Epidemiology of Measles in Taiwan: Dynamics of Transmission and Timeliness of Reporting during an Epidemic in 1988-9
Author(s): M. S. Lee, C. C. King, C. J. Chen, S. Y. Yang, M. S. Ho
Source: Epidemiology and Infection, Vol. 114, No. 2 (Apr., 1995), pp. 345-359 Published by: Cambridge University Press
Stable URL: http://www.jstor.org/stable/3864248 Accessed: 22/04/2009 02:17
Your use of the JSTOR archive indicates your acceptance of JSTOR's Terms and Conditions of Use, available at
http://www.jstor.org/page/info/about/policies/terms.jsp. JSTOR's Terms and Conditions of Use provides, in part, that unless you have obtained prior permission, you may not download an entire issue of a journal or multiple copies of articles, and you may use content in the JSTOR archive only for your personal, non-commercial use.
Please contact the publisher regarding any further use of this work. Publisher contact information may be obtained at
http://www.jstor.org/action/showPublisher?publisherCode=cup.
Each copy of any part of a JSTOR transmission must contain the same copyright notice that appears on the screen or printed page of such transmission.
JSTOR is a not-for-profit organization founded in 1995 to build trusted digital archives for scholarship. We work with the scholarly community to preserve their work and the materials they rely upon, and to build a common research platform that promotes the discovery and use of these resources. For more information about JSTOR, please contact support@jstor.org.
Cambridge University Press is collaborating with JSTOR to digitize, preserve and extend access to Epidemiology and Infection.
Copyright ? 1995 Cambridge University Press
Epidemiology of measles in Taiwan: dynamics of transmission and
timeliness of reporting during an epidemic in 1988-9
M. S. LEE1, C. C. KING1*, C. J. CHEN1, S. Y. YANG2 AND M. S. HO3 Institute of Epidemiology, National Taiwan University, Taipei, Taiwan,
Republic of China (ROC)
2Bureau of Communicable Diseases Control, Department of Health, Taiwan, ROC 3Institute of Biomedical Sciences, Academia Sinica, Taipei, Taiwan, ROC
(Accepted 27 October 1994) SUMMARY
We analysed nation-wide reported measles cases during the 1988-9 epidemic and found that longer duration and wider spread were two major characteristics of the outbreak. All the 22 county/city index cases were reported with a delay of
> 4 days and 64% were aged 5-14 years. This epidemic occurred mainly among 5-14-year-old school-children (59%), infants under 1 year (19%), and pre-school children (18%). The overall attack rate was 0-63 cases per 10000 population, with the highest attack rate (7-4 cases per 10000 population) occurring in infants. Among 280 confirmed cases < 15 months of age, 9-month-old infants (42 cases) had a higher risk of measles and peaked at 10 months (49 cases). This epidemic started in March 1988 among 5-9-year-old children in the northern suburban area, then spread to Taipei City and neighbouring counties or cities. It continued to spread from the northern to southern and western areas during the summer vacation and New Year holidays. Multiple logistic regression analysis showed that the delay of measles reporting was strongly associated with the cases infected early in the epidemic (OR = 6-9, P < 0'001) and reported from teaching hospitals (OR = 2-6, P < 0-001). The reappearance of high attack rates among 5-9-year-old children in the 1985 and 1988-9 measles epidemics in Taiwan indicated the persistence of pockets of susceptible individuals even after mass immunization.
INTRODUCTION
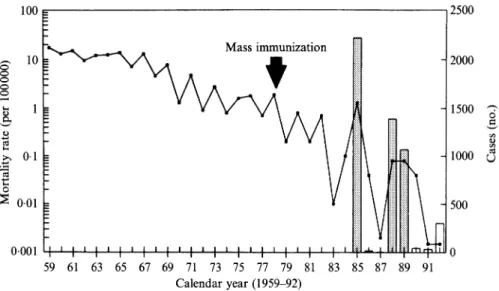
Measles in Taiwan was very widespread, with epidemics occurring every 2 years, before mass immunization programmes were implemented in 1978 [1]. Since then, measles mortality has decreased significantly and only one fatal case was reported in 1983. However, the virus persists in Taiwan and measles outbreaks continue to occur periodically (Fig. 1) [2]. Live attenuated measles vaccine was introduced to Taiwan in 1968. Mass immunization programmes with one dose of vaccine for all 9-36-month-old infants and children were instituted in the capital city (Taipei) in 1977, and the programme was extended to the whole Taiwan area for all children * Author for correspondence: Dr C. C. King, Institute of Epidemiology, National Taiwan University, Rm. 1549, No. 1 Jen-Ai Road Sec. 1, Taipei, Taiwan 100, Republic of China.
346
M. S.
LEE AND OTHERS 100 = 2500 Mass immunization cS 10_ '\n/\ . t ; -2000 Q 1 - /J \ | - 1500 . 01 I -100 0.01 500 0-001 I j I t I I I I ' | t ' I ' I t I'iL 1 0 f lO 59 61 63 65 67 69 71 73 75 77 79 81 83 85 87 89 91 Calendar year (1959-92)Fig. 1. The annual number of reported measles cases and measles mortality rates among individuals 0-19 years old in Taiwan, 1959-92. Measles became a reportable disease in 1985. Mortality rates were calculated from the number of individuals 0-19 years old as a denominator, because only 3 fatal cases occurred among adults > 19 years of age during 1959-89.-, Mortality rate; "g, reported cases.
15-21 months of age in 1978. The recommended ages for vaccination have been changed several times since 1978: (a) 2 doses at 9 and 15 months of age in May 1984; (b) one dose at 12 months in January 1988 together with a 2-dose strategy if measles epidemics occurred; and (c) 2 doses at 9 and 15 months of age in May 1988 after the island-wide measles outbreak. These frequent changes have confused many local health personnel and parents about the optimal age of measles immunization.
