行政院國家科學委員會補助專題研究計畫成果報告
探討人類乳頭狀瘤病毒和臺灣病人的肺癌之關係
The r ole of HPV in lung cancer tumor igenesis of Taiwanese patients
計畫類別:x 個別型計畫 □整合型計畫 計畫編號:NSC89-2320-B-040-041
執行期間:88 年 10 月 01 日至 89 年 09 月 30 日
計畫主持人:許國堂 共同主持人:助理教授
計畫參與人員:碩士研究生 蘇岳行 陳君萍
本成果報告包括以下應繳交之附件:
□赴國外出差或研習心得報告一份
□赴大陸地區出差或研習心得報告一份
□出席國際學術會議心得報告及發表之論文各一份
□國際合作研究計畫國外研究報告書一份
執行單位: 私立中山醫學院
中華民國 89 年 12 月 26 日
2
行政院國家科學委員會專題研究計畫成果報告
探討人類乳頭狀瘤病毒和臺灣病人的肺癌之關係
The r ole of HPV in lung cancer tumor igenesis of Taiwanese patients
計畫編號:NSC 89-2320-B-040-041 執行期限:88 年 10 月 1 日至 89 年 9 月 30 日 主持人:許國堂
執行機構及單位名稱 私立中山醫學院 毒理所 計畫參與人員:蘇岳行 陳君萍
一、中文摘要
肺癌是居於臺灣十大癌症死亡之首,
我們對於造成肺癌的危險因子感到非常得 有興趣,所以積極的尋找那些可能造成肺 癌的危險因子,尤其是造成臺灣病人的肺 癌的危險因子。根據抑癌蛋白 p53 基因活 性的獨特性,推測臺灣的肺癌的形成似乎 與歐美國家不同,因此我們想知道人類乳 頭狀瘤病毒是否可能成為臺灣肺癌的危險 因子。人類乳頭狀瘤病毒是可能造成子宮 頸癌的一個重要因素,可是還沒有足夠的 證據報告說人類乳頭狀瘤病毒和肺癌有直 接的關係。所以我們對於這個推論進行調 查。
我們使用 Nested PCR 的方法來篩選從 組織上萃取出來的 DNA,接著再決定人類乳 頭狀瘤病毒的株型(HPV-6, 11, 16, 18, 31, 33, 58)。經過偵測出來陽性的檢體,再 使用 PCR cycle sequencing 來決定其序列 的正確性。到目前為止,總計偵測了九十 三位病人的檢體。其中發現了 HPV 的 6(1
%)、11(16 %)、16(13 %)、18(47 %)
四種可以被鑑定出來,HPV 的 31, 33, 58 皆無法被偵測出來。其中 17 個檢體含有一 個以上不同型之 HPV。
從病毒的株型來分析;在肺癌的病人 組織中發現的人類乳頭狀瘤病毒以黏膜 性、高危險性的株型(18, 16)為多數。
在肺癌的病人組織中發現的人類乳頭狀瘤 病毒以 18 株型為最多,這和子宮頸癌病人 中發現的以 16 株型為最多,並不相同。根 據這個實驗的初步結果,我們似乎已經從
肺癌組織上找到可能造成細胞腫瘤化的生 物因子,未來將需清楚地調查人類乳頭狀 瘤病毒在肺細胞中的活性對細胞腫瘤化之 影響。有關於人類乳頭狀瘤病毒與肺癌之 關聯性,將會加以討論。
關鍵詞:
肺癌,人類乳頭狀瘤病毒,Nested PCR,
cycle sequencing
Abstr act
Examination of lung cancer patients in Taiwan and Hong Kong showed that the frequency of p53 gene mutation (20%) was lower than previously data reported from other countries (50-80%) (Ref 1,2). Tumor suppressor proteins have been shown that they were inactivated by E6 and E7 viral proteins of human papillomaviruses (HPV).
