The Requirement of Health Record to satisfy the patients’ safety management
Kiyomu Ishikawa
1), Hisashi Ohmichi
2), Yoshimasa Umesato
2), Hitoshi Terasaki
2), Hidehiko Tsukuma
1),
Norikazu Iwata
1), Takeshi Tanaka
1), Akie Kawamura
3), Kayo Sakata
3), Teruko Sainohara
3), Miyuki
Sugimura
3), Nakao Konishi
4), Masashi Tooya
5)1) Medical Informatics and Hospital Systems Management, Hiroshima University Hospital, Hiroshima, Japan
2) Hospital Administration Science, Nihon University, Tokyo, Japan
3) Maternity and Perinatal Center, Hiroshima University Hospital, Hiroshima, Japan 4) Department of Nurse, Hiroshima University Hospital, Hiroshima, Japan
5) Department of Safety Management, Japan Council for Quality Health Care, Tokyo, Japan E-mail: humind3@hiroshima-u.ac.jp
Abstract
Purpose: As a basic medium of team medical care
process under multi-specialties’ cooperation, EHR is required to secure patient safety and meet the information disclosure demand. Based on the reassessment of the structure and description requirement of EHR, its next generation construction policy is proposed.
Methods: Surveys as the basis for its work were carried
out by the authors organized and headed task forces in the hospitals certified by Japan Council for Quality Health Care (JCQHC). One of surveys was the assessment of the current state Health Record computerization. In addition, The Guidelines for healthcare record (HR) Structure and its computerization policy based on two questionnaire surveys were executed. Practically, they were used as criteria in evaluating handwritten health record and traditional EHR description.
Results: The survey of the above hospitals showed that
most have computer supported administrative procedures, but only few computer-based health records. Besides, in terms of healthcare record which could be disclosed to patients, the attitudes of the Hiroshima EHR users showed that while they expected efficiency and quality improvements, there were considerable gaps among their evaluations based on the new guidelines. Especially, the lack of description items, system imperfection, and description contents varied conspicuously.
Conclusion: Systematically, EHR is available for
integrated description. However, this result was caused by the subsystem construction for different users without sufficient understanding of medical care process. These insights led to the initiation of curricula educating “Health Information Technologist” which is promoted by Japan Association Medical Informatics and the criterion of Chart Review Promotion of JCQHC. They will also contribute to improved and advanced EHR.
1. Introduction
In order for the standardized HR to become the basic medium for the interaction of specialists and patients in the practice process, we have to comprehend the HR from the perspective of safety and quality of healthcare and reevaluate its computerization to arrive at a better blueprint for the next generation health system.
Since the Ministry of Health and Labor issued the basic design of the EHR in 2001, the computerization of the health record has met with increasing public interest. Additionally, the “IT policy objectives package 2005” released by Japanese government [1] will accelerate EHR development. As a next step, we plan to develop a Healthcare Navigation system over the next 5 years. The HR should serve as the basis for process and outcome evaluation. However, currently HR quality varies so widely that it is unlikely to serve as the basis for developing patients’ confidence in the healthcare process.
Though the EHR is expected to decrease the variation in record quality, there is still no consensus on its social role. The idea that it is just the computerized version of the paper record still prevails. In our view, it will be necessary to develop it beyond that into the key medium for interaction of specialists in medical care. Despite our effort to reflect the care process in the system operation, the current system in the opinion of medical staff is so complicated and unusable that it might impinge on operational efficiency and threaten patient safety.
2. Research organization and activity
The Chart Review Committee (CHC) headed by the first author consists of 35 appointed members: healthcare system investigators (5), chart review specialists (15), and clinical specialists (7 medical doctors and 8 nurses)
of member hospitals of the Patient Safety Promotion Organization of Hospitals certified by the Japan Council for Quality Health Care (JCQHC).
The JCQHC is the nationally authorized organization, which accredits hospitals based on neutral assessment with academic perspectives in order to improve the quality of healthcare. In March 2006, there were over 1997 accredited hospitals, and 1050 hospitals were also members of the Patient Safety Promotion (PSP) council, an independent organization. Since PSP established CHC in 2004, its projects have focused on the EHR structure as a strategic tool to improve medical care safety through the following initiatives:
1) A survey of the actual status of inspection and
evaluation of HR structure in the participating hospital, 2) Development of guidelines for HR structure with
emphasis on clinical safety management and on making these guidelines available to the hospitals, 3) In this context, the advantages and
disadvantages of HR computerization were analyzed in relation to their potential role in evaluating the quality of care process.
