Association Between Clinical Variables and Health-related Quality of Life in Patients with A Chronic Obstructive Pulmonary Disease
全文
(2) 156. Association Between Clinical Variables and Health-Related Quality of Life. decades [2]. According to an official report, COPD was the 11th leading cause of death in 2002 in Taiwan; however, this figure is an underestimation because of the different classification criteria used in Taiwan compared with that used in western countries [3]. The main symptoms of COPD include cough, sputum production, and dyspnea on exertion. Acute worsening of these symptoms often occurs episodically [1]. The physical effects of COPD include chronic shortness of breath and dyspnea, which reduces energy and vitality and can lead to anxiety, dependency, loss of selfesteem, and other psychiatric problems [4]. Smoking is an important risk factor for COPD [5]. The morbidity due to COPD increases with age and is greater in men than women [6]. The average survival time of COPD patients after diagnosis is about 15 years and mortality 10 years after diagnosis is above 50 percent [7,8]. However, COPD is not fully reversible and cannot be "cured". It can be managed using a combination of management strategies. The primary goals of COPD management are reduction of airflow obstruction, prevention or treatment of complications associated with the disease, and improvement of quality of life [9]. Quality of life is defined by the World Health Organization as an individual's perception of their position in life in the context of the culture and value systems in which they live, and in relation to their goals, expectations, standards, and concerns [10]. It is a broad ranging concept, incorporating in a complex way the persons' physical health, psychological state, level of independence, social relations, personal briefs, and relationship to salient features of environment. The World Health Organization QOL (WHOQOL) measurement is a multidimensional, multi-lingual profile that has been designed for cross-cultural subjective assessment [11,12]. The WHOQOL-BREF questionnaire used in this study includes 24 facets and 2 global WHOQOL items from the WHOQOL conceptual constructs, as well as two additional facets specifically designed for the. Taiwan WHOQOL-BREF version [13]. HRQL questionnaires, such as the WHOQOL-BREF, are increasingly being used as outcome measurements in clinical trials, effectiveness research, and research on quality of care [14]. The WHOQOL-BREF has been shown to have good internal reliability, test-retest reliability, content validity, discriminant validity and construct validity when applied to COPD patients [15]. Because COPD often affects older people, task performance may be less important than the ability to enjoy life. There is growing awareness that health status is better characterized by HRQL than standard physiologic outcomes [16-18]. Previous studies have shown that the relationship between respiratory impairment reflected by pulmonary functions such as the forced expiratory volume in one second (FEV 1 ), forced vital capacity (FVC), and the FEV 1/FVC ratio and HRQL measures in patients with COPD is only weakly significant [19-21]. Therefore, it is not possible to determine the impact of the disease on a patient by only examining the physiological index. The HRQL in elderly outpatients with chronic disease is a multidimensional construct which evaluates patients' health, psychological well-being, social relationships and their environment. Physicians may misinterpret patients' health status if they rely too heavily on physical symptoms and clinical variables [17]. Quality of life (QOL) is becoming an increasingly important outcome measure for physicians to evaluate the effectiveness of treatment strategies [22]. This type of selfperceived health outcome measure yields useful and relevant information because it reflects patients' experiences and perspectives. Physical symptoms alone may not accurately reflect patients' QOL. In order to gain a better understanding of the relationship between QOL and clinical parameters, we assessed the correlations between HRQL and clinical parameters of COPD patients, such as lung function (% predicted FEV1; FEV1/FVC), disease duration, and various medical symptoms as diagnosed by a physician..
