Herbal Medicines Used During the
First Trimester and Major
Congenital Malformations
An Analysis of Data from a Pregnancy Cohort Study
Chao-Hua Chuang,1,2 Pat Doyle,3 Jung-Der Wang,1,4 Pei-Jen Chang,5 Jung-Nien Lai1,6
and Pau-Chung Chen1
1 Institute of Occupational Medicine and Industrial Hygiene, National Taiwan University College of Public Health, Taipei, Taiwan
2 Department of Nursing, Fooyin University, Kaohsiung County, Taiwan
3 Department of Epidemiology and Population Health, London School of Hygiene and Tropical Medicine, London, UK
4 Department of Internal Medicine, National Taiwan University Hospital, Taipei, Taiwan 5 Department of Nursing, National Taipei College of Nursing, Taipei, Taiwan
6 Division of Gynecology, Traditional Chinese Medicine, Taipei City Hospital, Taipei, Taiwan
Background: Major congenital malformations place a considerable burden on the
Abstract
affected child, the family and society. Any kind of medicine used during pregnan-cy might have a harmful impact; therefore, such practice has raised concerns. The objective of the current study was to explore the relationship between the use of herbal medicines by pregnant women during the first trimester of pregnancy and the risk of major congenital malformation in their live born infants.
Methods: This was a cross-sectional analysis of data from a prospective
pregnan-cy cohort, which was established between 1984 and 1987. To assemble the cohort, pregnant women of ≥26 weeks of gestation who came to the Taipei Municipal Maternal and Child Hospital in Taiwan for prenatal care were enrolled in the study and interviewed using a structured questionnaire. Detailed information, including herbal medicine use during different periods of pregnancy, was obtained during the interview. Past medical history, current obstetric data and details on conven-tional medicines used during pregnancy were abstracted from medical records. Data on birth weight, gestational duration and characteristics of live born infants were gathered from the Taiwan national birth register. Congenital malformation information was obtained from multiple sources: the newborn examination record (1984–7); the national death register (1984–2003); and Taiwan National Health Insurance data (1996–2000). Multiple logistic regression was used to estimate the odds ratio [OR] of major congenital malformation by herbal medicines used during the first trimester.
Results: A total of 14 551 live births were analysed. After adjustment for
confounding factors, taking huanglian during the first trimester of pregnancy was found to be associated with increased risk of congenital malformations of the
nervous system (adjusted OR 8.62, 95% CI 2.54, 29.24). An-Tai-Yin was associ-ated with an increased risk of congenital malformations of the musculoskeletal and connective tissues (adjusted OR 1.61, 95% CI 1.10, 2.36) and the eye (adjusted OR 7.30, 95% CI 1.47, 36.18).
Conclusion: We found evidence for a possible link between the use of specific
herbal medicines during the first trimester of pregnancy and increased risks of specific groups of congenital malformations. We could not investigate whether the adverse effects were related to direct toxicity from the herbal medicines, or were from misuse, contamination or uncontrolled confounding. Nonetheless, we would advise caution regarding use of herbal medicines during pregnancy, and we suggest that further investigation of these findings is warranted.
Background nancy seemed to produce no adverse effects for either the mother or fetus;[25,26] however, a local
herbal medicine from South Africa used in labour Major congenital malformations occur in
approx-resulted in an increased rate of fetal distress.[27]
imately 3% of live births,[1,2] placing a considerable
burden on the affected child, the family and society. Several review articles have shown inconclusive The embryonic period, from the second to the eighth results for a variety of herbs used for different week of gestation, is the critical window of vulnera- purposes in pregnancy.[28,29] Several animal studies
bility for the developing fetus when exposure to have demonstrated potential adverse effects of herb-harmful agents such as drugs, chemical and biologi- al medicines in pregnancy. The administration of cal agents, and radiation,[3] as well as nutritional
berberine chloride dehydrate (berberine is the main deficiencies,[4] may cause structural malformations.
component of huanglian) to rats during pregnancy There are also other risk factors related to congenital decreased fetal weight.[30] Ginseng was found to be
anomalies such as multiple births,[5]
consanguini-teratogenic for rat embryos,[31] and some traditional
ty,[6] maternal life-event stress[7] and premature
Chinese medicines demonstrated inhibition of early birth.[8]
mouse embryogenesis.[32] Besides the direct toxicity
The use of herbal medicine is common in Tai- of herbal material,[33] issues to consider in any study
wan[9,10] and is gaining popularity worldwide,[11-13]
include contamination by microbes, heavy metals, including its use during pregnancy.[14-19] Because of
pesticides or even adulteration with Western the potential harmful impact of any kind of medicine medicines, which may confound the potential herbal during pregnancy, such practice has raised concerns toxicity.[34-37]
among public health practitioners and consumers
Although the safety and efficacy of herbal regarding benefit and risk.[15,19] Numerous studies of
medicines remain largely unassessed, their use is maternal drug consumption during pregnancy have
becoming increasingly fashionable in Western been carried out over the last few decades.[20-24]
countries.[38] Critical assessment of their safety and
However, most have dealt with prescription drugs
efficacy is an urgent necessity. The aim of this study and conventional medication and there is a general
was to explore the relationship between the use of lack of evidence for safety and efficacy regarding
herbal medicines during the first trimester of preg-the use of herbal medicines during pregnancy. The
nancy and the risk of major congenital malforma-few published studies on this topic have concluded
Methods naire. Education was stratified into four groups: university and college or above, senior high school, junior high school, and primary school and below. Study Population and Data Collection
Classifications of occupation were made according to the modified Taiwanese version of the Interna-The pregnancy cohort comprised pregnant
wo-tional Classification of Occupations, and were later man of ≥26-weeks gestation who came to the Taipei
summarised into four groups: non-manual, manual, Municipal Maternal and Child Hospital (TMMCH)
housewives and other occupations. Family income for prenatal care between September 1984 and June
was defined as the total parental monthly income 1987. A structured questionnaire was used to
pro-(US$1 ≈ NT$[new Taiwan dollar]33, in 2004) with spectively obtain detailed information regarding the
four categories: ≥40 001, 30 001–40 000, use of herbal medicines during different pregnancy
20 001–30 000 and ≤20 000 per month. periods, gynaecological and obstetric history, and
various demographic variables relating to family Previous gynaecological and obstetric histories life. The interviews were conducted in the third were obtained from the interview questionnaire. Ob-trimester of pregnancy by the same three interview- stetric and perinatal outcomes included previous ers. The medical records of each mother were then spontaneous abortion, stillbirth or neonatal death, reviewed by the same medical assistant to extract previous low birth weight or preterm delivery. pertinent information on their medical history and Gynaecological history included diseases related to use of conventional medicines during pregnancy. the uterus, ovary or fallopian tube, and infertility. Data on birth weight, gestation duration, and Medical histories of diabetes mellitus, hypertension characteristics of live born infants were gathered or antepartum haemorrhage, as well as conventional from the Taiwan national birth register (for births medicine use during pregnancy, were extracted from 1984–7). Congenital malformation information was the mothers’ medical records.
