Endothelial Functions in Healthy Adult Subjects: Better Hemodynamic Responses in Brachial Artery Than in Popliteal Artery?
Mike Lin, Kai-Sheng Hsieh*, Shoa-Lin Lin**, Hong-Ting Chiang**, Shen-Wen Kou***, and Shih-Chung Lin****
Department of Medicine, KJGH-PinTung, and United Clinical Center-KS and I-Sou University-KS, *Pediatric Department, VGH-KS,
**Department of Medicine, VGH-KS; NYMU,
***Department of Public Health, CMC-Taichung,
****Department of Medicine, KGH, Tainan Abstract
Endothelial function (EF) plays a central role in the development of vascular disease and represents a marker of prognostic relevance. Endothelial dysfunction (ED) in individuals with atherosclerosis and coronary risk factors contributes to the pathophysiology of acute cardiovascular syndromes. Ultrasound examination of brachial artery flow-mediated dilation (FMD) has emerged as a valuable noninvasive method for assessing EF and has developed into a potentially useful tool in the clinical setting. However, there is an unsettled puzzle regarding EF if both upper and lower limbs evaluated simultaneously in general healthy populations. Thus, the present study was aimed to investigate the difference of hemodynamic effects as well as EF between brachial artery (BA) and popliteal artery (PA) in normal healthy volunteers.
High frequency ultrasound was used to measure blood flow and percentage of BA dilatation after reactive hyperemia induced by forearm cuff occlusion (250mmHg) for 5 minutes (physiologic compression test, PCT) in 21 normal healthy volunteer
subjects, less than 45 years of age, without known any cardiovascular risk factors. The same protocol was also applied to test the PA subsequently.
All subjects stood up with PCT procedures well. Peak blood flow (PBF) increased form 44.3±32.5 at baseline to 102.9±80.5 (ml/min) post PCT in BA group (p<0.001) and from 41.9±30.3 to 61.5±46.3 (ml/min) in PA group (p<0.01). Increase in flow during reactive hyperemia (FIRH), which is expected to increase post PCT, was highly significant in BA group (269±136%) but mildly increased in PA group (164±97%). Thus, better vascular response of BA group was observed in contrast to PA group (P<0.01). FMD also showed the similar findings (P<0.05). Moreover, peak systolic velocity (PSV) and peak diastolic velocity (PDV), were significantly higher in BA group (PSV: 85±40 cm/sec; PDV: 14.8±14.5cm/sec) than in those of PA group (27±11cm/sec; 3.5±2.2cm/sec). The peak systolic gradient and diastolic gradient
between BA and PA also showed significant difference (p<0.05). Resistance index (RI), which is doomed to decrease during PCT, was not significantly changed in PA group but significantly decreased in BA group (p<0.05).
After PCT, as expected, both BA and PA dilated, and the reactive blood flow significantly increased. Both FMD did as well. Better EF as well as hemodynamic effects of BA group were significantly observed in contrast to PA group. These
findings may support the hypothesis that ED may first originate from the lower part of human body (below heart) in general healthy populations which may be correlated with natural human atherosclerotic progression. Briefly speaking, EF and vascular responses in both upper and lower limb were quite different to the human beings, highlighting the different prognostic importance of identifying early abnormalities in both upper and lower limbs vascular function in individual patients. Because ED is an independent predictor of future cardiovascular events, we may suggest noninvasive assessments of both upper and lower limb EF might prove valuable in any
cardiovascular risk assessment and finally become a target for future risk factors reduction and managements, making our methodology more practical for clinical use.