Recent measles epidemics in Taiwan occurred in 1985, 1988 and 1989 with 2219, 1386 and 1060 reported cases, respectively. The 1985 epidemic resulted in 97 deaths (mortality rate = 1-70 deaths per 100000 persons under age 15 years), whereas the 1988-9 epidemic caused only 12 deaths [3]. The 1988 epidemic started in the northern suburban area of Taiwan in March, but health authorities did not receive any reports until April. In order to prevent measles more effectively, the Advisory Committee of Immunization Practices (ACIP) in Taiwan decided to change the measles immunization schedule to 2 doses at 9 and 15 months of age as noted above. However, reported cases continued to increase and reached 2 peaks, the first in July 1988 and the second in January 1989, with 275 and 364 reported cases, respectively.
Epidemiological data of island-wide measles cases in Taiwan over the last 40 years have not hitherto been analysed, except for mortality analyses and a few local outbreak investigations [1, 2, 4]. Moreover, the effectiveness of the measles reporting system in Taiwan has not been evaluated since this disease became reportable in 1985. Therefore, we conducted this study with the following specific aims: (1) to characterize the epidemiology of measles during its outbreak in 1988-9 in Taiwan; (2) to explore the dynamics of measles transmission and (3) to evaluate the effectiveness of the passive surveillance system for measles. Our
Epidemiology of measles in Taiwan
findings may have strategic implications for eliminating measles from Taiwan and possibly for global eradication.
MATERIALS AND METHODS Surveillance and reporting forms
Measles surveillance in Taiwan has been based on passive reporting since 1985. Physicians mail the report forms to their County or City Health Bureau. The Department of Health (DOH) receives these reports from all the local health bureaux each month. The information collected on the report form includes age, sex, date of onset and clinical manifestations. The report form for measles has been simplified twice from 1985 to 1989. New forms have excluded important information, such as immunization history, source of exposure and location of infection since 1987. In 1988-9, there were 2446 reported measles cases from which 2332 (95-3 %) forms were available for analysis.
Epidemiological analysis
Reported measles cases were classified as confirmed or suspected. A 'confirmed case' was defined as having at least one of the following three criteria: (a) serological confirmation with positive measles IgM; (b) Koplik's spots on buccal mucosa; (c) fever, a generalized maculopapular rash, and at least one of the following signs or symptoms: cough, coryza, or conjunctivitis. The third criterion is similar to that of the CDC in the United States except the duration of rash (lasting for 3 or more days) [5], because patients in Taiwan often visit physicians once only without follow up. Reported cases that did not meet any of these criteria were classified as 'suspected cases'. An index case was defined as the first reported confirmed case in each county or city. In order to explore the possible differences between confirmed and suspected cases, factors such as sex, age, hospitalization, source of reporting, stage of epidemic, and delays in reporting were compared. Only confirmed cases were used to calculate cohort-specific attack rates by different immunization strategies. Reporting sources were classified as private clinic, public health station, private hospital, public hospital, teaching hospital and others (military hospital and unknown). Three epidemic stages were defined as follows: (1) starting period (Jan.-April 1988, prior to the first peak); (2) prevalent period (May 1988-March 1989); and (3) declining period (April-Dec.
1989). The reporting delay was defined as the number of days from the date of disease onset to the date that local health bureaux received the report.
Dynamics of measles transmission
Only confirmed cases were used to explore the dynamics of measles transmission. The spatial diffusion of this epidemic was analysed by month of onset with spot maps of cities and counties. Taiwan was divided into 23 administrative districts in 1989, including 2 national cities (Taipei and Kaohsiung), 5 provincial cities and 16 counties. Taipei and Kaohsiung Cities were the economical centres of northern and southern Taiwan, respectively. Taipei City, with the highest number of confirmed cases (478), was selected to examine the spread of measles among different age groups. In addition, Taipei City and Taidung County, where obvious
M. S. LEE AND OTHERS
double peaks of measles cases appeared, were chosen to explore the difference in age distribution between the first and the second peaks.
Evaluation of measles reporting
Reporting delays were grouped as follows: 0-1 day, in compliance with DOH regulations; 2-4 days, which is a critical period for public health action to prevent the third generation of measles cases; 5-9 days and > 9 days (the incubation period of measles). All reported cases were analysed by multiple logistic regression analysis to explore factors associated with the timeliness of reporting, such as hospitalization, sources of reporting, and stages of epidemic. For the multivariate model, reporting delays were regrouped into: 0-9 days and > 9 days.
Statistical analysis
The associations between two categorical variables were tested for statistical significance by chi-square test, Mantel-Haenszel chi-square test for trend, or Fisher's exact test for the number of any category < 5 using SAS software. The multiple logistic regression with categorical variables was analysed with Categorical Model (CATMOD) in SAS software.