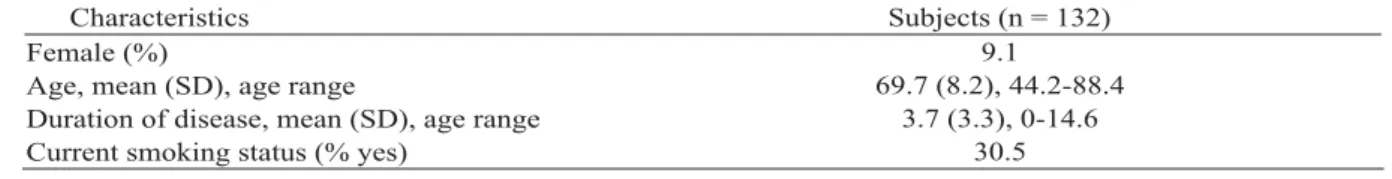
(3) Jian-Jung Chen, et al.. Table 1. Patients' characteristics Characteristics Female (%) Age, mean (SD), age range Duration of disease, mean (SD), age range Current smoking status (% yes). MATERIALS AND METHODS. Patient selection. A total of 132 COPD patients (12 females and 120 males) aged from 44 to 88 years (mean = 69.7 8.2), whose conditions had been diagnosed according to WHO GOLD guidelines [1] were enrolled in the study. Patients were recruited from outpatient clinics of the China Medical University Hospital (CMUH) and Changhua Christian Hospital (CCH) in central Taiwan from 1 August 2001 to 31 April 2003. Written informed consent was obtained from all participants in this study. Criteria for inclusion were as follows: 40 years of age or older; an FEV1/FVC < 70%, or an FEV1/FVC greater or equal to 70% associated with chronic bronchitis, or the presence of cough and sputum production for at least 3 months in each of two consecutive years. Subjects with cancer were excluded from our study. Lung function variables. FEV1 and FVC were evaluated on the same day as the questionnaire assessments. A diagnosis of COPD was confirmed by spirometry. Spirometric lung function parameters were determined by measuring FVC and FEV 1 and calculating the ratio between FEV 1 and FVC. Spirometric results were expressed as a predicted percentage using appropriate normal values for the person's gender, age, and height. Historically, patients with COPD typically show a decrease in both FEV 1 and FEV 1 /FVC. The degree of spirometric abnormality generally reflects the severity of COPD. Disease stage of COPD was determined using the GOLD criteria [1]. Clinical symptom variables. Patients' symptoms, including loss of appetite, fatigue, coughing frequency, and breathing difficulties, were assessed by the. 157. Subjects (n = 132) 9.1 69.7 (8.2), 44.2-88.4 3.7 (3.3), 0-14.6 30.5. physician during the physical examination using a self-developed questionnaire; the questionnaire had been validated by 3 physicians and 1 biostatistian. Each of the four symptoms was evaluated using a scale ranging from 0 to 100. For example, for appetite, 0 represented no appetite and 100 represented normal appetite. In the multiple regression analysis, each symptom score was divided into three groups (mild, moderate, and severe) by the 33.3 and the 66.7 percentiles. WHOQOL-BREF and other variables. WHOQOL-BREF questionnaire data were collected by interviewing patients in person at outpatient departments. All interviewers were well trained prior to data collection. Patients' demographic data and other basic information such as smoking status were collected during the interview. In addition, physicians attempted to determine the approximate duration of COPD. The Taiwan version of the WHOQOL-BREF was developed in compliance with WHO guidelines [23,24], and good reliability and validity of this version have been reported [25]. All items were rated on a five-point Likert scale with a higher score indicating a higher QOL. The scoring procedure was performed according to WHOQOL guidelines [26]. In WHOQOL-BREF, a score transformation was done for the "negative phrasing" items; so higher scores always indicated better HRQL. Each item score was transformed to a 0-100 score. Analysis of data. Pearson's correlation coefficients were determined to examine the degree of association among lung function parameters, clinical symptoms, and HRQL. To further examine the magnitude of each clinical variable on HRQL, we.