3. Survey of the health record inspection and
evaluation in PSP member hospitals
A questionnaire was mailed to 1370 PSP member hospitals by CHC in 2004, and 972 hospitals (70.9%) replied. The number of beds under operation ranges most evenly from across 100 beds or lower to over 500 beds or more .
3.1 Current standardization of EHR recording
There are 569 hospitals (58%) with individual guidelines and manuals for recording, and 341 hospitals (35%) do not have. In terms of summary forms for post-evaluation of medical care process, 654 hospitals (67%) use the unified forms in every department, but in 256 hospitals (26%) only main departments follow them.58% 6%
35%
1%
Yes Some Unit None NA
n = 972
Fig.1 Current standardization of EHR recording
3.2 Inspection condition of the HR
Sixty three percent of the hospitals serve as the center
of clinical education and training for interns.
Among thes e hospitals, 82% have the management sections of HR, and 86% of them have review or inspection committees for the HR.
3.3 Computerization circumstances
In 92% of hospitals, Patient Data were computerized, but health data documentation systems as “official document” is computerized in only 21% .
10% 11%
71%
8% 0%
Almost Computerized Partially Uncomuputerised Other NA
n= 972
Fig.2 Japan current situation of EHR recording
4. Recommended Health Record Structure
In order to make the HR the key medium for organized medical service involving a variety of specialists, the HR Structure Guideline as composed by CHC is based on the following seven principles.
4.1 Compliance with Personal Health
Information Act
Healthcare records must be structured in compliance with the Personal Healthcare Information Act and related laws so that inpatients can control their personal
information flow and at the same time rely on; a) Confidentiality
b) Disclosure of personal information to patients c) Correction of errors
d) Restricted use of personal information.
Careful documentation is required in order to protect the dignity of the inpatient and his/her family even after his death.
The primary use of information for the medical care of the patient has to be strictly distinguished from the secondary use, including social availability of
the purpose of secondary information use in advance in order to protect his/her dignity.
Appropriate information use should be guaranteed by appointing a managing specialist of healthcare
information in every facility.
4.2 Healthcare records as communication media
in team practice
In addition to records on medical treatment, operation, and anesthesia produced by doctors, organic coordination of documentation is also required for nursing records, rehabilitation records, records of pharmaceutical management and conduct, nutrition conduct, and medical consultation records.
In order to show the interrelation in team medical care, the form of document organization and filing should be documented.
The organization of the medical service is considered to be appropriately reflected by team-sequenced form of records, which integrates prioritized and ordering issues, setting targets, treatment plans, recording requested orders and their results, as well as conduct confirmation, and outcome evaluation.
Especially, the problem list and the care follow-up are expected to be integrated, precisely indicating the specialists’ reasoning.
4.3 Target-oriented description
The target of medical care, which ranges from short and mid to long term goals in physical, psychological, and social life environment, should be defined and documented.
The action plan for achieving the target must be specified.
The target and action plan need to be adapted to changes in the patient’s physical condition and circumstances.
4.4 The guarantee of generalization
Since various events and episodes occur in parallel during the care process, and the general condition of a patient and care process should be easy to grasp, it is necessary to arrange and specify medical care conducted and documented by other medical staff, so that
specialists with diverse viewpoints can cooperate in achieving the same treatment goal.
The lists of problems, targets, and the plan of action are to be placed at the beginning of the file, and an interim summary is to be included in the process records. It is crucial that each episode consists of the compact and clear description on facts, events, subjective/objective problems, assessments, plans, interventions, outcome evaluation, and a plan to the next stage.
In reappearance of problems, the previous listed
number is reused. While, in the case of unlisted episode the new number is added for achieving continuity. In order to promote information availability of the patient and his/her family, the use of jargon or
abbreviations is discouraged in favor of understandable terminology.
4.5 The guarantee of continuity
For newly emerging conditions, whether related to medical or nursing treatment, including interview, observation, measurement, evaluation, diagnosis, planning, procedure, treatment, and evaluation of outcome, recording of the date of occurrence is required. Recording of time is desirable when complex medical treatment is conducted during a single day. The start of an episode of the disease process, the time relation of change, the service sequence among several attending specialists should all be systematically described for easy understanding.
When reference is made to past episodes of medical or nursing care, the date and time of episode and those of the recording should both be documented.
