行政院國家科學委員會專題研究計畫 成果報告
全民健康保險連續處方市場之探討
計畫類別: 個別型計畫 計畫編號: NSC93-2416-H-004-049- 執行期間: 93 年 08 月 01 日至 94 年 07 月 31 日 執行單位: 國立政治大學財政系 計畫主持人: 周麗芳 共同主持人: 陳曾基 報告類型: 精簡報告 處理方式: 本計畫可公開查詢中 華 民 國 94 年 10 月 26 日
摘要 背景: 連續處方係指醫師於同一位病人持續的就診中開立相同的藥物。連續處 方是門診醫療作業中大宗的業務,具有重大的醫務管理意義。 目的: 利用自創的演算法,重新測量門診醫療連續處方的潛在規模與其財務意 義。 研究方法: 回溯性定量分析。以集合的概念,比較同一位病人連續兩次就診中 所得到的藥品異同。 研究對象: 國家衛生研究院全民健康保險研究資料庫的承保抽樣歸人檔(二十 萬人)門診資料。 主要測量變數: 病人人數,就診人次,連續處方比例(科別,主診斷),藥品 申報費用。 結果: 在 2002 年間,共有 161,532 人利用 1,994,936 次西醫門診,其中 363,231 診次開立藥品天數超過七天。在長天數藥品診次裡,140,409 診次的藥 品內容與同病人前一次在同科同主診斷的開立藥品內容相同,而 106,255 診次 則是部分藥品相同。內科、心臟科、精神科醫師開立最多連續處方,適應症則 以本態性高血壓與糖尿病為最大宗。連續開立的慢性藥品申報費用佔了西醫門 診藥費的 54.2%。 結論: 台灣全民健康保險門診連續處方的規模甚為可觀,其潛在的醫療品質與 財務意義值得進一步研究。 關鍵詞: 醫務管理、連續處方、門診醫學、藥物使用分析、藥物流行病學、資 料庫 ABSTRACT
Background: Repeat prescribing (RP), which means the transaction of issuing the same prescriptions and refilling the same drugs to patients on regular long-term treatment, forms a major part of ambulatory activities. In spite of its considerable significance in health care management, an operational definition of repeat prescribing is not yet universally available. Most of previous studies about the
dimension of RP merely performed data collection and calculation on a predetermined format.
Objective: This study presents a new approach of assessing the scale of RP with a new construct of measurement. The algorithm involves a re-classification of RP and utilizes basic concepts of set theory. The results will facilitate further understanding of practice activities.
Design: This study belongs to a retrospective and quantitative analysis. One instance of RP can be simplified by comparing the drugs prescribed to a patient on two
consecutive visits. A procedure consisting of the sets and multiple loops is written and run for the study purposes.
Subjects: The 200000-person cohort datasets from National Health Insurance Research Database of National Health Research Institutes.
Main outcome measures: Counts of patients and visits. The scale of RP (also RP subtypes) across specialties and main diagnoses. Expenses of drugs
Western medicine clinics. Among these visits, only 363231 (18.2%) visits had drug items prescribed with duration of more than seven days. In 140409 visits, all drug items of a visit were identical to those on the last visit of the same patient to the same clinic and in 106255 visits only partial drugs items. RP was frequently initiated by internists, cardiologists, and psychiatrists. The frequent indications were essential hypertension and diabetes mellitus. The drug costs in RP had accounted for 54.2% of all drug costs in the ambulatory care of Western medicine clinics.
Conclusions: The market of repeat prescribing within the National Health Insurance in Taiwan had a considerable scale. The underlying quality of care and financial meaning deserves further study.