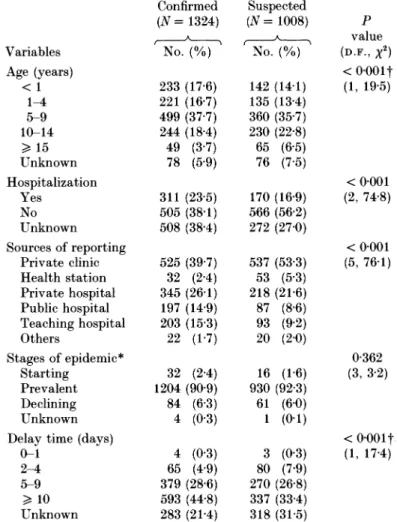
RESULTS Comparison between confirmed and suspected cases
Among 2332 available reported cases, 1324 (57%) were classified as confirmed cases by the presence of Koplik's spots (1016, 77%), CDC-compatible clinical criteria (273, 20%) and measles specific IgM antibody (35, 3%). Compared with the suspected measles cases, the confirmed measles cases had higher percentage of children under 10 years old (72 vs 63 %, P < 0-001, Mantel-Haenszel chi-square test), a higher hospitalization rate (23-4 vs 17%, P < 0-001, chi-square test) and a higher percentage of reporting delay > 9 days (44-8 vs 33'4%, P < 0001, Mantel-Haenszel chi-square test). In addition, the proportions of confirmed cases that were reported from private, public and teaching hospitals were 26-1, 14-9 and 153 % respectively; significantly higher than those of suspected cases (21-6, 8-6 and 9'2 %) (P < 0-001, chi-square test). In total, private clinics accounted for the majority (46%) of reported cases. Confirmed and suspected cases did not differ in sex (P = 0-83) and stages of epidemic (P = 0-36, chi-square test) (Table 1). Index case
The 22 index cases were mostly male (N = 13, 59%), children aged 5-14 years (N = 14, 64 %) and reported from private clinics (N = 7, 32 %) or public hospitals (N = 7, 32%). In addition, all of the index cases were reported to local health bureaux with a delay > 4 days (range = 6-159 days, median = 10 days, mode = 9 days, mean = 35 days), which is a critical period for prevention of the third generation of cases.
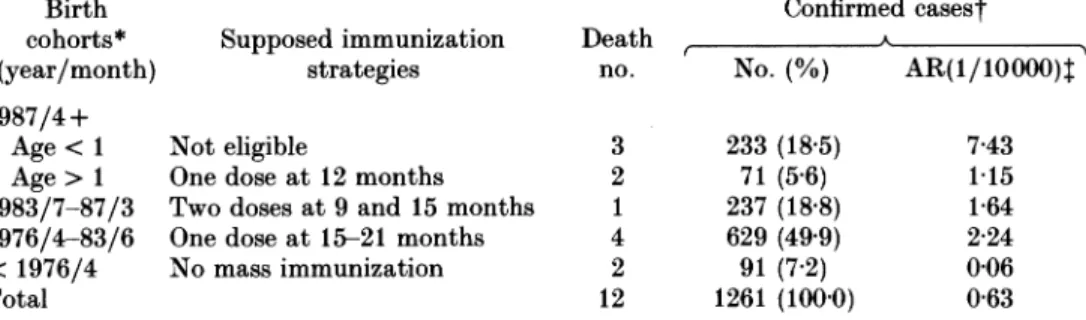
Attack rates
The overall attack rate was 0-63 cases/10000 people, with the highest cohort- specific attack rate (7-43 cases/10000 people) occurring among infants < 1 year of
Epidemiology of measles in Taiwan
Table 1. Comparison of epidemiological characteristics and reporting conditions
between confirmed and suspected reported measles cases in Taiwan, 1988-9* Confirmed Suspected
(N= 1324) (N= 1008) P
^ A value
Variables No. (%) No. (%) (D.F., X2)
Age (years) < 0-001t < 1 233 (17-6) 142 (14-1) (1, 19-5) 1-4 221 (16-7) 135 (13-4) 5-9 499 (37-7) 360 (35-7) 10-14 244 (18-4) 230 (22-8) > 15 49 (3'7) 65 (6-5) Unknown 78 (5-9) 76 (7-5) Hospitalization < 0'001 Yes 311 (23-5) 170 (16-9) (2, 74-8) No 505 (38-1) 566 (56-2) Unknown 508 (38-4) 272 (27-0) Sources of reporting < 0-001 Private clinic 525 (39-7) 537 (53-3) (5, 76-1) Health station 32 (2-4) 53 (5-3) Private hospital 345 (26-1) 218 (21-6) Public hospital 197 (14-9) 87 (8-6) Teaching hospital 203 (15-3) 93 (9-2) Others 22 (1-7) 20 (2-0) Stages of epidemic* 0-362 Starting 32 (2-4) 16 (1-6) (3, 3-2) Prevalent 1204 (90-9) 930 (92-3) Declining 84 (6-3) 61 (6-0) Unknown 4 (0-3) 1 (0 1)
Delay time (days) < 0-001t
0-1 4 (0-3) 3 (0-3) (1, 17-4) 2-4 65 (4-9) 80 (7-9) 5-9 379 (28-6) 270 (26-8) > 10 593 (44-8) 337 (33-4) Unknown 283 (21-4) 318 (31-5) *
Stages of epidemic were classified as follows: (1) starting period (Jan.-April 1988, prior to the rise of the first peak); (2) prevalent period (May 1988-March 1989) and (3) declining period (April-Dec. 1989).
t Mantel-Haenszel chi-square test; D.F., degrees of freedom.
age. The other cohort-specific attack rates were 2-24 cases/10000 people among children born April 1976-June 1983 (with immunization strategy of one dose of measles vaccine at 15-21 months of age) and 1-64 cases/10000 people among children born July 1983-March 1987 (with immunization strategy of 2 doses of measles vaccine at 9 and 15 months of age). The cohort born before mass immunization had the lowest attack rate (0'06 cases/10000 people) during this epidemic (Table 2).