4.6 The guarantee of authenticity
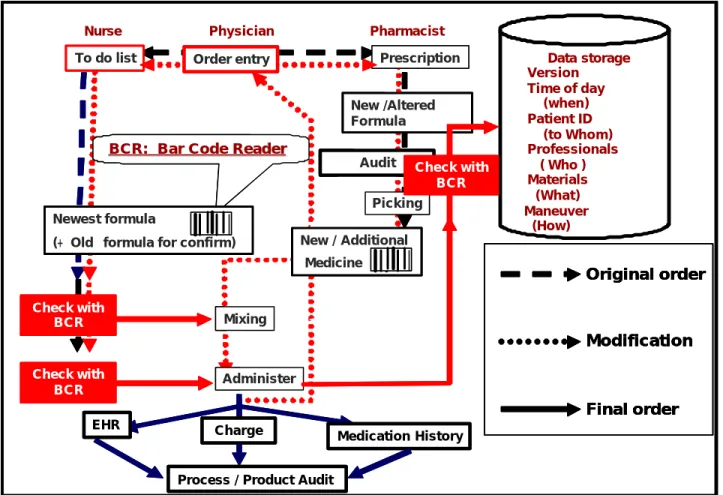
In order to make certain and correct communication among specialties, logging of the following items is indispensable with practical date and time. (Fig. 3)
a) Orderer
b) Subject and object c) Receiver
d) Check the order correctness to avoid mismatching with previous information
e) Doer
f) Confirmation of action
Objective description of events is required. Accurate verbs should be used in expressions of speculation and inference. The newest data should be shown. Basically, an episode must be recorded as soon as it is recognized while the staffs concerned are on duty. (At latest within the same day)
In the EHR, a permanent preservation file is required in order to avoid replacing the original records.
“Documentation errors” of care should be positively corrected. The date and time of correction, those of the recording of the outdated information, the content before and after correction, and the name of corrector all have to be documented.
Basically in correcting handwritten healthcare records, after double lines are drawn to show the incorrect content, new content is added. Use of correction fluid and erasers is not allowed.
In documentation, simple writing errors, which do not affect recorded context, serial correction stamps, and signatures, are unnecessary.
4.7 The guarantee of original records
Information meant to serve as official records should be shown individually according to forms such as the first record form for public insurance healthcare, patient
charts, ordering forms, process list, operation and anesthesia reports, summary, and test results .
Medical facilities, which use both handwritten records and EHR, need to define the official form for each healthcare record.
EHR Charge
Medication History
To do list Prescription
Process / Product Audit
Physician Pharmacist Nurse Alter / Cancel Data storage Ø Version Ø Time of day (when) Ø Patient ID (to Whom) Ø Professionals ( Who ) Ø Materials (What) ØManeuver (How) Order entry New / Additional Medicine Mixing Administer
Original order
Modification
Final order
BCR: Bar Code Reader
BCR: Bar Code Reader
New /Altered Formula
Audit Picking Newest formula
(+ Old formula for confirm)
Check with BCR Check with BCR Check with BCR EHR Charge Medication History To do list Prescription
Process / Product Audit
