Outcome Analysis of Arterio-venous Fistula in
Taiwan by National Health Insurance
Research Database (NHIRD) 1996-2001
Chung-Yih Yan , Chi-Min Pu , Tit-Kwok Lee, Jiau-Min Wong#,
I-Jen Chiang*, Charles C.H. Liu*#, Shiuh-Yen Lu, Simon Jui-Hsing Wu
Cathay General Hospital
*Graduate Institute of Medical Informatics, Taipei medical University #Institute of Biomedical Engineering, National Taiwan University
This study reports the outcome and revision history after arterio-
venous fistula operations in Taiwan by case linkage in the National
Health Insurance Research Database (NHIRD) from 1996 to 2000. 1520
patients with confirmed clinical details of arterio-venous fistulae were
queried from the 1/20-sampled hospitalization dataset, then the subsequent
revision operations were traced in the whole non-sampled database. The
methodology of follow-up study in NHIRD was validated by the consistent
patterns of vascular events selected by either loose or strict criteria of the
ICD procedural codes.
The primary patency rate by the hospitalization data was between
90.56% and 81.78%. The overall A-V fistula patency rate is 80% in the
first year, 72% in the second, and 66% in the third year. If revisions at
the outpatient service were added, the revision rate would double, but
the outpatient data was unreliable due to obscure ICD information. Our
methodology yielded consistent shapes of survival curves and the two
peaks of re-operations, the latter of which might be events after re-do
shunts. Freshness of the cases could be studied by the previous vascular
history in NHIRD. The revision rates are 16.37% and 27.71% for fresh
and non-fresh arterio-venous fistula respectively. (J Plast Surg Asso
R.O.C. 2004;13:80~89)
Key word: arterio-venous fistula, dialysis access, claim database,
population-based study
Introduction
The number of patients dependent on hemodialysis has steadily increased, with an
estimated 31,000 persons in Taiwan currently requiring long-term hemodialysis and more than two thousands of cases increased annually. Arterio-venous fistula (A-V fistula)
operation becomes the most performed operation of our reconstructive microsurgery team in Cathay General Hospital; about 150 to 200 fistulas are carried out annually. Care of patients with end-stage renal disease has considerable economic burden to health insurance systems both in Taiwan and USA. Currently, the cost exceeds 1 billion US dollars and access related hospitalization accounts for 25% of all hospital admissions in the USA.Up to 17% total spending for hemodialysis per patient per year is associated with hemodialysis access- related morbidity.1 Continuous care and repeated interventions are necessary to maintain A-V fistula patency. Quality assurance is especially important in the surgical intervention of this chronic disease. However, there are no population-based data available in Taiwan as the reference standards for quality management and improvement.
To understand the course of fistula patency and subsequent revisions, we drilled into datasets from the National Health Insurance Research Database (NHIRD) in Taiwan. The methodology of case follow-up and differentiation between fresh and revision cases would also contributed to other clinical studies of surgical procedures.
Materials and Methods
National Health Insurance Research Database (NHIRD, http://www.nhri.org.tw/ nhird/) covers 96% of population in Taiwan. Patient with “major diseases” (重大傷病) were nearly completely included in NHI, and follow-up study of these subject would be more convincing.
Patient selection and the primary fistula operation
Based on the confirmed patients selected in the 1/20 sampled hospitalization database (SDD dataset) with more clinical information (DO dataset) including the detailed medical orders, we could further explore the non- sampled complete “major disease” (重大傷病) dataset for the outcome after the confirmed vascular access operation, or explore the past history to differentiate between fresh and re- do cases. The non-sampled, complete “major diseases” (重大傷病) hospitalization (DD) and outpatient (CD) datasets were used for tracing the clinical course of these selected patients. The clinical details of non-sampled datasets are mainly derived from the five ICD diagnostic fields and the five ICD procedural fields, and could only be partly confirmed by the associated fee claims in different administrative categories. The clinical information in the latter (DD, CD) is relatively ambiguous, and should be used with reservation.
