ORIGINAL REPORT
J Rehabil Med 41 © 2009 The Authors. doi: 10.2340/16501977-0319
Objectives: To examine the reliability and validity of a Chi-nese version of the Pediatric Evaluation of Disability Inven-tory in children with cerebral palsy.
Design: A prospective study.
Subjects: Two samples: 58 children with cerebral palsy (mean age 65.4 (standard deviation 29.9) months) and 89 normally developing children (mean age 43.5 (standard de-viation 20.6) months).
Methods: The Pediatric Evaluation of Disability Inventory was translated and cross-culturally adapted into a Chinese version. The test-retest reliability, concurrent validity and discriminative validity were examined.
Results: Internal consistency was high (Cronbach’s α: 0.90– 0.99). Test-retest reliability was excellent (intraclass correla-tion coefficient: 0.982–0.998). The concurrent validity was good, as evidenced by the high correlation between the Pedia-tric Evaluation of Disability Inventory and the Functional In-dependence Measure for Children (Spearman’s ρ: 0.92–0.99). Logistic regression analysis demonstrated that the Pediatric Evaluation of Disability Inventory factor scores estimated by confirmatory factor analysis differentiated the children with cerebral palsy from normally developing children.
Conclusion: This study demonstrated that the Chinese ver-sion of the Pediatric Evaluation of Disability Inventory has good reliability and validity and provides support for its use in Chinese-speaking children with cerebral palsy.
Key words: cerebral palsy, Chinese version of the Pediatric
Evaluation of Disability Inventory, reliability, validity. J Rehabil Med 2009; 41: 273–278
Correspondence address: Mei-Hui Tseng, School of Oc-cupational Therapy, College of Medicine, National Taiwan University, No. 17 Xu-Zhou Road, Taipei, Taiwan 10016, ROC. E-mail: mhtseng@ntu.edu.tw
Submitted March 11, 2008; accepted October 14, 2008 INTRODUCTION
Cerebral palsy (CP) has a prevalence of more than 2 per 1000 live births (1), and is the most common cause of long-term disability in children (2). It permanently impairs motor
deve-lopment and restricts participation in daily activities. To help these children achieve as much as they can, clinicians assess and monitor their level of independence in daily activities.
Several measures are available for measuring functional per-formance in daily activities in children. Frequently used measures are the Vineland Adaptive Behavior Scales, the School Function Assessment, the Pediatric Evaluation of Disability Inventory (PEDI), and the Functional Independence Measure for children (WeeFIMTM) (3–6). Of these measures, only the WeeFIMTM and
the PEDI provide information about how much assistance and modification need to be provided for a child’s performance to indicate his or her level of independence in daily activities. The brevity of the WeeFIMTM, which consists of only 18 items, makes
it an efficient screening tool (5, 7). On the other hand, the PEDI (8), which consists of 237 items, provides more comprehensive information regarding a child’s functional performance and the level of assistance required in daily activities.
The PEDI includes a Functional Skills Scale, a Caregiver Assistance Scale, and a Modification Scale for measuring the capacity to perform an activity, real participation, and environ-mental modification, respectively, in daily life. Therefore, the conceptual basis of the PEDI fits the concepts of the International Classification of Functioning, Disability, and Health (ICF) (4, 9), and offers an international common language to compre-hensively understandfunction. As the PEDI follows the ICF’s conceptual model of activity and participation, using the PEDI for measuring functional performance promotes communication among different disciplines, and is valuable for both population survey research (10) and meta-analyses. In addition, the PEDI is comprised of comprehensive daily activities that occur in a natural context. Using the PEDI, clinicians can obtain a thorough understanding of the functional performance of a child with CP and how much assistance a caregiver provides in a child’s daily activities. This information obtained from the PEDI is useful for goal-setting and programme planning.
A clinically useful measure should possess sound psycho-metric properties, including reliability and validity. Reliability refers to the extent to which a measure is reproducible and va-lidity indicates whether a measure is assessing what it intends to assess (11, 12). The PEDI is frequently used to assess daily
RELIABILITY AND VALIDITY OF A CHINESE VERSION OF THE
PEDIATRIC EVALUATION OF DISABILITY INVENTORY IN CHILDREN WITH
CEREBRAL PALSY
Kuan-Lin Chen, BS
1, Ching-Lin Hsieh, PhD
1, 2, Ching-Fan Sheu, PhD
3, Fu-Chang Hu, ScD
4and
Mei-Hui Tseng, ScD
1, 2From the 1School of Occupational Therapy, College of Medicine, National Taiwan University, 2Department of Physical
Medicine and Rehabilitation, National Taiwan University Hospital, 3Institute of Education, National Cheng-Kung
University and 4National Center of Excellence for General Clinical Trial and Research, National Taiwan University
function in children with CP (13–16). The reliability and valid-ity of the PEDI has been studied (17–21). However, most of the studies used samples with various diagnoses. In one exception, McCarthy et al. (18), used an exclusively CP sample, but only the Functional Skills Scale’s psychometric properties were examined. Furthermore, neither the test-retest reliability of the PEDI nor the ability of the PEDI to differentiate children with CP from normal developing children has yet been examined in children with CP. As the reliability and validity of the PEDI has not been fully established specifically in children with CP, more studies with these children are warranted.