obtained from several sources. First, information
Information on the use of herbal medicines and was extracted from the newborn examination and
vitamin and iron supplements during the prenatal medical records for births during 1984–7. The other
period was obtained from questionnaires on prenatal sources of congenital malformation data were
na-care visits. For the purposes of this study, a herbal tional death registrations for the period 1984–2003
medicine is defined as any botanical product or and Taiwan National Health Insurance data on
criti-preparation with presumed therapeutic or other cal illness and injury registration during 1996–2000.
human health benefits that contains either raw or We used the national identification number (ID) of
processed ingredients from one or more plants.[39] In
mothers to link them to the Taiwan national birth
traditional Chinese medicine, materials of inorganic registration, and were able to obtain the ID of their
or animal origin may also be present. children. Using the ID of the child, we then searched
Major congenital malformations were defined as the national death registration and National Health
those that can adversely affect the health and devel-Insurance data on critical illness and injury
registra-opment of the infant. They were categorised accord-tion to obtain malformaaccord-tion informaaccord-tion.
ing to the 9th edition of the International Classifica-All study participants provided informed
con-tion of Diseases (ICD-9) list of congenital
malfor-sent, which was approved by the National Taiwan
mation, as described in the Eurocat Guide 1.2.[40]
University College of Public Health Ethic Review
The exclusion criteria were chromosomal anoma-Board.
lies, minor congenital malformations, small case numbers, or non-significant statistic. We examined Variables
12 categories of congenital malformation, relating to: other nervous system, neural-tube defects, eye, Data on age, education, occupation and family
ear, heart, cleft lip with or without cleft palate, cleft income were obtained from the interview
question-tential confounders.[41] It is the method that selects a
variable for control only if its control produces >10% change in a rate ratio estimate of interest.
Potential confounding variables included charac-teristics of the mothers (age, education, occupation, body height and pre-pregnant bodyweight); charac-teristics of the fathers (age, education, occupation and family income); characteristics of the infants themselves (number, sex, parity and gestational age); obstetric history and maternal exposures dur-ing pregnancy (previous histories of gynaecological diseases, previous low birth weight or preterm deliv-ery, previous spontaneous abortion, chronic diseas-es, diabetdiseas-es, hypertension, antepartum haemorrhage, medicines used during pregnancy, vitamin or iron supplements, fever >38°C, microwave oven use, x-ray radiography used, stressful events, general an-aesthesia used, chemical exposure in the workplace, laboratory work, cigarette smoking, alcohol intake during the first trimester); paternal exposures during the 1-year period before his partner’s current preg-nancy (long-term medication taken, chemical expo-Table I. International Classification of Diseases – 9th edition
(ICD-9) codes for the categories of major congenital malformations used in the study
Category of ICD-9 code malformation Other nervous 742.1–742.5, 742.8, 742.9 system Neural-tube defects 740.0–740.2, 741.0–741.9, 742.0 Eye 743.0–743.6 [excl. 743.65] 743.8–743.9 Ear 744.0–744.2 [excl. 744.11, 744.12] Heart 745.0–745.9, 746.0–746.9, 747.0–747.4 [excl. 747.0a]
Cleft lip with or 749.1–749.2 without cleft palate
Cleft palate 74.0
Digestive system 750.3–750.5, 750.7–751.9 Internal urogenital 752.0–752.3, 752.9, 753.0–753.9 system
External genital 752.4–752.8 [excl. 752.5] system
Musculoskeletal and 744.5, 754.0 connective tissues
Limbs 754.4–754.7 [excl. 754.52, 754.60, 754.73], 755.0–755.6 [excl. 755.60], 755.8–755.9 a Patient ductus arteriosus in preterm/low birth weight babies. excl. = excluding.
sure, x-ray radiography use, cigarette smoking, alco-hol intake, general anaesthesia); and history of con-palate, digestive system, internal urogenital system,
genital malformation in the parents and relatives. external genital system, musculoskeletal and
con-Statistical analysis was performed using SPSS for nective tissues, and limbs. A full list of ICD-9 codes
Windows, Release 11.0. is given in table I.