Keywords: Health Care Management, Repeat Prescribing, Ambulatory Medicine, Drug Utilization Review, Pharmacoepidemiology, Database Management System, Health Services Research
(Version 1)
The Potential Market of Repeat Prescribing within the
National Health Insurance in Taiwan
INTRODUCTION
In the literature, there was no official definition of repeat prescribing in the
ambulatory care. While some authors, especially those in the United Kingdom, used the term for issuing of any subsequent prescription without direct doctor-patient contact (also known as ‘repeat prescription’), others directly observed the consecutive prescriptions that a patient received and did not take the consultation into
consideration (1). On the other side, the introduction of computers into general
practice, was closely related to the development of prescribing software, especially for repeat prescribing, which had the largest share of drug items and costs (2,3,4). In spite of the considerable clinical and economic significance, an operational definition was not universally available for measuring the scale of repeat prescribing. Previous studies in this field usually collected and calculated data on a predetermined format, with either paper-based or computer-related methods (5,6). Although the researcher could identify the additional marking of repeat prescribing on each drug item, it was still impossible to tell whether the doctor had really seen the patient. Furthermore, a doctor not only might use a system of repeat prescribing during a normal consultation but also could change drugs with the same system. A differential approach would be needed for retrospective and large-scale prescribing analysis.
Repeat prescribing is different from ‘refilling’ in which the patient redeems the pre-issued prescriptions at the pharmacy. While there are regulations about issuing of ‘refill prescription for patients with chronic diseases’ within the National Health Insurance in Taiwan, the repeat prescription of the European style is not allowable legally. That is, the physicians in Taiwan cannot issue prescriptions without patient contact. Therefore, we proposed a new algorithm for estimating the extent of repeatedly prescribed medicines and demonstrated it in the claims file of a representative cohort. Additionally, we would analyze its financial significance.
MATERIALS AND METHODS
The National Health Insurance (NHI) program in Taiwan has been implemented since 1995. More than 97% of inhabitants were enrolled (21,984,415 beneficiaries in the end of 2003) (7). Since 1998, the Bureau of National Health Insurance began to delegate all the claims data in electronic form to the National Health Research Institutes in Taipei (now in Miaoli county) for research use. Under the project of the National Health Insurance Research Database (http://www.nhri.org.tw/nhird/), dozens of extracted datasets were publicly released each year. Any identification data about patients, physician and institutions had been encrypted to protect privacy.
person-based sampling. For each cohort dataset, the NHIRD at first randomly sampled 50,000 people from 23,753,407 people who had ever been insured from March 1, 1995 to December 31, 2000. Then, all insurance claims belonging to these people were drawn to make up one specific cohort dataset. Not only the past data of the cohort were retrieved, the NHIRD also followed up the cohort forwards in the coming years.
The first 4 cohort datasets (R01-R04) from 2001 to 2002 were used for the
analysis of the current study. Not every one of the 200,000-person cohort was insured through the study period because of new birth, death, immigration, and emigration. The structure of the insurance claim files had been described in details on the NHIRD web site and in other published literature (8).
Besides, a list of 21,146 approved drug items of Western medicine in Taiwan were downloaded from the web site of the Bureau of National Health Insurance
(http://www.nhi.gov.tw/, accessed January 12, 2002). Different brands, strengths, and forms of each drug had an official unique identifier for claims. The Bureau of
National Health Insurance also offered a list of ATC codes (the Anatomical Therapeutic Chemical classification system, version 2000) for each drug item (9).
Our analysis focused on the cohort datasets in 2002. The data in 2001 served as reference for the first prescription of a patient in 2002. We used only the ambulatory visit file (CD) and ambulatory prescription file (OO). The analysis was simplified by comparing the drugs prescribed to a patient on two successive visits to the same clinics (hospital plus department [specialty]) for the same problem (main diagnosis). Besides, the visits were limited to normal visits to Western medicine clinics with the duration of medication more than 7 days (i.e. excluding acute illnesses). We analyzed only approved drug items.