The aim of this study was to assess the psychometric proper-ties of a Chinese version of the PEDI (PEDI-C) in children with CP, by examining its internal consistency, test-retest reliability, concurrent validity, and discriminative validity. To improve the utility of the PEDI-C in children with CP, we recruited children with CP with differing motor impairments for this study.
MATERIAL AND METHODS
The study was carried out in 2 phases. First, the PEDI was forward- and backward-translated and adapted into Chinese following a standard pro-cedure (22, 23). Then, the psychometric properties of the PEDI-C were examined in children with CP. The study protocol was approved by the Institutional Review Board of the National Taiwan University Hospital. Pediatric Evaluation of Disability Inventory
The PEDI was designed primarily for assessing functional performance in children aged 6 months to 7.5 years (8). It can also be used for older children whose functional performance falls below that expected for 7.5-year-old normally developing children. The PEDI has been used frequently in children with CP who are aged more than 7.5 years (14, 24, 25).
The PEDI contains 3 scales that can be used together or separately: a Functional Skill Scale, a Caregiver Assistance Scale, and a Modifica-tions Scale. Each scale is divided into 3 domains: self-care, mobility and social function. The Functional Skills Scale contains 197 dichoto-mous items (1: capable, and 0: incapable) assessing daily activities in the 3 domains. The 3 domains in the Functional Skills Scale have 73 items (min. = 0, max. = 73), 59 items (min. = 0, max. = 59) and 65 items (min. = 0, max. = 65), respectively. The Caregiver Assistance Scale comprises 20 items in the 3 domains and reflects how much assistance is required. Each item in the Caregiver Assistance Scale is rated from 0 (total assistance required) to 5 (totally independent). The 3 domains in the Caregiver Assistance Scale have 8 items (min. = 0, max. = 40), 7 items (min. = 0, max. = 35) and 5 items (min. = 0, max. = 25), respec-tively. The Modifications Scale comprises the same 20 items as the Caregiver Assistance Scale and reflects what kinds of modifications are needed to the environment. Each item in the Modifications Scale is a 4-category rating of whether environmental adaptations are used to enhance performance. The 4 discrete categories are: no modifica-tions (N), child-oriented modificamodifica-tions (C), specialized rehabilitation equipment (R) and extensive modifications (E).
The scores obtained from the PEDI consist of a raw score for each of the 3 domains in the Functional Skills Scale and the Caregiver Assistance Scale, and a total frequency count in each category of the Modifications Scale.
There are 2 modes of administrating the PEDI: (i) parent report or structured interview with parents; and (ii) professional judgements of the child’s clinicians and/or teachers.
Translation and cultural adaptation of the Pediatric Evaluation of Disability Inventory
With permission from the Health and Disability Research Institute of Boston University, USA, we translated the PEDI from English into
Chinese. A standard translation process was used, which included forward-backward translation, expert validation and cognitive de-briefing (22, 23).
One occupational therapist and one physiotherapist translated the PEDI into Chinese and, whenever necessary, adapted items to suit the local context. For example, knife and fork were replaced by chopsticks and measuring units were converted into the metric system. The translators also adopted Taiwanese food examples, daily supplies, and common games.
Two bilingual speakers (an occupational therapist and a linguistic expert) examined the forward-translation to eliminate possible misunder-standings and semantic errors. The Chinese version was then translated back into English by a professional translator who is an American-born Taiwanese with no knowledge of the PEDI. The authors examined and revised the wording according to the differences between the backward-translation and the original PEDI. Then, 8 paediatric experts scrutinized each item of the preliminary version for applicability and cultural rel-evance. None of the experts was involved in the translation process.
In the cognitive debriefing, the preliminary version was field-tested on 15 parents, including parents of 3 normally developing children and 12 children with disabilities. The preliminary version of the PEDI-C was revised based on the feedback from the parents regarding the meaning and clarity of items. For example, 11 out of the 15 parents had difficulty answering the items with the criterion of “most situations” as in “capable of performing the tasks in most situations” (8) on the Functional Skills Scale. We consulted Berg et al.’s study (26) for the description of the criterion and we found that in Chinese dictionaries “most situations” means approximately 80% of the time. None of the parents in field test-ing had further difficulty with the items after replactest-ing “most situations” with “about 80% of the time”. The PEDI-C was then finalized. Subjects
The participants consisted of 2 groups: children with CP and normally developing children. The children with CP were recruited from 5 rehabilitation clinics in the cities of Taipei and Kaohsiung between January 2007 and August 2007. Children were included if: (i) they were aged between 6 months and 7.5 years, or older than 7.5 years old and below 12 years with functional abilities below those expected of 7.5-year-old children without disabilities; and (ii) their primary caregivers gave informed consent. Fifty-eight children with CP were eligible to participate in the study. The demographic information, subtype of CP, and severity of the motor function defined by the Gross Motor Func-tion ClassificaFunc-tion System (GMFCS) (27), of the 58 children with CP are shown in Table I.