( J Intern Med Taiwan 2002;13: 237-246 )
Key Words:Endothelial dysfunction (ED),Endothelial function (EF), Brachial artery (BA),
Popliteal artery (PA),Physiologic compression test (PCT),
Flow-mediated dilation (FMD),Flow-increase during reactive hyperemia (FIRH)
Introduction
The development of noninvasive methods to assess vascular endothelial function (EF) has allowed many studies of healthy subjects and also has confirmed independent associations of endothelial dysfunction (ED) with any traditional cardiovascular risk factors as well as hyperhomocysteinemia1-4. ED is an initial event in the
development of atherosclerosis and can contribute to the progression of the vascular disease1-4. The vascular endothelium plays a predominant role in circulatory
homeostasis via the liberation of various vasoactive substances such as nitric oxide (NO), prostacyclins and endothelins, etc1-2. When Furchgott and Zawadzki report that acetylcholine-induced vasodilation occurs only in the presence of an intact
endothelium3, we recognize that the endothelium-mediated vasodilation is largely due to endothelium-derived NO2-4, a single molecule with profound effects on
cardiovascular physiology2-4. Impairment of EF is now established as a major
contributor to any cardiovascular disease1-6. Many investigators also have shown that
ED is significantly related to the pathogenesis of coronary artery disease (CAD), vasospasm, and acute coronary syndrome (ACS)1,4,6. Takasi et al first reported that good correlation between brachial artery (BA) ED and coronary artery (CA) ED7, which is useful in prediction especially for future cardiovascular events in patients with suspected CAD7. In fact, ED underlies many stages in the progression of atherosclerosis from earliest onset to the lesions that result in CAD6-8. ED also is present in cardiovascular risk factor conditions such as hypertension, diabetes mellitus, smoking, and dyslipidemia that precede the onset of atherosclerosis5,6, and this has been documented even in children4,5. Given the pivotal role for ED as a central mechanism involved with many risk factor conditions as well as the disease
itself1,4,6,9,10, it seems reasonable to employ a noninvasive method to detect normal healthy adult volunteer upper and lower limbs function (EF)9-14. Then, an important question should be raised. Is there any difference between upper limb and low limb regarding EF? To the best of our knowledge, no study has solved this unsettled question yet. Thus, the first aim of this study was to exam both upper and low limbs EF simultaneously in normal healthy adult volunteer populations. Another purpose was to compare the hemodynamic effects of physiologic compression test in both brachial artery and popliteal artery in the same population.
Methods
Study population
Twenty-one adult healthy volunteers were recruited to receive morning vascular tests from our institution since 2000. All were normotensive, less than 45 years of age, non-smokers, non-diabetic, without any cardiovascular risk factors, together with normal serum lipid profiles and on no any medications. All subjects were required to have normal sinus rhythm.
Endothelial Function (FMD and FIRH)
Endothelial function of both brachial artery (BA) and popliteal artery (PA) were assessed. By means of high-resolution ultrasound, diameter changes of both limb arteries in response to reactive hyperemia (flow-mediated vasodilation [FMD]) were detected, referring to the standard protocols1,4,9-12. Flow-mediated vasodilation together with blood flow increase response to reactive hyperemia [FIRH] represents endothelium-dependent vasoreactivity4,9-14. Accuracy and reproducibility have been documented and reported before9-14. Reactive hyperemia, induced by distal cuff occlusion and release, leads to a release of endothelium-dependent vasodilator substances (NO) medicated by shear stress, rather than ischemic metabolites4,12. As the vessel diameter after reactive hyperemia is usually maximal after 45 seconds to 60 seconds, when flow velocity has already normalized4,12, vasodilation is not due to physical requirements of enhanced flow12. Thus, individual vascular EFs of both RA
and PA were then obtained.
Technical settings
Both arteries were examined by 2-D ultrasound images, with a 7.5 to 10 MHz compact linear transducer (Hewlett Packard Sonos 5500 or General Electric Vivid Systems). The transducer was positioned appropriately to achieve and obtain
longitudinal pictures of both brachial artery and popliteal artery. Transmit zone, depth and gain were set to optimize images of the lumen/arterial-well interface; images were magnified by resolution box function; machine operating parameters were not
changed during the study9-14. The ultrasonic vascular images were acquired ECG-Triggered at end-diastole throughout the study9-14. Arterial flow velocity of both arteries was measured by pulsed Doppler signal at a 600 angle to the vessel throughout the study12.