Moreover, HPV has been found in patients of bromchogenic carcinoma. We propose to investigate whether HPV is a risk factor for lung cancer in Taiwan. We apply nested- PCR and PCR cycle sequencing to screen and determine the specific typing of the HPV present in DNA extracted from 93 samples of lung cancer tissues. The most common HPV types that have been found in our screen were high-risk types HPV (51/93, 55%), which are HPV-18 (47%) and HPV- 16 (13%). Comparing the predominant type of HPV found in cervical cancer (HPV-16) to lung cancer (HPV-18), apparently, association of specific type of HPV with
lung cancer is observed. Multiple infection of HPV in lung cancer have been detected but always associated with a high-risk type of HPV. The correlation of HPV infection to lung cancer would be discussed.
Keywor ds:
lung cancer, human papillomaviruses (HPV), Nested PCR,cycle sequencing
二、緣由與目的
Lung cancer has already become the leading cause of cancer death in Taiwan. We are interested in defining biological risk factors that promote the tumorigenesis of the lung in Taiwanese patients. HPV is a factor may cause human cervical cancer that is supported by many reports but it has no directly evidence of HPV associates with lung cancer. The potential for HPV to alter regulation of proliferation has been confirmed by in vitro transfection of cervical, epidermal, and mammary epithelial cells, resulting in their immortalization (Ref 3, 4, 5, 6). By comparing the data obtained from Nested-PCR and the data from ISH, we would be able to conclude whether the presence of HPV may be a tumorigenesis factor for lung cancer of Taiwanese patients.
This investigation will provide important information for diagnosis and treatment of lung cancer patients in Taiwan.
三、結果與討論
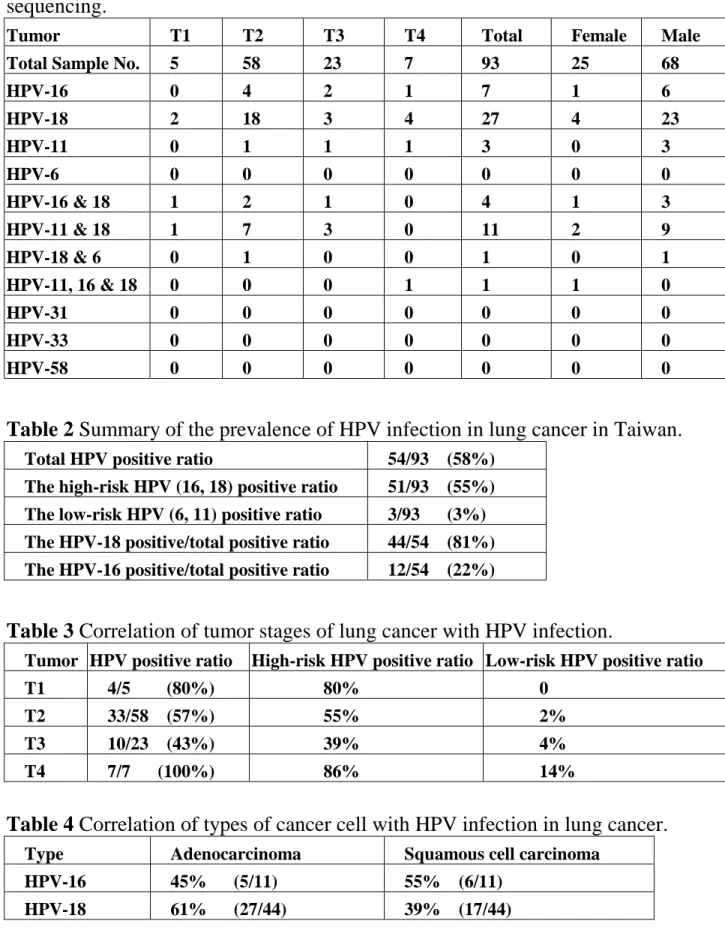
We have analyzed 93 lung cancer tissues collected in Taichung, Taiwan. From the Nested-PCR assay, HPV type 18, 16, 11, and 6 has been detected and confirmed by DNA sequencing. HPV type 58, 33, and 31 has not been detected in our PCR assay. The original data is in Table 1. The total positive ratio for detected HPV is 54/93 (58%) as summarized in Table 2, which including the high-risk HPV (HPV-18, 16) in a ratio of 51/93 (55%) and low-risk HPV (HPV-6, 11) in a ratio of 3/93 (3%). From the HPV positive samples, HPV-18 was detected in 44 out of 53 positive samples. Apparently, the possible virus infection in lung cancer patient is the high-risk HPV-18. Our HPV prevalence in lung cancer seems very high
(58%) but it is similar to what was reported from Okinawa in Japan (Ref). There were 17 samples contain more than one type of HPV DNA and in which at least a high-risk type of HPV is associated with a low-risk type.