There were several categories of herbal
Results
medicines used during the first trimester, including An-Tai-Yin, huanglian, ginseng, Ba-Zhen-Tang,
A total of 14 551 live births were included in the Szu-Wu-Tang, Dang-Gui-Saho-Yao-San and
study population. The mothers represented approxi-others.[9] Our final grouping for analysis was based
mately 80% of pregnant women accepting prenatal on frequency of use and consisted of An-Tai-Yin
care at our study hospital between 1984 and 1987. alone, huanglian alone, ginseng alone, and others.
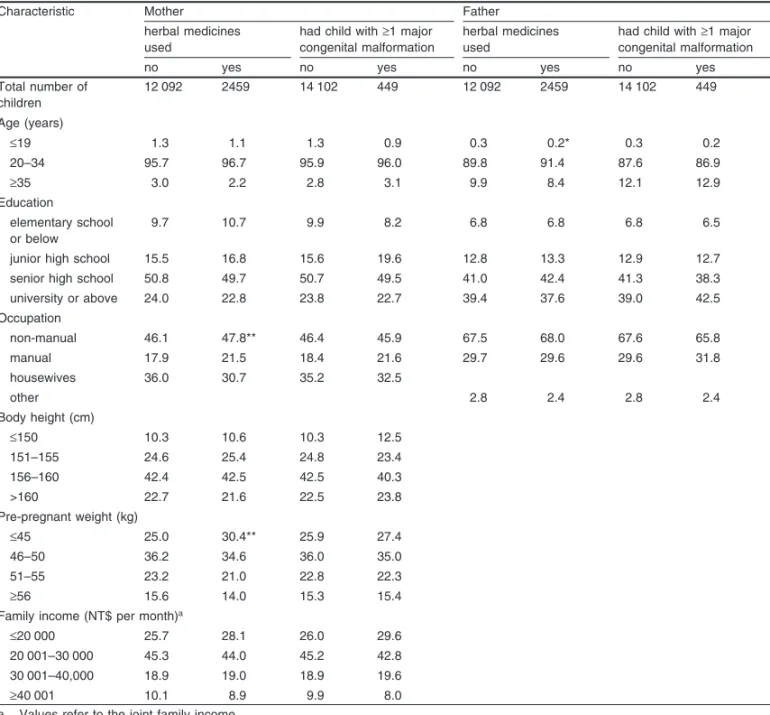
The majority of parents were 20–34 years old Other herbs either in single or combined use
includ-with a senior high school education, a non-manual ed any herbs except for An-Ti-Yin, huanglian and
occupation and a monthly family income of ginseng.
NT$20 001–30 000 (table II). Compared with the national census data during the period of 1984–7 in Analyses
Taiwan,[42] our sample seemed to have a higher
Multiple logistic regression was used to estimate proportion of women with a senior high school odds ratios [ORs] for each of the 12 categories of education or above (73.2% vs 34.7%), employment congenital malformation in live born children ac- (67.1% vs 45.4%) and professional job (8.5% vs cording to the usage of different herbal medicines 0.5%). The study participants were of higher socio-during the first trimester of pregnancy. A 10% economic status than the average Taiwanese citizen. change-in-estimate method was used to assess po- The majority of pre-pregnant bodyweights and
Table II. Percentages of live born children stratified by parental characteristics
Characteristic Mother Father
herbal medicines had child with ≥1 major herbal medicines had child with ≥1 major used congenital malformation used congenital malformation
no yes no yes no yes no yes
Total number of 12 092 2459 14 102 449 12 092 2459 14 102 449 children Age (years) ≤19 1.3 1.1 1.3 0.9 0.3 0.2* 0.3 0.2 20–34 95.7 96.7 95.9 96.0 89.8 91.4 87.6 86.9 ≥35 3.0 2.2 2.8 3.1 9.9 8.4 12.1 12.9 Education elementary school 9.7 10.7 9.9 8.2 6.8 6.8 6.8 6.5 or below
junior high school 15.5 16.8 15.6 19.6 12.8 13.3 12.9 12.7 senior high school 50.8 49.7 50.7 49.5 41.0 42.4 41.3 38.3 university or above 24.0 22.8 23.8 22.7 39.4 37.6 39.0 42.5 Occupation non-manual 46.1 47.8** 46.4 45.9 67.5 68.0 67.6 65.8 manual 17.9 21.5 18.4 21.6 29.7 29.6 29.6 31.8 housewives 36.0 30.7 35.2 32.5 other 2.8 2.4 2.8 2.4 Body height (cm) ≤150 10.3 10.6 10.3 12.5 151–155 24.6 25.4 24.8 23.4 156–160 42.4 42.5 42.5 40.3 >160 22.7 21.6 22.5 23.8 Pre-pregnant weight (kg) ≤45 25.0 30.4** 25.9 27.4 46–50 36.2 34.6 36.0 35.0 51–55 23.2 21.0 22.8 22.3 ≥56 15.6 14.0 15.3 15.4 Family income (NT$ per month)a
≤20 000 25.7 28.1 26.0 29.6 20 001–30 000 45.3 44.0 45.2 42.8 30 001–40,000 18.9 19.0 18.9 19.6 ≥40 001 10.1 8.9 9.9 8.0 a Values refer to the joint family income.
NT$ = new Taiwanese dollar; * p < 0.05; ** p < 0.001 in Chi-square test.
