Effects of home-based physical therapy on functional outcome of
disabled
elderly
:
the
Experience of Miaoli County in Taiwan
Wen-Dien Chang, Assistant Professor, Ph.D.,*
Department of Sports Medicine, China Medical University.
Present address: No. 91 Hsueh-Shih Road, Taichung City, Taiwan (R.O.C)
[E-mail: changwendien@mail.cmu.edu.tw]
*
Correspondence author:
Wen-Dien Chang, Assistant Professor, Ph.D.,
Department of Sports Medicine, China Medical University.
Present address: No. 91 Hsueh-Shih Road, Taichung City, Taiwan (R.O.C)
TEL: (886)- 4-22053366 ext. 7605
FAX: (886)-
4 -22061724
E-mail: changwendien@mail.cmu.edu.tw
ABSTRACT
〔Purpose〕In response to the increase of Taiwan's aging population, and to improve the daily living
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
year long-term care program providing home-based physical therapy services. The purpose of our study was to design an assessment form and analyze the effects of home-based physical therapy. 〔Subjects and Methods〕Disabled elderly who received home-based physical therapy were identified,
and therapists provided treatment and evaluated their functional improvement using the designed home-based assessment form.
〔Results〕 The results of our study showthat the total correlation coefficient (r) of test-retest reliability was 0.89 and the internal consistency reliability had a Cronbach's α was 0.91. The test-retest reliability was high as assessed by the intraclass correlation, and the home-based assessment form was highly correlated with the Barthel Index. Among the 255 subjects (age: 76.88 ± 9.69), 120 (47.1%) had cardiovascular diseases, and 108 (42.35%) had orthopedic diseases. Subjects received 4.54 ± 2.35 treatments, and the score of the home-based assessment form was 53.60 ± 23.77 before treatment, and 56.01 ± 21.01 after treatment.
〔Conclusions〕After a clinical test for disability, the home-based assessment is a suitable assessment
of improvement of function ability. However, the number of subjects was too small and the treatment time was too short, and further investigation of this issue is still needed.
Key words: home-based physical therapy, long-term care, disabled elderly.
INTRODUCTION
In response to the increase of Taiwan's aging population, and to improve the daily living function and quality of life of the elderly, the government of Miaoli County has implemented a ten-year long-term care program. It provides home-based rehabilitation services for the elderly. There are eighteen
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
townships in Miaoli County of Taiwan. The population of this county is mainlycomprised of 20 ~ 59
year-old, who account for 330,000 people, 59.13 % of the population. The elderly population, aged over 65 years old, numbers is about 70,000 people, representing 13.32 % of county's population1).
Therefore, the population of Miaoli County of Taiwan has entered the aging generation. The aging
tendency shows that Miaoli County has a higher aging index than neighboring districts, such as Taoyuan County, Hsinchu County, and Hsinchu City in Taiwan1).
The elderly population of Miaoli County in Taiwan is gradually increasing, but the services of
elderly care are still limited because of its remote district. There are also many problems in providing
home-based physical therapy for disabled elderly2). The government plans to promote long-term care
via integration of regional hospitals and the establishment of a long-term care center. The assessment and functional status of disabled elderly needed to be recorded. The Barthel Index is the most
commonly used index in long-term nursing care3), but it is not suitable for assessing the progression of
home-based physical therapy. Therapists cannot easily record the effect of home-based physical therapy, because of a lack of a suitable Chinese functional assessment for the elderly in Taiwan. Toward this aim, we designed an assessment form and analyzed the effects of home-based physical therapy.
SUBJECTS AND METHODS
43
44
45
46
47
48
49
50
51
52
53
54
55
56
57
58
59
60
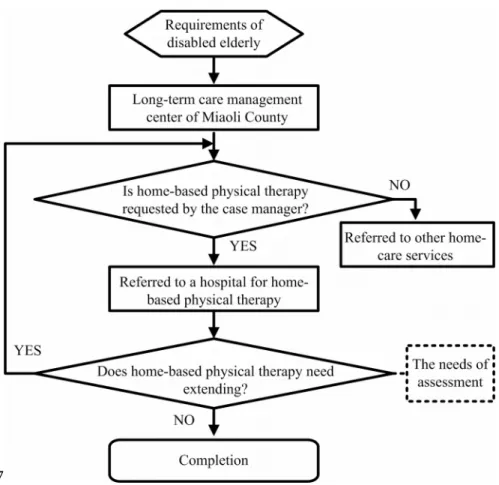
The long-term care center referral and treatment process are shown in Fig. 1. We found that
disabled elderly were referred to the local hospitals, and an assessment was needed for the treatment and re-treatment criteria for home-based physical therapy.The treatment programs include balance, indoor gait activities, flexibility and progressive strength training, and are professionally supervised by a physical therapist. The goals for home-based physical therapy for all disabled elderly are the
establishment of safe transfers and independent functional activity.
