Open Access
Research article
Use of the emergency department for less-urgent care among type 2 diabetics under a disease management program
Shang-Jyh Chiou*
†1, Claudia Campbell
†2, Ronald Horswell
4, Leann Myers
3and Richard Culbertson
2Address: 1Department of Health Care Administration, College of Health Science, Asia University, 500, Lioufeng Road, Wufeng, Taichung County 41354, Taiwan, 2Department of Health Systems Management, Tulane University School of Public Health and Tropical Medicine, 1440 Canal Street, Suite 1900, New Orleans, LA 70112, USA, 3Department of Biostatistics, Tulane University School of Public Health and Tropical Medicine, 1440 Canal Street, Suite 2000, New Orleans, LA 70112, USA and 4Louisiana State University Health Sciences Center, Health Care Services Division, P.O. Box 91308, Baton Rouge, LA 70821, USA
Email: Shang-Jyh Chiou* - chiouatg2@gmail.com; Claudia Campbell - ccampbel@tulane.edu; Ronald Horswell - RHorsw@lsuhsc.edu;
Leann Myers - myersl@tulane.edu; Richard Culbertson - rculber@tulane.edu
* Corresponding author †Equal contributors
Abstract
Background: This study analyzed the likelihood of less-urgent emergency department (ED) visits among type 2 diabetic patients receiving care under a diabetes disease management (DM) program offered by the Louisiana State University Health Care Services Division (LSU HCSD).
Methods: All ED and outpatient clinic visits made by 6,412 type 2 diabetic patients from 1999 to 2006 were extracted from the LSU HCSD Disease Management (DM) Evaluation Database. Patient ED visits were classified as either urgent or less-urgent, and the likelihood of a less-urgent ED visit was compared with outpatient clinic visits using the Generalized Estimating Equation methodology for binary response to time-dependent variables.
Results: Patients who adhered to regular clinic visit schedules dictated by the DM program were less likely to use the ED for less urgent care with odds ratio of 0.1585. Insured patients had 1.13 to 1.70 greater odds of a less-urgent ED visit than those who were uninsured. Patients with better-managed glycated hemoglobin (A1c or HbA1c) levels were 82 times less likely to use less-urgent ED visits. Furthermore, being older, Caucasian, or a longer participant in the DM program had a modestly lower likelihood of less- urgent ED visits. The patient's Charlson Comorbidity Index (CCI), gender, prior hospitalization, and the admitting facility showed no effect.
Conclusion: Patients adhering to the DM visit guidelines were less likely to use the ED for less-urgent problems. Maintaining normal A1c levels for their diabetes also has the positive impact to reduce less- urgent ED usages. It suggests that successful DM programs may reduce inappropriate ED use. In contrast to expectations, uninsured patients were less likely to use the ED for less-urgent care. Patients in the DM program with Medicaid coverage were 1.3 times more likely to seek care in the ED for non-emergencies while commercially insured patients were nearly 1.7 times more likely to do so. Further research to understand inappropriate ED use among insured patients is needed. We suggest providing visit reminders, a call centre, or case managers to reduce the likelihood of less-urgent ED visit use among DM patients. By reducing the likelihood of unnecessary ED visits, successful DM programs can improve patient care.
Published: 7 December 2009
BMC Health Services Research 2009, 9:223 doi:10.1186/1472-6963-9-223
Received: 13 January 2009 Accepted: 7 December 2009
This article is available from: http://www.biomedcentral.com/1472-6963/9/223
© 2009 Chiou et al; licensee BioMed Central Ltd.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background
According to the Centres for Disease Control and Preven- tion (CDC) [1], chronic diseases such as diabetes, cardio- vascular disease, asthma and cancer are the most common and costly health problems in America with an annual cost totalling $174 billion in 2007 [2]. Chronic diseases have been the leading causes of death and disability in the United States for the past decade. In 2005, diabetes was the sixth most common disease in the U.S., and over 14.6 million Americans suffered from diabetes and diabetes- related comorbidities, such as hypertension, stroke or infections of the kidney. However, studies have concluded that type 2 diabetes is preventable, and patients with the disease can have a higher quality of life without suffering the chronic situation of high health care expenditures, if they follow their physician's advice on diet, medicines, and lifestyle behaviours [3-5]. Disease management (DM) is a systematic approach to identify the population at risk for specific diseases, especially chronic diseases, and to intervene with a program of care. Many studies have con- firmed that DM can improve the quality of life or out- comes of treatment, ensure patient satisfaction and control costs [6] by empowering patients through educa- tion to better manage their own illness.
