* In 1990, a totalof 22.3 million people of Hispanic origin lived in the US * Various Hispanic populations not
onlytend tolivein
differentregions of the US but are
differentin
educa-tional, occupa-tional,economic, cultural,and health
backgrmund
Cross-cultural
Medicine
A
Decade Later
Getting By
at
Home
Community-Based Long-term Care of Latino Elders
STEVEN P.WALLACE, PhD, andCHIN-YIN LEW-TING,PhD, Los Angeles, CalifomiaAlthough
evidence suggests that the morbidity and mortality of Latino elders(of
any Hispanicancestry)
are similar tothose
of non-Latino whites, Latinos have higher rates of disability. Little is known about influences on the use of in-homehealth
services designed to assist disabled Latino elders. We examine the effects of various cultural and structural factors on the use of visiting nurse, home health aide, and homemaker services. Data are from the Commonwealth FundCommission's
1988national
surveyof
2,299Latinos aged 65 and older.Mexican-American
elders are less likely than the averageLatino
to usein-home health services despite similar levels of need. Structural factors including insurance status areimportant
reasons, butacculturation is not pertinent. Physicians should not assume that Latino families are taking careof their disabled elders simply
because of a cultural preference. They should provide information and advice on the use ofin-home
health services when an older Latino patient is physically disabled.(Wallace SP, Lew-Ting CY: Getting by at home-Community-based long-term care of Latino elders, In Cross-cultural Medicine-A Decade Later [Special Issue]. WestJ Med 1992Sep;157:337-344)
M rs Martinezis an 81-year-old widow with dementia. HerAlzheimer's disease isnowatthe point where she has trouble bathing and dressing independently. Although
she lives alone, her daughter brings herin formedicalvisits and acts as atranslator. The daughter has mentioned thatat
leasttwoother familymembersalso visitMrsMartinez
regu-larly. Born inMexico, MrsMartinezis a permanent United States resident with Medicare and Medi-Cal (California's Medicaid program) benefits. Should a physician discuss long-termcareoptions with thefamily?
Long-term careservices existtocompensate forlost(or neverexisting) functional capacity.IYetfewpatients or
fami-liesknowabout therangeandavailability of servicesintheir communities.2 Long-termcareisoftenerroneously equated only with nursing home care. Physicians play a key role
becauseolderpatientsandtheir familiescommonly turnto
them forinformationand assistance.3
Variousfactors influence the interestandability ofLatino
families(ofanyHispanicancestry)toseek formallong-term
care. Most of the influences can beplaced intotwo broad
categories: culturalandstructural. Wefocuson
identifying
patternsofuseof
community-based
in-homelong-term
carehealth services by Latino elders. We compare the relative importance of cultural and structural factors associated with theuseofthose services and relate those
findings
toclinical practice.Theissueofin-homecaretakesonincreased
importance
when the future demographics of Latino communities are considered. First, the number of Latinos older than 65 is
projectedto increaseby500% by the year
203O.4
This willincrease the strainonthefamily andinformalresourcesthat
currently provide care. Second, that strain will be com-poundedby thedecliningsize offamilies ofminoritygroups, furtherreducing theavailabilityofinformalcare tothe
grow-ingnumber ofaged.
Health Status and Needs ofOlder Latinos
Wetypicallydiscussthehealthofminority populations in
referenceto those withthebest health status inthe United
States, usuallynon-Latino whites. Thestatusfor older Lati-nos is mixed, however. Compared with non-Latino whites, olderLatinos have better health indicators insomeareasand worse inothers.
A commonindicatorofthe healthstatusofpopulations is
deathrates.Unfortunately, ethnicity (Latinoversus
non-La-tino)is notreported byallstatesand is oftenmissingfor some statesthat do report it. From 1979to 1981, 13 of 15 states*
thatwere hometoabout45% of the Latino
population
pro-videdusable dataon Latinodeaths. Inthose states Latinos
aged 65 and older had lower death rates than older
non-Latino whites for almost all causes,especially diseasesofthe heart (athirdlower), chronic obstructive pulmonary diseases
andallied conditions(50%
lower),
andmalignant
neoplasms (almost athirdlower).Higher
death rates occurredamong older Latinos for diabetes mellitus(twice
the non-Latinowhiterate); motorvehicle accidents(three-fourths
higher);
*Arizona,Colorado,Georgia,Hawaii,Illinois,Indiana,Kansas,Mississippi,
Ne-braska,NewYork,NorthDakota,Ohio,and Texasreporteddeathratesaccordingto
ethnicity.Califomia(which hasthelargestnumber of MexicanAmericans)and Florida (which has thelargestnumber ofCubans)didnotdifferentiate deathratesaccordingto
ethnicity.
FromtheDepartmentofCommunityHealthSciences,UniversityofCalifomia,LosAngeles,Schoolof Public Health. Presented in partatthe American Public Health Associationmeetings,Atlanta,Ga,November 1991.
This researchwassupportedbyfunds from the UCLA Academic Senate and computerresourcesprovidedbytheUCLA Office of AcademicComputing.