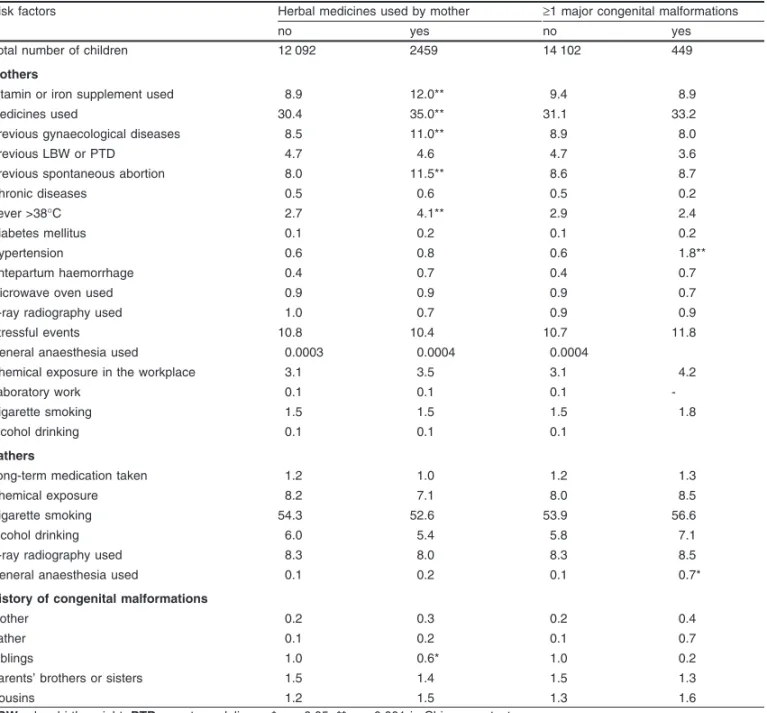
heights of mothers were in the ranges of 46–50kg of gynaecological diseases, low birth weight or and 156–160cm, respectively. In addition, approxi- preterm delivery, spontaneous abortion, chronic dis-mately 99% of infants were singleton and 97% were eases or fever >38°C during the first trimester. Less carried to full term. Approximately half of the in- than 1% of mothers experienced diabetes, hyperten-fants were male and first parity (table III). sion, or antepartum haemorrhage during pregnancy. Exposure to a microwave oven, x-ray radiography, Overall, 31% of mothers used medicines during
stressful events, general anaesthesia, chemicals, or pregnancy and approximately 9% used vitamin and
laboratory work during the first trimester was not iron supplements during the first trimester (table
quent groups were congenital anomalies of the mus-culoskeletal and connective tissues, external genital system, heart, internal urogenital system and ear. There were no differences in the frequency of re-ported malformations when the dataset was restrict-ed to mothers with no recordrestrict-ed diseases, such as chronic diseases, fever >38°C during first trimester, hypertension, diabetes or antepartum haemorrhage during pregnancy.
Adjusted ORs for maternal herbal medicine use during the first trimester of pregnancy and major congenital malformations are shown in table VII. After adjustment for confounding factors, taking huanglian during the first trimester of pregnancy was found to be associated with an increased risk of congenital malformation of the nervous system (ad-justed OR 8.62, 95% CI 2.54, 29.24). There were no cases of neural tube defects in the children of wo-men who took huanglian. There was some evidence Table III. Percentage of live born children stratified by their
charac-teristics
Characteristics Herbal medicines ≥1 major congenital used by mother malformation no yes no yes Total number of 12 092 2459 14 102 449 children Number singleton 98.7 99.0* 98.8 98.4 twin 1.3 0.9 1.2 1.6 triplet or higher 0.0003 0.1 0.0005 Sex male 51.3 51.6 51.2 55.9* female 48.7 48.4 48.8 44.1 Parity 1 49.4 57.7** 50.6 57.2* 2–3 48.6 40.9 47.5 41.9 ≥4 2.0 1.4 1.9 0.9 Preterm delivery no 96.9 96.5 96.9 97.3 yes 3.1 3.5 3.1 2.7 * p < 0.05; ** p < 0.001 in Chi-square test.
that huanglian was also associated with an increased risk to the external genital organs (adjusted OR 3.82, during the first trimester of pregnancy and <1% 95% CI 1.18, 12.40), although this finding was less
drank alcohol. robust when mothers with recorded disease were
excluded. An-Tai-Yin was associated with an in-Very few fathers took long-term medicines, had
creased risk of congenital malformations of the mus-been exposed to chemicals, x-ray radiography,
gen-culoskeletal and connective tissues (adjusted OR eral anaesthesia or alcohol during the 1-year period
1.61, 95% CI 1.10, 2.36) and eye (adjusted OR 7.30, before their partners’ current pregnancy (table IV).
95% CI 1.47, 36.18). There were no differences in Over half of fathers had smoked before the current
these findings when mothers with recorded diseases pregnancy. Very few congenital malformations
were excluded (table VII). were reported for parents or other relatives.
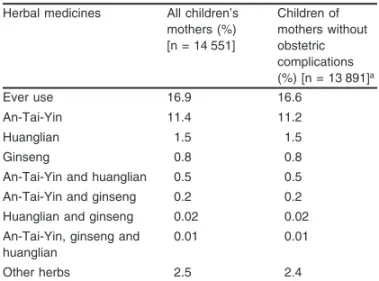
A total of 16.9% of the children’s mothers
report-Discussion
ed ever-use of any type of herbal medicine during
the first trimester of pregnancy (table V). An-Tai- This study found an association between the use Yin and huanglian were the most commonly con- of huanglian and An-Tai-Yin during the first trimes-sumed herbal medicines, with prevalences of 11.4% ter of pregnancy and an increased risk of specific and 1.5%, respectively. Less than one in 100 groups of major congenital malformations in the mothers (0.8%) took ginseng. There was no differ- resulting offspring. However, the validity of our ence in the pattern of use when the dataset was study methods needs to be carefully assessed before restricted to mothers who did not have any recorded making any firm conclusions.