Age distribution
Among the 1246 confirmed cases with known age, 40% (N = 499) occurred among 5-9-year-old school-children, 19-6% (N= 244) in 10-14 year, 18-7%
350 M. S. LEE AND OTHERS
Table 2. Cohort-specific attack rates of confirmed measles and the number of fatal cases by different immunization strategies during the 1988-9 measles epidemic in Taiwan
Birth Confirmed casest
cohorts* Supposed immunization Death A
(year/month) strategies no. No. (%) AR(1/10000)t 1987/4+
Age < 1 Not eligible 3 233 (18-5) 7-43
Age > 1 One dose at 12 months 2 71 (5-6) 1-15 1983/7-87/3 Two doses at 9 and 15 months 1 237 (18-8) 1-64 1976/4-83/6 One dose at 15-21 months 4 629 (49-9) 2-24 < 1976/4 No mass immunization 2 91 (7-2) 0-06
Total 12 1261 (100-0) 0-63
* Sixty-three confirmed measles cases with unknown birthday were not included for analysis. t Only the confirmed cases were used to calculate the cohort-specific attack rates (AR). t The cohort-specific population was estimated by the statistics in Dec. 1988.
(N = 233) in infants under < 1 year old and 17-7 % (N = 221) in 1-4-year-old pre- school children (Table 1). The age distribution of 12 fatal cases was 3 in infants < 1 year old, 3 in 1-4 years, 2 in 5-9 years, 3 in 10-14 years and 1 in 15-19 years. The youngest confirmed case was a newborn infant. The oldest one was 66 years old. Among the 280 confirmed cases < 15 months of age, measles cases rose significantly at 9 months old (N = 42) and peaked at 10 months old (N = 49). Their distribution was 9-3 % in 0-6 months, 28-9 % in 7-9 months, 45 % in 10-12 months and 16-8% in 13-15 months.
Dynamics of transmission
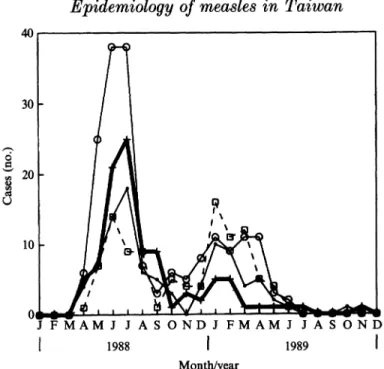
Two peaks appeared during the 1988-9 measles epidemic. The first confirmed case was a 10-year-old girl who developed measles on 12 March 1988 in Taipei County. This case was not reported to the local health bureau until 10 April 1988. Since then, the reported number rose dramatically and reached the first peak of 185 confirmed cases in June and July. Although the reported cases gradually decreased after July, the epidemic recurred in December 1988 and produced a second, higher peak of 187 confirmed cases in January 1989. Reported cases waned gradually over the next 5 months (the number of cases were 112, 67, 39, 18 and 15 in each following month of Feb.-June). After June 1989, only sporadic cases were reported (Fig. 2).
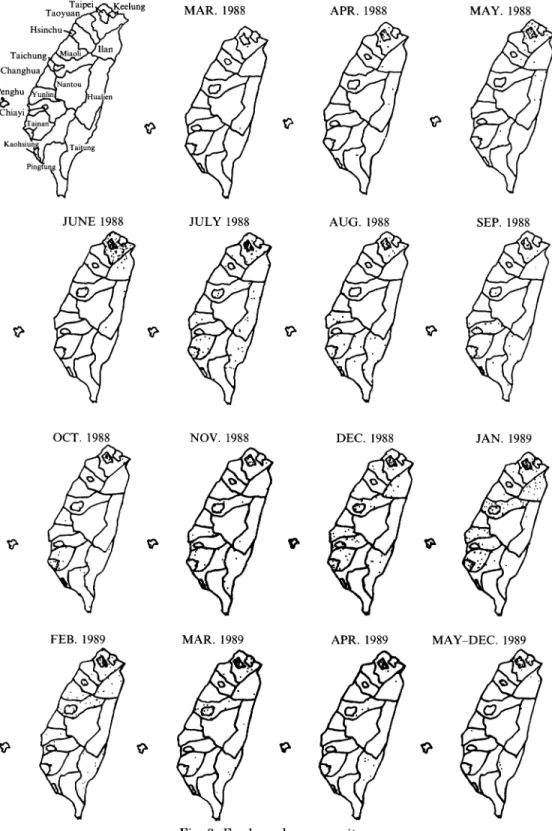
This island-wide epidemic spread geographically by a combination of neigh- bourhood and age-related transmission. The outbreak first emerged in the northern suburban area (Taipei County) in March 1988. It then spread to Taipei City (the capital of Taiwan, which has a population density of 9868 persons/km2) in April and diffused concurrently to the neighbouring counties/cities located in eastern (Ilan, 209 persons/km2) and northern Taiwan (Keelung, 2626 persons/ km2). Ilan County and Keelung City reported their first confirmed cases in April and May respectively, whereas the southeasternmost, rural county (Taidung, 74 persons/km2) began reporting measles cases in July. The first peak of this epidemic reached in June 1988 with 89% (164/185) of the cases reported from
Epidemiology of measles in Taiwan
200 150 - 100 - C) 50 - 0 ' ' ' I ' ' ' I IJ FMAMJ JASONDJ FMAMJ J A S OND
1 1988 1 1989 I
Date of measles onset
Fig. 2. Month distribution of reported measles during the 1988-9 epidemic in Taiwan. The school winter and summer vacations in Taiwan are in February and July-August, respectively. The 'confirmed case' was defined as having at least one of the following 3 criteria: (1) serological confirmation with positive measles IgM; (2) Koplik's spots on buccal mucosa; (3) fever, a generalized maculopapular rash, and at least one of the following signs or symptoms: cough, coryza, or conjunctivitis. [, Confirmed cases;
+, suspected cases.