LONG-TERMCAREOFLATINOELDERS
ABBREVIATIONSUSED IN TEXT ADL=activities of daily living
IADL=instrumental activities ofdailyliving
nephritis, nephrotic syndrome, and nephrosis (two-thirds higher); and chronic liver disease and cirrhosis (two-thirds higher). The pattern for older Mexican Americans and PuertoRicanswassimilar,exceptthat deathratesforchronic liverdisease and cirrhosiswerehigher forPuerto Ricans and
the deathrates fordiabetes mellituswerebetween those of
Mexican Americans and non-Latino whites. The deathrates
of older Latinos average a fifth lower than those of
non-Latino whites, with the non-Latino mortality advantage greatest
amongoldermen.5More complete data for 1987-18states
including California-show similar results, with heart
dis-ease accounting for an even lower proportion of the total
number ofdeaths of older Latinos and malignant neoplasms accounting fora somewhat higher proportion.6
Morbidity patterns provide a similar variation in
inci-denceofdiseases. Formostmajordiseasesexceptdiabetes, Latinosappeartohave lowerratesofillness than non-Latino whites. Both age-adjusted and age-specific hypertension
ratesaresubstantiallylower forLatinos than for non-Latino
whites,' contributing toalower Latino prevalence of
coro-naryheartdisease and stroke.8 The overallage-adjusted
inci-dence of cancer in Latinos is also lower than that in
non-Latino whites (246versus335cases per100,000
popu-lation). Latinos have a lower incidence ofcancer of the
breast, lung, and colon-rectum. Therate isaboutthesame
forprostatecancer,and Latinos haveahigherrateof stomach
cancer.8Themostnotabledisease for which Latinosclearly haveahigher prevalence is diabetes.Self-reported diabetes is
twotothree timesmore commonamongMexicanAmericans
thanamongallwhites.The prevalenceofdiabetes increases withage,with22.7% ofMexican Americans aged 65to74 reporting diabetes9 versus 9.3% of all whites aged 65 and
older.10
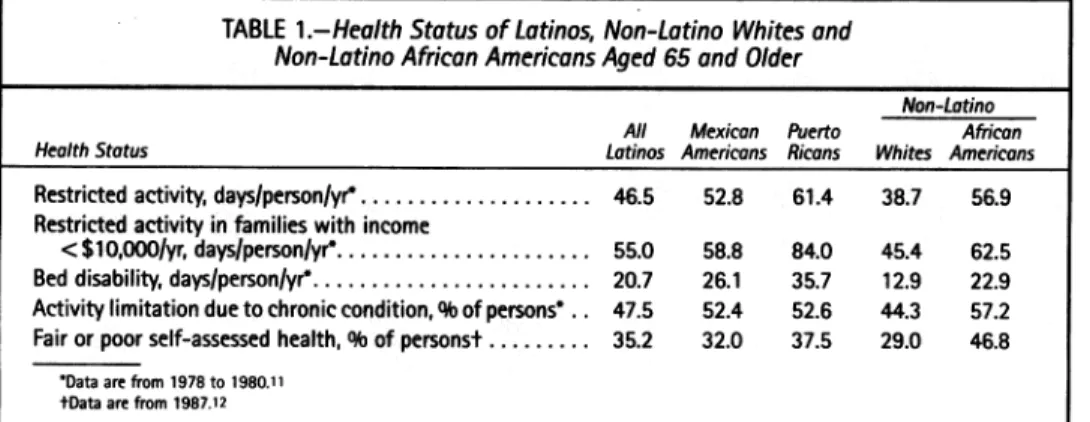
Although the death and diseasepatternsforolderLatinos
show several advantages over older whites, disability and
other health indicators are worse for older Latinos. Older
Latinosaveraged eightmoredaysofrestrictedactivityfrom
1978to 1980 than non-Latino whitesbuttenfewerdays than non-Latino blacks (Table 1). Puerto Rican elders reported
more restricted activity days than any group. Health status
declines withincome, buteven whenwelook onlyat
low-incomeelders, thepatternpersists. A more severe measure
ofdisability is the number of days that an older person is
confinedtobed
during
ayear.Thatmeasureshows that botholder PuertoRicans and Mexican Americanswere more
dis-abled than non-Latino African-American or white elders.
Therateofactivitylimitation duetochronicconditions for olderLatinoswasbetween that of older non-Latino African
Americans and whites. Themostcommonlyusedindicator of
general
healthstatusisself-assessed health. Table1showsthatmorethanathird of older Latinosreported their healthas
fairorpoor(versus goodorexcellent).This isslightly
higher
than theproportionof oldernon-Latino whites but
substan-tiallylower than theproportionofoldernon-Latino African Americans.
Our overallknowledgeofthe healthstatus ofLatino el-ders iscomplicated bydata inadequacies. In general older Latinos have better health than non-Latino whites in death
ratesandprevalences of certainlife-threateningchronic
dis-eases. The major disadvantages for older Latinos include
theirhigher prevalenceofdiabetes,theirgreateractivity
lim-itations,andtheirlowerglobal (self-assessed)healthstatus.
Because older Latinosare disadvantaged inactivity
limita-tions, examiningfactors thatinfluence theuseof
community-based
long-term
careisimportant.
Use of Health Care Services by Latino Elders
Althoughhealthstatusdataindicate the potential
impor-tanceofcommunity-basedin-home healthservices,mostof the researchonhealthcareusebyLatino elders has focused on theuse ofphysiciansand hospitals. In both areas older Latinos appear to receive similar or morecare than older
non-Latinos. Older Latinos havemore physician visits per
year than either non-Latino whites or African Americans
(Table 2).Thispatternholdsevenforthose reportingpoor or
fair health. Less variation occurs in the rates ofhospital admissions, althougholderLatinosareslightlymorelikely to use a hospital than older non-Latino whites or African
Americans.
Adifferentpatternemergeswhenwecontrolfor factors thatinfluence physician and hospitaluseamongmiddle-aged
and older Latinos. Puerto Ricans andMexican Americans
are morelikely than non-Latino whites orAfrican
Ameri-cans to see a physician as their physical activity becomes
limited,evenaftercontrolling forage, sex,healthstatus,and otherfactors. On the other hand PuertoRicans andMexican Americans are less likely tobe admitted to hospital when
theyrate their healthaspoor.13
Limited data existontheuseof long-termcareservicesby
Latino elders. Most data show that older Latinos are less
likely than either older whitesorAfricanAmericanstouse
TABLE 1.-HealthStatus ofLatinos,Non-Latino Whitesand Non-Latino AfricanAmericansAged65and Older
Non-Latino
All Mexican Puerto African HealthStatus Latinos Americans Ricans Whites Americans Restrictedactivity,
days/person/yr*
... 46.5 52.8 61.4 38.7 56.9Restricted activity in families with income
<$10,000/yr,days/person/yr*... 55.0 58.8 84.0 45.4 62.5
Beddisability,days/person/yr*... 20.7 26.1 35.7 12.9 22.9
Activity limitation duetochroniccondition,9bofpersons. . 47.5 52.4 52.6 44.3 57.2
Fairorpoorself-assessedhealth,9bofpersonst... .... 35.2 32.0 37.5 29.0 46.8
*Dataarefrom1978 to 1980.11
tDataarefrom1987.12
nursing homes,14,15evenafter other riskfactorsaretakeninto
account.16 The higher level of disability for Latinos in the communitymaybepartly because disabled Latinosremain in
thecommunity when similarly disabled whitesusenursing
homes.