disease. We collected detailed information about the ten
A total of 449 (3.1%) children had 469 major most commonly used herbal medicines by malformations (table VI). Since some degree of Taiwanese women in pregnancy. Other herbal underestimation of prevalence in registration data is medicines were used, but so rarely that we were expected, our observed prevalence of approximately unable to explore their effect. In particular, we had 3% appears reasonably accurate. The five most fre- insufficient power to investigate the effect of
gin-Table IV. Percentage of liveborn children stratified by parental risk factors
Risk factors Herbal medicines used by mother ≥1 major congenital malformations
no yes no yes
Total number of children 12 092 2459 14 102 449 Mothers
Vitamin or iron supplement used 8.9 12.0** 9.4 8.9
Medicines used 30.4 35.0** 31.1 33.2
Previous gynaecological diseases 8.5 11.0** 8.9 8.0
Previous LBW or PTD 4.7 4.6 4.7 3.6
Previous spontaneous abortion 8.0 11.5** 8.6 8.7
Chronic diseases 0.5 0.6 0.5 0.2
Fever >38°C 2.7 4.1** 2.9 2.4
Diabetes mellitus 0.1 0.2 0.1 0.2
Hypertension 0.6 0.8 0.6 1.8**
Antepartum haemorrhage 0.4 0.7 0.4 0.7
Microwave oven used 0.9 0.9 0.9 0.7
X-ray radiography used 1.0 0.7 0.9 0.9
Stressful events 10.8 10.4 10.7 11.8
General anaesthesia used 0.0003 0.0004 0.0004
Chemical exposure in the workplace 3.1 3.5 3.1 4.2
Laboratory work 0.1 0.1 0.1
-Cigarette smoking 1.5 1.5 1.5 1.8
Alcohol drinking 0.1 0.1 0.1
Fathers
Long-term medication taken 1.2 1.0 1.2 1.3
Chemical exposure 8.2 7.1 8.0 8.5
Cigarette smoking 54.3 52.6 53.9 56.6
Alcohol drinking 6.0 5.4 5.8 7.1
X-ray radiography used 8.3 8.0 8.3 8.5
General anaesthesia used 0.1 0.2 0.1 0.7*
History of congenital malformations
Mother 0.2 0.3 0.2 0.4
Father 0.1 0.2 0.1 0.7
Siblings 1.0 0.6* 1.0 0.2
Parents’ brothers or sisters 1.5 1.4 1.5 1.3
Cousins 1.2 1.5 1.3 1.6
LBW = low birth weight; PTD = preterm delivery; * p < 0.05; ** p < 0.001 in Chi-square test.
seng in pregnancy. We did attempt to analyse the exposed to An-Tai-Yin. According to the national association between congenital malformations and Taiwan congenital malformation registration data combined use of common herbal medicines such as for live born infants in 1993 (the initial year of An-Tai-Yin, huanglian, and ginseng. The results did monitoring),[43] the prevalence rate of congenital
not show any significant effects, most probably
be-malformation of the nervous system and eye was cause of low statistical power due to the small
approximately 0.18% and 0.02%, respectively. The numbers of combined exposures and congenital
expected numbers of nervous system anomalies in malformations. There were only three cases of
ner-our study population would be about 0.4 and 0.3, vous system anomalies in children exposed to
founding by indication of use for specific herbal medicines.
We were concerned about the potential con-founding factor of pre-existing disease in the moth-er, or obstetric complications occurring during preg-nancy. For this reason we stratified our subjects into two groups: one group included all pregnant women enrolled in the study, the other included only preg-nant women without chronic diseases, fever >38°C during the first trimester, diabetes, hypertension, or antepartum haemorrhage during pregnancy. Apart from the findings for huanglian and malformations of the genital system, the pattern of results was similar in both groups and we are confident that pre-existing maternal disease or obstetric complications cannot explain the findings presented here.
We thus conclude that the habit of pregnant wo-Table V. Percentages of children whose mother used herbal
medicines during the first trimester
Herbal medicines All children’s Children of mothers (%) mothers without [n = 14 551] obstetric complications (%) [n = 13 891]a Ever use 16.9 16.6 An-Tai-Yin 11.4 11.2 Huanglian 1.5 1.5 Ginseng 0.8 0.8
An-Tai-Yin and huanglian 0.5 0.5 An-Tai-Yin and ginseng 0.2 0.2 Huanglian and ginseng 0.02 0.02 An-Tai-Yin, ginseng and 0.01 0.01 huanglian
Other herbs 2.5 2.4
a Excluding mothers with chronic diseases, fever >38°C during first trimester, hypertension, diabetes mellitus, or antepartum haemorrhage during pregnancy.
men using herbal medicines during pregnancies was associated with increased risk of congenital malfor-need to be taken into account for interpreting our
mations. We can say little about mechanisms. The results, in addition to small numbers.
adverse effect of herbal medicines might result from There were 12 categories of major congenital
direct herbal toxicity, or contamination of herbal malformations included in our study. The congenital
medicines from microbes, heavy metals, or pesti-malformation relating to chromosomes was
exclud-cides, or even adulteration with Western medicines. ed because there were only nine cases of congenital
It is important to understand why women take anomalies of chromosomes, and most of them were
herbal medicines during pregnancy. Traditionally, Down’s syndrome. In general, Down’s syndrome is
initiated around the time of fertilisation, so the effect of herbal medicines on the occurrence of Down’s syndrome could be excluded. Most of the structural congenital malformations occur in the first trimes-ter, so we focused on the effects of hazards on this period.