Study Protocol
All subjects' height and weight were recorded and body mass index was derived. After the subjects had rested in the recumbent position for at least 5 minutes, right arm and leg blood pressure were measured using a mercury sphygmomanometer. Diastolic pressure was determined as Korotkoff phase V and the mean of two recordings was used. The subjects' right arm was comfortably immobilized in the extended position to allow consistent imaging of the brachial artery12. The brachial artery segment 1-6 cm above the antecubital crease was located and imaged in the longitudinal plane,
ensuring the lumen diameter was maximized and the gain optimized to provide clear arterial wall interfaces12. The distance from the antecubital crease was noted and the following examinations were all performed in the same position12. Arterial flow velocity measurements were obtained using a pulsed Doppler signal at 600 to the vessel with the range gate (1.5mm) in the center of the artery12. Images were recorded on videotapes or discs for subsequent off-line analysis. After an initial 15 min resting period, baseline recordings of brachial artery diameter and flow velocity were performed12. A standard sphygmomanometer cuff, placed around the forearm distal to the imaged brachial artery segment, was inflated to a pressure of 250mmHg for 5 min12. Blood flow was recorded prior to and immediately after cuff release for at least 30 to 60 seconds12. Continuous B-mode images were also collected for 1-2 min after cuff release12. All subjects took 5 minutes rest and received right popliteal artery vascular endothelial function and hemodynamic examination. As to popliteal artery evaluation, the transducer is positioned posteriorly for imaging of the popliteal artery (PA)15. The leg remains in an externally rotated position with the knee slightly flexed15. Imaging from the posterior projection is sometimes necessary15. Using color coding, the thigh level is especially easy to
evaluate, due to the extended course of the femoral artery15. The entire distance can
be rapidly followed to the adductor canal15. In this position, however, a change in position is sometimes necessary15. The popliteal artery, which is located near the surface, is easily displayed from a dorsal direction15. The popliteal artery segment within the posterior knee joint area was then clearly located and imaged in the longitudinal plane, ensuring the lumen diameter was maximized and the gain optimized to provide clear arterial wall interfaces15.
B-mode ultrasound and arterial flow velocity together with lower limb endothelial functions were
also obtained according to the same protocol12,15. Besides, PA/BA index as well as total hyperemic response were also thoroughly evaluated12,15. Subsequent
hemodynamic data were collected for further analysis.
Data Analyses
Images were digitally acquired from the disk and/or videotapes and measured in random order by a single observer blinded to the phase of the study12. The brachial artery and popliteal artery diameters were measured using the leading edge of the near wall to the leading edge of the far wall of the artery along a line perpendicular to the artery's long axis using an electronic calliper12,15. Both brachial and popliteal artery diameter were derived form the mean of four measurements (two on each of two images)12,15 . Flow increase during reactive hyperemia (FIRH), flow-mediated dilation (FMD), and total hyperemic responses were expressed as the percentage change relative to the mean baseline scan4,12,15. Volume flow was calculated by multiplying the velocity time integral of the Doppler flow signal for a single pulse wave by the heart rate and vessel cross-sectional area10-12. Volume flow was
measured during rest and at the peak response of the maximal flow in a single cardiac cycle during the 10-60 seconds period after cuff release10-12. The percent increase in the blood flow of the BA and PA, observed immediately after the cuff deflation, was calculated as the maximal flow recorded after the cuff deflation divided by the flow at baseline10-12.
Statistical analysis
Measurements are expressed as mean±SD. The two-sided paired student t test was used to compare alternations in vascular responses and hemodynamic changes between BA and PA subsets, with p≦0.05 an indicator of statistical significance12.
Results
Clinical Characteristics
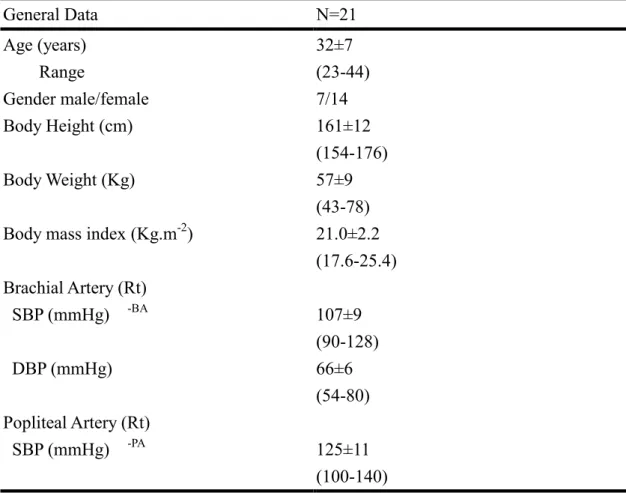
Twenty-one subjects participated in the study (fourteen female and seven male), mean age (32 years), blood pressure and PA/BA index were within normal limits ( Table 1 ).
