Traumatic Rupture of Renal Angiomyolipoma Managed with
Angioembolization Followed by Elective Surgery: A report of
Two Cases
Yu-Pao Hsu, MD, Ray-Jade Chen, MD, Jen-Feng Fang, MD, and Being-Chuan Lin, MD
J Trauma. 2005;59:737–741.
R
enal angiomyolipoma (AML) is a rare benign neoplasmof kidney origin. It is mainly comprised of varying amounts of adipose tissue, smooth muscle, and blood vessels. Most patients with small tumors have no clinical symptoms and the tumors are frequently detected by ultra-sound or computed tomography (CT).1 The tumor size is always related to clinical symptoms. Steiner et al. reported that patients with tumor sizes greater than 4 cm were more frequently symptomatic (46%) and required surgery (54%).2 Spontaneous rupture of renal AML is the most severe com-plication. Koh and George speculated that large intratumoral pseudoaneurysm on contrast-enhanced CT was an important predictor or potential life-threatening tumor hemorrhaging.3 Ya-makado et al. demonstrated that groups with spontaneous tumor ruptures have significantly larger sizes of tumors and aneurysm than groups with unruptured ones. Tumor size of 4 cm or larger and aneurysm size of 5 mm or larger were used as predictors of rupture.4In the acute setting of a hemorrhage, transarterial em-bolization has been used as the treatment of choice for hemo-stasis in cases of stable hemodynamics.5,6This could provide
immediate access to locate the precise site of bleeding and to block the bleeder at the same time.6On the other hand, angio-embolization may occlude the aneurysm, destroy solid mass, and eventually, may reduce the size of parts of the tumors.2,4,7– 8
When the patient’s clinical condition was stable after emboliza-tion, elective surgery or CT follow-up was recommended.9
Regarding the traumatic rupture of renal AML, there have been no reports related to its management. Here, we report two cases of renal AML with traumatic rupture, and suggest the management guidelines for this kind of tumor rupture.
CASE REPORTS
Case 1
A 31-year-old female was struck by a car while she was riding a motorcycle. Two weeks before the accident, she had palpated a mass on her right abdomen and was scheduled to receive radiologic investigation in a hospital. She was ini-tially sent to a local hospital. No specific examinations or treatments were performed there, and she was discharged 6 hours after admission. The next morning she complained of severe pain over her right abdomen and flank. She was immediately brought to our emergency department (ED). On arrival, initial homodynamic status was stable, but physical examination revealed a huge tender mass palpated on the right side of her abdomen and flank. Gross hematuria was also noted.
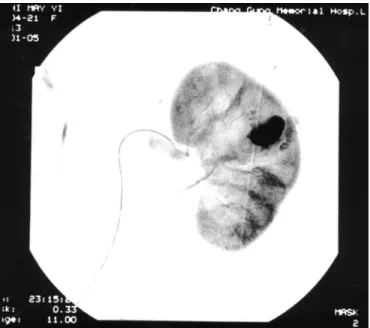
Abdominal CT showed a huge mass, which measured 10⫻ 15 cm and contained adipose tissue, was ruptured with perirenal hematoma and contrast extravasation on the right kidney (Fig. 1). Hypovolemic shock (blood pressure was 73/28 mm Hg) developed 4 hours after her arrival. Resusci-tation, crystalloid (1,000 cc) and blood transfusion (red blood cells, 2 units) made her hemodynamics return to normal. Renal angiography was performed immediately. It revealed a space-occupying lesion from the low pole of the right kidney and abnormal hyper tropic arteries with multiple tiny aneu-rysms (1–2 mm) and contrast extravasation (Fig. 2). Trans-catheter arterial embolization with micro-coil and gel form powder was performed.
Two days after the accident, respiratory distress developed and end tracheal intubation was performed; diffusion haziness of the right lung field was found on chest x-ray film. A chest tube was inserted on the right and 800 cc of blood initially flowed out. Right flank pain was complained of and persistent drop of hemoglobin was noted. Due to suggested ongoing tumor hem-orrhaging, repeated angiography (Figure 3) was performed and it demonstrated a small pseudoaneurysm (2 mm) with contrast extravasation of the inferior branch of right renal artery. Micro-coil embolization was performed.