In general, Western medicines are only used for specific indications during pregnancy, which im-plies a high correlation between indications and prescribed medicines. However, pregnant women in Taiwan traditionally use most herbal medicines without any specific purpose. The exception is An-Ta-Yin, which seemed more likely to be used when there was a previous history of abortion. However, in the multiple logistic regression model, controlling for the possible confounding effect of history of previous abortion did not change the estimate be-tween An-Tai-Yin and musculoskeletal and connec-tive tissues or eye anomalies, suggesting little
con-Table VI. Percentages of children with ≥1 major congenital malfor-mation
Malformation category % of children (n = 14 551)a
Any major congenital malformation 3.1 Musculoskeletal and connective 1.3 tissues
External genital system 0.4
Heart 0.4
Internal urogenital system 0.4
Ear 0.3
Other nervous system 0.2 Neural-tube defects 0.04
Limbs 0.1
Digestive system 0.1 Cleft lip with or without palate 0.1 Cleft palate 0.1
Eye 0.04
a These figures did not change when data from mothers with chronic diseases, fever >38°C during first trimester, hypertension, diabetes mellitus or antepartum haemorrhage during pregnancy were excluded.
Drug Safety 2006; 29 (6)
malformations n OR n OR (95% CI) n OR (95% CI) n OR (95% CI) n OR (95% CI)
All mothers
Other nervous system 20 1.00 1 4.99 (0.66, 37.47) 3 8.62 (2.54, 29.24)*** 3 1.09 (0.32, 3.68) 1 1.70 (0.23, 12.67)
Neural-tube defects 4 1.00 0 0 2 3.65 (0.67, 19.92) 0
External genital system 45 1.00 0 3 3.82 (1.18, 12.40)* 6 0.97 (0.41, 2.28) 0
Muscloskeletal and 143 1.00 4 2.52b (0.91, 6.92) 2 0.75b (0.19, 3.08) 33 1.61b(1.10, 2.36)* 4 0.93b (0.34, 2.53)
connective tissues
Eye 3 1.00 0 0 3 7.30 (1.47, 36.18)* 0
Heart 41 1.00 0 0 10 1.78 (0.89, 3.56) 3 2.49 (0.77, 8.08)
Ear 34 1.00 0 0 4 0.86 (0.30, 12.42) 0
Cleft lip with or without 11 1.00 0 0 0 0
palate Cleft palate 6 1.00 0 0 3 3.65 (0.91, 14.60) 0 Digestive system 9 1.00 0 1 6.33 (0.80, 50.21) 3 2.43 (0.66, 8.99) 1 3.77 (0.48, 29.85) Internal urogenital 44 1.00 1 2.02c(0.27, 14.85) 2 2.30c (0.55, 9.63) 5 0.81c (0.32, 2.05) 0 system Limbs 12 1.00 0 0 1 0.61 (0.08, 4.67) 1 2.83 (0.37, 21.81)
Mothers without diseasesd
Other nervous system 20 1.00 1 5.30 (0.71, 39.87) 3 8.50 (2.51, 28.84)*** 3 1.16 (0.33, 3.76) 1 1.74 (0.23, 12.01)
Neural-tube defects 4 1.00 0 0 2 3.72 (0.68, 20.35) 0
External genital system 45 1.00 0 2 2.50 (0.60, 10.38) 6 0.99 (0.42, 2.33) 0
Muscloskeletal and 138 1.00 3 2.33 (0.73, 7.42) 2 0.81 (0.20, 3.29) 28 1.52 (1.01, 2.29)* 3 0.75 (0.24, 2.38) connective tissues
Eye 3 1.00 0 0 3 7.45 (1.50, 36.96)* 0
Heart 38 1.00 0 0 10 1.96 (0.98, 3.95) 3 2.76 (0.85, 8.99)
Ear 33 1.00 0 0 4 0.90 (0.32, 2.55) 0
Cleft lip with or without 9 1.00 0 0 0 0
palate Cleft palate 5 1.00 0 0 2 2.98 (0.58, 15.37) 0 Digestive system 9 1.00 0 1 6.24 (0.79, 49.51) 3 2.48 (0.67, 9.18) 1 3.87 (0.49, 30.66) Internal urogenital 42 1.00 1 2.24c(0.30, 16.50) 2 2.34c (0.56, 9.81) 5 0.87c (0.34, 2.20) 0 system Limbs 10 1.00 0 0 1 0.74 (0.10, 5.82) 1 3.49 (0.45, 27.31) a Reference group. b Adjusted for parity.
pregnant women in Taiwan believed that taking asked whether or not they used herbal medicines, huanglian could help to provide the newborn, and then asked about frequency. In addition, we used a themselves, with a beautiful skin. A previous study structured questionnaire administered by well showed that pregnant women who gave birth to trained interviewers in order to collect data for the male infants seemed to experience more skin study. Thus, we hopefully minimised recall bias problems, such as polymorphic eruption or pruritic with regard to exposure information. There is, of folliculitis, because of hormonal effects from the course, the possibility of random misclassification fetus.[44] Interestingly, our data show that the sex
of exposure status, but this would not be expected to ratio of all births was higher in the group that took produce false-positive findings.
huanglian. The sex ratio was 128 : 105 for the group The pregnant women that participated in the taking huanglian and the group not taking huang- study were ≥26 weeks of gestation and only data lian, respectively. Thus, we suspect that the women relating to live born infants were analysed here. with male fetuses might have had more skin Spontaneous abortions or stillborn infants were not problems that drove them to take huanglian at an included. It is known that both these outcomes are
earlier stage of pregnancy. associated with high rates of congenital
malforma-As mentioned previously, traditional wisdom in tions and we recognise that any early effect of Taiwan is that An-Tai-Yin prevents spontaneous exposure on offspring who die will be missed. These abortion and indeed the name implies that in Chi- exclusions could result in a selection bias, but not nese. However, according to an ancient Chinese one that produces a false-positive result. Rather, book,[45] the main effect of An-Tai-Yin is to help
such a bias would result in an underestimation of the pregnant women deliver smoothly. Hence, the most true effect. In other words, our study, which includes appropriate time to use An-Tai-Yin is in the third only live births, may have underestimated the true trimester. Similarly, advice for using huanglian to effect of herbal medicines on the risk of congenital improve skin conditions is to take it in the second or malformations in all pregnancies.