(4) 158. Association Between Clinical Variables and Health-Related Quality of Life. Table 2. Clinical variables and HRQL of the study population. Subjects (n = 132) Lung function: Mean (SD) 56.0 (20.1) FEV1 (% predicted) 61.4 (10.6) FEV1/FVC ratio Disease stages of severity*: n (%) 12.0 (9.1) Stage 0: at risk 6.0 (4.6) Stage I: mild 61.0 (46.2) Stage II: moderate 40.0 (30.3) Stage III: severe 13.0 (9.9) Stage IV: very severe Clinical symptoms scores: Mean (SD) 84.9 (19.5) Loss of appetite 73.4 (21.0) Fatigue 68.7 (16.9) Coughing frequency 60.8 (19.7) Breathing difficulties HRQL: Mean (SD) 59.4 (13.5) Physical 60.7 (13.5) Psychological 67.8 (8.8) Social 66.8 (9.8) Environmental Each symptom was evaluated using a scale of 0-100 (0 = most severe; 100 = normal). Each HRQL domain ranged from 0 to 100 (0 = very bad; 100 = very good). *Disease stage of COPD was determined using the GOLD criteria.. divided the clinical symptoms into three groups of severity (mild, moderate and severe). The stages of COPD were also combined to form three groups (stage 0 and I, stage II and III, and stage IV). We then applied multiple regression analysis to assess the relationship between each clinical variable and HRQL after adjusting for age and gender. SAS software [27] was used for all statistical analyses. A p value of < 0.05 was regarded as statistically significant. RESULTS. Patients. The characteristics of the 132 COPD patients are presented in Table 1. About 91% of patients were men and 9% were women with an average age of 69.7 years (SD = 8.2 yr, range = 44.2 to 88.4 yr). Duration of COPD ranged from 0 (recent diagnosis) to 14.6 years (mean = 3.7 yr; SD = 3.3 yr). Most patients stated that they were non-smokers (69.5%). Clinical variables and HRQL. The clinical variables and HRQL of the study population are presented in Table 2. Mean. FEV1% predicted was 56.0% and the FEV1/FVC ratio was 61.4. For clinical symptoms, the lowest score was for breathing difficulties (60.8), followed by coughing frequency (68.7), fatigue (73.4), and loss of appetite (84.9). Most patients (46.2%) were in lung function stage II, followed by stage III (30.3%), stage IV (9.9%), stage 0 (9.0%) and stage I (4.6%). For HRQL, the lowest scores were in the physical domain (59.4), followed by the psychological (60.7), environmental (66.8) and social (67.8) domains. Correlation between clinical variables and HRQL. The Pearson's correlation coefficients for clinical variables and HRQL in the four domains are presented in Table 3. FEV 1 (% predicted) correlated significantly with the physical domain (p = 0.0034). Fatigue and breathing difficulties were significantly related to the physical domain (p = 0.0062 and 0.0059, respectively). Breathing difficulties were also significantly related to the environmental domain (p = 0.0052). None of the other parameters (FEV 1 /FVC ratio, loss of appetite and coughing frequency) correlated with.
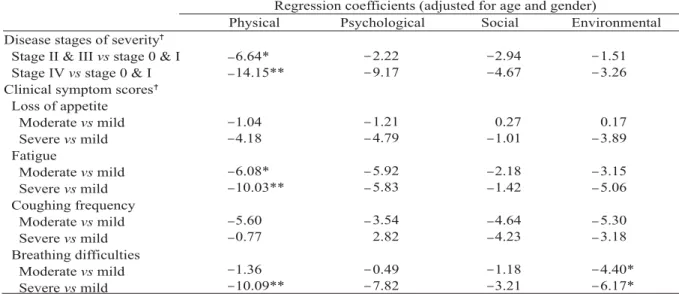
(5) Jian-Jung Chen, et al.. 159. Table 3. Pearson's correlations coefficients between clinical variables and HRQL Pearson's correlation coefficients Physical Psychological Social Lung function 0.15 0.04 0.25** FEV1 (% predicted) 0.02 0.01 0.15 FEV1/FVC ratio Clinical symptom scores 0.08 0.001 0.14 Loss of appetite 0.01 0.07 0.26** Fatigue 0.14 0.11 0.05 Coughing frequency 0.17 0.12 0.26** Breathing difficulties. Environmental 0.01 0.04. 0.11 0.13 0.002 0.27** Each symptom was evaluated using a scale of 0-100 (0 = most severe; 100 = normal). Each HRQL domain ranged from 0 to 100 (0 = very bad; 100 = very good). **p < 0.01.. Table 4. Multiple regression analysis of each clinical variable on HRQL Regression coefficients (adjusted for age and gender) Social Environmental Psychological Physical Disease stages of severity 2.22 2.94 1.51 6.64* Stage II & III vs stage 0 & I 9.17 4.67 3.26 14.15** Stage IV vs stage 0 & I Clinical symptom scores Loss of appetite 1.21 0.27 0.17 1.04 Moderate vs mild 4.79 1.01 3.89 4.18 Severe vs mild Fatigue 5.92 2.18 3.15 6.08* Moderate vs mild 5.83 1.42 5.06 10.03** Severe vs mild Coughing frequency 3.54 4.64 5.30 5.60 Moderate vs mild 4.23 3.18 2.82 0.77 Severe vs mild Breathing difficulties 0.49 1.18 4.40* 1.36 Moderate vs mild 7.82 3.21 6.17* 10.09** Severe vs mild Each HRQL domain ranged from 0 to 100 (0 = very bad; 100 = very good). For disease severity, stages 0 and I are combined to comprise the reference group. For clinical symptoms, scores of 0-100 were divided into three groups, mild, moderate and severe, based on the 33.3 and 66.7 percentiles, and the mild group served as the reference group. *p < 0.05, **p < 0.01.. any of the four domains. Multiple regression analysis of HRQL. Table 4 shows the regression coefficients from the multiple regression analysis between each clinical variable and each of the four HRQL domains after adjustment for age and gender. The results are similar to those in Table 3. The results revealed that