Diabetes is prevalent in Louisiana, and management of the disease is challenging due to large low-income populations who may not follow guidelines strictly [7]. According to most studies, patients with type 2 diabetes receive better quality of care from primary care providers than those who seek services in ED. The Health Care Services Division (HSCD) of Louisiana State University is a key provider of care to the uninsured and Medicaid populations in Louisi- ana. LSU HCSD has implemented a comprehensive, evi- dence-based, diabetes disease management program to continuously improve diabetic care processes. In the diabe- tes management program, the components include evi- dence-based guidelines for physicians and establishment of actionable patient goals with education, medication and clinical support to improve patients' diabetes situations.
When diabetic patients choose the ED for their care, not only do they pay more with no guarantee of appropriate quality services (especially in non-urgent situations) [8- 11], but also the health system consumes more resources.
From the perspective of disease management, patients with less-urgent conditions in the ED can seek primary care instead. The primary objective of this study is to examine the likelihood that patients who are adhering to the DM program's clinic visit schedules will use the ED for less-urgent problems and conditions.
Methods
Population and setting
The primary data source is the Health Care Services Divi- sion Disease Management Evaluation Database (DMED),
created to monitor patients enrolled in several initiatives of LSU HCSD's disease management programs. The study population was extracted from all 89,567 LSU HCSD dia- betes patients with a diagnosis code ICD-9: 250.xx seen in one of the HCSD's eight hospital EDs between 1998 and 2006. After excluding patients with type 1 and other types of diabetics, patients with only one visit, prisoners, and some cases with obvious errors, the resulting data set con- tained 30,097 type 2 diabetic (ICD-9: 250.x0 and 250.x2) patients with two or more visits in the study period.
Type 2 diabetes patients (n = 30,097) consisted of three groups: the 6.5% of patients who used only emergency department services; the 8.8% who used only the LSU HSCD DM clinics; and 84.6% of patients (n = 25,475) who used both the DM clinics and the ED sites of care. We kept only the last group of patients for this study. Within the study group, we eliminated an additional 10,176 patients who received some type of care in 1998 because we did not know when their DM treatment was initiated.
Only the 8,596 patients whose first records appeared in 1999 were retained for the study.
The 8,596 patients in the study group had a total of 220,719 clinic visits and 60,189 ED visits between 1999 and 2006. The ED visits were classified as urgent and less- urgent, based on the ICD-9 codes and review by two nurses who both agreed on the less-urgent ED classifica- tion (n = 28,5440) for the visit. Patient ED visits that occurred before the patient's first diabetes-related visit (chief complaint diagnosis codes, ICD-9: 250 to 250.93) were not counted, as well as ED visits that occurred on weekends because the clinics were not open. We kept only data from 6,412 patients who were 45 years and older.
The resultant data set contained 119,695 outpatient clinic visits and 16,249 less-urgent ED visits after the first diabe- tes-related visit occurring on weekdays. This study was approved by Tulane University's Institutional Review Board (IRB#C0344).
Measures
After removing all urgent ED visits, type 2 diabetic patient visits were classified as less-urgent ED (Y = 1) or clinic vis- its (Y = 0). Ten independent variables were used in the analyses based on other studies [12,13] including patient age, health plan, duration in the DM program, and facility size where services were received. For the analysis, facili- ties were classified as large versus small size based on the facility beds (over 100 or below 100 beds). Other varia- bles included the Charlson Comorbidity Index (CCI); a normal A1c rate over the past 12 months based on labo- ratory test results (normal A1c rate); 12 month adherence to clinic schedules (adherence rate); and the experience of a prior year hospitalization.
Patients with a range of comorbid conditions had each condition assigned a score from 1, 2, 3 and 6 based on Charlson's study [14]. A higher final score means more or more severe comorbidities. We then summed each patient's scores and assigned a total score to represent his/
her comorbid conditions as CCI. The observed A1c test results were grouped into three levels (<7% normal, 7-9%
borderline and > = 9% high) to calculate the index of nor- mal A1c rate. (= Σ normal level/(Σ normal level + Σ bor- derline level + Σ high level) in past 12 months).