third trimester. However, our results showed that
A limitation of this study was that we did not 11.4% and 1.5% of all pregnant women in the cohort
have the information of the newborns’ examination used An-Tai-Yin and huanglian, respectively,
dur-if they were not delivered at TMMCH, which was ing the first trimester. Our data also showed 95%
about 16% of the total. To minimise this effect we and 40% pregnant women who used huanglian and
linked the national death registration for the period An-Tai-Yin used it without a Chinese physicians’
during 1984–2003 and searched National Health prescription: they bought from Chinese herbal
drug-Insurance data for critical illnesses and injuries in stores by themselves or via their family. Clearly, any
the children occurring from 1996 to 2000. Because prevention strategy would need to involve an
educa-some congenital malformations might not be tion programme at the population level.
recognised until the late childhood or even teenage period, the above efforts actually identified 55 addi-Strengths and Limitations of the Study
tional cases. Thus, the potential selection bias of this study relating to missing data was also minimised to Prospective ‘exposure’ data collection during
some extent. pregnancy, before the outcome of pregnancy is
Another limitation when exploring the health ef-known, is recognised as the best method of
gather-fects of herbal products is the lack of product ing reliable data on herbal medicine use during
standardisation and quality assurance.[46] Besides
pregnancy. We interviewed our subjects in the third
the direct toxicity of herbal material, issues to con-trimester of pregnancy on their use of herbal
sider in any study include contamination by mi-medicines during the first trimester, before the
pres-crobes, heavy metals or pesticides, or even adultera-ence of malformations or the outcome of the
preg-tion with Western medicines, which may confound nancy was known. To reduce recall bias we firstly
4. Mone SM, Gillman MW, Miller TL, et al. Effects of environ-the potential herbal toxicity. This may have an
im-mental exposures on the cardiovascular system: prenatal peri-pact on the effects seen with herbal products. od through adolescence. Pediatrics 2004; 113: 1058-69
5. Li SJ, Ford N, Meister K, et al. Increased risk of birth defects In addition, the concept of the first trimester is
among children from multiple births. Birth Defects Res A Clin old fashioned now. We calculated the gestational Mol Teratol 2003; 67: 879-85
age from the first day of the last menstrual period; 6. Becker SM, Al Halees Z, Molina C, et al. Consanguinity and congenital heart disease in Saudi Arabia. Am J Med Genet thus, pregnant women are not pregnant during the
2001; 99: 8-13 first 2 weeks of gestation. The 3rd and 4th weeks
7. Carmichael SL, Shaw GM. Maternal life event stress and con-cover the pre- and implantation period of zygotes/ genital anomalies. Epidemiology 2000; 11: 30-5
8. Rasmussen SA, Moore CA, Paulozzi LJ, et al. Risk for birth blastocysts. There exists the ‘all-or-nothing effect’
defects among premature infants: a population-based study. J rule in the first gestational month. It means that the
Pediatr 2001; 138: 668-73
second and third gestational months are considered 9. Chuang CH, Lai JN, Wang JD, et al. Prevalence and related factors of Chinese herbal medicine use in pregnant women of as critical period for most major congenital
malfor-Taipei, 1985-1987. Taiwan J Public Health 2005; 24: 335-47 mations caused by environmental hazards.
Unfortu-10. Chuang CH, Lai JN, Wang JD, et al. Use of coptidis rhizoma nately, this study was designed in the 1980s. We did and foetal growth: a follow-up study of 9895 pregnancies.
Pharmacoepidemiol Drug Saf 2006; 15: 185-92 not have the data to separate the gestational weeks.
11. Goldbeck-Wood S, Dorozynski A, Lie LG, et al. Complementa-ry medicine is booming worldwide. BMJ 1996; 313: 131-3
Conclusion 12. Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA 1998; 280: 1569-75 We found evidence for a possible link between
13. Ni H, Simile C, Hardy AM. Utilization of complementary and the use of specific herbal medicines during the first alternative medicine by United States adults: results from the 1999 national health interview survey. Med Care 2002; 40: trimester of pregnancy and increased risk of specific
353-8 groups of congenital malformations. We could not
14. Nordeng H, Havnen GC. Impact of socio-demographic factors, investigate whether the adverse effect related to knowledge and attitude on the use of herbal drugs in
pregnan-cy. Acta Obstet Gynecol Scand 2005; 84: 26-33 direct toxicity of herbal medicines, from misuse or
15. Nordeng H, Havnen GC. Use of herbal drugs in pregnancy: a contamination, or from uncontrolled confounding.
survey among 400 Norwegian women. Pharmacoepidemiol These findings indicate that further research is Drug Saf 2004; 13: 371-80
16. Tiran D. The use of herbs by pregnant and childbearing women: needed in this area. Nonetheless, we would advise
a risk-benefit assessment. Complement Ther Nurs Midwifery caution regarding their use during the first trimester
2003; 9: 176-81
of pregnancy. 17. Tsui B, Dennehy CE, Tsourounis C. A survey of dietary
supple-ment use during pregnancy at an academic medical center. Am J Obstet Gynecol 2001; 185: 433-7
Acknowledgements
18. Gibson PS, Powrie R, Star J. Herbal and alternative medicine use during pregnancy: a cross-sectional survey. Obstet
This study was supported by grants (BHP-PHRC-92-4 Gynecol 2001; 97 Suppl. 1: S44-5
and DOH93-HP-1702) from the Bureau of Health Promotion, 19. Pinn G, Pallett L. Herbal medicine in pregnancy. Complement Ther Nurs Midwifery 2002; 8: 77-80
Department of Health, Taiwan.
