Central Neurogenic Hyperventilation in A Conscious Patient with
Chronic Brain Inflammation
Yi-Jen Chen
1, Sheng-Feng Sung
2, and Yung-Chu Hsu
21 Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine;
2 Division of Neurology, Department of Internal Medicine, Ditmanson Medical Foundation, Chia-Yi Christian Hospital
Abstract
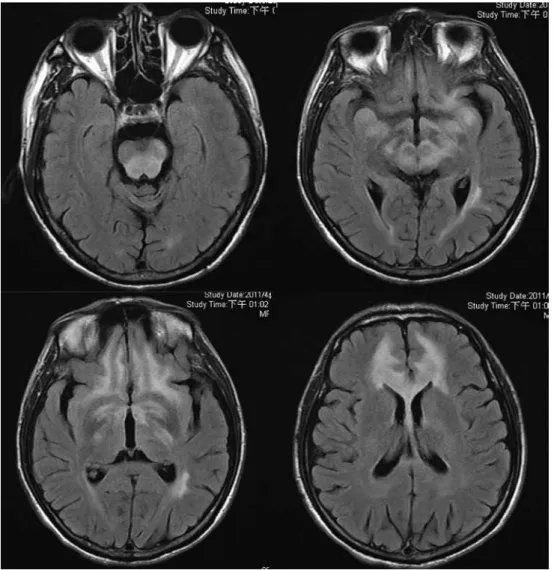
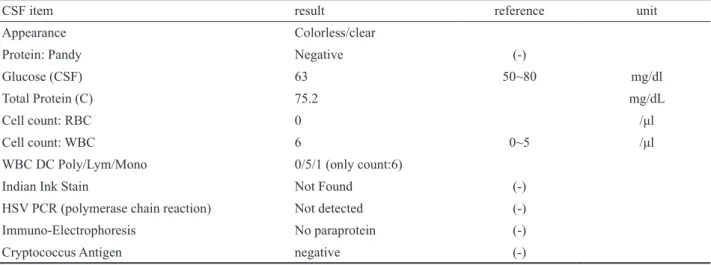
Central neurogenic hyperventilation (CNH) is a rare and easily forgotten diagnosis. A 53-year-old male patient presented with dyspnea for the past 1 month. His consciousness was clear and had bilateral upward gazing palsy. The arterial blood gas analysis showed severe respiratory alkalosis. Brain magnetic resonance imaging revealed symmetric hyperintense lesions involving the midbrain and the area surrounding the fourth ventricle. A brain biopsy showed gliosis and chronic inflammation. CNH results from an uninhibited respira- tory drive due to pons or medulla disorders, and a conscious patient can mislead the initial judgment of the physician. However, severe respiratory alkalosis and persistent nocturnal dyspnea should raise the clinical suspicion of CNH. Chronic brain inflammation with CNH has seldom been reported in the literature. This case provides another pathological possibility of CNH. (J Intern Med Taiwan 2013; 24: 328-333)
Key Words: Central neurogenic hyperventilation, Inflammation, Conscious
Introduction
Hyperventilation is defined as an increase in alveolar ventilation that results in excessive metabolic carbon dioxide expulsion. It may result in a decrease in arterial carbon dioxide tension to below the normal range. Many clinical conditions and diseases can lead to an excessive ventilatory drive, such as hypoxemia, pulmonary disorder, and metabolic disorder. Central neurogenic hyperventi- lation (CNH) is a rare respiratory syndrome which was first reported by Plum and Swanson in 1959.
1It
is defined as respiratory alkalosis induced by lesions in the central nervous system without cardiac, pulmonary or other organic disease. Herein, we present the case of a conscious patient with CNH.
Case presentation
This 53-year-old male patient visited our emergency room (ER) with the chief complaint of progressive dyspnea in the recent one month. He denied drinking, smoking, or having previously undergone gastrointestinal surgery. The rapid respiratory rate was persistent even when he slept.
Reprint requests and correspondence:Dr. Yung-Chu Hsu
Address:Division of Neurology, Department of Internal Medicine, Ditmanson Medical Foundation Chia-Yi Christian Hospital, No. 539, Jhongsiao Rd., Chia-Yi City, Taiwan 60002