Adherence to annual patient diabetes-related clinic visit schedules was based on American Diabetes Association suggestions [15], which were separated into three levels of adherence: none (1 point), midpoint (2 points), and high (3 points). For instance, patients who had no diabetes- related clinic visits within the past 12 months got 1 point;
patients with 1 or 2 visits, and where the time between the first and second visit was less than 6 months got 2 points;
patients with at least 2 visits, where one of the visit periods was longer than 6 months, received 3 points.
Data Analysis
This study is a longitudinal, retrospective analysis of clinic and less-urgent ED visits from 1999 to 2006. Generalized Estimating Equation (GEE) regression methods for binary responses are appropriate to analyze longitudinal data, especially models with time-dependent variables and repeated measures on the same case. GEE methodology examines the relationship between the occurrence of less- urgent ED visits as compared with clinic visits based on a number of predisposing and enabling factors. The GEE regression model for binary responses identifies those fac- tors that can be altered to reduce the unnecessary use of the ED by diabetic patients participating in the LSU HCSD diabetes disease management program. First, we analyzed the relationship between the outcome and each single unadjusted effect. Then, we computed a full model with all predictors to assess the adjusted variables. All analyses were conducted using SAS 9.12 (SAS Institute, Cary, NC).
Results
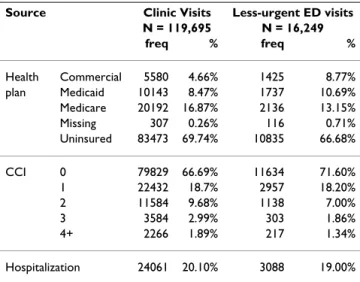
Table 1 and 2 display the descriptive statistics associated with each type of visit. Since the LSU HCSD provides care to uninsured citizens of Louisiana, uninsured patients make up the majority of both less-urgent ED visits and clinic visits, at 69.74% and 66.68% respectively. Most ED and clinic visits were not associated with a serious comor- bid condition (CCI = 0). Prior hospitalization over the past 12 months was slightly higher among those who used the clinic rather than the ED; maintaining a normal A1c level over the past 12 months was also slightly greater for patients who sought care in the clinic; and finally clinic visits were more likely to be used by patients who
had been more compliant with their DM schedules in the past 12 months.
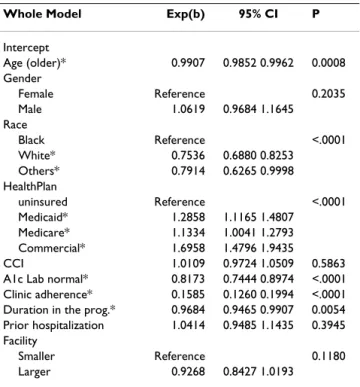
As seen in the full model in Table 3, age (being older), having a normal A1c level, good adherence rates to the clinic schedule, and duration in the program reduced the likelihood of a less-urgent ED visit. Odds ratios (OR) were 0.9907 (CI: 0.9852 - 0.9962, p = 0.0008) for age; 0.8173 (CI: 0.7444 - 0.8974, p < 0.0002) for a normal A1c rate;
0.1585 (CI: 0.1260 - 0.1994, p < 0.0001) for adherence to clinic schedule in the past 12 months; and 0.9684 (CI:
0.9405 - 0.9907, P = 0.0054) for duration in the program.
Being Caucasian or being of another race decreased the likelihood of a less-urgent ED visit as compared with being African-American. ORs were 0.7536 (CI: 0.6880 - 0.8253, p < 0.0001); and 0.7914 (CI: 0.6165 - 0.9998, p = 0.0498), respectively.
Patients with insurance coverage at the time of the visit had an increased likelihood of a less-urgent ED visit, rang- ing from 1.13 for being covered by Medicare, and 1.29 for Medicaid enrolees, to 1.70 for commercial insurance cov- erage as compared with those who were uninsured. Gen- der, comorbidity, experience of hospitalization in the prior year, and facility size were not statistically significant in predicting the odds that a patient would seek less- urgent care in the ED.