NHI procedure code “69032B” was the main criteria of inclusion of patients with A-V fistula operation. 1520 cases were found in the 1/20-sampled hospitalization datasets from 1996 to 2000 with detailed ICD diagnostic and operation codes.
Another 26 cases in the 1/500-sampled outpatient datasets were included in this study, but the outpatient data was used cautiously as reference data only due to small case numbers.
Considering the sampling rate of 1/20 and 1/500 for inpatient and outpatient datasets, the true case numbers performed in the 4 years were 30,760 and 13,000. The
中華整形外科醫誌:民國 93 年/13 卷/2 期
latter should be used with conservation due to large variation.
Follow-up and criteria of queries for vascular events
We followed-the clinical course of these 1520 inpatient and 26 outpatient cases in complete “major disease” (重大傷病) datasets 1996-2001. We use ICD-OP-Code to identified revision vascular operations according to different search strategy. By loose criteria, we identified that 664 redo or revision operations had been performed in 419 patients. Multiple revisions were performed in 142 patients.
Three query criteria were used for the database search of vascular events after the primary operation. The strict, the moderately strict, and loose selection were illustrated in Table 1. Strict selection used only the 392.7 ICD-op-code (dialysis arteriovenotomy) for the query; moderately strict selection searched for various vascular revision procedures of ICD-codes 394 and 395; loose selection searched for ICD-op-codes 392.7, 394, and 395, and included related vascular procedures scattered in 393, 393.0, 393.1, 393.2. The details of the ICD-op-codes were listed in Table 1.
In our analysis, the three selections yielded consistent occurrence patterns of vascular events after the primary fistula operation. For the clarity of presentation, only the two extreme selections (strict and loose) were shown in the result section if not specified.
Statistics
The non-freshness of cases was determined by the presence of related ICD-OP- Code in the past history before the SDO confirmed events. Loose criterium was used (Table 1).
The NHIRD data was kept in an Oracle data warehouse. Data of the selected cases was prepared in Microsoft Access database for further processing and queries. The statistical analyses were performed in SPSS 10.0 and Statistica 6.0 package.
Results
Characteristics of patients and the primary fistula operation
Average age of the patients was around 60 years old (Table 2). The age distribution of single peak with right skew pattern was illustrated in Fig. 1. The incidence increased from 30s, steadily to the peak of 60s, then dropped. The distributions were stable over 1997 and 2000. The case number in 1996 was too small (22 patients) and should not be used for comparison.
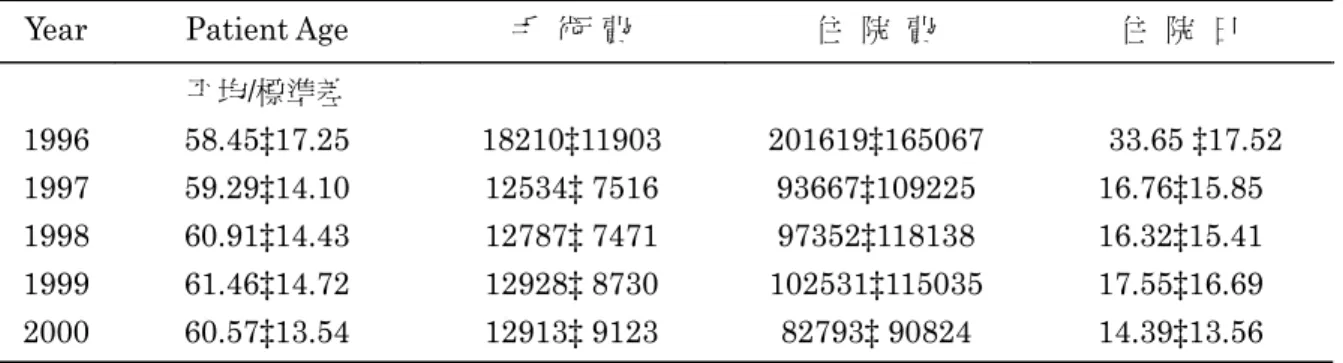
Male and female were equally 760 and 759. The sex was unknown in 1 patient. Average length of stay, the total operation fees, and the ward expenses in the whole hospitalization periods were listed in Table 2.