In-home healthcareisviewedas analternativeto institu-tionalization, but we know little about the effects ofrace,
ethnicity, culture, and class ontheusepatterns of
commu-nity-based and informal long-termcareservices.17Older
La-tinosandnon-Hispanic whitesusepaidin-homecareinabout the sameproportions nationally, whereas older Latinos
re-ceivemoreinformalcare.'8This doesnot,however, control
forlevel ofdisability, availability of family, financialstatus,
orotherfactors that mightincreaseordecrease theneedfor formal and informalcare.
Astudy ofcase-managementclients in Arizona found that olderLatinoswerelesslikelytousecommunity-based
long-term care services than non-Latino whites despite their
greateractivitylimitations."9 The lower level of formal
sup-port received by Latino elders was balanced, however, by
higher levels of informalsupport. Greene and Monahan
cau-tionthat their datadonotindicate whetherthe familysupport
wasprovidedbecause formalsupportwasnotavailableorin
preferencetoformal services. This distinction between
ser-viceusepatternsas aresultof preferencesversusbarriers in
thestructureofthehealthcaresystemforms thecoreofthe
debateoverdifferencesin theuseofhealth servicesby
minor-ity elders.
Culture andInstitutionalStructure Influencing Health Care Use
Forces thatinfluence theuseof health services by
minor-ityelderscanbedivided intotwogeneral categories:cultural
and structural. Cultural influences include the belief
sys-tems,behaviors, and preferences ofa groupthat mightcause
certainpatternsofhealthcare use. Structural influences
in-cludethewaythehealthcaresystemand othersocial
institu-tions are organized and operated. They may present both
incentives andbarriers totheuse ofhealth services.
Culture. Cultural influences would beexpectedtoshape
theusepatternsoflong-term care,especially because
long-termcareofteninvolvesnontechnicalassistance thatcanbe
providedbyfamily members. Culturemayinfluence theuse
offamilyversuspaidcarethroughconceptsoffamily
respon-sibility and attitudes toward the useofpublic services for
those eligible for Medicaid. The strength and centrality of
familyare commonLatinovalues.'5 Apossible explanation
ofwhy Latinoeldersuse nursinghomes less often than do
non-Latinos is that Latino family roles make Latinos more
disposedthan non-Latinostomake the sacrificesnecessary tohelpolder relatives.20
Culturecanalso influence how satisfied patientsarewith their medicalcare.Healthcareprofessionals' lackof
knowl-edgeabout Latino culturalnormsandinabilityto
communi-cateinSpanishareoften citedasfactorsdiscouraging Latinos from seeking needed health care.21-23 Acculturation-an im-migrant's adoptionof attitudes andcommonbehaviors from
the dominantsociety-canaffect both familyfunctioning24 and health serviceuse.25It issurprising,therefore,that most
researchonhealthcare for Latino elders has notexpressly investigated the importance ofacculturation (others26 also
notethisdeficiency). Althoughacculturation doesnot
neces-sarily weaken Latino family functioning
overall,2"
there is evidence that acculturated families provide lower levels of informalsupport totheaged.28Thus,wemightexpectaccul-turatedLatino elderstouse moreformal services than
tradi-tional Latino elders.
Institutionalstructure. Incomeand health insuranceare
themostimportantstructuraldeterminants ofaperson's abil-ity to obtain health care. Older Latinos are
disproportion-atelypoorbecauseofthestructure ofouroccupationaland
economicsystem. Also,ourhealthcaresystemrations care
basedonabilitytopay. Almostall olderpeoplehave
insur-ance coverageforacutecare fromMedicare,but Medicare
paysless than 6% ofall long-term carecosts in the United
States.29
Giventheimportanceofincome and insurance in
deter-mining long-termcareuse,there isamajorgapinthe health
insurance statusofLatinoelders. Inthegeneralpopulation
many more Latinosareuninsured(33%)than whites(13%) orAfricanAmericans(19%).This islargelybecause Latinos
areconcentrated in industries suchaspersonal servicesand
construction that do not offer insurance and because they
disproportionately live in states-Texas and Florida-with
stringentMedicaideligibility criteria.30Asaresult, serious illness in thefamilyis consideredafinancialproblemalmost
twice asoften among Latinos asother whites (39% versus
19%).31
Retrospective Study
The following analysis reports on the use of in-home healthservices forallolder Latinos and for specific Latino
subgroups.Theiruseof services isexaminedby need,
indi-vidual characteristics, family status, acculturation, and health insurance.
Methods of Analysis
The datawerefromthe 1988 nationalsurveyofHispanics
aged65 and older sponsored by the Commonwealth Fund
Commissionon OlderPeopleLiving Alone. Telephone
in-terviews, doneprimarilyinSpanish, wereconducted of 937
MexicanAmericans, 714 CubanAmericans, 368 mainland
TABLE 2.-Use of HealthServices by Latinos, Nn-Latino Whites, and Non-Latino African AmericansAged65andOlder*
Non-Latino All Mexican Africon
Health Service Latinos Americans Whites Americons
No.ofphysicianvisits/person/yr... 8.2 9.1 6.3 6.7
No.of physician visits forthose withfairorpoorself-assessed
health/person/yr. 1.5 12.1 9.6 8.9
>1 Hospitalepisodes, %ofpersons .18.7 18.5 18.3 17.3
LONG-TERM CARE OF LATINO ELDERS
Puerto Ricans, and 280 other Hispanics.* The data were weighted to reflect US population estimates. The survey con-tractor's final report contains a complete methodologic
dis-32
cussion.