Physician Pharmacist Nurse Alter / Cancel Data storage Ø Version Ø Time of day (when) Ø Patient ID (to Whom) Ø Professionals ( Who ) Ø Materials (What) ØManeuver (How) Order entry New / Additional Medicine Mixing Administer
Original order
Modification
Final order
Original order
Modification
Final order
BCR: Bar Code Reader
BCR: Bar Code Reader
New /Altered Formula
Audit Picking Newest formula
(+ Old formula for confirm)
Check with BCR Check with BCR Check with BCR
Fig. 3 Business flow for guarantee of responsibility of action and authenticity (Ex. the data accumulation and storage process model in injection)
5. Audit of handwritten HR and classical
EHR on safety management
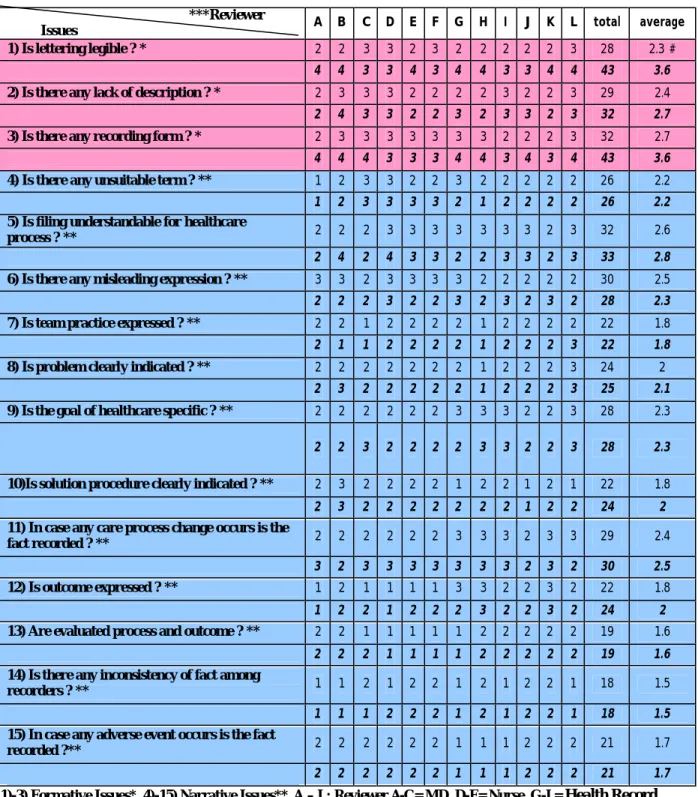
Based on the recording guideline mentioned above, the recording evaluation guideline was established to secure patient safety.
In order to obtain the objective outcome, it consists of 15 items from the view point of “Formative Issues ” and “Narrative Issues ”. The one focuses on the readable description without misleading expression, and the other team practice. In hospitals, diverse specialists are involved in evaluating operation. Tentatively, 12 reviewers (3 doctors, 3 nurses, and 6 health record inspectors) made the evaluation by means of 3
handwritten healthcare record files and 3 provided print out EHR files.
According to its outcome shown in Table 1, there was a gap among individual evaluation scores though
cases concerned were insufficient for making statistics. Specifically, in terms of “Formative Issues ”, EHR got higher score than handwritten HR. In contrast, in “Narrative Issues ”, they were almost equal, or handwritten HR was superior
6. An example of the EHR to the safety of
medical care
6.1. To guarantee the generalization and
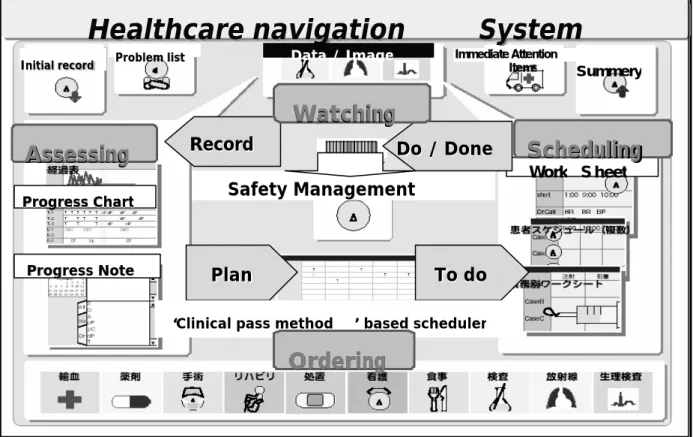
continuity of practice
The Health Record (HR) should serve as the basis for process and outcome evaluation. Here, as a practical case of safety management, Healthcare Navigation System is presented. (A model of the HNS, which is the core of the EHR in the Hiroshima University Hospital, may serve as a practical example of the implementation of HNS in the
service of safety management. [2]) The HNS has to facilitate safe team practice see. (Fig.4)
Data through patient healthcare (PHD) are accumulated not only by physicians, but also by all
co-workers. This may be the basis for team
communication and a reliable way of treating in such a way that the evidence of conducted practices is traced.