Table I. Characteristics of children with cerebral palsy (n = 58)
Characteristics Frequency
Age, months, mean (SD) 65.4 (29.9)
Gender, male/female, n 27/31
Type of cerebral palsy, n (%) Spastic Quadriplegia 32 (55.2) Triplegia 1 (1.7) Diplegia 6 (10.3) Hemiplegia 9 (15.5) Dyskinetic 2 (3.4) Hypotonic 6 (10.3) Mixed 2 (3.4) GMFCS, n (%) I 19 (32.8) II 14 (24.1) III 10 (17.2) IV 6 (10.3) V 9 (15.5)
SD: standard deviation; GMFCS: Gross Motor Function Classification System.
A total of 89 normally developing children (47 boys, 42 girls), ranging in age from 11 months to 7 years and 6 months (mean 43.5 months, standard deviation (SD) 20.5 months), were recruited from the well-baby clinics of the National Taiwan University Hospital and 2 nursery schools in Taipei between July 2007 and August 2007. Other measures
The GMFCS (27) is a 5-level system providing a standardized clas-sification of the patterns of motor disability for children with CP from birth to 12 years of age. Distinctions between the 5 levels, ranging from level I (least limitation) to level V (greatest limitation), are based on motor limitations and the needs for mobility devices in 4 age bands. The GMFCS has good reliability and validity (27–30).
The WeeFIMTM (31–33) measures the amount of assistance a child
needs in order to perform daily activities. The WeeFIMTM can be
ap-plied to normally developing children aged 6 months to 7 years and children with disabilities aged 6 months to 21 years. The WeeFIMTM
contains 18 items and covers 3 domains: self-care, mobility and cogni-tion. Each item is ranked from complete dependence (scored as 1) to complete independence (scored as 7). The reliability and validity of the WeeFIMTM have been well established (32, 33).
Procedure
For test-retest reliability, the caregivers of the children with CP were interviewed with the PEDI-C twice, 2 weeks apart, by an occupational therapist with 4 years’ experience in the evaluation and treatment of paediatric patients. Prior to this study, she had received a 20-h train-ing course in understandtrain-ing the conceptual framework, applications, administration and scoring of the PEDI. Following training, she had practiced administering the PEDI-C on 10 children with disabilities and 3 typically developing children. All her assessments during practice were required to be in agreement with an experienced instructor’s as-sessments on at least 90% of the items. All interviews of the PEDI-C used the following sequence: the Functional Skills Scale was admin-istered first, followed by the Caregiver Assistance Scale and then the Modifications Scale.
To assess concurrent validity, the therapist interviewed all the care givers with the WeeFIMTM in the week subsequent to the second
PEDI-C interview. For the discriminative validity, 2 occupational thera-pists interviewed all caregivers of the normally developing children. Statistics
Since Taiwanese norms are not yet available, the raw scores of the PEDI-C were used in all analyses. The internal consistency of each domain in the Functional Skills Scale and the Caregiver Assistance Scale was assessed by Cronbach’s alpha (α) based on the first measure-ment. The value of Cronbach’s α was interpreted as follows (34): poor (< 0.5); moderate (0.5–0.75); good (0.75–0.9); excellent (> 0.9).
The test-retest reliability for the Functional Skills Scale and the Caregiver Assistance Scale was examined using intraclass correlation coefficients (ICCs). The ICC2,1 was used to analyse the agreement
between the 2 interviews for each domain. The value of ICC was interpreted as follows (12): poor (< 0.5); moderate (0.5–0.75); good (0.75–0.9); excellent (> 0.9).
For the categorical scores of the Modifications Scale, Cohen’s kappa statistic (κ) was used to assess the agreement of the 2 interviews (35). A value of the κ coefficient between 0.61 and 0.80 was considered good and between 0.81 and 1.00 was considered near perfect (36).
The concurrent validity of the PEDI-C and the WeeFIMTM was
as-sessed using Spearman’s rank correlation coefficient (ρ) to examine the relationship between the PEDI-C domain scores of the Functional Skills Scale and the Caregiver Assistance Scale and each domain score of the WeeFIMTM. The relationship was interpreted as highly correlated
when ρ was at least 0.60, moderately correlated when ρ was between 0.30 and 0.60, and weakly correlated when ρ was 0.30 or less (12).