Wewereprimarily interested in explaining the previous year's use of in-home health services (home health nurse, home health aide, or homemaker). We focused on these ser-vices for two reasons. First, these serser-vices are often covered
byMedicaid, Medicare, or both, and target the most disabled
elders. Second, physicians arecentral to these services be-causephysiciancertification of need or a care plan is required
before Medicare or Medicaid will pay for them in many
situations. Evenwhen physician approval is not necessary, physicians can be an important source of referrals.
Explanatory variables include five health status indica-tors asevidence of need for in-home services: limitations in
activities of daily living (ADL)-bathing or showering,
dressing, transferring, walking, getting outside, using the
toilet; limitations in instrumental activities of daily living
*The largest nationality was Dominican (95 interviewees) followed by in decreasing frequency Spanish, Colombian, Salvadoran, Ecuadoran, Nicaraguan, and 15 other nationalities.
(IADL)-preparing own meals, managing money, using the
telephone, doing light housework,doing heavy housework; self-assessed health status; hospital admission within the past year; and frequent physicianvisits in the past year.
Demographic and social characteristics are often associ-ated withdifferences in the use of health services. We exam-ined the demographic variables of sex and age. Social level variables are subject to intervention and change. They in-cludeindicatorsoftraditional culture (acculturation),
educa-tion, social support(living alone, living withspouse,living
without spouse butwith or near children), income (poverty), and health insurance.
Two variables are frequently used to indicate levels of
acculturation: languageability21'33and agewhenthe
respon-dent arrivedon the USmainland.34 Wecreateda summary variable thatincludes both of these dimensionsand can be interpreted as the extent of acculturation of the respondent in
comparisontotheaveragelevelofacculturation (low)ofall
older Latinos.
Results
Needs and resources of Latino elders. The need for in-homehealthservices forolder Latinosappears tobe
substan-TABLE3.-Characteristics ofLatinos Aged 65and OlderbySubgroup'
All
Latino Mexican Puerto x2
Elders,t American, Cuban, Rican, Statistical
Charocteristic 4l 9b 4b * Significonce
Health
1 or moreADL difficulty ...
1 or moreIADLdifficulty...
Self-assessed health-fairorpoor...
Hospitalusepastyear...
Physicianuse > 12times pastyear...
Demographic
Women... Aged65-74yr...
Social
Immigratedatage55orolder...
Immigratedatage31-54 ...
Immigratedatage17-30 ...
Immigratedatage0-16...
Born in USlmainland ...
NoEnglish (monolingual Spanish)... Poor English§... Speaks English well...
<5yrschool...
6-11 yrschool...
Highschoolgraduateandup...
Livesalone... Lives withspouse...
Withoutspouse,lives withchildrenor
within 30min ... Family income Above poverty... Belowpoverty... Unknownorrefused... CoveredbyMedicare ... CoveredbyMedicaid...
ADL activities ofdaily living,IADL instrumental activities ofdaily
WeightedtoreflectUnitedStatespopulation estimates for oldi tlncludes "otherHispanics:'notpresented separately. *Significanceofx2comparisons amongthreesubgroupsisgiver
§Primary languageisSpanishandreportsfairorpoorEnglishat
39.1 39.6 32.0 44.6 .005 53.4 54.5 44.8 54.3 .005 53.3 57.0 46.7 62.7 .000 22.1 20.7 21.5 31.8 .001 23.9 20.5 28.8 36.7 .000 55.9 53.2 61.7 55.8 .019 62.1 62.3 54.7 69.5 .001 16.0 6.2 41.4 13.1 .000 21.2 10.6 49.8 40.4 12.1 12.4 5.3 34.2 12.4 17.9 3.0 12.3 38.4 52.9 0.5 0.0 39.4 33.8 57.3 37.4 .000 32.5 37.4 30.6 37.3 28.1 28.7 12.1 25.3 42.5 54.3 17.1 41.5 .000 38.7 33.8 49.1 45.1 18.7 12.0 33.8 13.4 22.4 22.3 23.1 26.2 >.05 48.7 50.0 44.6 46.5 >.05 36.6 38.1 33.5 35.6 >.05 31.9 29.8 37.6 30.5 .005 42.2 45.1 35.8 41.8 25.9 25.1 26.6 27.7 79.9 79.6 87.3 79.8 .007 42.2 39.0 52.8 50.7 .000 y living erLatinos. 340
tial but varies among the groups. In general older Puerto Ricans have the highestlevels ofneed,followed by Mexican
Americans and Cubans. Morethanathirdofall older
Lati-noshad one or moredifficulties inADLs, morethan half had
one or moredifficulties in IADLs, and more than half re-ported fair or poor health(Table 3). Morethantwofifths of all older Latinos hadahospitaladmission, andmorethantwo
fifthssaw aphysicianatleast 12 timesduring thepast year.
OlderPuertoRicans hadthe highestuseof medical services. The highADLand IADLdependencies, thelow self-assess-mentof health,andthecommon useof physician and hospital carereinforce the data presented earliershowingahigh need by Latino elders forcommunity-based long-termcare.
The olderLatino population includes more women than men,with most elders in the "young elderly" range (ages 65 to 74). The Cuban population had even more women and wereolder, reflectingtheir different history of migration to
theUnited States.35
Some social characteristics (Table 3) are liabilities for
those needing supportive services, including recent
immi-gration, limited English, low education, and poverty. Only
half of the Mexican-Americanelders and almost no Cuban or
Puerto Ricanelders reported being born in the United States. Asizable proportion, especially Cubans, immigrated at age
55andolder.Almost40%ofolder Latinosreportedspeaking
noEnglish, eventhough morethana quarter reported good
Englishskills. Almost half oftheolder Latinos had less than
aprimary schooleducation. Athird of olderCubans, how-ever,werehigh school graduates.Povertyisa common
prob-lem that ismost acuteamong Mexican-American elders. Resources fordisabled Latino elderspotentially include
health insurance and theavailability of family. Most older
Latinos live witha spouse orwithouta spouse but with or near (within 30 minutes of) their children. The living ar-rangementis theonlycharacteristicwhere there are no
statis-tically significant differences between the Latino subgroups. Althoughmostolder Latinos haveMedicare, the proportion
withoutcoverageis twice the nationalaverage.32On the other
hand older Latinos have high rates of Medicaid coverage,
partlyas aresultoftheirhighpoverty rates.
