration among information platforms forces users to search in many places for the information they need.
Through additional research on PEF values and changes in environmental factors, we can develop individual web-based and mobile asthma management services that include personal allergy records that would enable us, for example, to provide dietary recommendations for asthma patients (diet can improve lung function). In addition, we can provide environmental factor reminders and other alerts such as for pollen (when the flowering season approaches, patients can avoid going to high-pollen regions). Apple Inc. has produced an iPhone 3G that already has an asthma monitoring software loaded. We propose to increase the collection of asthma symptoms so that patients can access the ACT through the touch screen to reduce traditional input errors.
As we have shown, development efforts are ongoing in many directions. We expect to construct an integrated management system for asthma patients, and the architecture of our proposed system is shown in Figure 1. The functions of our proposed system are shown in Figure 2. Users would need to use peak flow meters to obtain PEF values at home and then, through an Internet-access “smart phone,” upload the information to a server. In addition to PEF values, patients will be able to upload allergy history and ACT test results, and physicians can send recommendations back to the users. The server will automatically calculate the patient’s PEF rate and variability, and then draw PEF trend charts to illustrate the user’s lung function. Also, the server will automatically download daily allergen asthma indicators from the Taiwan Association of Asthma Education web site so that users can easily review daily outdoor asthma inducement factors.
Other future research topics include an asthma monitor designed as a GPS-enabled asthma inhaler. Such an inhaler would enable researchers to track asthma inhaler use time and geographic location, which after a long period of observation could be correlated to find asthma inducement factors. Also, in Taiwan, research is ongoing to develop a tool that predicts asthma attacks through the sound of a patient’s wheezing. There are many asthma topics for us to explore.
Figure 1. The architecture of our proposed system.
Users would need to use peak flow meters and input their data to a smart phone. The server will calculate the PEF rate and variability then automatically draw the PEF chart. Also, the server can automatically download daily allergen asthma indicators for users
Figure 2. The purpose of our proposed system.
Patients would need to register their individual data, including sex, age, and weight, and input information that includes PEF values twice a day, allergy history, and ACT results. Patients would be able to obtain daily outdoor asthma inducement factor indicator information.
Table 1. Comparison of Web-based Asthma Management Tools
Author Jennifer Lee Francis Jacob Anhøj Michael Vedran
Research samples and development of tools 10 patients and 2 researchers Toolkit ASP.NET Mobile Internet 7 children with moderate to severe asthma 12 users Test in UK and Greece 16 patients
Do the users need to use PEF monitoring? Yes or No
Y Y N N Y Y
Does the system draw the PEF values graph?
Y Y N N Y Y
Can users use mobile devices to manage their asthma?
Y Y N N N Y
Which guidelines are used for the collection of asthma symptoms? Royal College of Physicians Three Key Questions NIH guidelines N N N GINA guidelines
Can asthma symptom alerts or
recommendations be obtained?
Y/ sent the pollen, and air pollution condition Y/ short message service (SMS), e-mail Y/telephone, e-mail Y/message Y/message, e-mail Y/message
5. Reference
[1] Global Initiative for Asthma, Pocket Guide for Asthma Management and Prevention, updated to 2008.
[2] Taiwan Department of Health, available from: http://www.doh.gov.tw/cht2006/index_populace.aspx. [3] Frost and Sullivan, available from:
http://www.frost.com/prod/servlet/frost-home.pag.
[4] Cheng YP, Eco-City Conference, Taipei, Taiwan. Jan.19-20 2009.Available from:
http://www.ecocity.org.tw/progress/index.aspx.
[5] Matthew M. Global Burden of Asthma, Global Initiative for Asthma, updated to 2008.
[6] National Heart Lung and Blood Institute. Expert Panel Report 2: Guidelines for the Diagnosis and Management of Asthma. Bethesda: NIH Press, 1997.
[7] Taiwan Asthma Council, Global Strategy for Asthma Management and Prevention, 2006.
[8] Chou CH. Evaluation of Asthma Disease Management on Patient continuous care under National Health Insurance based on a medical teaching hospital in southern Taiwan.
Unpublished doctoral dissertation, Kaohsiung Medical University, 2004.