We referred to previous studies4, 5), and designed the home-based assessment form for assessing the
motor function of disabled elderly. This Chinese form contains 12 items: ability to independently feed and eat, wash face and brush teeth, wear clothes, wear pants, take a bath or shower, urinate, defecate,
transfer from toilet, take pants off before bowel movement, transfer from bed to chair or wheelchair, walk 45 meters, and walk up and down 12 steps. A 7-point scoring criterion is used. 7 points,
completely independently; 6 points, needs assistive devices but independent; 5 points, need to be reminded and requires supervision; 4 points, minimum assistance (requires 25% assistance); 3 points,
medium assistance (requires 50% assistance); 2 points, maximum assistance (requires 75%
assistance); 1 point, fully dependent (requires 100% assistance). The reliability and validity of these items were tested by eight experts in the field of rehabilitation with an average 9.31 ± 4.67 yearsof experience.
This study procedure was approved by the Institutional Review Board of Human Research of Da-chien general hospital. The clinical tests were conducted from September 2010 to December 2011, and
61
62
63
64
65
66
67
68
69
70
71
72
73
74
75
76
77
78
79
recruited subjects were the cases that were referred from the long-term care center of Miaoli County to
the hospital. The records of physical therapy outcomes were analyzed using the statistical analysis software, SPSS 13. Wilcoxon's test was used to analyze the difference in each item between before and after physical therapy. We also used Spearman's correlation coefficient to examine the correlation between the scales of the home-based assessment form and the Barthel Index.
RESULTS
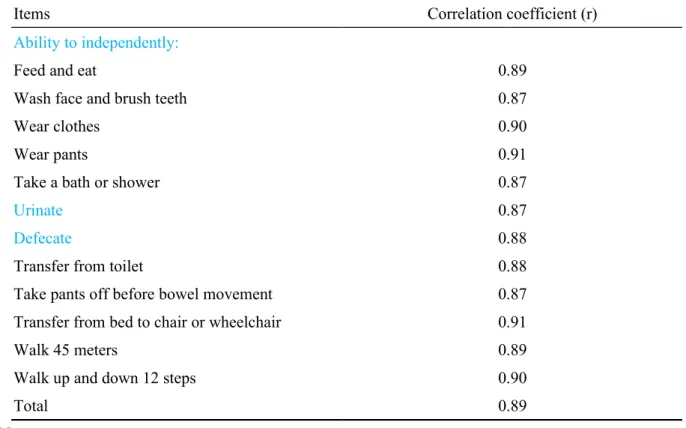
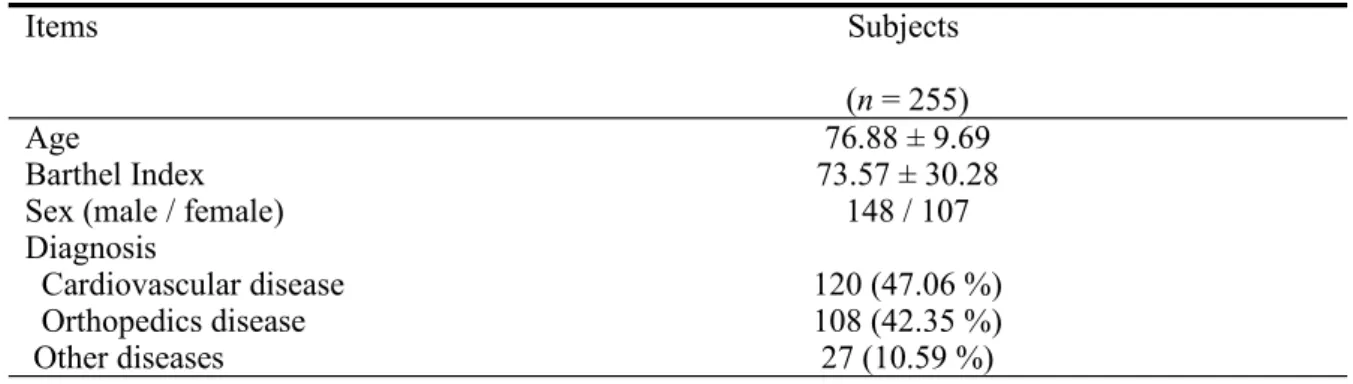
For the test-retest reliability within 2 weeks pilot testing of the home-based assessment form (Table 1), the total correlation coefficient (r) was 0.89 and Cronbach's α was 0.91. The test-retest reliability was high as assessed by the intraclass correlation, and the home-based assessment form was also highly correlated with the Barthel Index. The 255 subjects of home-based physical therapy, who were diagnosed as disabled elderly (Table 2), had an average age of 76.88 ± 9.69 years. The average number of treatment times was 4.54 ± 2.35,and the average total score of home-based assessment was
53.60 ± 23.77 (Table 3). After physical therapy, the total score increased to 56.01 ± 21.01, but there were no significant differences between before and after treatment (p > 0.05)in any item except for
“Transfer from bed to chair or wheelchair” (p < 0.05). The Barthel Index score before treatment was 73.57 ± 30.28, and there was a positive correlation between the Barthel Index and the total scores of
the home-based assessment (p < 0.01).