Taipei City and Taipei County. The virus continued to circulate in these areas and was transmitted to the central metropolitan area (Taichung City, 4469 persons/km2) in June and the southern metropolitan areas (Tainan City, 3801 persons/km2 and Kaohsiung City, 8868 persons/km2) in July. Concurrently, measles cases mushroomed in 16 of 23 cities/counties during July 1988, the school summer vacation. After September, measles activity decreased gradually and only sporadic cases occurred in northern and southern areas. However, the disease recurred in December and reached the second peak in January 1989 in Taipei City and western counties (Fig. 3). Apparently, Taipei areas with the highest population density had measles cases from the beginning to the end of the epidemic. However, the Central Mountain Range, located longitudinally across Taiwan island, forced the virus diffused from northern to eastern, southeastern, central and finally southwestern areas. Infected individuals in Taipei and Kaohsiung Cities facilitated measles virus island-wide transmission continuously.
The dynamics of measles transmission among different age groups in Taiwan demonstrated that the disease spread from younger (5-9 years of age) to older school-children ( 10 years of age) and pre-school children (< 4 years of age) in both the urban (Taipei City) (Fig. 4) and suburban areas (Taipei County, data not shown). In addition, more cases occurred among infants (22-2%) and children older than 10 years (32-7 %) in the second wave than that of the first wave (18-4
352 Taipei ,~Keelung Taoyuan , Hsinchu s /,.. '-Y/ilan Taichung nao Changhua antou
Penghu unL ualien
Chiayi
Kaohsiun TJug
Pingtu
JUNE 1988
M. S. LEE AND OTHERS
MAR. 1988 JULY 1988 NOV. 1988 APR. 1988 AUG. 1988 DEC. 1988 APR. 1989 MAY-DEC. 1989
Fig. 3. For legend see opposite.
SEP. 1988
JAN. 1989
Epidemiology of measles in Taiwan
40,, 20 -
10- V
J FMAMJ J ASONDJ FMAMJ JASOND
1988 1 1989
Month/year
Fig. 4. Age-specific monthly distribution of reported confirmed measles in Taipei City (N= 478). Age (years): U, < 1; +, 1-4; 0, 5-9; 1, > 10.
Table 3. Age distribution of reported measles by epidemic wave in Taipei City and Taidung County during 1988-9 epidemic in Taiwan
Age distribution (years)
< 1 1-4 5-9 > 10 Total
Areas No. (%) No. (%) No. (%) No. (%) No. (%)
Taipei City* 94 (19-7) 98 (20-5) 183 (38-3) 103 (21-5) 478 (100) 1st wavet 58 (18-4) 80 (25-3) 128 (40-5) 50 (15-8) 316 (66) 2nd wavet 36 (22-2) 18 (11-1) 55 (34-0) 53 (32-7) 162 (34) Taidung Countyt 20 (25-3) 14 (17-7) 36 (45-6) 9 (11-4) 79 (100) 1st wavet 8 (20-5) 9 (23-1) 19 (48-7) 3 (7-7) 39 (49) 2nd wavet 12 (30-0) 5 (12-5) 17 (42-5) 6 (15-0) 40 (51) *
X2 = 26-7, degree of freedom = 3, P < 0-001, chi-square test.
t The epidemic waves were classified as: (1) January-November 1988 and (2) December 1988-December 1989.
t P = 0-4, Fisher's Exact Test (2-tail).
and 15-8%, respectively) in Taipei City (P < 0-001, chi-square test). Taidung County which has much lower population density also had a similar trend without statistical significance because of small sample size (P = 0'4, Fisher's Exact test) (Table 3).
Fig. 3. The geographical distribution of monthly confirmed measles case numbers during the 1988-9 measles epidemic in Taiwan. The Central Mountain Range, which occupies about half of the island, stretches north to south a distance of 205 miles, and east to west a maximum width of 50 miles. Numerous peaks rise to between 12000 and 13000 ft. Therefore, the dynamics of measles transmission in eastern Taiwan is different from the western areas.
M. S. LEE AND OT:HES
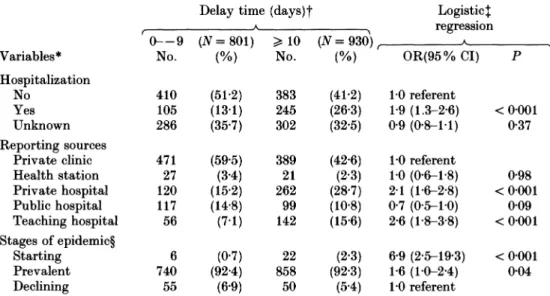
Table 4. Factors associated with delay of measles reporting during the 1988-9 measles epidemic in Taiwan
Delay time (days)t Logistic$
rA regression
(0-9 (N=801) >10 (N=930), A
Variables* No. (%) No. (%) OR(95% CI) P
Hospitalization
No 410 (51-2) 383 (41-2) 1-0 referent
Yes 105 (13-1) 245 (26-3) 1-9 (1.3-2-6) < 0-001 Unknown 286 (35-7) 302 (32-5) 0-9 (0-8-1-1) 0-37 Reporting sources
Private clinic 471 (59-5) 389 (42-6) 1-0 referent
Health station 27 (3-4) 21 (2-3) 1-0 (0-6-1-8) 0-98 Private hospital 120 (15-2) 262 (28-7) 2-1 (1-6-2-8) < 0-001 Public hospital 117 (14-8) 99 (10-8) 0-7 (0-5-1-0) 0-09 Teaching hospital 56 (7-1) 142 (15-6) 2-6 (1-8-3-8) < 0-001 Stages of epidemic? Starting 6 (0-7) 22 (2-3) 6-9 (2-5-19-3) < 0-001 Prevalent 740 (92-4) 858 (92-3) 1-6 (1-0-2-4) 0-04 Declining 55 (6-9) 50 (5-4) 1-0 referent *
Twenty-seven cases without data on medical settings were excluded.
t Six hundred and one cases without data on delay time were not analysed, including 221 (37 %) which lacked the data on disease onset, 339 (56 %) which lacked data on reporting dates by health bureaux and 41 (7 %) lacked both sets of data.
t Multiple logistic regression with the following equation: Ln(odds ratio of delay reporting) = - 155+0-63 (hospitalization = yes) -011 (hospitalization = unkown) + 0-01 (health station) + 074 (private hospital)-0-30 (public hospital) + 0-97 (teaching hospital)+ 1-93 (starting stage)+0-45 (prevalent stage).