Table 1 Outcome of Recording Guideline-based Trial Evaluation to Secure Patient Safety
***Reviewer
Issues A B C D E F G H I J K L total average 1) Is lettering legible ? * 2 2 3 3 2 3 2 2 2 2 2 3 28 2.3 # 4 4 3 3 4 3 4 4 3 3 4 4 43 3.6
2) Is there any lack of description ? * 2 3 3 3 2 2 2 2 3 2 2 3 29 2.4
2 4 3 3 2 2 3 2 3 3 2 3 32 2.7
3) Is there any recording form ? * 2 3 3 3 3 3 3 3 2 2 2 3 32 2.7
4 4 4 3 3 3 4 4 3 4 3 4 43 3.6
4) Is there any unsuitable term ? ** 1 2 3 3 2 2 3 2 2 2 2 2 26 2.2
1 2 3 3 3 3 2 1 2 2 2 2 26 2.2
5) Is filing understandable for healthcare
process ? ** 2 2 2 3 3 3 3 3 3 3 2 3 32 2.6 2 4 2 4 3 3 2 2 3 3 2 3 33 2.8 6) Is there any misleading expression ? ** 3 3 2 3 3 3 3 2 2 2 2 2 30 2.5
2 2 2 3 2 2 3 2 3 2 3 2 28 2.3
7) Is team practice expressed ? ** 2 2 1 2 2 2 2 1 2 2 2 2 22 1.8
2 1 1 2 2 2 2 1 2 2 2 3 22 1.8
8) Is problem clearly indicated ? ** 2 2 2 2 2 2 2 1 2 2 2 3 24 2
2 3 2 2 2 2 2 1 2 2 2 3 25 2.1
9) Is the goal of healthcare specific ? ** 2 2 2 2 2 2 3 3 3 2 2 3 28 2.3 2 2 3 2 2 2 2 3 3 2 2 3 28 2.3
10)Is solution procedure clearly indicated ? ** 2 3 2 2 2 2 1 2 2 1 2 1 22 1.8
2 3 2 2 2 2 2 2 2 1 2 2 24 2
11) In case any care process change occurs is the
fact recorded ? ** 2 2 2 2 2 2 3 3 3 2 3 3 29 2.4 3 2 3 3 3 3 3 3 3 2 3 2 30 2.5
12) Is outcome expressed ? ** 1 2 1 1 1 1 3 3 2 2 3 2 22 1.8
1 2 2 1 2 2 2 3 2 2 3 2 24 2
13) Are evaluated process and outcome ? ** 2 2 1 1 1 1 1 2 2 2 2 2 19 1.6
2 2 2 1 1 1 1 2 2 2 2 2 19 1.6
14) Is there any inconsistency of fact among
recorders ? ** 1 1 2 1 2 2 1 2 1 2 2 1 18 1.5 1 1 1 2 2 2 1 2 1 2 2 1 18 1.5
15) In case any adverse event occurs is the fact
recorded ?** 2 2 2 2 2 2 1 1 1 2 2 2 21 1.7
2 2 2 2 2 2 1 1 1 2 2 2 21 1.7
1)-3) Formative Issues*, 4)-15) Narrative Issues**, A – L: Reviewer A-C= MD, D-F= Nurse, G-L= Health Record Inspectors***In each field Upper Row: handwriting HR, Lower Row: EHR, Score #: suitable < 4 , 3, 2, 1 > unsuitable
6.2. Contribution to safety healthcare
The system is designed to share the information among all attendants and the patient concerned topromote team practice, which is expected to enhance safety and high-quality medical care as well as rational hospital treatment. Modules of HNS are available not only to the physicians but also to all other health professionals concerned. [2]
A physician may give orders to other professionals
who show order confirmation signed on the same browser. The interactions of information management in the clinical process are implemented and presented on a browser chronologically and iteratively.
Progress Note Progress Note Problem list Problem list Initial record Initial record Progress Chart Progress Chart Work S heet
Assessing
Assessing
Scheduling
Scheduling
Healthcare navigation
System
Healthcare navigation
System
Plan
Plan
To do
To do
‘Clinical pass method ’ based scheduler
Data / Image
Safety Management
Record
Record
Do / Done
Do / Done
Ordering
Ordering
Watching
Watching
Immediate Attention Items SummeryFig4 the Index browser of Healthcare Navigation System; Specialists are able to access suitable function module on demand with this integrated browser.
6.3. Responsibilities for data users
Using conventional technology, it is difficult to fit our traditional handwriting with the clinical process. (In Japan, the common procedure for “official document” is simultaneous recording by physician himself with conducting medical treatment except operation or invasive treatment record. It is unusual that physicians make oral record of the findings of his patients’ condition, results of examination and treatment and so on.)
In the case of the Hiroshima University Hospital and associated hospitals, the process of problem
identification, target setting, planning, ordering, order confirmation, result reporting, and evaluation are carried out with a combination of computerized and manual documentation.