80
81
82
83
84
85
86
87
88
89
90
91
92
93
94
95
96
97
DISCUSSION
After the home-based physical therapy, the average total score of the designed home-based assessment form increased by 2.41 ± 3.90. This shows that physical therapy improved the functional activities of the elderly at home. This is in agreement with the result of De Jonge et al6). We also find
that the time for contacting with family members or patients was insufficient due to fewer home-based physical therapies. Lin et al. indicated that detailed assessment records of home-based physical therapy need to be kept, starting with discharge planning records7). A single and suitable assessment
form would help to record and improve the efficiency of home-care. Jao et al. expressed the opinion
that a detailed record of home-based physical therapy needed to be integrated with those of home-care services provided by other health care professionals8). It would make the collation of patients’
information more efficient. Therefore, the assessment record (containing the referral of the case report) and treatment records (including health education and rehabilitation) need to be clear and well-documented, in order to improve the effect of long-term care.
The results of this study found that the average number of home-based physical therapy treatments
was only 4.54 times, and the treatment frequency was once a week. In aprevious study of long-term care, it was reported that once a week home-based physical therapy improved lower limb motor function9). Lin et al. also found that weekly home-based physical therapy helped to improve the
functional performance of patients with muscle atrophy lateral sclerosis and maintained their physical and mental functions10). The results of our study also found once a week home-based physical therapy
99
100
101
102
103
104
105
106
107
108
109
110
111
112
113
114
115
116
117
helped the elderly to increase their functional abilities. When Wang et al. compared the effects of different courses of home-based physical therapy, they found a twice a week course had better treatment effects than a once a week course11). Therefore, we also suggest that the government should
increase the treatment frequency and provide other treatments, such as occupational therapy and psychotherapy. This may significantly improve the functional abilities of the elderly.
Our home-based assessment scale was consistent with the Barthel Index, and could be used for the assessment of disabled elderly. Because the Barthel Index is used to record the individualize care services and supportive services, it is a common used evaluation tool for patients, and it is also a popular body function index in nursing care3). But its validity is deficient for home-based
rehabilitation evaluation, and there are no adequate evaluation tools for home-based physical therapy. As all the rehabilitation programs in this research were physical therapy, we used a self-developed
evaluation form, which is limited to home-based physical therapy.
In this study, the referral document of the case manager provided patients’ basic information, Barthel Index and general status, which are not sufficient for determining subjects' disability and
requirements for home-based physical therapy. This resulted in therapists spending time on their first visit re-evaluating patients, and highlights a problem in service coordination. Hsieh et al. discussed the family assessment model as a framework for patients’ status evaluation12). The information collected
by interview, including basic personal and family information, family development stage and tasks,
118
119
120
121
122
123
124
125
126
127
128
129
130
131
132
133
134
135
environment, structure, function and pressure management, can be used for reference and as a guide
for home-based physical therapy.
This research found that the home-based physical therapy onlyimproved “transfer from bed to chair or wheelchair” (p < 0.05). It means that the improvement of patients’ function ability also can be found after a short treatment program. The improvement may have been a result of the home-based physical therapy training. This study was limited by the small number of subjects and the short treatment programs, and further investigation is required.
REFERENCES
1) Chiu TI, Spencer GA: Functional health status among rural and urban older adults in Taiwan: the effect of personal control and social control. Int J Older People Nurs, 2010, 5: 202-210.