The patients were mostly admitted to medical departments (1076 cases). As for the surgical departments involved, 217, 114, 19 patients were served by the departments of general surgery, of vascular surgery, and of plastic surgery. 94 patients were unspecified of their departments (Table 3).
Since the cases were derived from inpatient dataset, the numbers managed in medical centers (醫學中心), regional hospitals (區域醫院), and local hospitals (地區醫院) were 639, 564, and 313, respectively.
The vascular revision events
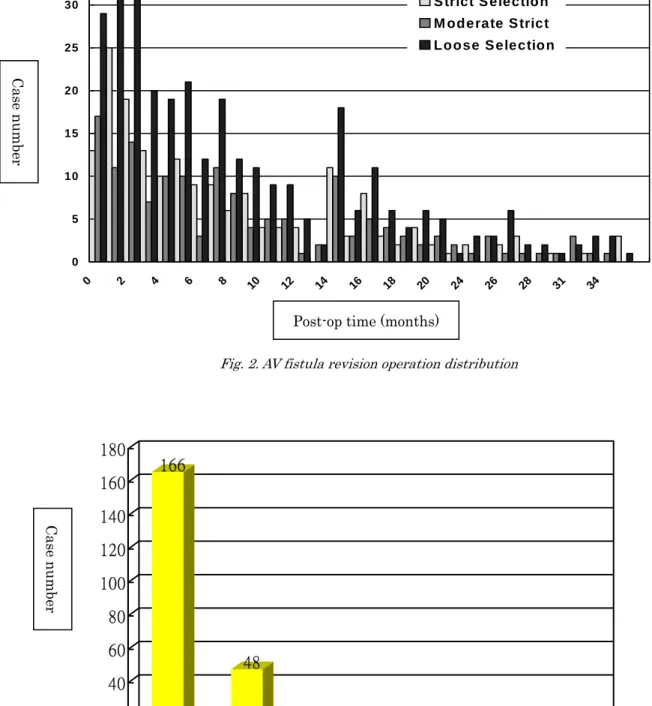
The vascular revision events after the primary fistula operation were illustrated by
the number of events versus the interval to the primary operation (Fig. 4).
The intervals between primary and revision fistula operation were analyzed in Fig. 2. We found there was constant distribution of the revision events between the three stricter or looser selection criteria, which confirmed the validity of our follow-up methodology in the insurance claim database.
Another significant finding was the “two peaks” of revisions. The frequency of revisions dropped rapidly after the third months after the primary fistula, but in the 15th post- operative months, the incidence of revisions increased to the level 6 – 8 months ago. The 316 events occurred in only 229 cases. 63 patients received multiple revisions in the follow-up period. The total number of revision operations for each patient was listed in Fig. 3. 48 patients received two revisions, and 10 patients, three revisions, and 5 patients, more than four revisions.
Primary patency rate and the freshness and age effects
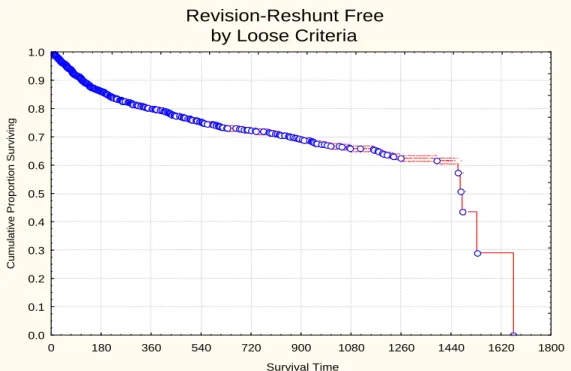
For calculation of the primary patency rate, we only count the first revision for each
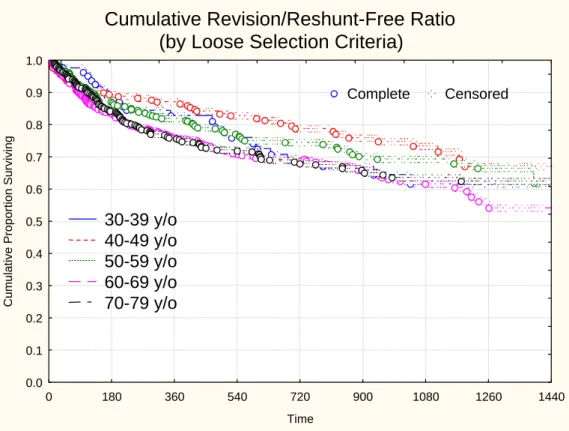
patient in the subsequent presentations. The survival curves of cumulative proportion methods were drawn for all cases, for the fresh cases versus non-fresh cases, and for different age groups.