Mexican-Ameri-can elders, however, have the highest poverty rate and the
lowest Medicaid rate.
Characteristics of eachgroupreflect its immigrationand
occupational history. Older Mexican Americans are most
likelyto have been born in the United States but have had
limited occupational opportunities and have faced housing
discrimination.35 Among thisgroup, for example, 21%
re-ported farm work as their primary lifetime occupation.32 Thishistory explainswhyolderMexican Americans have the lowest educational levels, only average English abilities,
above-average
povertyrates, andincomplete Medicare cov-erage(Table 3).Inaddition,someolderMexican
Americans avoidgovernmentprograms, suchasMedicaid,and servicesbecausetheyareundocumented residents. In the1986
immi-gration legalization program,
1%
of Mexican immigrantsapplyingtoregularize theirstatus wereaged65orolder.36In contrast, olderCubans include manyprofessionals who
im-migratedasadults afterthe end of theCuban revolution in
1959.3' Consequently, Cuban elders have the most educa-tion, the least English ability,andoldestagesatthe timeof immigration. They can receive Medicaid because oftheir
special refugee status.38 Puerto Ricans are like Mexican Americansinmostsocialcharacteristics, althoughnoPuerto
Ricanelder in this survey was born on themainland. Puerto Ricans, however, are all US citizens as a function of the
commonwealthstatusofPuertoRico and thereforeneverface immigration status barriers to the receipt ofMedicaid.
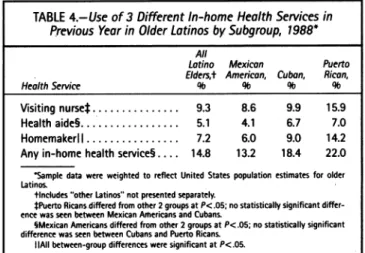
Useofservices.Given thehighlevels ofdisabilityamong the Latinoelders,weexpectedtofindhigh levels of service use. Table4shows thehighuseofcommunityservices,with somedifferences by subgroup.Visitingnurses werethemost commonly used in-home healthservice, followedby
home-makers andthen home health aides. Thehigheruseof most
in-home health services byolderPuertoRicans mirrors their higher levelsofdisability andpoorerhealth.
Mexican-Amer-ican eldersuse in-home health services less than Cuban
el-dersintwoof thethreeservices, but thislowerusedoesnot
reflectanyhealth status differences. It isimportant tonote
that each population is concentrated in different areas:
Puerto Ricans in New York City, Cubans in Florida, and Mexican Americans in the Southwest. Some of the
differ-encesinuse mayhave resulted from differences in the
avail-abilityofservicesinthe different areas.
Correlations show therelationshipsbetween theuseof
in-home healthservices and theneeds, individual characteris-tics, and social characteristics of each subgroup of Latino elders(Table 5). For correlations thatarestatistically
signifi-cant, we need to compare the size of the correlations to
determine the practical relevance. In particular, the
cor-relationsshow therelatively high importance of need factors
and Medicaidand therelatively lowimportanceof cultural factors.
Theneed indicators of ADL and IADLdisabilityhave the
largestcorrelations with theuseof in-home healthcare
(Ta-ble 5). Medical care use-hospital and frequent physician
care-has smaller butimportantcorrelations withtheuseof
in-home healthcare. Theonlyother correlations similarin
magnitude to theneed indicators are advanced ageand
re-ceiptofMedicaid. Smaller correlationsinclude thenegative relationship-decreases the chance of service
receipt-be-tweenlivingwithaspouseandin-home health services. For
Mexican-American and Puerto Rican elders, living alone
increases the chance that serviceswill be used.
Aswewouldexpect, ADLs, IADLs,andbeingadmitted
to a hospitalare each predictors of in-home health service
use. Part of the role ofvisiting nurses, homemakers, and
home health aides istoassist the disabledelderlywith ADLs
and IADLsorotherneeds thoseimpairmentsmightcreate.
TABLE4.-Use of 3 Different In-home Health Services in Previous Year in Older LatinosbySubgroup, 1988*
All
Lotino Mexican Puerto Elders,t Americon, Cubon, Rican,
HealthService 0lb 9l 0b 9lb
Visitingnursel... 9.3 8.6 9.9 15.9
Healthaide§... 5.1 4.1 6.7 7.0
Homemakerl ... .... 7.2 6.0 9.0 14.2
Anyin-homehealthservice§.... 14.8 13.2 18.4 22.0
Sampledata wereweightedtoreflect United Statespopulationestimates for older Latinos.
tincludes "otherLatinos"notpresented separately.
tPuertoRicansdifferedfrom other2groupsatP<.05;nostatistically significant
differ-ence was seenbetween MexicanAifericansandCubans.
SMexican Americansdiffered from other2groupsatP<.05;nostatistically significant differencewas seenbetween Cubans and Puerto Ricans.
Similarly, the pushtodischargethe elders fromhospitals as early as possible has moved some of the care formerly
pro-videdin the hospital into the home, increasing the need for
posthospitalnursing and other care.39 Further analysis, not
presented here, foundthatself-assessed health and physician visits did not predict the use of in-home health services after
controlling for other variables.40 Bothaglobal assessment of
healthas poor andfrequent physician visits can be the result
ofavariety of health conditionsnotrelated to a disability that requires long-term care. Consequently, older Latinos who use in-home care are more likely than non-in-home care users to see aphysician (the correlation), but physicianuse
itself doesnotincrease the use of in-home health services.