? Stages of epidemics were classified as follows: (1) starting period (Jan.-April 1988, prior to the rise of the first peak); (2) prevalent period (May 1988-March 1989) and (3) declining period (April-Dec. 1989).
Timeliness of measles reporting
Among 1731 reported cases with documented dates of measles onset and reporting, the mean, median, mode and range of the reporting delay were 14, 10, 8 and 0-213 days, respectively. The hospitalized cases [odds ratio (OR)= 1-9, P < 0-001], private hospital (OR = 2-1, P < 0-001), teaching hospitals (OR = 2-6, P < 0001), the starting stage (OR = 6-9, P < 0001) and prevalent stage (OR = 1'6, P = 0-04) of the epidemic had significant associations with the longer reporting delay (> 10 days) in multiple logistic regression analysis (Table 4).
DISCUSSION
Measles is a suitable model with which to explore the dynamics of transmission, the mechanism of virus circulation and for developing effective control and eradication strategies for specifically human diseases transmitted via air-borne spread [6-10]. The recent global resurgence of measles epidemics in several developed countries in 1988-91 reinforces the importance of timely measles surveillance and the need to investigate the dynamics of measles transmission
354
Epidemiology of measles in Taiwan
after mass immunization [11-15]. This study illustrates a longer duration of epidemics in Taiwan compared to the pre-vaccination era. The spread of measles in Taiwan started from a suburban area (Taipei County) to a metropolitan city (Taipei City), and then spread to other regional cities and rural areas. It also showed that the epidemic spread from younger (5-9 years of age) to older school- children and then to pre-school children. In addition, the delay in reporting of index cases, the fact that about 10% of primary school-children remained susceptible in spite of a mass immunization programme and past epidemics [14, 16], the low vaccine coverage (73-89%) [17], and a high attack rate among infants facilitated the longer persistence of this island-wide epidemic.
Two characteristics of measles epidemiology, seasonality and age distribution, have changed over 10 years of mass immunization in Taiwan. The peak season of measles epidemics during 1959-81 in May disappeared in the 1984-5 and 1988-9 outbreaks [1, 2]. The 1988-9 epidemic started in March after school opened in late February, similar to the findings of Fine and Clarkson in England and Wales [18]. The different peak month of June-July 1988 and January 1989 coincided with the summer vacation and New Year holidays and spread measles island-wide. Furthermore, mass immunization programmes tend to raise the age of susceptibles from preschool to school-children [19-20]. More cases appeared among 10-14- year-old children in 1988-9 (20%) than in 1976-85 (12 %) [2] and signified that the problems of a 'honeymoon period' after mass immunization occurred in Taiwan [20]. Infants had a significantly increased risk of measles infection after 9 months of age, implying the urgent need to immunize them at 9 or 6 months once a measles outbreak occurs [21]. The strategy of 2 doses of measles vaccine at 9 and 15 months during 1984-7 should theoretically reduce the attack rate among those children < 5 years of age, but low coverage rate (50%) for the second dose may still increase the overall risk of measles among this birth cohort [22]. A booster dose of measles vaccine (or MMR) among school-children to improve both individual protection and herd immunity is widely applied to many countries [23]. Its optimal age should be determined by seroepidemiological data, particularly the duration of measles neutralization antibody and the protective level. In addition, the spreading of this island-wide epidemic started from younger school- children (5-9 years of age) to older population (b 10 years old) and preschool children (< 4 years of age), consistent with our previous serosurvey in a rural community [14]. It is very likely that the high contact rate among younger school- children was associated with the initiation of the outbreak, particularly in an urban city [24]. In addition, the school holidays certainly facilitated transmission to wider areas. These findings demonstrate the urgent need to establish a school- based surveillance system, to implement school immunization requirements [25] and to investigate the possible role of declining immunity in the effective control of vaccine-preventable diseases in Taiwan.
A long duration and widespread infection were common characteristics of the 1988-9 measles epidemic in Taiwan as well as several other countries during 1988-91 [11-15]. The epidemic diffused from the northern suburban area, where 14% of population were migratory in 1989 [26], to a metropolitan city and then out to other regional cities and rural areas. Interestingly, the majority of the migratory population in Taipei County came from those areas with poor economic
356 M. S. LEE AND OTHERS
status. Cliff and colleagues also found that measles dispersed from the capital to regional centres and then to the neighbouring hinterlands in most of 16 epidemics in Iceland during 1904-74 [6]. Children from migratory families often missed their immunizations and became the 'dead-corners' of prevention and the 1989-90 measles epidemic in the United States started in such families in Los Angeles, Chicago and Houston [11]. Low vaccine coverage among migratory families was also responsible for the 1982 epidemic of poliomyelitis in Taiwan [27] and the 1989-90 outbreaks of poliomyelitis in mainland China, despite high overall immunization coverage [28]. In addition, widely distributed susceptible pockets plus high population density and frequent hometown visits during holidays may explain this longer and wider epidemic. The slow diffusion of this island-wide outbreak from suburban areas with many migratory families to other areas suggests the importance of monitoring this high risk group and the possibility of effective outbreak control if target populations could be defined immediately and be immunized in time.