For the discriminative validity, first, to avoid the multicollinearity among these important predictors, we conducted 3 separate 1-factor confirmatory factor analyses (CFA): one for the 3 domains of the
Func-tional Skills Scale, one for the 3 domains of the Caregiver Assistance Scale, and the third for the 6 domains of both scales combined (see Appendix I). CFA helps us to identify the core of the integral part of the daily function, which links the 3 highly correlated domains together, for each of the 2 scales and both scales combined.
Next, we fitted 3 separate multiple logistic regression models to examine the discriminative validity of the Functional Skills Scale, the Caregiver Assistance Scale, and both scales combined, for the diagnosis of CP (coded “0” for a normally developing child and “1” for a child with CP) using the corresponding estimated factor scores, respectively. Basic model-fitting techniques for (i) variable selec-tion, (ii) goodness-of-fit assessment, and (iii) regression diagnostics were used in the regression analyses to ensure the quality of analysis results. In each of the 3 separate logistic regression analysis, age, the estimated factor score, and their interaction were considered. The final multiple logistic regression model was obtained by applying the stepwise variable selection procedure with both significance levels for entry and for stay set to 0.15 or larger. The goodness-of-fit (GOF) measures (including the percentage of concordant pairs, estimated area under the receiver operating characteristic (ROC) curve, and the adjusted generalized R2) and the GOF tests (including deviance GOF
test, Pearson χ2 GOF test, and the Hosmer-Lemeshow GOF test) were
used to assess the adequacy of the fitted final model.
All statistical analyses were performed using SPSS 15.0 Software (SPSS Inc., Chicago, IL, USA) except the discriminative validity, which was analysed using LISREL 8 (37) and SAS 9.1.3 software (SAS Institute Inc., Cary, NC, USA). Two-sided p ≤ 0.05 was considered statistically significant.
RESULTS
The mean scores and SD for each domain of the Functional Skills Scale and the Caregiver Assistance Scale from the test-retest assessments in children with CP are shown in Table II. No significant gender difference was observed for any domain of the PEDI-C. The differences between the means of the 2 assessments were smaller than 5% for all domains of the PEDI-C.
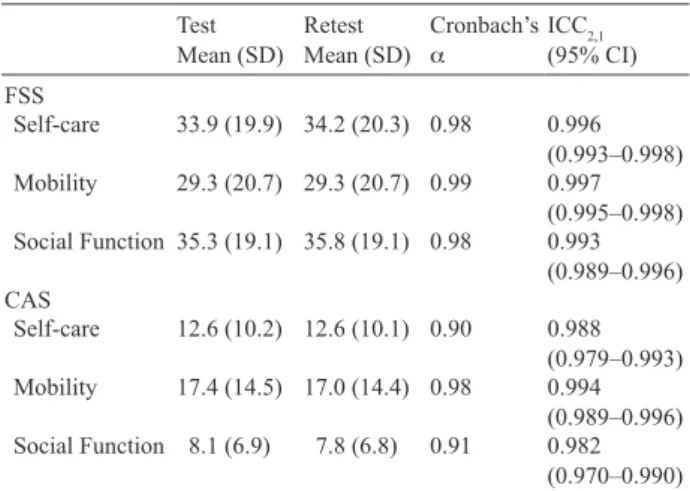
The results regarding internal consistency and test-retest reliability obtained from the sample of children with CP are also presented in Table II. Cronbach’s α ranged between 0.90 Table II. Summary of the Chinese version of the Pediatric Evaluation of Disability Inventory (PEDI-C) scores (raw scores) and the reliability of the Functional Skills Scale (FSS) and the Caregiver Assistance Scale (CAS) for the children with cerebral palsy (n = 58)
Test
Mean (SD) RetestMean (SD) Cronbach’s α ICC2,1 (95% CI) FSS Self-care 33.9 (19.9) 34.2 (20.3) 0.98 0.996 (0.993–0.998) Mobility 29.3 (20.7) 29.3 (20.7) 0.99 0.997 (0.995–0.998) Social Function 35.3 (19.1) 35.8 (19.1) 0.98 0.993 (0.989–0.996) CAS Self-care 12.6 (10.2) 12.6 (10.1) 0.90 0.988 (0.979–0.993) Mobility 17.4 (14.5) 17.0 (14.4) 0.98 0.994 (0.989–0.996) Social Function 8.1 (6.9) 7.8 (6.8) 0.91 0.982 (0.970–0.990) ICC: intraclass correlation coefficients; CI: confidence interval; SD: standard deviation.
and 0.99, indicating excellent internal consistency within each domain of the PEDI-C. All the ICC2,1 values ranged from 0.982
to 0.998. Agreement of the 2 assessments was excellent in all domains of the PEDI-C when used in children with CP. All the 95% confidence intervals (CI) of ICC2,1 were very narrow,
ranging from 0.970 to 0.999.