Hemodynamic and vascular endothelial functions physiologic compression test was associated with a significant increase in the resting brachial artery diameter, resting
peak blood flow (PBF), heart rate, and total limb flow product (TLFP). The similar trend was also observed in the popliteal artery. But heart rate was unchanged. The percent changes of PBF and TLFP under PCT were also significantly
different between BA and PA groups (p<0.01) (Table 2).
The PBF and TLFP after the cuff release during PCT exams were significantly
increased not only in BA but also in PA. The basal vessel diameter in both BA and PA was different, 2.71±0.45 mm and 3.55±0.71 mm, respectively. On the contrary, basal TLFP in both BA and PA was approximately the same, 3.07±2.01 liter/min2 and 3.04±2.36 liter/min2, respectively. In terms of endothelial function, however, the percentage increase in FMD, FIRH was significantly higher in BA than in PA as shown in Table 2.
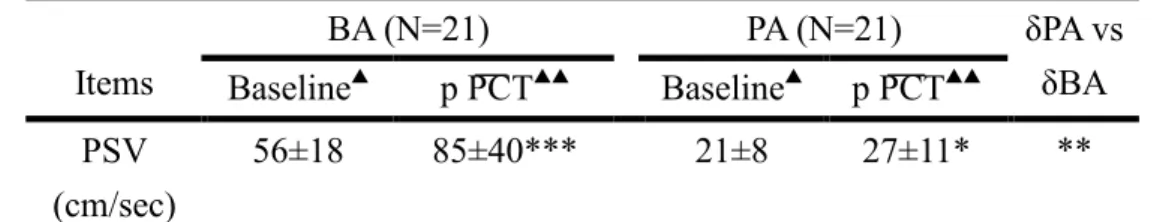
Hemodynamic alternations post PCT between BA and PA groups
Baseline hemodynamic pattern regarding PSV, PDV, MN, AT, S/D,PI and RI was obviously different between PA and RA groups (Table 3). Better hemodynamic
responses were highly observed in BA than in PA as shown in Table 3. The significant increase of PSV, PDV and MN post PCT were found in the BA group; while only blunted responses was noted in the PA group. The significant differences between PA and RA groups as to hemodynamic changes were noted in Table 3.
Furthermore, S/P ratio and PI post PCT were significantly reduced in the BA group in contrast to the PA group (p<0.01). Both RI was lower than that of baseline level. The whole hemodynamic changes were illustrated in Table 3.
PCT safety and adverse reactions
All healthy subjects tolerated the PCT well. Sometimes, local tightness and redness were complained as well as numbness sensation. Four of 21 subjects (19%) suffered from minor adverse reactions. During the PCT, the heart rate was relatively
unchanged when the blood pressure cuff was inflated or deflated.
Discussion
The vascular endothelium is involved in the control of vascular tone and homeostasis and exerts regulatory influences on vascular remodeling1-4. A large body of data has accumulated to indicate that endothelial dysfunction (ED) is associated with most of the known risk factors for cardiovascular (CV) disease1,4-6 and may constitute a contributing cause of atherosclerosis1-6. Many investigators have shown that endothelial dysfunction is related to the pathogenesis of coronary artery disease (CAD)1,6-8. Many studies have shown that impaired endothelial function (EF) exists early in the development of atherosclerosis, before the appearance of visible
lesions13,14, and in numerous conditions associated with an increased risk for CV disease, including hypertension, hypercholesterolemia, cigarette smoking, diabetes mellitus, and estrogen deficiency in postmenopausal women1,2,10-15. Since Takasi et
al first reported high correlation value between brachial artery (BA) EF and coronary artery (CA) EF suggesting flow mediated dilation (FMD) in BA could well serve as an index of dilation of CA7. Thus, EF may be referred to as systemic affair9. What does this means in the long-term follow-up regarding the prevention of any CV disease or modifying risk factors? Therefore, it is very interesting for us to search for EF of brachial artery and popliteal artery (PA) simultaneously in adult healthy
volunteer populations. Then, another question should be raised, "What is the
difference between BA and PA in terms of EF and hemodynamic changes post PCT?"
As far as we know, that question has not been addressed anywhere simultaneously in the world-wide literature. Thus, the first aim of this study was to detect whether upper and lower limb EF is different or not in addition to hemodynamic changes. Second, another purpose was to establish the normal data value of general healthy adult subjects in oriental volunteer population.