20. Koren G, Pastuszak A, Ito S. Drugs in pregnancy. N Engl J Med
The authors have no conflicts of interest that are directly
1998; 338: 1128-37
relevant to the content of this study.
21. Lacroix I, Damase-Michel C, Lapeyre-Mestre M, et al. Prescrip-tion of drugs during pregnancy in France. Lancet 2000; 356: 1735-6
References
22. Hansan WF, Peacock AE, Yankowitz J. Safe prescribing prac-1. Anthony S, Kateman H, Brand R, et al. Ethnic differences in
tices in pregnancy and lactation. J Midwifery Womens Health congenital malformations in the Netherlands: analyses of a
2002; 47: 409-21 5-year birth cohort. Paediatr Perinat Epidemiol 2005; 19:
23. Malm H, Martikainen J, Klaukka T, et al. Prescription of haz-135-44
ardous drugs during pregnancy. Drug Saf 2004; 27: 899-908 2. Kalter H. Teratology in the 20th century: environmental causes
24. Andrade SE, Gurwitz JH, Davis RL, et al. Prescription drug use of congenital malformations in human and how they were
in pregnancy. Am J Obstet Gynecol 2004; 191: 398-407 established. Neurotoxicol Teratol 2003; 25: 131-282
3. Hoffmann W. Fallout from the Chernobyl nuclear disaster and 25. Gallo M, Sarkar M, Au W, et al. Pregnancy outcome following congenital malformations in Europe. Arch Environ Health gestational exposure to Echinacea: a prospective controlled
26. Simpson M, Parsons M, Greenwood J, et al. Raspberry leaf in 39. World Health Organization. General guidelines for methodolo-pregnancy: its safety and efficacy in labor. J Midwifery gies on research and evaluation of traditional medicines. Gene-Womens Health 2001; 46: 51-9 va: World Health Organization, 2000: 27 (document reference
WHO/EDM/TRM/2000.1) 27. Mabina MH, Pitsoe SB, Mood LJ. The effect of traditional
medicines on pregnancy outcome. The King Edward VIII 40. Eurocat. Eurocat guide 1.2: instructions for the registration of Hospital experience. S Afr Med J 1997; 87: 1008-10 congenital anomalies. Northern Ireland: Eurocat Central
Reg-istry, 2002 28. Murphy PA. Alternative therapies for nausea and vomiting of
pregnancy. Obstet Gynecol 1998; 91: 149-55
41. Maldonado G, Greenland S. Simulation study of confounder-29. Conover EA. Over-the-counter products: nonprescription medi- selection strategies. Am J Epidemiol 1993; 138: 923-36
cations, nutraceuticals, and herbal agents. Clin Obstet Gynecol
42. Directorate-General of Budget, Accounting & Statistics. Man-2002; 45: 89-98
power statistic annual report, 2004. Census Bureau, Director-30. Price CJ, George JD, Marr MC, et al. Developmental toxicity ate-General of Budget, Accounting & Statistics (DGBAS), evaluation of berberine chloride dehydrate (BCD) in Sprague- Taiwan, 1985-7 [online] [in Chinese]. Available from URL: Dawley (CD) rats [abstract]. Teratology 2001; 63: 279
http://www.dgbas.gov.tw/census~n/four/yrtable4,5,13.xls 31. Chan LY, Chiu PY, Lau TK. An in-vitro study of ginsenoside [Accessed 2005 Jan 1]
Rb1-induced teratogenicity using a whole rat embryo culture
43. Chen PC, Fu WL, Wang TR. Congenital malformation statistics model. Hum Reprod 2003; 18: 2166-8
in Taiwan, 1993. Taipei, Taiwan: Department of Health, The 32. Tzeng CR, Yang LL, Chien LW, et al. Effect of traditional Excusive Yuan/National Taiwan University Hospital, 1995
Chinese medicine on mouse embryo development. J Taipei
44. Vaughan Jones SA, Hern S, Nelson-Piercy C, et al. A prospec-Med Coll 1993; 22: 43-6
tive study of 200 women with dermatoses of pregnancy corre-33. Cosyns JP. Aristolochic acid and Chinese herbs nephropathy: a
lating clinical findings with hormonal and immunopathologi-review of the evidence to date. Drug Saf 2003; 26: 33-48
cal profiles. Br J Dermatol 1999; 141: 71-81 34. Penson RT, Castro CM, Seiden MV, et al. Complementary,
45. Fu Q-Z, Yang S-Z, Liu D-W. Fu Qing-zhus gynecology. Boul-alternative, integrative, or unconventional medicine?
Oncolo-der, (CO): Blue Poppy Press, 1999 gist 2001; 6: 463-73
46. Wen KC. The turnover rate of marker constituents in Chinese 35. Angell M, Kassirer JP. Alternative medicine: the risks of
untest-ed and unregulatuntest-ed remuntest-edies. N Engl J Muntest-ed 1998; 339: 839-41 herbal medicines. J Food Drug Anal 2000; 8: 270-7 36. Ko RJ. Adulterants in Asian patent medicines. N Engl J Med
1998; 339: 847
Correspondence and offprints: Dr Pau-Chung Chen, Insti-37. Ernst E. Adulteration of Chinese herbal medicines with
synthet-tute of Occupational Medicine and Industrial Hygiene, ic drugs: a systemic review. J Intern Med 2002; 252: 107-13
National Taiwan University College of Public Health, 17 38. World Health Organization. WHO traditional medicine strategy
Syujhou Road, Taipei 100, Taiwan. 2002-2005. Geneva: World Health Organization, 2002