Discussion
Diabetes DM programs are intended to improve health status and quality of life for type 2 diabetics and reduce costs by educating patients about the benefits of going to clinics and monitoring their disease conditions regularly [16,17]. Other benefits arise from a successful DM pro- gram--namely patients who adhere to their DM program
Table 1: Patient Characteristics
Source Clinic Visits Less-urgent ED visits N = 119,695 N = 16,249
freq % freq %
Health Commercial 5580 4.66% 1425 8.77%
plan Medicaid 10143 8.47% 1737 10.69%
Medicare 20192 16.87% 2136 13.15%
Missing 307 0.26% 116 0.71%
Uninsured 83473 69.74% 10835 66.68%
CCI 0 79829 66.69% 11634 71.60%
1 22432 18.7% 2957 18.20%
2 11584 9.68% 1138 7.00%
3 3584 2.99% 303 1.86%
4+ 2266 1.89% 217 1.34%
Hospitalization 24061 20.10% 3088 19.00%
CCI: Charlson Comorbidity Index
[18] or effectively manage their A1c reduce the likely usage of the ED care. Patients go to clinics for diabetes not only for check-ups but also to monitor their diabetes con- dition through foot and eye exams and to receive updated information to reduce the risk of complications.
Most studies agree that A1c is an important indicator of patient diabetes control. From this study, patients who maintain their A1c at closer to normal levels reduce their likelihood of less-urgent ED visits about 1.22 times. Fur- ther, patients who remain in the program longer have a decreased likelihood of less-urgent ED visits even though the effects are all slight. The reason is that, after checking the ED visits' distribution, the most less-urgent emergency situations usually occur during the patient's early visits, such as during the first or second year of the DM program.
Aggressive case management to maintain patients' adher-
ence and enhance communication with patients, espe- cially in the first year, may reduce the possibility of future inappropriate ED visits.
In addition, most studies indicate differences in the prev- alence of diagnosed diabetes between racial groups. Afri- can-Americans are more likely to have diabetes, experienced more complications and face unfavourable prognoses. In this study, African-Americans tended to use more ED services in less-urgent situations than other patients after controlling for insurance coverage, adher- ence and management of A1c levels. One possible reason may be that they lack access to sufficient primary care resources, resulting in use of less appropriate care from an ED, which may affect their diabetes outcomes.
The Charlson comorbidity index (CCI) did not provide significant information on ED visit use in this study. One reason is that patient visits associated with severe health conditions were more likely to be classified as urgent and thus dropped from the study [19,20].
This study also triggered some interesting questions for future investigations in diabetes research. For example, according to other studies, uninsured patients are more likely to use the ED for care [21,22]. In this study, the uninsured were less likely to seek care in the emergency department for less-urgent situations. A recent study also found that the uninsured do not use the ED more often [23]. We also examined the effect of a patient changing health plans during the study period on the likelihood of less-urgent ED visits, but this variable did not reveal any significant difference.
One of the reasons for patients with health coverage to use the ED for less-urgent visits may be the need to use after- hour services as well as the inability to get timely appoint- ments at the clinic [24,25]. In this study, we controlled for visits over the weekend when the clinics were closed, but could not control for evening visits during the week.
Another reason that those with insurance coverage are more likely to use the ED for less-urgent visits may the effect of moral hazard on use. Health insurance reduces the out-of-pocket costs of seeking care in the ED. Some of uninsured may be held liable for the costs of the ED visit
Table 2: The distribution of risk factors by visits
Source Clinic Visits Less-urgent ED visits
Mean SD N Mean SD N
A1c normal rate* 0.4069 0.44665 79637 0.3536 0.44855 6397
Clinic adherence* 1.34 0.717 105090 1.02 0.181 11386
Duration 3.0005 1.87428 119695 2.7550 1.98243 16249
Note: 1. *those indicators are based on past 12 months period from every visit 2. study period: 1998 - 2006
Table 3: Multi-variable model estimates of the probability of less- urgent ED visits (adjusted for repeat visits)
Whole Model Exp(b) 95% CI P
Intercept
Age (older)* 0.9907 0.9852 0.9962 0.0008
Gender
Female Reference 0.2035
Male 1.0619 0.9684 1.1645
Race
Black Reference <.0001
White* 0.7536 0.6880 0.8253
Others* 0.7914 0.6265 0.9998
HealthPlan
uninsured Reference <.0001
Medicaid* 1.2858 1.1165 1.4807
Medicare* 1.1334 1.0041 1.2793
Commercial* 1.6958 1.4796 1.9435
CCI 1.0109 0.9724 1.0509 0.5863
A1c Lab normal* 0.8173 0.7444 0.8974 <.0001 Clinic adherence* 0.1585 0.1260 0.1994 <.0001 Duration in the prog.* 0.9684 0.9465 0.9907 0.0054 Prior hospitalization 1.0414 0.9485 1.1435 0.3945 Facility
Smaller Reference 0.1180
Larger 0.9268 0.8427 1.0193
* is significant, P < 0.05
CCI: Charlosn Comorbidity Index
Note: Estimates from a GEE model that accounts for repeat visits by the same patient
if they are not considered indigent [26]. Further study is required to examine the ED usage by insurance status to understand which strategy is suitable to implement in the future.