Mexican-American and Cuban men are somewhat less
likelytousein-home health services thanwomen (Table 5)
becausetheyaregenerallyyoungerthan thewomenand more
likelytobelivingwith a spouse. Gender by itself does not
influence theuse ofin-home health services.40 Frail older
TABLE
W-;tro
bh ealt5i~Os
by
AD',
Iy:.;:_mom)e L...:2uu8 .3
lAi. I( ormore.).27 .25 .33 .33 1 -fai -rpor,
60-eceto
rgood ....17 .18 .18 .12Hos0pita
admission ps y 0-nio,1-Yes .28 .25 .26 .23*-12
y... 13 .11 .11 .23 Sex-0female f male. -.08 -.11 -.12 .09t Age, r0-i65-7441 75.7 .23 .24 .24 .24 Accultuaion.V...C.-.04. -.01± -.05± -.10± Educatlion- <6 yr 6Allyr,12yrandup . -.05 -.03± --.06± -~.18Liv aWene-O-no, I-yes. 12A .17 .02± .15
Liewt
puse--0=o,1-yf-es... ~-.11 --.09 --.13 --.15
Live witout spouse and
0-no yes.0.±...17 .02± .02±
FmilpvryQ-o1ys .09 .10 .01± .19
§Mdicare-.0 0-n =yes.fI ** 09 .-.07± .00 .16
:edaid-Q-no,1=y1es ...20 .17 .19 .17
M)-clisof dail living,IADL=~instumntlactvitesofdailiving Smpl dataiewited withthenl00o08ied
tAli 0ltnarevigniflcantat.t:000 P<05e.n.tstatistical2etOsew which ar y
;significant - 7. 23 24 .4 2
Latinos (age 75 andolder) are morelikelyto usein-home
services independent of need and social factors.40Agemay
increase the number and severity of disabilities (we only
measured theirpresence) or weaken informal support(for
instance,anagingspouse may nolonger bephysically ableto
provide thesamelevel of assistance), orboth.
Asweexpected, wealsofound correlations between
in-homehealthcare useandsomeof the socialresources.
Liv-ing alone, which indicatesalower level ofavailablesupport,
increases the chance ofusing in-home health services for
mostsubgroups.Accessibilitytofamily help,asindicatedby
living with a spouse, reduces the use of in-home services.
When other variables arecontrolled, living without a spouse but with or near childrenalso reduces the use of in-home healthservices.40 What the data do not show is the causal order-whether family is used in preference to formal
ser-vicesorbecause formal servicesareunknown orunavailable.
Latinoelders with Medicaidcoverage are morelikely to use services,* demonstrating the importance of financial barri-ers to in-home service use. Medicaidcan pay for in-home
health services, reducing the financial burden for low-in-comeLatino elders.
The small and not statistically significant correlations
withsome variables are asimportantasthe larger correla-tionsjust described. Inparticular, acculturationhas an
unex-pectedlysmall or notsignificant correlation withthe use of
in-home health services (Table 5). Similarly, despitethe
em-phasisonfamily in Latino culture, the accessibility of
chil-dren for those living without a spouse had no statistically significant correlation with the use of in-home health
ser-vices. Acculturation, whichwasmeasuredby knowledge of English and age atimmigration, hadnorelevant correlation within-home health serviceuse. Evenwhencontrolling for othervariables, acculturation remainednotsignificant.
Sim-ilarly, graduation from high school hadnoindependent effect
on the use of in-home services.40 The lack of any overall
acculturation effectsupportsthe conclusion thatfamily sup-portisnotprimarily aresult ofastrongculturalpreference for family help. Cuban elders had few significant correla-tions of socialcharacteristics with serviceuse.
Aftercontrolling for all the other variables,PuertoRican eldersarestill twiceaslikelyto usein-homehealthservices
astheother Latinogroups.40 This is possibly because older
PuertoRicanscommonlylive in New YorkCity, which hasa
relatively well-developednetworkof in-home services com-pared with otherparts of the country (V. Levy, New York
City Department for the
Aging,
oralcommunication,
No-vember 1991). Similarly, Mexican-American elders may
have lower in-home health serviceusebecausesomelivein
nonurbanareasandin states where fewer services exist.
Summary
Latinoelderscompriseadiversesetofsubgroups.t Our data showthat allsubgroupsfrequently have functional
limi-tationsand low health status, with PuertoRicanshaving the
worsthealth. Acculturation has littleor noeffectontheuseof in-home healthservicesfor anysubgroup, whereas structural factorssuchashealth insurance andthe localavailability of services have a moderate effect on all subgroups. These structural factors are the most likely reasonthat
Mexican-American elders use in-home health services less than the othersubgroups.
StructureorCulture-WhatDoesIt Matter?
Inanidealhealthcaresystem,theuseofservices would
bedeterminedonly byneed andpersonal preferences. Our datashowthat needfactorsareamongthe strongest predic-tors oftheuse of in-homehealth services. Weconsistently
*The increased chance of usebythose in poverty ismostlycausedbythose in povertybeingmorelikelytohaveMedicaid,tolivealone,and tohave ADL or IADL
limitations,each of whichindependentlyincreases the use of in-home health services.
tTherewere notenoughCentral Americans in thesampletoform any
generaliza-tions,butthoselivinginthe Southwestprobablyhave many characteristics similar to Mexican-American elders: asignificantproportion willbe undocumentedresidents,
and mostwill have lowincomes,lowMedicaid coverage, and low in-home health service use. Few will have been bom in the United States.41
found,
however,
that health insurance status andliving
ar-rangements alsoinfluence theuseof in-homehealth services.
Ifwe are to ensure that Latino elders receive appropriate
health
services,
we need tounderstand the extent to whichstructural andcultural forces arealsoinvolved intheuseof services.
The
importance
ofliving arrangements-especially
after otherfactors aretaken into account-could bedescribed asthe result ofacultural
preference
forfamily help
inplace
of formal assistance. Acculturation has nosignificant
effect,however,
which contradicts theinterpretation
that relianceonfamily
inplace
offormal in-home health services isasimple
cultural
preference.