severity of the disease, fatigue and breathing difficulty were significantly related to physical quality of life, and that breathing difficulty was significantly related to environmental quality of life. With disease stages 0 and I serving as the reference group for the physical domain, there were significant. differences in physical QOL scores in disease stages II and III group (p = 0.0030) and in disease stage IV group (p = 0.0447), respectively. Similarly, the physical quality of life decreased with worsening fatigue and breathing difficulty; and the environmental quality of life decreased with worsening breathing difficulty. DISCUSSION. The present study reveals that, for patients with chronic obstructive pulmonary disease (COPD), clinical variables are well related to the physical domain. This result was expected. Measurements of patients' clinical variables may.
(6) 160. Association Between Clinical Variables and Health-Related Quality of Life. not reflect their quality of life. Quality of life is a considerably more comprehensive measure than health status and includes other experiences that may or may not be affected by health or treatment [28]. Furthermore, our findings from both correlation and multiple regression analysis revealed that clinical variables were unrelated to the social and psychological domains, and only breathing difficulty was related to the environmental domain. In assessing patients' health status, physicians generally only measure basic physical clinical variables using a simple, self-designed questionnaire. However, such assessments do not measure non-physical characteristics such as psychological well-being, social relationship, and perception of environment. Increasingly, it has been recognized that health-related quality of life (HRQL) is an important outcome of medical care [28,29] and is a powerful predictor of hospitalization and all-cause mortality [7,30]. There are a number of well established health related quality of life questionnaires which have been shown to be useful in a clinical setting. For example, HRQL can markedly increase in COPD patients even when lung function variables remain unchanged, which demonstrates that HRQL can sensitively measure the influence of intervention programs on patients' prognosis independent of the physical domain [13,28,31,32]. A better understanding of the relationships between clinical variables and the measures of HRQL will enable physicians to conduct a more comprehensive evaluation of their patients. Breathing difficulty and coughing are two major symptoms of COPD [1,5]. In our study population, breathing difficulty and coughing were the two most bothersome symptoms followed by fatigue and loss of appetite. Breathing difficulty and fatigue correlated well with the physical domain, but coughing frequency and loss of appetite did not, possibly because of the nature of these symptoms. For example,. coughing in COPD patients is a very common symptom but HRQL was assessed during the day when coughing may be less severe. In addition, coughing symptom is readily influenced by other factors such as air pollutants and allergens which may induce intermittent episodes of coughing. It was therefore difficult to establish a strong link between coughing frequency and HRQL. Dyspnea though was strongly related to HRQL because it represents a worsening of health status and is a much more unpleasant physical symptom than coughing. Recent studies have shown that differences in health status may not be detected until the later stages of the disease [2]. As such, physical HRQL in COPD patients is better correlated with dyspnea than with coughing. A methodological limitation of the study was its cross sectional design, which does not allow for much scope to make predictions or generalizations. Most COPD patients in this study were in disease stages II and III, so the data did not adequately represent patients in stages 0, I and IV. The only QOL questionnaire used in this study was the generic WHOQOL-BREF; we did not use a disease-specific QOL questionnaire. Smoking is an important risk factor for COPD patients but in this study we only measured current smoking status. We did not collect detailed data, such as age at smoking commencement and total packs smoked per year. In addition, most patients had quit smoking by the time the disease was diagnosed. Therefore current smoking status did not yield any significant trend with regard to QOL in the analysis. Duration of disease is often difficult to determine because many patients at diagnosis are already at disease stage II or III. Because duration of disease is often underestimated, it is not a good predictor of HRQL [2,33]. Hence, in our regression analysis, smoking status and duration of disease were not included because these factors were problematic. In conclusion, COPD patients' clinical variables only give the physician limited information about their health status. Assessment.