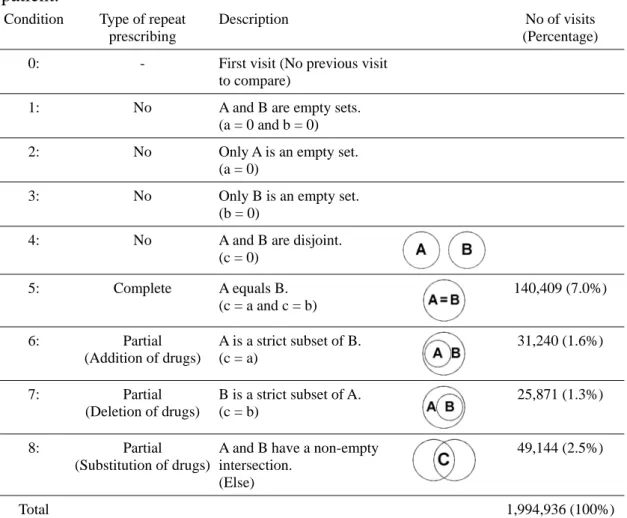
According to the set theory, there could be eight possible relationships between the set of drugs prescribed on a visit and that on the ensuing visit. The Venn diagrams were illustrated within the table. We differentiated between complete and partial repeat prescribing. The latter was further divided into three categories that
respectively represented adding, deleting and substituting some drug(s) from those prescribed on the last visit. A special program involving multiple loops of calculation was written in Perl version 5.8.7 (http://www.perl.com/).
The regular descriptive statistics were displayed. The 95% confidence interval (CI) would be added where appropriate.
This study was a secondary analysis of claims collected for the NHI in Taiwan. The analyses of the publicly available, anonymized data were permitted by the Law of Personal Data Protection in Taiwan and also exempted from review by the
institutional review board.
RESULTS
During the year of 2002, 161532 patients accounted for 1994936 ambulatory visits to Western medicine clinics (including redemption of ‘refill prescription for patients with chronic diseases’ at the clinics). Among all the visits, only 363231 (18.2%) visits had
drug items prescribed with duration of more than seven days. In 140409 (7.0% of all visits and 38.7% of visits with longer medication duration) visits, all drug items in a visit were identical to those on the last visit of the same patient to the same clinic. Besides, 106255 (= 31240 + 25871 + 49144) (5.4% of all visits and 29.3% of visits with longer medication duration) visits fell into three categories of partial repeat prescribing (Table). Totally, 12.4% of all visits and 67.9% of visits with longer medication duration resembled to the last visit to some extent with respect to drug prescription; 34428 (21.3%) patients had such an experience.
When we stratified the repeat prescribing by specialty, the internists accounted for 15.2% (21393) of visits with complete repeat prescribing, followed by cardiologists (15662), psychiatrists (12496), family physicians (11453), general practitioners (10736), neurologists (10414), gynecologists (9536), and endocrinologists (8852).
When we stratified the repeat prescribing by main diagnosis in first three digits, essential hypertension [ICD-9-CM code: 401] accounted for 14.0% (19598) of visits with complete repeat prescribing, followed by diabetes mellitus [250] (16676), Menopausal & postmenopausal disorders [627] (9335), hypertensive heart disease [402] (9075), neurotic disorders [300] (4962), schizophrenic disorders [295] (4265), chronic ischemic heart disease [414] (3403), hyperplasia of prostate [600] (3403), affective psychoses [296] (3069), chronic liver disease & cirrhosis [571] (2947), and osteoarthrosis & allied disorders [715] (2940).
In the cohort datasets of the current study, the clinics had claimed a total of 575,426,322 New Taiwan dollars for drugs in 2002. The sum included the drugs dispensed at emergency departments, dental and traditional Chinese medicine clinics. For normal visits to Western medicine clinics, 514,718,671 dollars were claimed for drugs. The visits with longer medication duration had accounted for 365,104,497 dollars (70.9% of Western medicine visits) in drug expenses. The drug items that were prescribed repeatedly had amounted to 279,164,173 dollars (76.5% of Western
medicine visits with longer medication duration, 54.2% of Western medicine visits, and 48.5% of all visits).
DISCUSSIONS
With the proposed algorithm we found that 12.4% of all visits to Western medicine clinics within the National Health Insurance in Taiwan got total or partial drug items identical to those prescribed on the last visit to the same clinics by the same patient. If a patient received a prescription with longer duration, there was a two-third chance of repeat prescribing in broader meaning. Because the medications for chronic use had reasonably a large share of pharmaceutical market, it would be not surprising to know that the monetary value of drugs in repeat prescribing had amounted to nearly a half of all drugs in the ambulatory setting.
The extent of repeat prescribing in Taiwan, even in our expanded meaning, was less that that described in one paper in the British National Health Service (6). The possible explanation might be the differences in the age structure and morbidity of patients, the accessibility for acute care (shorter waiting time), and the coverage of medical benefits.