The agreement of each item of the Modifications Scale is presented in Table III. The mean κ statistics for the Self-care (0.88) and the Social Function domain (1.00) were excellent. The mean κ statistic for the Mobility domain (0.78) was good. At the item level, the κ statistics of all areas in the Modifica-tions Scale were good or excellent.
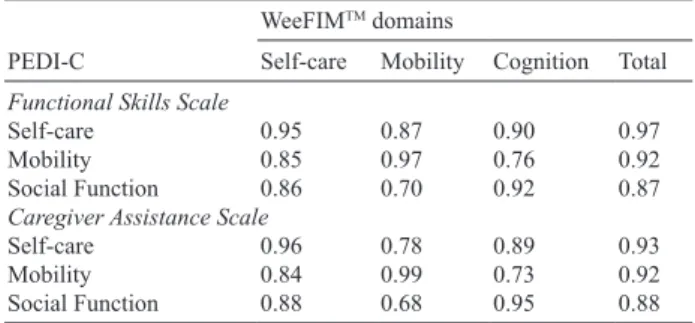
The Spearman’s ρ of the PEDI-C and the WeeFIMTM, ranged
from 0.68 to 0.99, and were all highly correlated (Table IV). The strongest associations were found between the correspond-ing domains of the 2 instruments.
In the discriminative validity, the mean domain scores of the PEDI-C were significantly higher (p < 0.001) in the normally developing children than in those with CP. In the first 2 CFAs, the 1-factor 3-domain factor models fitted to the observed data were all saturated factor models. Thus, they fitted the observed data perfectly. In the third CFA, the 1-factor model fitted the
6 domains of both scales combined well, as indicated by the goodness-of-fit measures (χ2 = 11.94, df = 6, Comparative Fit
Index = 1.00, root mean square error of approximation = 0.08). Based on these 3 well-fitted 1-factor models, the corresponding factor scores were estimated for the latent constructs of the Functional Skills Scale, the Caregiver Assistance Scale, and both scales combined, respectively (see Appendix I).
As listed in Table V, the 3 fitted multiple logistic regression models showed that conditioning on children’s age, the Func-tional Skills Scale, the Caregiver Assistance Scale, and both scales combined could effectively differentiate the children with CP from the normally developing children, respectively. Specifically, after adjusting for the effect of children’s age, the children with an increase of one point on the estimated Func-tional Skills Scale factor score would have 0.21 times smaller odds (p < 0.0001) of being diagnosed as CP, where the odds are the ratio of the probability of being diagnosed as CP vs that of not being diagnosed as CP. Likewise, after adjusting for the ef-Table III. Test-retest reliability for the items in the Modifications Scale
(MS) of the Chinese version of the Pediatric Evaluation of Disability Inventory (Cohen’s kappa)
Domain of the MS
Items of each domain
1 2 3 4 5 6 7 8 Mean
Self-care 0.87 0.91 0.63 0.83 0.95 0.85 1.00 0.97 0.88 Mobility 0.88 0.93 0.63 0.77 0.77 0.72 0.78 – 0.78 Social
Function 1.00 1.00 1.00 1.00 1.00 – – – 1.00
Table IV. Correlations between of the Chinese version of the Pediatric Evaluation of Disability Inventory (PEDI-C) and the Functional Independence Measure for children (WeeFIMTM) for the 58 children with
cerebral palsy (CP) (Spearman’s correlation coefficients: ρ) PEDI-C
WeeFIMTM domains
Self-care Mobility Cognition Total Functional Skills Scale
Self-care 0.95 0.87 0.90 0.97
Mobility 0.85 0.97 0.76 0.92
Social Function 0.86 0.70 0.92 0.87
Caregiver Assistance Scale
Self-care 0.96 0.78 0.89 0.93
Mobility 0.84 0.99 0.73 0.92
Social Function 0.88 0.68 0.95 0.88
Table V. Discriminative validity of the Chinese version of the Pediatric Evaluation of Disability Inventory (PEDI-C) Functional Skills Scale, Caregiver Assistance Scale, and combined both: multiple logistic regression model for diagnosis of cerebral palsy (CP)
Covariate Estimate Standard error Waldchi-square p-value Oddsratio
CP group logistic regression model I1: Functional Skills Scale factor scores (FSSfs) and age
Intercept –8.80 1.60 30.31 <0.0001 –
Age 2.71 0.53 26.50 <0.0001 15.01
Age × FSSfs –1.57 0.31 25.09 <0.0001 0.21
CP group logistic regression model II2: Caregiver Assistance Scale factor scores (CASfs) and age
Intercept –8.23 1.49 30.44 <0.0001 –
Age 2.29 0.44 26.95 <0.0001 9.87
Age × CASfs –1.14 0.22 26.37 <0.0001 0.32
CP group logistic regression model III3: both combined factor scores (CBfs) and age
Intercept –9.59 1.77 29.21 <0.0001 –
Age 2.85 0.55 26.53 <0.0001 17.22
Age × CBfs –1.49 0.30 25.57 <0.0001 0.23
1CP group logistic regression model I: n = 147, percentage of concordant pairs = 94.1%, percentage of discordant pairs = 5.9%, adjusted generalized
R2 = 0.7729, Deviance goodness-of-fit test p = 1.00 > 0.05 (df = 144), Pearson goodness-of-fit test p = 0.40 > 0.05 (df = 144), and Hosmer-Lemeshow
goodness-of-fit test p = 0.23 > 0.05 (df = 8).