2)Chen SL, Mefford L, Brown J, et al.: Predictors of American elders' home stay: a secondary data analysis study. Nursing and health sciences, 2008, 10: 117-124.
3) Chang SH, Wung SF, Crogan NL: Improving activities of daily living for nursing home elder persons in Taiwan. Nurs Res, 2008, 57: 191-198.
4) Kidd D, Stewart G, Baldry J, et al.: Functional independence measure: a comparative validity and reliability study. Disabil Rehabil, 1995, 17: 10-14.
5)Dodds TA, Martin DP, Stolov WC, et al.: A validation of the functional independence measurement and its performance among rehabilitation inpatients. Archives of physical medicine and rehabilitation, 1993, 74: 531-536.
136
137
138
139
140
141
142
143
144
145
146
147
148
149
150
151
152
153
154
155
6)De Jonge KE, Taler G, Boling PA: Independence at home: community-based care for older adults with severe chronic illness. Clinical geriatrics, 2009, 25: 155-169.
7)Lin KH, Hu MH, Tang PF, et al.: The development of evaluation and referral system of physical therapy in discharge planning. FJPT, 2007, 32: 51-58.
8)Jao FC, Duh YJ: Improving muscular strength in home-care cases using multi-disciplinary physical therapy education. VGH Nursing, 2010, 27: 296-304.
9) Lin JH, Hsieh CL, Lo SK, et al.: Preliminary study of the effect of low-intensity home-based physical therapy in chronic stroke patients. Kaohsiung J Med Sci, 2004, 20: 18-23.
10) Lin KH, Hu MH, Chien WJ, et al.: The care pattern and effect of home physical therapy in individuals with amyotrophic lateral sclerosis: a preliminary report. FJPT, 2004, 29: 384-395. 11)Wang RY, Hsiung CL, Chen LH, et al.: Effects of home health physical therapy frequency on
functional outcome of stroke patients. FJPT, 2003, 28: 65-70.
12)Hsieh CC, Huang HC: The application of family assessment model to physical therapy: a stroke case report. FJPT, 2005, 30: 243-249.
156
157
158
159
160
161
162
163
164
165
166
167
168
169
170
171
172
173
174
175
Fig. 1. The referral and treatment process
177
178
179
180
181
182
183
184
185
186
187
188
189
Table 1. The test-retest reliability of the home-based assessment form
Items Correlation coefficient (r)
Ability to independently:
Feed and eat 0.89
Wash face and brush teeth 0.87
Wear clothes 0.90
Wear pants 0.91
Take a bath or shower 0.87
Urinate 0.87
Defecate 0.88
Transfer from toilet 0.88
Take pants off before bowel movement 0.87 Transfer from bed to chair or wheelchair 0.91
Walk 45 meters 0.89
Walk up and down 12 steps 0.90
Total 0.89
190
191
192
193
194
195
196
197
198
199
200
201
The data of age and Barthel Index are shown as mean ± standard deviation, and each items of diagnosis is shown as n (percentage).
Table 3. Scores before and after home-based physical therapy
Items Before (n = 255) After (n = 255) Ability to independently:
Feed and eat 5.24 ± 2.01 5.29 ± 1.90
Wash face and brush teeth 4.08 ± 2.24 4.12 ± 2.20
Wear clothes 4.35 ± 2.15 4.57 ± 1.94
Wear pants 4.29 ± 2.18 4.44 ± 2.04
Take a bath or shower 4.35 ± 2.24 4.48 ± 2.10
Urinate 5.33 ± 2.21 5.45 ± 2.00
Defecate 5.29 ± 2.22 5.41 ± 2.02
Transfer from toilet 4.55 ± 2.16 4.65 ± 2.04
Items Subjects
(n = 255)
Age 76.88 ± 9.69
Barthel Index 73.57 ± 30.28
Sex (male / female) 148 / 107
Diagnosis Cardiovascular disease 120 (47.06 %) Orthopedics disease 108 (42.35 %) Other diseases 27 (10.59 %)
203
204
205
206
207
208
209
210
211
212
Take pants off before bowel movement 4.45 ± 2.25 4.64 ± 2.11 Transfer from bed to chair or wheelchair 4.56 ± 2.16* 5.27 ± 1.47
Walk 45 meters 3.78 ± 2.24 3.97 ± 2.07
Walk up and down 12 steps 3.32 ± 2.18 3.65 ± 1.98
Total 53.60 ± 23.77 56.01 ± 21.01
* p < 0.05.