Our results might be overestimated in the conventional meaning of repeat prescribing but underestimated in our expanded meaning. Because other acute illnesses might interpose between regular follow-ups of a long-term treatment, the mere comparison between two successive visits overlooked the continuity of repeat prescribing and confounded the calculation. Although our algorithm could have tried to differentiate acute and chronic consultations, we still encountered the occasions on which drugs for different purposes and of different supply spans were prescribed together. Furthermore, we did not include the dispensing at pharmacies in the current study. The format of claims at independently practicing pharmacies differed from that at clinics so that a linkage between prescribing and dispensing at different facilities was not easily feasible. It could not be ruled out that some prescriptions were actually not redeemed.
Traditionally, the meaning of repeat prescribing might be confined to the transaction of issuing the same medication without seeing the patient. In the era of practice computerization with electronic prescribing the reality becomes more difficult to verify and the scale of repeat prescribing remains indecipherable. We welcome a standard definition with refined algorithms that facilitates extensive understanding of practice activities.
ACKNOWLEDGEMENT
This study is based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by National Health Research Institutes, Taiwan. The interpretation and conclusions contained herein do not represent those of Bureau of National Health Insurance, Department of Health or National Health Research Institutes. This study is also supported by a grant from the National Science Council, Taipei, Taiwan (NSC 93-2416-H-004-049-).
REFERENCES
1 De Smet PAGM, Dautzenberg M. Repeat prescribing: scale, problems and quality management in ambulatory care patients. Drugs 2004;64:1779-1800. 2 Meldrum D. Simple computerised repeat prescription control system. Br Med J
1981;282:1933-7.
3 Difford F. Computer controlled repeat prescribing used to analyse drug management. Br Med J 1984;289:593-5.
4 Roland MO, Zander LI, Evans M, Morris R, Savage RA. Evaluation of a
computer assisted repeat prescribing programme in a general practice. Br Med J 1985;291:456-8.
5 Drury VWM. Repeat prescribing – a review. J R Coll Gen Pract 1982;32:42-5. 6 Harris CM, Dajda R. The scale of repeat prescribing. Br J Gen Pract
1996;46:649-53.
7 Bureau of National Health Insurance. 2003 National Health Insurance Annual Statistical Report. Taipei: Bureau of National Health Insurance, 2004.
coprescription patterns for antacids in Taiwan. Clin Ther. 2003;25:2453-2463. 9 WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC
Classification and DDD Assignment, 3rd ed. Oslo, Norway: WHO Collaborating Centre for Drug Statistics Methodology; 2000.
Table Relationships between the drug item sets of two consecutive visits of a
patient.
Condition Type of repeat prescribing
Description No of visits
(Percentage) 0: - First visit (No previous visit
to compare)
1: No A and B are empty sets. (a = 0 and b = 0) 2: No Only A is an empty set.
(a = 0)
3: No Only B is an empty set. (b = 0)
4: No A and B are disjoint. (c = 0) 5: Complete A equals B. (c = a and c = b) 140,409 (7.0%) 6: Partial (Addition of drugs) A is a strict subset of B. (c = a) 31,240 (1.6%) 7: Partial (Deletion of drugs) B is a strict subset of A. (c = b) 25,871 (1.3%) 8: Partial (Substitution of drugs)
A and B have a non-empty intersection.
(Else)
49,144 (2.5%)
Total 1,994,936 (100%)
A : The set of drugs prescribed to a patient on a visit
B : The set of drugs prescribed to the same patient on the ensuing visit
C : The set of drugs prescribed on both of the visits (i.e. the intersection of the sets A and B)
a : The number of elements (i.e. the count of drug items) in the set A b : The number of elements in the set B
計畫成果自評
本研究計畫成果內容係依照原申請計畫逐步執行,完全與原計畫相符,亦達成 預期目標。相關議題近兩年內仍陸續有文獻出現,本研究計畫成果應具有學術 價值。目前已完成英文論文初稿,將尋找合適的醫務管理類國際期刊,依據投 稿規定,修飾論文並請英文編修後投稿。