A questionnaire survey of all healthcare staff of several hospitals in Hiroshima was conducted, focusing on assessing the perceived advantages and disadvantages of the EHR on medical care safety and operation efficiency.
The results are the following:
6.3.1. Advantages of the EHR. The perceived
advantages of the EHR include:
a) Availability of objective information; the medical and nursing care process are documented in line with the organizational rules such as operation management, procedures, and recording forms.
b) The need for repeated copying is reduced, which potentially increases operation efficiency. Furthermore, some specialists answered that computerization was effective in overcoming the drawbacks of handwritten records.
6.3.2. Disadvantages of the EHR. These contrast with
the following perceived disadvantages:
a) Security assurance is difficult; Accidental system troubles disrupt recording or daily operation. Sometimes, a stored record is deleted.
b) It is difficult to draw attention to specific issues in the clinical process; with handwriting, it is easy to emphasize important parts of a document.
c) Lack of flexibility in operation; specifically, slow response. Due to the complicated s creen layers and monotone screen layout and presentation, the recording operation is made difficult. d) Time sequences are difficult to represent;
information retrieval is difficult, especially across different data classes, such as test results and pharmaceutical history (Database structure has to be improved.)
e) Interactive use involving several specialties is particularly inconvenient. This impacts team care negatively. (Traditionally, specialized sections have evolved independently, which now leads to the need to integrate these separate systems.)
7. Discussion
Recently, Japan is facing the critical issue of accountability to secure patient safety. Then, the appropriate recording and post-evaluation of medical care process is expected as effective solution measures. ( Motive for the increased attention to quality is a number of adverse or incorrect events that were identified in the clinical process. As a result, the management of the safety of the healthcare process and the manner of disclosure of patients’ information have become high priority issues [3]-[6].) This paper focuses on the HR architecture
7.1. Confidentiality and Data disclosure are skeletal essentials of patient oriented care
The Japan Personal Data Protection Act was established in May, 2003. It is based on OECD 8 principles which practically became the major pillar of US HIPPA-led worldwide legislation. After adding new clauses such as the obligation of organizations dealing with personal data (Hospitals, healthcare facilities, nursing homes and so on in the medical field), it was put into effect in April, 2005. [7]
Since the act urges that ministries which manage the project “should develop the guidelines for the right” use of personal data, the National Life Council issued a guideline on personal data protection based on the fundamental principles and anticipated future direction of the act. [8]
Under the ongoing sophisticated computerization, and with consideration of the usefulness of personal data to both the public and private sectors, the act aims to protect personal right and benefit, including individuality, dignity, and property. This is expected to lead to
well-balanced data access. [9]
It is not too much to say that medical services rely on the accumulation and use of PHD.
Besides, without doubt, “right” data access is the key to the improvement in public health and the development of science. Here, the Personal Data Protection Act will be
refocused in order to patient oriented healthcare.
7.2. Requirements for Safety Management of
Healthcare Record
7.2.1. Securing accountability and Authenticity.
Healthcare record originates from patients and their families who are benefited by medical service. Then, medical care record is described by diverse medical specialists who extract information from patients based on their individual viewpoints in the process of medical examination, treatment, and nursing. Furthermore, the recording responsibility is certified as original sources.
7.2.2. Securing integrity. Team medical practice
concerns diverse specialists. In addition to the conscious manipulation, the content change caused by copying errors during information transmission is unaccepted.
7.2.3. Securing availability. Securing availability is
the top priority in PHD computerization. It is essential that the medical care beneficiaries and the authorized specialists for information use can refer PHD as needed. Consequently, the following requirements are the major pillar.
a) “Correct information” is recorded in “understandable expression.”
b) “Integrated information sharing” is carried out between medical care beneficiaries and specialists concerned.
c) “Information flow” is “shown in record.”
d) Not only personal record but also ”information of similar cases” can be referred as needed.
7.3. The requirements for EHR functionality
The following principles have been defined for EHR functionality:a) Security, authenticity, accessibility on demand, and preservation
b) Convenient and reliable documentation in
accordance with the need of the medical staff during the team treatment process
c) Support for prompt overview and easy generalization of medical treatment process on demand
d) Information sharing by all staff concerned On the other hand, despite our effort to fit the care process to system operation, the current imperfect system has, in the opinions of the healthcare staff, the potential to become so complicated and unusable that it might decline the operation efficiency and threaten safety. We therefore have to re-evaluate the structure; functionality and architecture of our HR system form the perspective of safety and healthcare quality in order to arrive at a better blueprint for the next generation system.