Themorelikely explanation
isthat fami-lies coulduseandbenefit from theextrahelp provided by
in-home health care,regardless
of their cultural orientation. Latinoelders,
theirfamilies,
and all otherelders, however,
generally
havealowawarenessoftheexistence and purpose of in-home health services.2"3 Their low-incomeback-grounds
make them lesslikely
to think that paid help is feasible.A moderate use of
physician
services did notindepen-dently
increase older Latinos' use ofin-home healthser-vices,
despite
the fact that thephysicians
are the mostcommon sourceof information about
long-term
care inthegeneral population.3
Ifmostphysicians
assessedthe disabili-ties of the older Latinopatients they
see often and made referralstoin-home health services when indicatedby need,wewould expectto see
physician
visitsindependently
associ-ated with increased serviceuse.One reason
physician
visits may not increase in-home health servicesuseisthat manyphysicians
mayobserve thefamily providing
in-home assistance and assumethat such assistance isprovided
for cultural reasons. It is possible,however,
that thefamily
assistance isprovided
because the elder and thefamily
are notaware ofthe range ofoptions
availableoraredeterred
by
thecomplexity
of thelong-term
caresystem and itsfinancing.
Families may also think that because caregiving
has not yet become acrisis,
it is notappropriate
toask for additionalhelp.
ForLatino elders who have Medicaid and therefore access to a case manager, it would behelpful
forphysicians
to assessthefunctionaldis-ability
level oftheirpatients
andcounsel their disabled older Latinopatients
about the range ofcommunity
services availa-ble tosupplement
the carethey
mayalready
be receiving from theirfamilies. Researchonthegeneral
olderpopulation finds that formalservicescomplement
rather thanreplace
the efforts offamily.42
Older Latinos often holdexpectations
of assistance from theirfamilies,2"
43butthoseexpectations
donotmeanthat formal services wouldnot
improve
thestatusofthe eldersandtheircare
givers
orthatin-home health carewould be refused if offered.
For Mrs Martinez
(opening
paragraph),
thephysician
should discuss the
availability
ofMedicaid and otherhome-makerservicesas an
option
forproviding
someofthebasiccarethat she needs.Ahomemaker could
help
MrsMartinez get up,bathe,
anddressinthemorning,
thereby allowing
thefamily
tocontinueproviding
otherADL, IADL,
andemo-tional support. Because the
steadily deteriorating
nature of Mrs Martinez'sdementia willplace increasing
demandsonher
family
supportsystem,the formal assistancemight help
preventthefamilysupportfrombecoming prematurely
over-whelmed.
Weshouldalsonot
ignore
theroleofculture in thecareofLatinoelders. Attention to cultural values such as respect,
the involvement of family members inhealth decisions, and
use of the Spanish language have beenshown to beimportant
aspects of thequalityof care forLatinos.21'44'45 Attentionto
culture should notdiverthealth careprofessionals from en-suring that older Latinos have theopportunity toreceive in-home health services when their physical conditionmerits it.
For Mexican-American elders especially, who facethe most
structural barriers tothe receipt ofcare, physicians should
make an effort to ensure access to needed visiting nurse, home health aide, and homemaker services.
REFERENCES
1. KaneRA, Kane RL: Long-TermCare:Principles,Programs, and Policies. New York, NY, Springer, 1987
2. Holmes D, Teresa J, Holmes M: Differences among black, Hispanic, andwhite people in knowledge about long-term care services. Health Care Financ Rev 1983;
5:51-67
3. Local Information on Long-Term Care: Consumers' and Providers' Points of
View. Washington,DC, Health Advocacy Services Section, American Association of RetiredPersons, 1991
4. US Senate Special Committee on Aging: Aging America: Trends and Projec-tions.Washington DC,GovernmentPrinting Office, 1989
5. Mauren JD, Rosenberg HM, Keemer JB: Deaths of Hispanic origin, 15 report-ing states, 1979-1981. VitalHealth Stat[201 1990; (18):1-73
6. National Centerfor Health Statistics: Advance report of finalmortality statis-tics, 1987. MonthlyVital Stat Rep 1989; 38(5 suppl)
7. Pappas G, Gergen PJ, Carroll M: Hypertension prevalence and the status of awareness, treatment,and control in theHispanic HealthandNutrition Examination Survey(HHANES) 1982-1984. Am J Public Health 1991; 80:1431-1436
8. Report of the Secretary's Task Force on Black andMinorityHealth.Washington,
DC, US Dept of Health and HumanServices (DHHS), 1985
9. Perez-Stable EJ, McMillen MM, Harris MI, et al: Self-reported diabetes in Mexican-Americans: HHANES 1982-1984. Am J Public Health 1989; 79:770-772
10. Ries PW: Health of black and white Americans, 1985-1987.Vital Health Stat
[1011990; (171):1-114
11. Trevino FM, MossAJ:Healthindicators for Hispanic, black, and white Amer-icans.Vital Health Stat [101 1984; (148):1-88
12. RiesPW:Americans assess their health: United States, 1987. Vital Health Stat [10] 1990;(174):1-63
13. Wolinsky FD, Benigno EA, Fann U, et al: Ethnic differences in the demand for physician and hospitalutilization among older adults in major cities: Conspicuous evidence of considerable inequalities. Milbank Q 1990; 67:412-449
14. Sirrocco A: Nursing home characteristics: 1986 Inventory of long-term care places.Vital Health Stat [14] 1989; (33):1-32
15. Wallace SP, Facio EL: Moving beyond familism: Potential contributions of gerontologicaltheory to studies of Chicano/Latino aging. J Aging Stud 1987; 1:333-354