(7) Jian-Jung Chen, et al.. of patients' health-related quality of life may provide additional, useful information relevant to the patients' psychological, social, environmental as well as physical needs. It is necessary for healthcare workers to measure and promote QOL because for this group of patients enhancement of self-perceived well-being is as important as managing the physical aspects of the disease. ACKNOWLEDGMENTS. This work was supported by grants from the National Health Research Institute, Taiwan, R.O.C., (NHRI-EX94-9204PP) and from the China Medical University, Taiwan, R.O.C. (CMC89-EM-04). We would like to thank Drs. Jen-Ho Wen, Kai-Huang Lin, Chu-Hsien Wang and Ming-Lin Ho at the Changhua Christian Hospital for their assistance in recruiting COPD patients. We are also grateful to Dr. Jung-Der Wang for his guidance in the field of quality of life. REFERENCES. 1. Pauwels RA, Buist AS, Calverley PM, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. [Review] Am J Respir Crit Care Med 2001; 163:1256-76. 2. Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease (COPD). [Review] Lancet 2004;364:613-20. 3. Kuo LC, Yang PC, Kuo SH. Trends in the mortality of chronic obstructive pulmonary disease in Taiwan, 1981-2002. J Formos Med Assoc 2005;104:89-93. 4. Stavem K, Boe J, Erikssen J. Health status, dyspnea, lung function and exercise capacity in patients with chronic obstructive pulmonary disease. Int J Tuberc Lung Dis 1999;3:920-6. 5. Janssens JP, de Muralt B, Titelion V. Management of dyspnea in severe chronic obstructive pulmonary disease. [Review] J Pain Symptom Manage 2000;19: 378-92. 6. Higgins MW, Thom T. Incidence, prevalence, and mortality: intra- and inter-country differences. In: Hensley M, Saunders N, eds. Clinical Epidemiology. 161. of Chronic Obstructive Pulmonary Disease. New York: Marcel Dekker, 1989:23-43. 7. Traver GA, Cline MG, Burrows B. Predictors of mortality in chronic obstructive pulmonary disease. Am Rev Respir Dis 1979;119:895-902. 8. Ferguson GT, Cherniack RM. Management of chronic obstructive pulmonary disease. [Review] N Engl J Med 1993;328:1017-22. 9. Make B. COPD: management and rehabilitation. [Review] Am Fam Physician 1991;43:1315-24. 10. Szabo S. The World Health Organization Quality of Life (WHOQOL) assessment instrument. In: Spiker B, ed. Quality of Life and Pharmacoeconomics in Clinical Trials. Philadelphia: Lippincott-Raven, 1996:355-62. 11. The WHOQOL Group. The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Soc Sci Med 1998;46:1569-85. 12. The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psych Med 1998;28:551-8. 13. Lin MR, Yao KP, Hwang JS, et al. Scale descriptor selection for Taiwan-version of questionnaire of World Health Organization quality of life. Chin J Pub Health (Taipei) 1999;18:262-70. (In Chinese; English abstract). 14. Hui KP, Hewitt AB. A simple pulmonary rehabilitation program improves health outcomes and reduces hospital utilization in patients with COPD. Chest 2003;124:94-7. 15. Chen JJ, Chang YY, Liang WM, et al. Factor construct and health profile which define the quality of life in patients with chronic obstructive pulmonary disease. Mid Taiwan J Med 2004;9:103-12. 16. Pearlman RA, Uhlmann RF. Quality of life in chronic diseases: perceptions of elderly patients. J Gerontol 1988;43:25-30. 17. Mahler DA. How should health-related quality of life be assessed in patients with COPD? [Review] Chest 2000;117(2 Suppl):54-7. 18. Yohannes AM, Roomi J, Waters K, et al. Quality of life in elderly patients with COPD: measurement and predictive factors. Respir Med 1998;92:1231-6. 19. Schrier AC, Dekker FW, Kaptein AA, et al. Quality of life in elderly patients with chronic nonspecific lung disease seen in family practice. Chest 1990;98:894-9. 20. Okubadejo AA, Jones PW, Wedzicha JA. Quality of.