Current study vs previous studies
The principle findings of this study are (1) vascular EFs are better observed in BA rather than that of PA; in other words, impairment of PCT induced FMD may occur first in the lower body artery (i, e; PA ) but not in the upper body artery (i, e; BA), which may suggest that human atherosclerosis may first occur in the same way; (2) according to hemodynamic curves and responses, there are good reasons to assess better EF and hemodynamic BA responses were observed in contrast to the PA group (Table 3). It was well established that vascular endothelium performs a number of regular activities that maintain vascular structures and functions, including vascular tone, growth, hemostasis, inflammation, and redox state15-17. The imbalance between NO and angiotensin II activation associated with endothelial dysfunction (ED) and risk factors for atherosclerosis causes oxidative stress, which results from excessive production of oxygen free radicals and subsequent catabolism of NO1,16.
Increased product of oxygen free radicals counteracts the effect of NO, stimulates expression of adhesion molecules, and promotes adhesion of leukocytes to the endothelium1,6,16,17. These actions cause an vascular disease1,6,16,17. Stary et al reported ED underlies many stages in the progression of atherosclerosis from earliest onset to the lesion that result in CAD8. ED also is present in many risk factors or any oxidative stress conditions8,15. Given the key role of EF in any CV disorders, it sounds good approach to utilize a PCT that has direct check on evaluating EF and hemodynamic changes in both BA and PA groups. Thus, our preliminary results may be expected to answer important questions as to human atherosclerosis progression and may help further define the exact roles of both EFs in the future clinical practice.
Hemodynamic comparisons between BA and PA groups after PCT, all PSV (peak systolic velocity), PDV (peak diastolic velocity), together with MN (mean velocity)
were significantly increased in BA group; while these parameters only showed mild elevation in PA group. Significant differences of both hemodynamic alternations were shown in Table 3. Both acceleration time (AT) was reduced after PCT test. These quantitative measurements of different parameters increases the precision of the hemodynamic informations18. Different indices have been developed to measure the flow pulses18.
Among these, the pulsatility index (PI), in particularly, has gained widespread acceptance, following Gosling and King18,19. For this calculation, the height between the positive systolic peak and the negative diastolic backflow is measured, and this quantity is divided by the average flow velocity (MN)18,19. Thus, the advantage of PI lies in the fact that it is relatively independent of the angle between the probe and the vascular axis18-20. This is so because a potential error defects both the numerator and the denominator to the same degree18-20. For the most normal assessment, an index of around 5 indicates a normal value18-20. Thus, in general, BA group almost showed the normal findings in healthy adult population. On the contrary, PA value was below the normal status, which may suggest that early atherosclerotic lesion develop in the lower human body that results in slight to mild impairment of NO-dependent vasodilation as illustrated in Table 3. In vitro studies have shown that the endothelial response to vascular injury is dependent on the production of nitric oxide1,6. Generally speaking, PI was reduced after PCT test in normal BA
hemodynamic curve without delay; while PI was paradoxically increased slightly in the PA group. The latter findings may suggest that human being having suffered from atherosclerosis may first originate from the lower part artery. The observational findings still warrant large-scale, prospective survey for further confirmations.
Moreover, Cober et al. (1986) and Scharf et al (1988), examined, both in vitro and in vivo, the PI, the RI (resistance index), and the systolic half-life (SHL) or S/D ratio in relation to different degrees of luminal stenosis and varying peripheral
resistances18,21,22. To the best of our knowledge, we first demonstrated that RI would be reduced not only in the BA but also in the PA post PCT test. Only BA showed the obvious reduction, which may reflect no atherosclerotic lesion in BA system at all. In contrast, early atherosclerotic lesion in PA system is expected to exist, in which EF reveal early impairment sign and obtundated hemodynamic changes before visible atheromatous plague was well established18-24. Thus, these examinations are of very great importance to detect any early pathological cardiovascular functional impairment status. Since even in healthy individuals, a hyperemic reaction, i.e, a flow velocity increase, especially in the diastolic component, can be observed after exercise18-22. According to Fronek et al, it amounts on average to 226% after a four minutes suprasystolic compression18,23. In our healthy
population study, BA achieved up to 269%, while PA only attained up to 164%. Thus,
"Better EF, Less atherosclerotic plaque burden" concept may be clarified based on our observational study.