16. Greene VL, OndrichJI: Risk factors for nursing home admissions and exits: A discrete-time hazard function approach. J Gerontol Soc Sci 1990; 45:S250-258
17. Antonucci TC, Cantor MH:Strengtheningthe family support system for older minoritypersons,InJackson JS (Ed): Minority Elderly: Longevity, Economics, and Health.Washington, DC, Gerontological Society of America, 1991, pp 32-37
18. Hing E: Long-Term Care Use By Black and White Elderly. Presented at the annual meeting of the American Public Health Association, New York City, October 1990
19. Greene VL, Monahan DJ:Comparative utilizationof community based long term care services by Hispanic and Anglo elderly in a case management system. J Gerontol 1984;39:730-735
20. Morrison BJ: Sociocultural dimensions: Nursing homes and the minority aged, In Getzel GS, Mellor MJ (Eds): Gerontological Social Work Practice in Long-term Care. New York, NY, Haworth Press, 1983, pp127-145
21. Valle R, Mondoza L: The Elder Latino. San Diego,Calif,Campanile Press, 1978
22. Lacayo CG: A National Study to Assess the Service Needs of the Hispanic Elderly. Los Angeles,Calif,Asociacion Nacional Pro Personas Mayores, 1980
23. Berkowitz SG: Assessing the Unmet Service Needs of Elderly Homebound Blacks, Hispanics, and Vietnamese in Arlington: Recommendations for Improving Delivery and Overcoming Barriers to Utilization, FinalReport. Washington, DC, Gerontological Society of America Technical Assistance Program, 1989
24. Becerra RM: The Mexican-American-Aging in a changing culture, In McNeely RL, Colen JN(Eds): Aging in Minority Groups. Beverly Hills,Calif,Sage, 1983, pp108-1 18
25. Wells KB, Golding JM, Hough RL,BumamMA, Karno M: Acculturation and the probability of use of health services by Mexican Americans. Health Serv Res 1989; 24:237-257
26. HarelZ, McKinney EA, Williams M: Aging, ethnicity and services: Empirical and theoretical perspectives,InGelfand DE, Barresi CM (Eds): Ethnic Dimensions of Aging. New York, NY,Springer, 1987, pp 196-2 10
27. Keefe SE, Padilla AM:Chicano Ethnicity. Albuquerque, NM, University of New MexicoPress, 1987
28. Lubben JE, Becerra RM: Social support among black, Mexican, and Chinese elderly, In Gelfand DE, Barresi CM (Eds): Ethnic Dimensions of Aging. New York, NY,Springer, 1987, pp 130-144
LONG-TERM CARE OFLATINOELDERS
29. Policy Choices for Long-term Care. Washington, DC, US Congressional Bud-getOffice, 1991
30. HispanicAccess toHealth Care:SignificantGaps Exist. Testimony before the HouseSelect Committee onAging and theCongressional HispanicCaucus, publica-tion GAO/T-PEMD-91-13.Washington, DC, General Accounting Office, 1991
31. Anderson RM, Giachello AL, Aday LA: AccessofHispanics to health care and cutsin services: A state-of-the-art review. Public HealthRep1986; 101:238-252
32. A Survey of Elderly Hispanics, Final Report-Conducted for the Common-wealth Fund Commission on Elderly People Living Alone. Rockville,Md, Westat,
1989
33. Cuellar 1, Harris LC, Jasso R: An acculturation scale for Mexican American normaland clinicalpopulations. Hispanic J Behav Sci1980;2:199-217
34. Zuniga-Martines M: Los Ancianos: A Study of the Attitudes of Mexican AmericansRegarding Support for the Elderly(Dissertation). Waltham, Mass, Bran-deisUniversity, 1980
35. Portes A, Bach R: Latin Journey. Berkeley,Calif, Universityof California Press, 1986
36. US Immigration and Naturalization Service: ProvisionalLegalization
Applica-tionStatistics, Dec1,1991.Washington, DC, StatisticsDivision,Office of Plans and Analyses, 1991
37. Queralt M: The elderly of Cuban origin, In McNeely RL, Colen JN (Eds): Aging in MinorityGroups. Beverly Hills, Calif, Sage, 1983, pp 50-65
38. Pedraza-BaileyS: Political and Economic Migrants in America: Cubans and Mexicans. Austin, Tex, University of TexasPress, 1985
39. Morrisey MA, Sloan FA, Valvona J: Shifting Medicare patients out of the hospital. Health Aff (Millwood) 1988; 7:52-64
40. WallaceSP, Lew-Ting CY: Formal Service Use and Family Support of Latino Elderly. Presented at the annual meeting of the American Public Health Association, Atlanta, Ga, October 1991
41. Wallace SP: The new urban Latinos: Central Americans in a Mexican immi-grantenvironment. Urban AffQ 1989; 25:239-264
42. Noelker LS, Poulshock SW: TheEffects on Families of Caring for Impaired Elderly in Residence. Washington, DC, US DHHS, Administration on Aging, 1982
43. MarkidesKS, Martin HW, Gomez E: Older Mexican Americans. Austin, Tex, University of Texas Press, 1983
44. Cuellar JB:Hispanic Americanaging: Geriatric education curriculum devel-opmentfor selectedhealth professionals, In Harper MS (Ed): Minority Aging. Wash-ington, DC, US DHHS, Health ResourcesAdministration,1990, pp 365-413
45. ApplewhiteSR,Daley JM: Cross-cultural understanding for social work prac-tice with the elderly, chap 1, InApplewhite SR (Ed): Hispanic Elderly in Transition. New York, NY, Greenwood Press, 1988, pp 3-16
* * *
IN
APRIL, HEARING THE NEWS
it's beforebeing
ahostageto
lossanddying numbsandeach
word ischarged
andwhen my mother tells me I'mso
prettyasI see
her sit down
inSearslooking lost then looks
upatme and
waves asshe does
from the other
twin bed whenI can'ttellsince
she often sleeps with hereyes open ifshe's sleepingand I wasn'tdrained fromstaying 11 weeks in ahouse that's acageis fullof cages as mysister tries to jail everything
thatshouldbreathe
before thenight
mare ofliving inahouse in
enemyterritory wastheprice
forhaving
her still
LYN LIFSHIN©)
Niskayuna,NewYork 344