There were only 3 cases of HPV-11 detected alone without other type of HPV coexistence.
The only one HPV-6 detected was found with the presence of HPV-18. There are 4 cases of both HPV-16 and 18 positive, 11 cases of HPV-11 and 18 positive, HPV-6 and 18 positive and 1 case of HPV-11, 16, 18 positive.
There are two significant differences were observed from our data when compare with the HPV infection in cervical cancers.
The first significance is that HPV-18, but not HPV-16 is the major type of HPV detected in lung cancer in Taiwan. It has been reported that the majority of squamous cell carcinoma of cervical cancers in Taiwan contained HPV-16 (50%) (Ref 7). The second significance is that we could not detect any HPV-58, 31, or 33 in lung cancer, whereas these three types are frequently detected in cervical cancers. These data indicate that although HPV may associate with lung cancer, the specific type of HPV found in lung cancer is dissimilar to cervical cancers.
It has been proposed that HPV-18-containing tumors have a more aggressive clinical course than do similar cervical cancers with other HPV types (Ref 8, 9). Whether the different type of HPV infection in lung cancer is mediated by virus- tissue preference or oncogenic natural of virus has to be determined.
The clinical stage of tumor associated with HPV infection is listed in Table 3. We could not tell the significance of the tumor stage correlate with HPV infection but it seems that adenocarcinoma is favored by HPV-18 (Table 4).
計畫成果自評
We proposed to correlate the role of HPV in lung cancer tumorigenesis of Taiwanese patients. The following data were expected from this study in our proposal: [1]
What is the prevalence of HPV in lung cancer patients in Taiwan? [2] Which type of
4
HPV is involved? [3] Does HPV viral genes highly expressed in lung cancer patient in Taiwan?
We have successfully answered these questions by using nested-PCR, DNA sequencing to reveal that HPV infection in lung cancer in Taiwan has a prevalence of 58% and the majority of HPV type associated with lung cancer is a high-risk type-18 (55%).
To examine whether the genome of HPV is present in the tissue, we are currently using Catalyzed Signal Amplification (CSA) system that offers in situ PCR sensitivity for in situ hybridization The CSA system has been tested with cervical cancer cell lines that has integrated HPV, for example, SiHa and CaSki with satisfied results in our laboratory. The degree of difficulty is increased when using lung tissues for CSA-in situ hybridization. We are evaluating the performance of CSA system in lung cancer tissue to establish the role of HPV in lung cancer. The last piece of data obtained from CSA-in situ hybridization will enable the results from our research ready for publication.
參考文獻
(1). Takagi Y, Koo LC, Osada H, Ueda R, Kyaw K, Ma C-C, Suyama M, Saji S, Takahashi T, Tominaga S, and Takahashi T.
(1995) Distinct mutational spectrum of the p53 gene in lung cancers from Chinese women in Hong Kong. Cancer Res. 55:
5354-5357.