It seems likely that less-urgent ED visits can be reduced by improving efficiency in primary care by providing a call centre to arrange appointments or case managers to help patients better manage their conditions.
This study used rigid criteria to select the target study pop- ulation. However, several limitations need to be men- tioned. First, we used secondary data and some restrictions, such as the method of data collection, and the coding system, could not be changed. The second limita- tion is the data time frame. DMED established the data collection system in 1998, and we only selected patients who had medical records from 1999. However, this did not mean these DM programs across the state started at the same time, and some programs were in operation ear- lier than the start of DMED's implementation. In other words, some patients may have gone to LSU-HCSD (or to another provider for diabetes treatment) before 1998, which may have affected their behaviour during the period of the study. Additionally, some patients may have received some clinical procedures prior to the start date in this study or obtained care in other non-HCSD facilities.
There was no information on utilization outside of the HCSD system to enable exclusion of these patients from this study. The third limitation is the behaviour of patients who were only in the DM program for a short duration -- less than one year. Patient attrition of non compliant patients may affect the likelihood of non- urgent ED visits when comparing those who have longer durations of care. The final limitation is a generalized application restriction. These research results apply only to the public system of care and may not be suitable for other health care organizations.
Conclusion
In this study, we assessed the factors that predispose or enable less-urgent ED visit use among a group of Type 2 diabetes patients seen within a disease management pro- gram. Our study provides an example in a natural envi- ronment rather than using a randomized controlled trial.
The information from this study can help managers adopt strategies to reduce improper patient use of emergency services. Disease managers need to continually improve the clinical protocol that encourages patients to follow the guidelines for clinic visits and obtain regular laboratory tests and examinations. In particular, patients need to remain in their diabetes disease management programs over several years. Adherence to clinic schedules, includ- ing guidelines, is still the best way to reduce the likelihood of less-urgent ED visits. We suggest providing reminders
for clinic visits, creating continuous care by calling patients regularly or using case managers to reduce the likelihood of less-urgent ED visits. The primary outcome from this investigation provides important information to identify the specific populations who are more likely to use less-urgent ED services. It also provides useful long- term suggestions for reducing the use of ED services while improving quality.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
SCJ and CC jointly drafted every version of the manu- script. RH, LM and RC participated in the design and anal- ysis of the study. RH supervised in acquisition of data. LM provided the statistical consultation. All authors contrib- uted to the discussion and to reviewing the manuscript.
All authors read and approved the final manuscript.
Acknowledgements
The study was supported by LSUHSC HCSD, which provided the original data. We are indebted to Dr. Gene Beyt who provided the background to start this research and also wish to acknowledge the assistance of Dr.
Jolene Johnson and Dr. Ke Xiao, which was essential for finishing this study.
The authors thank Donna Kulawiak, MPH, of Tulane University's Depart- ment of Health Systems Management for her contributions. In addition, we thank Miss Hsiu Mei Wei, Miss Fei Yun Yu and Chi-Jeng Hsieh for their excellent assistance in ICD-9 classification and data programs.
References
1. Chronic Disease Overview [http://www.cdc.gov/nccdphp/over view.htm]
2. Economic costs of diabetes in the U.S. In 2007. Diabetes care 2008, 31(3):596-615.
3. The Diabetes Prevention Program (DPP): description of life- style intervention. Diabetes Care 2002, 25(12):2165-2171.
4. Dorr DA, Wilcox A, Donnelly SM, Burns L, Clayton PD: Impact of generalist care managers on patients with diabetes. Health Serv Res 2005, 40(5 Pt 1):1400-1421.
5. DPP: The Diabetes Prevention Program. Design and meth- ods for a clinical trial in the prevention of type 2 diabetes.
Diabetes Care 1999, 22(4):623-634.
6. Cooper GS, Armitage KB, Ashar B, Costantini O, Creighton FA, Raiz P, Wong RC, Carlson MD: Design and implementation of an inpatient disease management program. Am J Manag Care 2000, 6(7):793-801.