2CP group logistic regression model II: n = 147, percentage of concordant pairs = 95.1%, percentage of discordant pairs = 4.8%, adjusted generalized
R2 = 0.7774, Deviance goodness-of-fit test p = 1.00 > 0.05 (df = 144), Pearson goodness-of-fit test p = 0.46 > 0.05 (df = 144), and Hosmer-Lemeshow
goodness-of-fit test p = 0.63 > 0.05 (df = 8).
3CP group logistic regression model III: n = 147, percentage of concordant pairs = 95.8%, percentage of discordant pairs = 4.1%, adjusted generalized
R2 = 0.8035, Deviance goodness-of-fit test p = 1.00 > 0.05 (df = 144), Pearson goodness-of-fit test p = 0.09 > 0.05 (df = 144), and Hosmer-Lemeshow
fect of children’s age, the children with an increase of one point in the estimated Caregiver Assistance Scale factor score or the estimated factor score of both scales combined would have 0.32 or 0.23 times smaller odds (p < 0.0001) of being diagnosed as CP, respectively. The GOF measures and testing results listed in the bottom of Table V indicated that all these 3 logistic regression models fitted the observed binary data very well.
DISCUSSION
In this study, the PEDI-C used in Chinese children with CP exclusively had excellent internal consistency, test-retest re-liability, concurrent validity and discriminative validity, and could differentiate the functional performance of children with CP with differing severities of motor function from that of normally developing children. These findings support the use of the PEDI-C by clinicians and researchers as a measure to evaluate functional performance in self-care, mobility and social function in Chinese children with CP.
The internal consistency of the PEDI-C was excellent and there were no negative item-total point biserial correlations, indicating that all items contributed positively to the total score of each domain and confirming the homogeneity of all items in the PEDI-C for measuring functional performance of children with CP in each domain.
Excellent test-retest reliability is a prerequisite if a measure is to be used for repeated evaluations and outcome follow-up. The high ICC values indicate that the PEDI-C has excellent test-retest reliability and could consistently measure functional performance of the children with CP over time.
The concurrent validity of the PEDI-C in children with CP was supported by the high correlations between corresponding domains of the PEDI-C and the WeeFIMTM, suggesting that
the 2 functional measures assessed the same construct. These results were consistent with the results of other studies of the PEDI and the WeeFIMTM using clinical samples with various
diagnoses (7, 8).
The discriminative validity of the Functional Skills Scale, the Caregiver Assistance Scale, and both combined for distin-guishing between the children with and without disability in daily functional performance was supported by the results of logistic regression analysis with a high discriminative accuracy (Table V). These 3 well-fitted logistic regression models also lend support to the test design of the PEDI, that the 3 scales of the PEDI can be used separately or together.
Among all domains, the Mobility domain in both the Functional Skills Scale and the Caregiver Assistance Scale, showed better psychometric properties than the Self-care and the Social Function domains in children with CP. This finding is consistent with the results of studies using the PEDI in both Dutch and Norwegian children (20, 21). It might be that the items in the Mobility domain were less subjected to choice of parents than those in the Self-care and the Social Function domains. Many items in the Self-care and the Social Function domains were not carried out by a child as often as those in the Mobility domain. Accordingly, the child’s parents had fewer opportunities to observe his or her performance and needed
to recall from memory in answering the item questions in the Self-care and the Social Function domains.
This study has 3 potential limitations. First, the data collec-tion for children with CP was carried out by only one therapist. The values of the test-retest reliability and internal consistency might have been over-estimated. Future studies of the PEDI-C should assess inter-rater reliability for children with CP. The PEDI-C, with acceptable inter-rater reliability in children with CP, would allow it to be used reliably by different clinicians to assess clients’ functional performance.
Secondly, our results are restricted to the modes of structured interview. Interviewing caregivers with the PEDI-C provides clinicians a clear and comprehensive understanding of caregiv-ers’ actual way of taking care of their children in a natural context. The reliability and validity of the PEDI-C should be investigated further using the mode of professional judgements that has often been used in published studies.
Thirdly, the study adopted participants with different types of CP and various degrees of severity, who might have different profiles of functional limitations in daily lives. The reliability and validity of the PEDI-C could be investigated further in homogeneous groups of children with specific types of CP.