Her condition became stable after two of arterial embo-lizations. Due to huge and fragile ruptured tumor with indis-tinct anatomy, elective nephrectomy including the mass was performed 1 month after admission. The pathology
demon-Submitted for publication May 16, 2003. Accepted for publication January 20, 2004.
Copyright © 2005 by Lippincott Williams & Wilkins, Inc.
From the Department of Trauma and Emergency Surgery, Surgical Department, Chang Gung Memorial Hospital, Taoyuan, Taiwan.
Address for reprints: Yu-Pao Hsu MD, Department of Trauma and Emergency Surgery, Chang Gung Memorial Hospital, Chang Gung Univer-sity, 5 Fushing Street, Taoyuan, Taiwan; email: yupao@cgmh.org.tw.
strated renal AML. She was discharged 1 week after the operation.
Case 2
A 62-year-old female on foot was struck by a car on her back left side. On arrival to our ED, shock (blood pressure was 86/55 mm Hg) was noted; after resuscitation with crys-talloid (Lactate Ringer 2,000 cc) and blood transfusion (whole blood, 2 units), her homodynamic status returned to normal. Physical examination revealed an ecchymosed on the
left side of her back. Abdominal tenderness, especially on the left side of her abdomen, was found.
Emergent abdominal CT (Fig. 4) showed that an adipose-containing tumor (measured 10 ⫻ 10 cm) with perirenal hematoma and contrast extravasation was noted at the upper pole of the left kidney. Traumatic rupture of the renal AML was impressed. Emergent angiography of the left renal artery (Fig. 5) showed a huge aneurysm (15 mm) with contrast pooling on the upper pole of the left kidney. Selective em-bolization with micro coil was performed smoothly. After angioembolization, her condition was stable. She was dis-charged 2 weeks after angioembolization with restriction of her activities at home. Follow-up CT (Fig. 6) 2 months after
Fig. 1. A large adipose-containing mass, measured 20⫻ 15 cm,
with perirenal hematoma and contrast extravasation located on the low pole of the right kidney.
Fig. 2. This shows that a space-occupying lesion with abnormal hypertrophy arteries and multiple tiny aneurysms (1–2 mm) com-bined with contrast extravastion on the low pole of the right kidney.
Fig. 3. Repeated angiogram shows that a small aneurysm (2 mm)
with contrast extravasation on the inferior branch of the right renal artery.
Fig. 4. This shows that an adipose-containing mass with huge perirenal hematoma and contrast pooling, measured 10⫻ 10 cm, on the upper pole of the left kidney.
angioembolization demonstrated absorption of the perirenal hematoma, which measured 7.0 ⫻ 7.0 cm. Partial nephrec-tomy was scheduled. However, attributed to severe adhesion of tumor to surrounding organs and massive hemorrhage from ruptured tumor during manipulation, she eventually underwent left nephrectomy after the image study was per-formed. She was uneventfully discharged 1 week after sur-gery. Pathology demonstrated renal AML.
DISCUSSION
Renal AML is composed of varying amounts of three tissues including mature adipose tissue, smooth muscle and
thick walled blood vessels. It predominately occurs in women (74%–94%).2,4,10 –11 Thirteen of 25% of neoplasm involve bilateral kidneys, in which patients have high rate of tuberous sclerosis.2,10Most patients are asymptomatic, and are often incidentally diagnosed using results of CT, or ultrasound. However, the symptom severity of patients is frequently related to the tumor size. Those with tumor sizes less than 4 cm are less often symptomatic (24%), while those with tumor sizes greater than 4 cm are more often symptomatic (52%).2 The most common symptoms of patients with renal AML are abdominal or flank pain (84%), palpable mass (53%), hem-orrhage (32%), anemia (21%) and hypertension (21%).2
Spontaneous rupture of renal AML, which is a rare but potentially life-threatening condition, is the most severe complication.9 –10,12Ultrasound and CT are the most valuable initial examinations. Ultrasound can easily demonstrate peri-renal and subcapsular fluid collections as a screening test. CT can reveal a more definitive and precise image of the exact location and extent of the hemorrhage.13–15In cases of spon-taneous tumor rupture with perirenal hematoma, Belville et al. reported that the accuracy of CT for the diagnosis of renal AML was 92%, when a renal mass was demonstrated and interpreted using established criteria.16Zagoria et al. recom-mended that CT should be performed first, then angiogram as the second examination if no mass was detected.17 If both imaging studies failed to demonstrate a renal mass, then follow-up with thin-slice CT was indicated. Repeat CT may not only allow for resorption of perirenal hematoma and allow for the appearance of a small tumor previously hidden by blood, but also enable differentiation between a benign and malignant neoplasm.17–18Osterling et al. recommended that symptomatic tumors smaller than 4 cm should be ob-served regularly with CT or ultrasound, while those greater than 4 cm should be studied by angiography and considered for arterial embolization or surgery.10