Study limitations
Although our study is prospective, the sample size is still too small to draw any absolute conclusions. We need more data in the near future to establish true efficacy and to build up normal data bank informations. Establishment of EF in relationship with atherosclerotic burden and related luminal stenosis will be the next step to research the human atherosclerosis progression and regression regarding risk factor modifications and aging as well as hypertension and diabetics.
Conclusion
The present study demonstrated for the first time, to the best of our knowledge, that there are different responses in the endothelial functions between the RA and PA groups in adult healthy population, which maybe associated with the natural human atherosclerosis progression.
In further, endothelial function is an essential part of any cardiovascular disorder, and may reflect human vascular characteristics. Brachial artery EF may show what kind of vascular function in upper part of human body is; while popliteal artery EF may reveal the earliest sign of general vascular disorder of human beings. General speaking, EF and hemodynamic parameters in BA are better than those of PA, in which suggest that human atherosclerosis progression originate from the lower part artery (below heart). Here, we may raise the new clinical concepts as follows: "Better EF, less AS burden" for future challenges. Thus, we may have to check both upper and lower limbs EF simultaneously and balance with our own's eyes and multiple risk factors judgements. EF as well as hemodynamic curves alternations by their nature, do not follow the whims of previous CV exams, for they are based on the traditions.
EF exams maybe furnished with elegant modern L-arginine-nitric oxide pathway concept to demonstrate their distinguished intrinsic value for any cardiovascular risk evaluations and managements in the field of molecular vascular biology in the near future.
References
1.Cooke JP. Therapeutic interventions in endothelial dysfunction: endothelium as a target organ. Clin Cardiol 1997; 20: Sup II-45-51.
2.Cooke JP, Dzau VJ. Derangements of the nitric oxide synthase pathway, L-arginine, and cardiovascular diseases. Circulation 1997; 96: 379-82.
3.Furchgott RF, Zawadzki JV. The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature 1980; 288: 373-6.
4.Mike Lin. L-arginine-NO pathways: from bench to bedside. J Intern Med Taiwan 2002; 13: 51-78
5.Woo KS, Chook P, Lolin YI, et al. Hyperhomocysteinemia is a risk factor for arterial endothelial dysfunction in humans. Circulation 1997; 96: 2542-4.
6.Mike Lin. New preventive concepts of cardiovascular disease. J Intern Med Taiwan 2001; 12: 62-78.
7.Takasi B, Uehata A, Akima T, et al. Endothelium dependent flow mediated vs vasodilation in coronary and brachial arteries in suspected coronary artery disease.
Am J Cardiol 1998; 82: 1535-9.
8.Stary HC, Chandler AB, Dinsmore RE, et al. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis: report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation 1995; 92: 1355-74.
9.Conti CR. Is endothelial function or dysfunction a systemic affair? Eur Heart J 2000;
21: 10-1.
10.Celermajer DS, Sorenser KE, Gooch VM, et al. Non-invasive detection of
endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 1992;
340: 1111-5.
11.Neunteufl T, Priglinger U, Heher S, et al. Effects of vitamine E on chronic and acute endothelial dysfunction in smokers. J Am Coll Cardiol 2000; 35: 277-83.
12.Agewall S, Wright S, Doughty RN, et al. Does a glass of red wine improve the endothelial function? Eur Heart J 2000; 1: 74-8.
13.Celermajer DS, Sorensen KE, Spiegelhalter DJ, et al. Aging is associated with endothelial dysfunction in healthy men years before the age-related decline in women.
J Am Coll Cardiol 1994; 24: 471-6.
14.Celermajor DS, Sorensen KE, Gooch VM, et al. Non-invasive detection of
endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 1992;
340: 1111-5.
15.Polark JF. Peripheral arterial disease. In: Polark JF, eds. Peripheral vascular sonography-a practical guide. 1st ed. Baltimore, Maryland; Willians and Wilkins-A Weverlry Co., 1992; 7: 247-302.
16.Blum A, Hathaway L, Mincemoyer R, et al. Effects of oral L-arginine on endothelium-dependent vasodilation and markers of inflammation in healthy postmenopausal women. J Am Coll Cardiol 2000; 35: 271-6.
17.Leyva F, Rauchhaus M, Anker SD, et al. Non-invasive assessment of vascular function: paradoxical vascular response to intravenous glucose in coronary heart disease. Eur Heart J 2000; 21: 39-44.