7. Schectman JM, Nadkarni MM, Voss JD: The association between diabetes metabolic control and drug adherence in an indi- gent population. Diabetes Care 2002, 25(6):1015-1021.
8. Hwang U, Concato J: Care in the emergency department: how crowded is overcrowded? Acad Emerg Med 2004, 11(10):1097-1101.
9. Miro O, Sanchez M, Espinosa G, Coll-Vinent B, Bragulat E, Milla J:
Analysis of patient flow in the emergency department and the effect of an extensive reorganisation. Emerg Med J 2003, 20(2):143-148.
10. Rivers EP, Nguyen HB, Huang DT, Donnino MW: Critical care and emergency medicine. Current opinion in critical care 2002, 8(6):600-606.
11. Siegel B: The emergency department: rethinking the safety net for the safety net. Health affairs (Project Hope) 2004:W4-146.
12. Benoit SR, Fleming R, Philis-Tsimikas A, Ji M: Predictors of glyc- emic control among patients with Type 2 diabetes: a longi- tudinal study. BMC Public Health 2005, 5(1):36.
Publish with BioMed Central and every scientist can read your work free of charge
"BioMed Central will be the most significant development for disseminating the results of biomedical researc h in our lifetime."
Sir Paul Nurse, Cancer Research UK
Your research papers will be:
available free of charge to the entire biomedical community peer reviewed and published immediately upon acceptance cited in PubMed and archived on PubMed Central yours — you keep the copyright
Submit your manuscript here:
http://www.biomedcentral.com/info/publishing_adv.asp
BioMedcentral 13. Honish A, Westerfield W, Ashby A, Momin S, Phillippi R: Health-
related quality of life and treatment compliance with diabe- tes care. Dis Manag 2006, 9(4):195-200.
14. Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies:
development and validation. J Chronic Dis 1987, 40(5):373-383.
15. Diabetes management in correctional institutions. Diabetes Care 2006, 29(Suppl 1):S59-66.
16. Krumholz HM, Currie PM, Riegel B, Phillips CO, Peterson ED, Smith R, Yancy CW, Faxon DP: A taxonomy for disease management:
a scientific statement from the American Heart Association Disease Management Taxonomy Writing Group. Circulation 2006, 114(13):1432-1445.
17. Osterberg L, Blaschke T: Adherence to medication. N Engl J Med 2005, 353(5):487-497.
18. Legorreta AP, Christian-Herman J, O'Connor RD, Hasan MM, Evans R, Leung KM: Compliance with national asthma management guidelines and specialty care: a health maintenance organi- zation experience. Arch Intern Med 1998, 158(5):457-464.
19. Farley JF, Harley CR, Devine JW: A comparison of comorbidity measurements to predict healthcare expenditures. Am J Manag Care 2006, 12(2):110-119.
20. Dominick KL, Dudley TK, Coffman CJ, Bosworth HB: Comparison of three comorbidity measures for predicting health service use in patients with osteoarthritis. Arthritis Rheum 2005, 53(5):666-672.
21. McCall N, Korb J, Petersons A, Moore S: Constraining Medicare home health reimbursement: what are the outcomes? Health care financing review 2002, 24(2):57-76.
22. Wharam JF, Landon BE, Galbraith AA, Kleinman KP, Soumerai SB, Ross-Degnan D: Emergency department use and subsequent hospitalizations among members of a high-deductible health plan. JAMA 2007, 297(10):1093-1102.
23. Newton MF, Keirns CC, Cunningham R, Hayward RA, Stanley R:
Uninsured adults presenting to US emergency departments:
assumptions vs data. JAMA 2008, 300(16):1914-1924.
24. Carret ML, Fassa AG, Kawachi I: Demand for emergency health service: factors associated with inappropriate use. BMC Health Serv Res 2007, 7:131.
25. Blanchard J, Ogle K, Thomas O, Lung D, Asplin B, Lurie N: Access to appointments based on insurance status in Washington, D.C. J Health Care Poor Underserved 2008, 19(3):687-696.
26. Dubay L, Holahan J, Cook A: The uninsured and the affordability of health insurance coverage. Health Aff (Millwood) 2007, 26(1):w22-30.
Pre-publication history
The pre-publication history for this paper can be accessed here:
http://www.biomedcentral.com/1472-6963/9/223/pre pub