The nontraumatic rupture of neoplasm is related to tumor size. As the tumor grows, the blood flow supplying the tumor increases, which leads to vessel dilation and aneurysm formation.4,19On the other hand, rupture of an aneurysm may cause an increase in tumor size. Yamakado et al. reported that aneurysm formation was observed in 22 (76%) of 29 tumors of renal AML, in which 100% of the ruptured tumors had aneurysm formation. The mean tumor size (11.4 cm) and aneurysm size (13.3 mm) were significantly larger than those (5.0 cm and 2.4 mm respectively) in the group with unrup-tured tumors. Aneurysms formation appeared to be related to tumor size, and large aneurysms had higher probability of rupture.4
In cases of acute hemorrhages of tumors, transcatheter arterial embolization has been used as the treatment of choice to stop active bleeding.4,14 –17,19 The embolization could be useful in preventing growth and spontaneous rupture not only in ruptured tumors but also in unruptured ones.4 – 6,19 Embo-lization may help prevent tumor growth by resulting in oc-clusion of the aneurysm, destruction of the solid mass, or
Fig. 5. Emergent angiogram shows a huge aneurysm (15 mm) with
contrast pooling on the upper pole of the left kidney.
Fig. 6. Follow-up Ct shows that the mass reduced (from 10⫻ 10 cm
to 7.0 ⫻ 7.0 cm) in size after angioembolization and hematoma absorption at 2 months after angioembolization.
both. In spontaneous AML ruptures, most of the cases raging from 83-100%, were successfully managed with arterial embolization.2,4,6,18 The tumor sizes reduced in 57-80% of the tumors and size regression of 13-46% according to long-term follow-up.4,6,19
As far as traumatic rupture of AML, there have been two case reports in the literature,20 –21 but neither concerned the
angioembolization management. In our two cases, both had initial hypovolemic shock after trauma. After resuscitation, homodynamic status soon returned to normal. Initial abdom-inal CT revealed huge retroperitoneal perirenal hematomas with contrast extravasation. Both were managed with emer-gent arterial embolization, though the former case needed repeat arterial embolization for aneurysm formation with con-trast extravasation. In conditions of emergent laparotomy for ruptured tumor bleeding, there is major blood loss, even uncontrolled hemorrhage during manipulation, in part due to pre-operative massive bleeding, possible ensuing hypother-mia, and coagulopathy. This is in part due to the huge fragile tumor and blood clot interfering with the anatomic dissection, and difficulty for hilar accessibility for vascular control. However, transcatheter arterial embolization could localize the bleeding site and perform an embolization for immediate hemostasis during the limited amount of critical time. In cases of stable homodynamic status, the vascular access could provide a more noninvasive and effective method to control acute hemorrhaging of tumors than an emergent lapa-roscopy could.
After angioembolization, the conditions of both cases sta-bilized. Owing to the high possibility for rebreeding of the large tumor in the former case and the large aneurysm (15 mm) of the latter case, elective surgery with nephrectomy was performed in both cases. Partial nephrectomy remains the standard of surgical intervention of AML.10,22 However, due to enormous fragile ruptured tumor for the former case, and post-embolization se-vere adhesion of tumor and uncontrolled hemorrhage on manip-ulation for the latter case, nephrectomies were performed. Both were discharged without complications.
According to our experiences, we designed an algorithm for the management of traumatic rupture of renal AML (Fig. 7). When the homodynamic status of the patient was persistently unstable after resuscitation, emergent laparoscopy for nephrec-tomy is mandatory. However, in cases of stable hemodynamic status after resuscitation, emergent Transcatheter arterial embo-lization is indicated for hemostasis. After the angioemboembo-lization, when the homodynamic status of patient is unexpectedly unsta-ble, emergency laparoscopy nephrectomy is mandatory. When the hemodynamic status is stable and there are no signs of further tumor bleeding, elective surgical intervention or conser-vative management with CT follow-up is chosen according to the tumor size and the aneurysm formation.