In conclusion, the PEDI-C is a reliable and valid instrument when used to evaluate functional performance in self-care, mobility and social function in Chinese children with CP. Furthermore, the PEDI-C can discriminate children with CP in various degrees of severity from normally developing children, based on their functional performance in daily activities. This study adds to available research with respect to the reliability and validity of the PEDI in children with CP.
ACKNOWLEDGEMENTS
We thank the children’s caregivers for their participation. We also thank occupational therapists of the National Taiwan University Hospital, the Kaohsiung Municipal Hsiaokang Hospital, the Country Hospital, the Sheng-Yuan Children Developmental Center, the San Min Nursery School and the Ji Li Nursery School for their assistance with data collection; the project would not have been possible without their contributions. We are also sincerely grateful to Professor Anne Henderson for her valuable comments on the manuscript. The study was supported by the National Science Council of Taiwan (NSC 97-2410-H-002-044-MY2).
REFERENCES
1. Odding E, Roebroeck ME, Stam HJ. The epidemiology of cerebral palsy: incidence, impairments and risk factors. Disabil Rehabil 2006; 28: 183–191.
2. Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl 2007; 109: 8–14. 3. Schenker R, Coster W, Parush S. Participation and activity
perform-ance of students with cerebral palsy within the school environment. Disabil Rehabil 2005; 27: 539–552.
4. Ogonowski J, Kronk R, Rice C, Feldman H. Inter-rater reliability in assigning ICF codes to children with disabilities. Disabil Rehabil 2004; 26: 353–361.
5. Ottenbacher KJ, Msall ME, Lyon N, Duffy LC, Ziviani J, Granger CV, et al. Functional assessment and care of children with neurodevelop-mental disabilities. Am J Phys Med Rehabil 2000; 79: 114–123.
6. Donkervoort M, Roebroeck M, Wiegerink D, van der Maessen H, Stam H. Determinants of functioning of adolescents and young adults with cerebral palsy. Disabil Rehabil 2007; 29: 453–463.
7. Ziviani J, Ottenbacher KJ, Shephard K, Foreman S, Astbury W, Ireland P. Concurrent validity of the Functional Independence Meas-ure for Children (WeeFIM) and the Pediatric Evaluation of Disabili-ties Inventory in children with developmental disabiliDisabili-ties and acquired brain injuries. Phys Occup Ther Pediatr 2001; 21: 91–101. 8. Haley SM, Coster WJ, Ludlow LH, Haltiwanger JT, Andrellos
PJ, editors. Pediatric Evaluation of Disability Inventory (PEDI): development, standardization and administration manual. Boston, MA: New England Medical Center Hospitals; 1992.
9. Ostensjo S, Bjorbaekmo W, Carlberg EB, Vollestad NK. Assessment of everyday functioning in young children with disabilities: an ICF-based analysis of concepts and content of the Pediatric Evaluation of Disability Inventory (PEDI). Disabil Rehabil 2006; 28: 489–504. 10. Gannotti ME, Handwerker WP. Puerto Rican understandings of
child disability: methods for the cultural validation of standardized measures of child health. Soc Sci Med 2002; 55: 2093–2105. 11. Hobart JC, Lamping DL, Thompson AJ. Evaluating neurological
outcome measures: the bare essentials. J Neurol Neurosurg Psy-chiatry 1996; 60: 127–130.
12. Portney LG, Watkins MP, editors. Foundations of clinical research: applications to practice. NY: Prentice Hall Health; 2000. 13. Ödman P, Öberg B. Effectiveness of intensive training for children
with cerebral palsy – a comparison between child and youth rehabilita-tion and conductive educarehabilita-tion. J Rehabil Med 2005; 37: 263–270. 14. Ohata K, Tsuboyama T, Haruta T, Ichihashi N, Kato T, Nakamura
T. Relation between muscle thickness, spasticity, and activity limitations in children and adolescents with cerebral palsy. Dev Med Child Neurol 2008; 50: 152–156.
15. Volman MJ, Visser JJ, Lensvelt-Mulders GJ. Functional status in 5 to 7-year-old children with Down syndrome in relation to motor ability and performance mental ability. Disabil Rehabil 2007; 29: 25–31. 16. Voorman JM, Dallmeijer AJ, Schuengel C, Knol DL, Lankhorst
GJ, Becher JG. Activities and participation of 9- to 13-year-old children with cerebral palsy. Clin Rehabil 2006; 20: 937–948. 17. Custers JW, van der Net J, Hoijtink H, Wassenberg-Severijnen JE,
Vermeer A, Helders PJ. Discriminative validity of the Dutch Pedi-atric Evaluation of Disability Inventory. Arch Phys Med Rehabil 2002; 83: 1437–1441.