18.Hennerici M, Neuerburg-Heusler D. Peripheral arteries. In: Hennerici M,
Neuerburg-Heusler D, Karasch T, et al, eds. Vascular Diagnosis with Ultrasound. 1st ed. Thieme, Stuttgart, New York; Thieme Medical Publishers; 1998; 5: 133-87.
19.Gooding GA, Perez WS, Rapp JH, Krupski WC. Lower-extremity vascular grafts placed for peripheral vascular disease: prospective evaluation with duplex Doppler sonography. Radiology 1991; 180: 379-86.
20.Hatsukami TS, Primozich J, Zierler E, Strandness JDE. Color doppler
characteristics in normal extremity artery. Ultrasound Med Biol 1992; 18: 167-72.
21.Cossman DV, Ellison JE, Wagner WH, et al. Comparison of contrast arteriography to arterial mapping with color-flow duplex imaging in the lower entremities. J Vase Surg 1989; 10: 522-9.
22.Scharf R, Cobet U, Millner R. Die Wertigkeit von
Ultraschall-Doppler-Pulskurveen-Parametern bei der Beurteilung stenotischer ArterienerKranKungen. Ultraschall 1988; 9: 67-71.
23.Fronek A, Coel M, Bernstein EF. The importance of combined multisegmental pressure and Doppler flow velocity studies in the diagnosis of peripheral arterial occlusive disease. Surgery 1978; 84: 840-7.
24.Woo KS, Chook P, Lolin YI, et al. Folic acid improves arterial endothelial function in adults with hyperchomocysteinemia. J Am Coll Cardiol 1999; 34: 2002-6.
Table 1. Baseline Characteristics of Healthy Subjects
General Data N=21
Age (years) Range
Gender male/female Body Height (cm)
Body Weight (Kg)
Body mass index (Kg.m-2)
Brachial Artery (Rt) SBP (mmHg) -BA
DBP (mmHg)
Popliteal Artery (Rt) SBP (mmHg) -PA
32±7 (23-44) 7/14 161±12 (154-176) 57±9 (43-78) 21.0±2.2 (17.6-25.4)
107±9 (90-128) 66±6 (54-80)
125±11 (100-140)
DBP (mmHg)
PA/BA Index
Heart rate (beats/min)
77±8 (62-90) 1.17±0.09 (1.03-1.43) 70±8 (56-85) Abbreviations: SBP= systolic blood pressure;
DBP= diastolic blood pressure.
Table 2. Hemodynamic and Vascular Parameters before and after PCT in Healthy Subjects
BA (N=21) PA (N=21)
Items
Baseline p PCT Baseline p PCT δPA
vs δBA (A)Basic Data
Heart rate (HR, beats/min)
70±8 72±8* 71±8 71±8 NS
Vessel diameter (mm)
2.71±0.45 3.20±0.48** 3.55±0.71 4.06±0.99** NS
Peak blood flow (PBF, ml/min)
44.3±32.5 102.9±80.5*** 41.9±30.3 61.5±46.3** **
Total limb flow product (TLFP)
3.07±2.01 7.19±4.98*** 3.04±2.36 4.52±3.67** **
(HR×PBF, liter/min2) (B)Vascular Endothelial Functions
Flow Increase during reactive hyperemia (%) (FIRH)
269±136 (%) 164±97% **
Flow-mediated
Dilation (%) (FMD)
18.1±2.9% 14.0±3.2% *
BA: brachial artery; PA: popliteal artery; p PCT: post physiological compression test; *p≦0.05; **p 0.01; ***P 0.001≦ ≦ ;
NS: not-significant
Table 3. Comparisons of Hemodynamic Changes of BA and PA
BA (N=21) PA (N=21)
Items Baseline▲ p PCT▲▲ Baseline▲ p PCT▲▲
δPA vs δBA PSV
(cm/sec)
56±18 85±40*** 21±8 27±11* **
PDV (cm/sec)
5.8±5.9 14.8±14.5** 2.4±1.8 3.5±2.2* *
MNV (cm/sec)
12.9±7.5 28.6±17.3** 4.7±2.2 6.0±2.6* **
AT (sec) 0.06±0.01 0.07±0.02 0.09±0.04 0.10±0.04 NS S/D (ratio) 29.5±26.8 21.4±32.2** 13.7±9.9 12.7±10.6 **
PI (unit) 6.3±6.1 4.8±5.4* 3.2±1.6 3.4±2.1 **
RI (unit) 0.89±0.11 0.83±0.12* 0.87±0.09 0.85±0.12 * PSV= peak systolic velocity; PDV= peak diastolic velocity; MNV= mean velocity; RI= resistance index.