Passive surveillance is often associated with delayed and low reporting [29-31]. Because measles is highly contagious and the virus is particularly communicable during catarrhal stage (about 7 days post exposure or 3 days before onset of rash) [32], an index case may cause two further generations of cases by the fourth day after onset of rash. All the index cases in this study were reported to local health bureaux with a delay > 4 days, indicating the ineffectiveness of current reporting systems in detecting outbreaks within the critical 4 day period. Delay in case reporting is also common with other infectious diseases surveillance systems such as shigellosis with a delay of 11 days, a length sufficient to generate secondary and tertiary transmission cycles [29]. Teaching hospitals had the worst reporting delay, possibly because of referral of severe cases from primary medical clinics. Here we could not differentiate the delay of measles reporting due to delay in visiting a physician from that due to a delay of reporting. However, 7 cases were reported to local health bureaux by facsimile within one day of onset of the disease. We believe that integrating the 'sentinel physician' and 'sentinel school- nurse' reporting systems with a network of facsimile could improve the timeliness of infectious diseases surveillance.
National data on disease notification are valuable for evaluating the effectiveness of control programmes and monitoring their future trends, even if such systems are incomplete [33-36]. Completeness of measles reporting in Taiwan is poor, with a physician reporting rate of 6 % and sensitivity of 4 % in rural areas [14]. In Keelung (a provincial city), none of 20 serologically-confirmed cases was reported to the health bureau [16]. However, the low reporting rate did not distort the major characteristics of this epidemic, because there were multiple sources of reporting from different types of medical institutes. Many cases were classified as 'suspected cases' due to missing medical information on the reporting forms. In addition, the fact that suspected cases were significantly older than confirmed cases (Table 1) and a rubella epidemic concurrently occurred in 1988-9 [14] so that that we used only confirmed cases for analysing epidemiologic characteristics. The low reporting rate, missing data on the reporting forms, and similar symptoms of measles and rubella indicate the need for active investigation of reported cases to collect detailed medical information, ascertain more linked cases, and conduct
Epidemiology of measles in Taiwan
serological testing that would differentiate atypical measles from other ex- anthematous diseases [37, 38].
Measles is a useful indicator with which to evaluate the effectiveness of immunization programmes. The worldwide emergence of large-scale measles epidemics in many developed countries during 1988-91 is alarming. New findings have changed our understandings of measles, including the occurrence of subclinical infection [14, 38, 39] at immunized individuals may transmit the virus [38-40], the lack of life-long immunity in certain individuals [41-42], the genetic variability of the virus [43] and the significance of air-borne transmission [44-46]. Future measles control, in Taiwan and globally, should include: (1) increasing the timeliness and completeness of surveillance, (2) prospective immunological evaluation of vaccinees, (3) reassessment of the roles of immunized and asymptomatic individuals in the dynamics of transmission, and (4) utilization of local seroepidemiological data as well as residual maternal antibody levels for optimizing age and doses of immunization programmes.
ACKNOWLEDGEMENTS
The authors sincerely appreciate Ms Shwu-Fang Chen in the Taipei City Health Bureau, Ms Shoei Tzeng in the Taiwan Provincial Health Department, Ms Lih- Shiang Wu in the Kaohsiung City Health Bureau, and the students in the Department of Public Health at the National Taiwan University for their help in collecting and coding measles reporting forms. We would also like to express our sincere gratitude to the American Bureau for Medical Advancement in China (ABMAC) and Ms Hope N. F. Phillips for their financial support in presenting this measles research at the Chinese Bioscientists 1990 Symposium in Hong Kong. We also acknowledge Dr Jean Levine at the National Institute for Occupational Safety and Health (USA) and Dr Robert T. Chen at the Centers for Disease Control and Prevention (CDC), USA for their detailed reviews of this manuscript, Dr James Chin at U.C. Berkeley (USA) for his kind supply of computer mapping program and critical review of this manuscript and Mr Min-Ho Lai at the National Quarantine Service, Taiwan, R.O.C. for his mapping assistance.
REFERENCES
1. Chen CJ, Lin TM, Yeh TL. Analysis of the secular trend and seasonal variation of measles mortality rate in Taiwan. Ann Acad Med 1984; 13: 136-41.
2. Hsu ST. Analysis of measles epidemic and vaccine efficacy: 10 years' experience in a pediatric clinic, Changhwa. Acta Pediatr Sin 1987; 28: 342-7.
3. Department of Health, Taiwan, Republic of China, 1986. Health Statistics (2): Vital statistics, 1985.
4. Gao JP, Malison MD. The epidemiology of a measles outbreak on a remote offshore island near Taiwan. Int J Epidemiol 1988; 17: 894-8.
5. Centers for Disease Control (USA). Classification of measles cases and categorization of measles elimination programs. MMWR 1983; 31: 707-11.
6. Cliff AD, Haggett P, Ord JK, Versey GR. Measles epidemic cycles in Iceland. In: Spatial diffusion, an historical geography of epidemics in an island community. Cambridge: Cambridge University Press; 1981: 55-91.
7. En'ko PD. On the course of epidemics of some infectious diseases. Int J Epidemiol 1989; 18: 749-55.
358 M. S. LEE AND OTHERS
8. Yorke JA, Nathanson N, Pianigiani G, Martin J. Seasonality and the requirements for perpetuation and eradication of viruses in populations. Am J Epidemiol 1979; 109: 103-23. 9. Anderson RM, May RM. Vaccination and herd immunity to infectious diseases. Nature
1985; 318: 323-9.
10. Anderson RM, May RM. Dynamics aspects of eradication and control. In: Infectious diseases of human: dynamics and control. Oxford: Oxford University Press, 1991: 144-54. 11. Centers for Disease Control (USA). Measles - United States, 1989 and first 20 weeks 1990.
MMWR 1990; 39: 353-63.
12. Varughese PV. Measles in Canada- 1989. Canada Disease Weekly Report 1990; 16: 6. 13. Agocs MM, Markowitz LE, Straub I, Domok I. The 1988-1989 measles epidemic in
Hungary: assessment of vaccine failure. Int J Epidemiol 1992; 21: 1007-13.