18. McCarthy ML, Silberstein CE, Atkins EA, Harryman SE, Sponseller PD, Hadley-Miller NA. Comparing reliability and validity of pediat-ric instruments for measuring health and well-being of children with spastic cerebral palsy. Dev Med Child Neurol 2002; 44: 468–476. 19. Custers JW, Wassenberg-Severijnen JE, Van der Net J, Vermeer
A, Hart HT, Helders PJ. Dutch adaptation and content validity of the “Pediatric Evaluation Of Disability Inventory (PEDI)”. Disabil Rehabil 2002; 24: 250–258.
20. Berg M, Jahnsen R, Froslie KF, Hussain A. Reliability of the
Pediatric Evaluation of Disability Inventory (PEDI). Phys Occup Ther Pediatr 2004; 24: 61–77.
21. Wassenberg-Severijnen JE, Custers JW, Hox JJ, Vermeer A, Helders PJ. Reliability of the Dutch Pediatric Evaluation of Dis-ability Inventory (PEDI). Clin Rehabil 2003; 17: 457–462. 22. Gandek B, Alacoque J, Uzun V, Andrew-Hobbs M, Davis K. Translating
the Short-Form Headache Impact Test (HIT-6) in 27 countries: meth-odological and conceptual issues. Qual Life Res 2003; 12: 975–979. 23. Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation
of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol 1993; 46: 1417–1432. 24. Ödman PE, Öberg BE. Effectiveness and expectations of intensive
training: a comparison between child and youth rehabilitation and conductive education. Disabil Rehabil 2006; 28: 561–570. 25. van Empelen R, Jennekens-Schinkel A, Gorter JW, Volman MJ,
van Nieuwenhuizen O, Helders PJ. Epilepsy surgery does not harm motor performance of children and adolescents. Brain 2005; 128: 1536–1545.
26. Berg M, Jahnsen R, Holm I, Hussain A. Translation of multi-disci-plinary assessment-procedures to achieve functional equivalence. Adv Physiother 2003; 5: 57–66.
27. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 1997; 39: 214–223.
28. Bodkin AW, Robinson C, Perales FP. Reliability and validity of the gross motor function classification system for cerebral palsy. Pediatr Phys Ther 2003; 15: 247–252.
29. Palisano RJ, Hanna SE, Rosenbaum PL, Russell DJ, Walter SD, Wood EP, et al. Validation of a model of gross motor function for children with cerebral palsy. Phys Ther 2000; 80: 974–985. 30. Wood E, Rosenbaum P. The gross motor function classification
system for cerebral palsy: a study of reliability and stability over time. Dev Med Child Neurol 2000; 42: 292–296.
31. Uniform Data System for Medical Rehabilitation. WeeFIM IISM System Clinical Guide, version 5.01. Buffalo, NY: Uniform Data System for Medical Rehabilitation; 2002.
32. Wong SS, Wong VC. Functional Independence Measure for Chil-dren: a comparison of Chinese and Japanese children. Neurorehabil Neural Repair 2007; 21: 91–96.
33. Wong V, Wong S, Chan K, Wong W. Functional Independence Measure (WeeFIM) for Chinese children: Hong Kong Cohort. Pediatrics 2002; 109: E36.
34. Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika 1951; 16: 297–334.
35. Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas 1960; 20: 37–46.
36. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–174.
37. Jöreskog KG, Sörbom D, editors. LISREL 8: user’s reference guide. Chicago, IL: Scientific Software International; 1996. APPENDIx I. Confirmatory factor analyses (CFA) of the Functional Skills Scale, the Caregiver Assistance Scale, and both scales combined In the analysis of discriminative validity, a serious multicollinearity
problem was found between 2 sets of 3 domains of the Functional Skills Scale and the Caregiver Assistance Scale in the fitted multiple logistic regression model. A standard way of handling such a problem is to apply principal component analysis or factor analysis to reduce the dimension of the predictors (according to Hamilton LC. Regression with graphics: a second course in applied statistics. Belmont, CA: Duxbury; 1992) Thus, to avoid the multicollinearity among these important predictors, we conducted 3 separate 1-factor confirmatory factor analyses (CFA): one for the 3 domains of the Functional Skills Scale, one for the 3 domains of the Caregiver Assistance Scale, and the third one for the 6 domains of both scales combined. In the first 2 CFAs, the 1-factor 3-domain factor models fitted to the observed data were all saturated
factor models in the sense that the number of parameters to be estimated was equal to the number of unique elements in the variance-covariance matrix of the observed scores of the 3 domains. Thus, they fitted the observed data perfectly. In the third CFA, the 1-factor model fitted the 6 domains of both scales combined well as indicated by the goodness-of-fit measures (χ2 = 11.94, df = 6, Comparative Fit Index = 1.00, root
mean square error of approximation = 0.08). Based on these 3 well-fitted 1-factor models, the corresponding factor scores were estimated for the latent constructs of the Functional Skills Scale, the Caregiver Assistance Scale, and both scales combined, respectively. In summary, CFA helps us identify the core of the integral part of the daily function, which links the 3 highly correlated domains together, for each of the 2 scales and both scales combined.