AT= required time interval from nidir to peak flow regarding peak vessel flow curve; PI= pulsability index.
Baseline▲ and p PCT▲▲ parameters between BA & PA were quite different significantly.
PSV= peak systolic velocity; PDV= peak diastolic velocity; MNV= mean velocity;
RI= resistance index.
AT= required time interval from nidir to peak flow regarding peak vessel flow curve;
PI= pulsability index.
Baseline▲ and p PCT▲▲ parameters between BA & PA were quite different significantly.
評估正常人上 下肢之血管動力學暨內皮功能
林廷燦 謝凱生* 林少琳** 姜洪霆** 郭憲文*** 林世崇****
屏東國仁醫院內科部/高雄聯合門診中心暨高雄義守大學
*高雄榮總小兒部/國立陽明大學 **高雄榮總內科部/國立陽明大學
***中國醫藥學院公共衛生學系暨公研所 ****台南郭綜合醫院內科部
摘 要
血管內皮功能失常在國人心臟血管疾病以及危險因子當中彼彼皆是。而其中一氧 化氮扮演相當重要的角色。對於精氨酸--一氧化氮系統之缺陷將導致眾多血管 內皮系統功能失常。然而在正常健康族群中國人之上下肢血管功能如何?以及內 皮功能變化仍是有待探討之熱門話題。因此本篇前瞻性研究旨在探討健康正常之
國人上下肢血管功能以及生理性加壓後血流動力學之變化。其中並探討上下肢為 何不同之處。此外內皮功能與動脈硬化關係之探討仍有待釐清。
使用高頻之血管超音波來測量血流以及肱動脈血管以及膕動脈擴張程度。生理加 壓方法如下:右前臂/右下肢使用 250 毫米汞柱加壓 5 分鐘,然後再釋放。同時
評估血流動力學之變化以及測量血管內皮功能。所有測試者皆是45 歲以下年青
年至中年健康人自願測試者。無任何心臟血管疾病危險因子。所有測試者血壓、
心律、血脂皆屬正常。我們先測量右上臂,經過5 分鐘休息後,再測量右下肢血
流動力學變化及內皮功能。
加壓生理試驗後在肱動脈部份,尖峰血流量從44.3±32.5 毫升/每分鐘上昇至
102.9±80.5 毫升 每分鐘(p<0.001)。而在膕動脈僅由 41.9±30.3 上昇至 61.5±46.3 毫升/每分鐘。反應性充血後血流量增加幅度(FIRA)於肱動脈為 269±136﹪,但是
在膕動脈僅有164±97﹪,兩組明顯有差距存在(p<0.01)。而整體充血反應亦呈現
類似之效果。若以同樣試驗比較尖峰血管擴張程度(FMD)而言:肱動脈為 18.1±2.9
﹪,明顯優於膕動脈為14.0±3.2﹪(p<0.05)。經過生理試驗後,肱動脈尖峰收縮
血流速度為85±40CM/sec,而膕動脈為 27±11CM/sec;明顯有差距存在(p<0.01)。
而在尖峰舒張血流速度也呈現相同之結果。而血管阻力指數(RI)暨脈動指數(PI) 在生理加壓試驗後肱動脈會明顯減低(P<0.05)但膕動脈不明顯。因此純就正常人 血管生理加壓試驗而言,肱動脈反應皆比膕動脈來的好。
正常人經過上 下肢血管生理加壓試驗後,肱/膕動脈皆會明顯血流增加、血管擴 張。血流動力學表現肱動脈明顯優於膕動脈。這些表現或許可間接證明血管內皮 功能失常是從身體下部開始(動脈硬化從下腹部主動脈以及下肢開始)。無論如 何,吾人之內皮功能暨血流表現,以健康年青 中年人角度而言,肱動脈血流表 現暨內皮功能的確優於膕動脈。簡言之,人類上 下肢血管內皮功能是不同的。
關於內皮功能失常是心血管疾病預測之一項重要指標。同時監測上下肢血管內皮 功能或許能提供臨床上早期心血管疾病危險因子之控制及袪除之另一種功能性 監測指標。