[9] Appleby J. My child has asthma: some answers to parents question, Profession Care of Mother & Child, 1996; 6 (1):13-15.
[10] Eusenbeis C. Full parter in care, Nursing, 1996; (1): 48-51. [11] Tu ML. Evaluation of Asthma Disease Management Program in a Medical Center. Unpublished doctoral dissertation, Kaohsiung Medical University, 2005.
[12] American college of allergy asthma and immunology, overview of Asthma Disease Management, in Asthma Disease Management Resource Manual, 1998.
[13] Baldaia L. An educational approach to successful management of childhood asthma as a chronic illness. Journal Pediatric Nursing, 1996; 11(5):335-336.
[14] Michael G, Panagiotis C. Technological innovations in asthma patient monitoring and care. Expert Systems with Applications, 2004; 121-131.
[15] Lee HR, Yoo SK, Jung SM, Kwon NY, Hong CS. A Web-based mobile asthma management system. Journal of Telemedicine and Telecare. 2005; 11: S1: 56-59.
[16] Cleland J, Caldow J, Ryan D. A qualitative study of the attitudes of patients and staff to the use of mobile phone technology for recording and gathering asthma data. Journal of Telemedicine and Telecare. 2007 ;13: 85-89.
[17] Hung SH. Care Asthma via Mobile Phone (CAMP), NCHC Taiwan. Available from: http://www.medicalgrid.org [18] Chu HT, Huang CC. A ubiquitous warning system for asthma-inducement. Proceedings of IEEE International Conference on Information Technology Applications in Biomedicine. 2006.
[19] Taiwan Association of Asthma Education, 2009.Available from: http://www.asthma-edu.org.tw/asthma.
[20] Malone F, Callahan CW, Chan DS, Sheets S, Person DA. Caring for Children with Asthma through Teleconsultation: “ECHO-Pac, The Electronic Children’s Hospital of the Pacific”. Telemedicine Journal and e-HEALTH. 2004; 10(2):138-46. [21] Anhøj J, Møldrup C. Feasiblity of Collecting Diary Data From Asthma Patients Through Mobile Phones and SMS:Response Rate Analysis and Focus Group Evaluation From a Pilot Study. Journal of Medical Internet Research. 2004; 6(4):e42.
[22] Verschelden P, Cartier A, Trudeau C, Malo J. Compliance with and accuracy of daily self-assessment of peak expiratory flows (PEF) in asthmatic subjects over a three month period. European Respiratory Journal. 1996; 9: 880–5.
[23] Kamps AW, Roorda RJ, Brand PL. Peak flow diaries in childhood asthma are unreliable. Thorax 2001; 56:180–2. [24] Hartert TV, Windom HH, Peebles S, Friedhoff T. Inadequate outpatient medical treatment of asthma for patients admitted to two urban hospitals. The American Journal of medicine. 1996; 100: 386–399.
[25] Shenoy N, Nazeran H. PDA based personal asthma management system. IFMBE Proceedings. 2005; 5(1):5186-5189.
[26] Finkelstein J, Cabrera M.R, Hripcsak, G. Web-based monitoring of asthma severity: a new approach to ambulatory management. Proceedings of IEEE International Conference on Information Technology Applications in Biomedicine. 1998, 139-143.
[27] Finkelstein J, Friedman R.H. Telemedicine system to support asthma self-management. Proceedings of IEEE EMBS International Conference on Information Technology
Applications in Biomedicine. 2000, 164-167.
[28] Finkelstein J, Friedman R.H. Home asthma telemonitoring (HAT) system. Proceedings of the IEEE 26th Annual Northeast Bioengineering Conference. 2000, 103-104.
[29] Morlion B, Verbandt Y, Paiva M, Estenne M, et al. A telemanagement system for home follow-up of respiratory patients. IEEE Eng Med Biol Mag. 1999;18(4):71-9.
[30] Ostojic V, Cvoriscec B, Ostojic SB, Reznikoff D, et al. Improving Asthma Control Through Telemedicine: A Study of Short-Message Service. Telemedicine Journal and e-HEALTH. 2005 Feb; 11(1):28-35.