14. Lee MS, King CC, Jean JY, et al. Seroepidemiology and evaluation of passive surveillance during 1988-1989 measles outbreak in Taiwan. Int J Epidemiol 1992; 21: 1165-74. 15. Yvonne G, Paul SG. Surveillance for measles - New Zealand, 1991. MMWR 1992; 41(SS-4):
13-17.
16. Hung ML. Seroepidemiologic study of measles and rubella in Taiwan. Master thesis, Institute of Public Health, National Yang-Ming Medical College, Taiwan, ROC, 1992. 17. Department of Health (ROC). Vaccine coverage survey. Epidemiol Bull 1986; 2: 37-9,
53-5.
18. Fine PEM, Clarkson JA. Measles in England and Wales. I. An analysis of factors underlying seasonal patterns. Int J Epidemiol 1982; 11: 5-14.
19. Fine PEM, Clarkson JA. Measles in England and Wales. II. The impact of the measles vaccination program on the distribution of immunity in the population. Int J Epidemiol 1982; 11: 15-25.
20. McLean AR, Anderson RM. Measles in developing countries. Part II. The predicted impact of mass vaccination. Epidemiol Infect 1988; 100: 419-42.
21. Centers for Disease Control (USA). Measles prevention: Recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR 1989; 38(S-9): 1-18. 22. Department of Health (ROC). Investigations of immunization coverage rates of infants and
children in five cities or counties in Taiwan. Epidemiol Bull 1993; 9: 27-33.
23. Tulchinsky TH, Ginsberg GM, Abed Y, et al. Measles control in developing and developed countries: the case for a two-dose policy. Bull WHO 1993; 71: 93-103.
24. Anderson RM, May RM. Age-related changes in the rate of disease transmission: implications for the design of vaccination program. J Hyg 1985; 94: 365-436.
25. Centers for Disease Control (USA). Measles and school immunization requirements - United States. MMWR 1978; 27: 303-4.
26. Ministry of the Interior (ROC). Demographic fact book, Taiwan-Fukien, Republic of China. 1989: 968.
27. Chen CJ, Lin TM, You SL. Epidemiological aspects of a poliomyelitis outbreak in Taiwan, 1982. Ann Acad Med 1984; 13: 149-55.
28. World Health Organization. Expanded Programme on Immunization (EPI): program review (China). Wkly Epidemiol Rec 1992; 15: 109-11.
29. Rosenberg ML. Shigella surveillance in the United States, 1975. J Infect Dis 1977; 136: 458-9.
30. Thacker SB, Parrish RG, Trowbridge FL, and Surveillance Coordination Group. A method for evaluating systems of epidemiological surveillance. World Health Stat Q 1988; 41: 11-18.
31. Birkhead G, Chorba TL, Root S, Klaucke DN, Gibbs NJ. Timeliness of national reporting of communicable diseases: the experience of the National Electronic Telecommunications System for Surveillance. Am J Public Health 1991; 81: 1313-15.
32. Katz SL. Measles and subacute sclerosing panencephalitis. In: Joklik WK, Willet HP, Amos DB, eds. Zinsser microbiology, 18th edn. new York: Appleton-Century-Crofts, 1985: 1062.
33. Clarkson JM, Fine PEM. The efficiency of measles and pertussis notification in England and Wales. Int J Epidemiol 1985; 14: 153-68.
34. Markowitz LE, Preblud SR, Orenstein WA, et al. Patterns of transmission in measles outbreaks in the United States, 1985-1986. N Eng J Med 1989; 320: 75-81.
35. Cliff AD, Hagget P, Stroup DF. The geographic structure of measles epidemics in the northeastern United States. A J Epidemiol 1992; 136: 592-602.
Epidemiology of measles in Taiwan
36. Hersh BS, Markowitz LE, Maes EF, et al. The geographic distribution of measles in the United States, 1980 through 1989. JAMA 1992; 267: 1936-41.
37. Smith FR, Curran AS, Raciti KA, et al. Reported measles in persons immunologically primed by prior vaccination. J Pediatr 1982; 101: 391-3.
38. Chen RT, Markowitz LE, Albrecht P, et al. Measles antibody: reevaluation of protective titers. J Infect Dis 1990; 162: 1036-42.
39. Pederson IR, Mordhorst CH, Glikmann G, et al. Subclinical measles infection in vaccinated seropositive individuals in arctic Greenland. Vaccine 1988; 7: 345-8.
40. Brandling-Bennett AD, Landrigan PJ, Baker EL. Failure of vaccinated children to transmit measles. JAMA 1973; 224: 616-18.
41. Mathias RG, Meekison WG, Arcand TA, et al. The role of secondary vaccine failure in measles outbreaks. Am J Public Health 1989; 79: 475-8.
42. Dai B, Chen Z, Lin Q, et al. Duration of immunity following immunization with live measles vaccine: 15 years of observation in Zhejiang Province, China. Bull WHO 1991; 69: 415-23. 43. Rota JS, Hummel KB, Rota PA, Bellini WJ. Genetic variability of the glycoprotein genes
of current wild-type measles isolates. Virology 1992; 188: 135-42.
44. Chen RT, Goldbaum GM, Wassilak SGF, et al. An explosive point-source measles outbreak in a highly vaccinated population. Am J Epidemiol 1989; 129: 173-82.
45. Remington PL, Hall WN, Davis IH, et al. Airborne transmission of measles in a physician's office. JAMA 1985; 253: 1574-7.
46. Thacker SB, Millar JD. Mathematical modeling and attempts to eliminate measles: a tribute to the late professor George MacDonald. Am J Epidemiol 1991; 133: 517-25.