8. Conclusion
In Japan, majority of medical facilities have aimed at constructing the integrated-typed EHR, whose current function is still imperfect in terms of information sharing in local healthcare network. Specifically, despite the need of common data item set, Japanese EHR system is facing the following issues. 1) Due to the individual data item sets expression in each EHR, it is difficult for medical specialists to understand the record description of other medical teams. 2) Under the popular
time-sequenced recording, medical process is not easily understandable. The reasons are; 1) Primarily, the construction of EHR was based on hand-written HR of individual medical facilities. 2) HR description methods did not focus on the concept that recording of medical process would lead to medical safety. Consequently, based on the preceding points, this study drew out the new guidelines from 7 viewpoints.
Guidelines for healthcare record description will enable medical professionals to record systematically the common data on patients concerned during medical practices, which aims at the further efficient and continuous patient-oriented medical care.
Self check sheet for safety medical care: Based on the above guidelines, this sheet will be available in checking and evaluating the recording descrip tion. At the same time, nation-wide network systems of their procedures and standards are its ongoing project. Furthermore, in 2005, we began the related research which focuses on EHR construction used as strategic tool to improve the safety medical care. Traditionally, in terms of healthcare record, disclosure to patients has not been the priority. At the same time, medical professionals have been heavily tasked due to several data input including ordering of medical practices, assuring orders, and recording practices. Conclusively, current EHR cannot cope with thinking and practicing process of doctors and nurses in the innovative medical playing field. Here, this workshop will discuss its future direction based on the working hypothesis that the conception of “simple recording” will give a negative impact to its development.
Information technology guided communication should be the priority for the future in order to enhance the patient’s participation in his healthcare, as well as safe management of team practice. In addition, our concept for the next generation EHR emphasizes safety management and patient participatory health care.
Though the EHR is expected to render documentation quality more comparable, its social comprehension has not yet reached a consensus, and the idea that it is just the computerized version of the traditional paper record is still prevalent.
In order to develop information basis which contributes to securing higher quality, efficiency, and transparency of healthcare, not only technical innovation,
but also health information officers with global standard for healthcare play the leading role. Therefore , fostering such specialists in information venders and management hospital staffs will be the key.
Japan Association of Medical Informatics (JAMI) launched the human development program to educate “Healthcare Information Technologists (Health IT)”since 2003. Now, at the end of 2005, there are 3843 Health Information Technologists. This is expected to contribute to a solution of the identified issues.
9. References
[1] IT policy objectives package 2005,
http://www.kantei.go.jp/jp/singi/it2/kettei/050224/0502 24pac.html (Visited at 03.19.2006)
[2] K. Ishikawa, Nakao Konishi, Hidehiko Tsukuma, Satoko Tsuru, Akie Kawamura, Norikazu Iwata, Takeshi Tanaka. A Clinical Management System for patient participatory : Health Care Support, International Journal of Medical Informatics 2004; 73:243 -249
[3] Kohn LT, Corrigan JM, Donaldoson MS. To err is Human: Building a safer Health System. Washington, DC: National Academy Press; 1999
[4] Brenan TA, Leap LL, et al. Incidence of Adverse Events and Negligence in Hospitalized Patients: Results of the Harvard Medical Practice Study I. N England J Medicine. 324:307-376, 1991.
[5] Thomas EJ,Studdent DM, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med. Care. 38:261-271,2000.
[6] Wilson RM, Runciman WB, et al. The quality in Australian Health Care Study. Med J Australia. 163:458-471, 1995. [7] Japan’s personal information act, [Law No.57, 2003] [completely enforced on April 1, 2005]
http://www.privacyexchange.org/japan/JapanPIPA2003v3_1.pd f (Visited at 03.19.2006)
[8] The guideline for the appropriate handling of personal health data
http://www.mhlw.go.jp/shingi/2004/12/dl/s1224-11a.pdf (Visited at 03.19.2006)
[9] The guideline for safety manage ment of the health information systems
http://www.mhlw.go.jp/shingi/2005/03/dl/s0331-8a1.pdf (Visited at 03.19.2006)
(Acknowledgements)
I would like to thank Jochen Moehr, Francis Roger France, Albert Bakker, and Barry Barber for giving advice for this article.This research was supported by the Japanese Ministry of Education 2005 and Sciences and Ministry of Health Welfares and Labors 2004 -2005.