Research Express@NCKU - Articles Digest
Research Express@NCKU Volume 12 Issue 10 - March 5, 2010 [ http://research.ncku.edu.tw/re/articles/e/20100305/4.html ]
Analysis and detection of patient-ventilator asynchrony
via a computerized algorithm
Chang-Wen Chen
1,2,*, Wei-Chieh Lin
1, Chih-Hsin Hsu
1, Kuo-Sheng Cheng
2,3, Chien-Shun Lo
41Department of Internal Medicine, College of Medicine, National Cheng Kung University Medical Center; 2Institute of Biomedical Engineering, National Cheng Kung University; 3College of Information Technology, Kun Shan University;and 4Department of Multimedia Design, National Formosa
University, Taiwan.
cwchen@mail.ncku.edu.tw
Critical Care Medicine 36, 455-461(2008)
A
round seventy percent of the patients admitted to our medical intensive care unit need mechanical ventilatory support. It is not unusual to detect patient- ventilator asynchrony as discrepancy between neurally and mechanically assisted breath is prone to occur. Ineffective triggering in expiratory phase (ITE) is documented to be the principal type of patient-ventilator asynchrony and manual calculation is the usual way to quantitate it. As ITE is characterized by its high temporal variability and quantification of patient-ventilatorasynchrony is known to be important in assessing the appropriateness of ventilator settings. We proposed and validated a computerized algorithm in quantitating ITEs in mechanically ventilated patients.
Methods:
Fourteen mechanically ventilated patients, spanning a nine-month period, with high level of patient-ventilator asynchrony were enrolled in this study. An average of 20 minutes recordings of airway pressure, flow, volume and esophageal pressure were made in each case. The expiratory phase was selected according to the flow signal and ITEs were manually identified first. Thereafter, we aimed at two parameters in the ITE-containing segment. The first was maximum flow deflection (Fdef), which is equal to the largest magnitude of flow change when the ventilated patient could not trigger the ventilator. The second was the maximum airway pressure deflection (Pdef), which is the correspondent magnitude of airway pressure change in the same segment of expiration. Graphic illustrations of Fdef and Pdef are shown in Fig. 1. For computerized determination of Fdef , the expiratory phase was selected and Fdef was obtained by applying the local maximum and minimum search algorithm and their consequent difference.
Computerized determination of Pdef was obtained by utilizing a similar algorithm but in reversed direction.
Results:
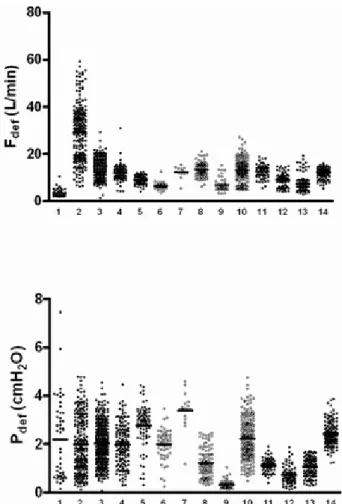
A total of 5899 breaths were analyzed and 1831 breaths belonged to ITEs. The distribution of Fdef and Pdef in these patients are shown in Fig. 2. Mean value for Fdef and Pdef was 13.94 ± 8.0 L/min , 1.91 ± 0.97 cmH2O respectively.
From a starting value of 0.1 L/min for Fdef and 0.01 cmH2O for Pdef, the calculated area under the receiver operator characteristics (ROC) curve of Fdef and Pdef for the identification of ITEs was 0.98 and 0.97 correspondingly. By analysis via a logistic regression model with repeated measurements and computations, the best detection criteria of Fdef was 5.45 L/min with a sensitivity of 91.5% and a specificity of 96.2%; 0.45 cmH2O for Pdef with a sensitivity of
1 of 2
Research Express@NCKU - Articles Digest
93.3% and specificity of 92.9%.
Fig.1: A depiction of ineffective triggering in the expiratory phase (ITE). Paw: airway pressure, Pes:
esophageal pressure. Fdef : maximum flow deflection.
Pdef : maximum airway pressure deflection.
Fig. 2: Scatter plot of the distribution of Fdef and Pdef of breaths containing single ITE in all patients.
Conlusion:
This article is an original approach to automatically quantitate one major type of patient-ventilator asynchrony and we have showed that computerized detection of ITE is feasible in mechanically ventilated patients. Actually following acceptance of our manuscript, we noticed publication of a similar algorithm for detecting patient-ventilator
asynchrony from a ventilator manufacturer (ResMed). The study reflected our team’s capability in doing respiratory physiology in mechanically ventilated patients. This capability is a result of continuing devotion to ventilator physiology in our university hospital. An intimate cooperation between physician and engineer is the key factor for this successful study.
2 of 2