REFERENCES
1. Haidu SI, Foote FW Jr. Angiomyolipoma of the kidney: report of 27 cases and review of the literature. J Urol. 1969;102:396–401. 2. Steiner MS, Goldman SM, Fishman EK, Marshall, FF. The natural
history of renal angiomyolipoma. J Urol. 1993;150:1782–1786. 3. Koh KB, George J. Radiological parameters of bleeding renal
angiomyolipoma. Scand J Urol Nephrol. 1996;30:265–268. 4. Yamakado K, Tanaka N, Kobayashi S, Yanagawa M, Takeda K.
Renal angiomyolipoma: relationships between tumor size, aneurysm formation, and rupture. Radiology. 2002;225:78–82.
5. Zerhouni EA, Schellhammer P, Schaefer JC, Drucker JB, Jaffe AH, Gonzalez JE. Management of bleeding renal angiomyolipoma by Tran catheter embolization following CT diagnosis. Urol Radiol. 1984;6:205–209.
6. Earthman WJ, Mazer M, Winfield AC. Angiomyolipoma in tuberous sclerosis: subselective embolotherapy with alcohol with long term follow up study. Radiology. 1986;160:437–441.
7. Lemaitre L, Robert Y, Dubrulle F, et al. Renal angiomyolipoma: growth followed up with CT and/or US. Radiology. 1995;197:598– 602.
8. Mourikis D, Chatziioannou A, Antoniou A, Kehagias D, Gikas D, Valahos L. Selective arterial embolization in the management of symptomatic renal angiomyolipomas. Eur J Radiol. 1999;32:153– 159.
9. Yip KH, Peh WCG, Tam PC. Spontaneous rupture of renal tumors: the role of imaging in diagnosis and management. Br J Radiol. 1998;71:145-154.
10. Oesterling JE, Fishman EK, Goldman SM, Marshall FF. The management of renal angiomyolipoma. J Urol. 1986;135:1121–1124. 11. Tsai HN, Chou YH, Huang SP, Wu WJ, Wang CJ, Huang CH. The
management strategy of renal angiomyolipoma. Kaohsiung J Med
Sci. 2002;18:340–346.
12. Bosniak MA. Spontaneous sub capsular and perirenal hematomas.
Radiology. 1989;172:601–602.
13. Srinivasan V, Turner AG, Blackford HN. Massive intraperitoneal hemorrhage associated with renal pathology. J Urol. 1994;151:980–981. 14. Peh WCG, Yip KH, Tam PC. Spontaneous renal pseudo aneurysm
rupture presenting as acute intraabdominal haemorrhage. Br J
Radiol. 1997;70:1188–1190.
15. Chan IKW, Chan KL. Spontaneous rupture of renal tumors presenting as surgical emergency. Br J Urol. 1993;71:253–255. 16. Belville JS, Morgentaler A, Loughlin KR, Tumeh SS. Spontaneous
perinephric and sub capsular renal hemorrhage: evaluation with CT, US, and angiography. Radiology. 1989;172:733–738.
17. Zagoria RJ, Dyer RB, Assimos DG, Scharling ES, Quinn SF. Spontaneous perinephric hemorrhage: imaging and management.
J Urol. 1991;145:468–471.
18. Bosniak MA, Megibow AJ, Hulinick DH, Horii S, Raghavendra BN.
CT diagnosis of renal angiomyolipoma: the importance of detecting small amounts of fat. AJR. 1988;151:497–501.
19. Igarashi A, Masuyama T, Watanabe K, Higaki Y, Kuramoto N, Yoshida H. Long-term result of the Tran catheter arterial
embolization for ruptured renal angiomyolipoma. Jpn J Urol. 2002; 93:702–706.
20. Comes Almeida F, Reis J, Riberio AM. Traumatic rupture of angiomyolipoma: a case report. Archivos Espanoles de urologia. 2002;53:286–289.
21. Renz B, Sorini P, Watchtel TL, Perry R. Traumatic rupture of a renal angiomyolipoma. Injury. 1989;20:50–51.
22. Heidenreich A, Hegele A, Varga Z, von Knobloch, R, Hofmann R. Nephron-sparing surgery for renal angiomyolipoma. Eur Urol. 2002; 41:267–273.