(8) 162. Association Between Clinical Variables and Health-Related Quality of Life. life in patients with chronic obstructive pulmonary disease and severe hypoxaemia. Thorax 1996;51:44-7. 21. Guyatt GH, Townsend M, Berman LB, et al. Quality of life in patients with chronic airflow limitations. Dis Chest 1987;81:45-54. 22. Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA 1995;273:59-65. 23.World Health Organization. WHOQOL Study Protocol. Geneva: WHO (MNH/PSF/93.9), 1993. 24. Anderson RT, Aarson NK, Bullinger M, et al. A review of the progress towards developing healthrelated guality-of-life instruments for international clinical studies and outcomes research. [Review] Pharmacoeconomics 1996;10:336-55. 25.Yao G, Chung CW, Yu CF, et al. Development and verification of validity and reliability of the WHOQOL-BREF Taiwan version. J Formos Med Assoc 2002;101:342-51. 26.World Health Organization. WHOQOL-BREF: Introduction, Administration, Scoring and Generic Version of the Assessment — field Trail Version. Geneva, 1996.. 27. SAS/STAT User's Guide, Vol 1 and 2. Version 6, 4th edition. 1990. SAS Institute Inc., Cary, NC. 28.Curtis JR, Patrick DL. The assessment of health status among patients with COPD. [Review] Eur Respir J Suppl 2003;21:36-45. 29. Hsiung PC, Fang CT, Chang YY, et al. Comparison of WHOQOL-BREF and SF-36 in patients with HIV infection. Qual Life Res 2005;14:141-50. 30. Fan VS, Curtis JR, Tu SP, et al. Using quality of life to predict hospitalization and mortality in patients with obstructive lung diseases. Chest 2002;122:429-36. 31. Bourbeau J, Julien M, Maltais F, et al. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific selfmanagement intervention. Arch Intern Med 2003;163: 585-91. 32. Nelson EC, Berwick DM. The measurement of health status in clinical practice. [Review] Med Care 1989;27 (3 Suppl):77-90. 33. Rennard S, Decramer M, Calverley PM, et al. Impact of COPD in North America and Europe in 2000: subjects' perspective of Confronting COPD International Survey. Eur Respir J 2002;20:799-805..
(9) 163. 1. 1. 2. 3. 3. 1. 3. 1. 2. (COPD) (HRQL) COPD 132. COPD. 44.2. 2003. 88.4. 2001 (WHOQOL-. BREF) (FEV1%. ). 2006;11:155-63. 404. 91. 2005. 8. 16. 2006. 5. 10. 2005. 11. 9.
(10)
數據
相關文件
Of the 19 patients with clinical stage 2, one (5.3%) patient had a normal epithelium, 16 (84.2%) patients had only epithelial changes (EE + HE), and two (10.5%) patients had
The clinical and radiological features of 6 cases of NBCCS were characterized into major and minor criteria and compared with features reported in Indian patients and in patients
In view of both spread of the HIV epidemic in Africa and poor access to highly active antiretroviral therapy (HAART), infected patients often develop rapidly progressive KS with
28 Specifically, in this study we determined that (1) individuals having comorbid OSA and MetS, that is SZ, have a greater prevalence of calcified carotid artery atherosclerotic
原文題目(出處): Prevalence of calcified carotid artery atheromas on the panoramic images of patients with syndrome Z, coexisting obstructive sleep apnea, and metabolic
In clinical trials involving patients with DDwoR, however, most authors usually define their samples based on the duration of symptoms (i.e. locking duration or time since
SUMMARY The purpose of this systematic review was to describe the prevalence of whiplash trauma in patients with temporomandibular disorders (TMDs) and to describe clinical signs
The clinical and radiographic records of 208 patients suffering from neurological symptoms in maxillofacial region. They had referred to neurology department and then