(2). Wang Y-C, Chen C-Y, Chen S-K, Cherng S-H, Ho WL, and Lee H (1998) High Frenquency of deletion mutations in p53 gene from squmaous cell lung cancer patients in Taiwan. Cancer Res. 58: 328-333.
(3). Band V, Zajchowski D, Kulesa V, and Sager R (1990) Human papilloma virus DNAs immortalize normal human mammary epithelial cells and reduce their growth factor requirement. Proc. Natl. Acad. Sci. USA. 87:
463-467.
(4). Durst M, Dzarlieva-Petrusevska RT, Boukamp P, Fusenig NE and Gissman L.
(1987) Moleclar and cytogenic analysis of immortalized human primary katinocytes obtained after transfection with human
papillomavirus type 16 DNA. Oncogen, 1:
51-256.
(5). Hawley-Nelson P, Vousden KH, Hubbert NJ, Lowy DR, Schiller JT. (1989) HPV16 E6 and E7 proteins cooperate to immortalize human forskin keratinocytes. EMBO J. 8:
3905-3910.
(6). Pirisi, L., Yasumoto, S. et al (1987) Transformation of human fibroblasts and keratinocytes with human papillomavirus type 16 DNA. J. Virol. 61: 1061-1066.
(7). Show-Li Chen, Chih-Ping Han, Yeou- Ping Tsao, Jeng-Woei Lee and Chang-Sheng Yin. (1993)Identification and typing of human papillomavirus in cervical cancers in Taiwan. Cancer 72: 1939-45
(8). Walker J, Bloss JD, Liao SY, Berman M, Bergen S, Wilczynski SP. (1989) Human papillomavirus genotype as a prognostic indicator in carcinoma of the uterine cervix.
Obstet Gynecol. 74: 781-5
(9). Barnes W, Delgado G, Kurman RJ, Petrilli ES, Smith DM, Ahmed S, et al. (1988) Possible prognostic significance of human papillomavirus type in cervical cancer.
Gynecol Oncol. 29: 267-73.
Table 1 Types of HPV DNA detected by Nested-PCR in lung cancer in Taiwan. T1 to T4 are the tumor stages. Sequence of HPV DNA was determined by PCR cycling sequencing.
Tumor T1 T2 T3 T4 Total Female Male
Total Sample No. 5 58 23 7 93 25 68
HPV-16 0 4 2 1 7 1 6
HPV-18 2 18 3 4 27 4 23
HPV-11 0 1 1 1 3 0 3
HPV-6 0 0 0 0 0 0 0
HPV-16 & 18 1 2 1 0 4 1 3
HPV-11 & 18 1 7 3 0 11 2 9
HPV-18 & 6 0 1 0 0 1 0 1
HPV-11, 16 & 18 0 0 0 1 1 1 0
HPV-31 0 0 0 0 0 0 0
HPV-33 0 0 0 0 0 0 0
HPV-58 0 0 0 0 0 0 0
Table 2 Summary of the prevalence of HPV infection in lung cancer in Taiwan.
Total HPV positive r atio 54/93 (58% ) The high-r isk HPV (16, 18) positive r atio 51/93 (55% ) The low-r isk HPV (6, 11) positive r atio 3/93 (3% ) The HPV-18 positive/total positive r atio 44/54 (81% ) The HPV-16 positive/total positive r atio 12/54 (22% )
Table 3 Correlation of tumor stages of lung cancer with HPV infection.
Tumor HPV positive r atio High-r isk HPV positive r atio Low-r isk HPV positive r atio
T1 4/5 (80% ) 80% 0
T2 33/58 (57% ) 55% 2%
T3 10/23 (43% ) 39% 4%
T4 7/7 (100% ) 86% 14%
Table 4 Correlation of types of cancer cell with HPV infection in lung cancer.
Type Adenocar cinoma Squamous cell car cinoma HPV-16 45% (5/11) 55% (6/11)
HPV-18 61% (27/44) 39% (17/44)