We found the crude revision rate of all cases in the 4-year study period was between 9.41% and 18.22%, according to the strict or loose criteria of the ICD procedural codes. Hospitalization with one of the major diagnoses as vascular related cause was considered very strong suggestion of vascular thrombosis. We think it is more adequate for calculation of primary patency rate. Data from loose criteria were used for survival analysis.
We analyzed primary patency of A-V fistula operation as revision-free survival time in Fig. 4. The overall patency rate is 80% in the first year, 72% in the second, and 66% in the third year. The survival curves were also different in fresh and non-fresh cases (Fig. 5). The 2-year patency rates were 75% and 61% for fresh and non-fresh cases. Survival of different age groups was shown in Fig. 6. Age group 40-49 year-old was significantly better than the other groups.
Table 1. NHI ICD-op-code selection for AV fistula revision operation
STRICT SELECTION
3927 DIALYSIS ARTERIOVENOSTOM LOOSE SELECTION
393 SUTURE OF VESSEL* 3930 SUTURE OF VESSEL NOS 3931 SUTURE OF ARTERY 3932 SUTURE OF VEIN
394 VASC PROCEDURE REVISION* 3941 POSTOP VASC OP HEM CONT 3942 REVIS REN DIALYSIS SHUNT
3943 REMOV REN DIALYSIS SHUNT 3949 VASC PROC REVISION NEC 395 OTHER VESSEL REPAIR* 3950 ANGIO/ATH NON-CORO VES 3951 CLIPPING OF ANEURYSM 3952 ANEURYSM REPAIR NEC 3953 ARTERIOVEN FISTULA REP
3954 RE-ENTRY OPERATION
3955 REIMPLAN ABERR RENAL VES 3956 REPAIR VESS W TIS PATCH 3957 REP VESS W SYNTH PATCH 3958 REPAIR VESS W PATCH NOS
中華整形外科醫誌:民國 93 年/13 卷/2 期
Table 2. AV fistula patient database analysis
Year Patient Age 手 術 費 住 院 費 住 院 日
平均/標準差 1996 58.45‡17.25 18210‡11903 201619‡165067 33.65 ‡17.52 1997 59.29‡14.10 12534‡ 7516 93667‡109225 16.76‡15.85 1998 60.91‡14.43 12787‡ 7471 97352‡118138 16.32‡15.41 1999 61.46‡14.72 12928‡ 8730 102531‡115035 17.55‡16.69 2000 60.57‡13.54 12913‡ 9123 82793‡ 90824 14.39‡13.56
Table 3. Admitted department of AV fistula patient
Internal Medicine 內科 600 Nephrology 腎臟內科 476 Surgery 外科 217 Cardiovascular Surgery 心臟血管外科 114 Plastic Surgery 整形外科 19 Others 其他科 94 Cas e number Age groups
0
20
40
60
80
100
120
10-20 y/o 20-30 y/o 30-4 0 y/o 40-50 y/o 50-60 y/o 60-70 y/o 70-80 y/o 90-00 y/o 10-20 y/o 1996 1997 1998 1999 20000 5 10 15 20 25 30 35 0 2 4 6 8 10 12 14 16 18 20 24 26 28 31 34 S trict S electio n M od erate S trict Loose S electio n
Post-op time (months)
Case number
Fig. 2. AV fistula revision operation distribution
Fig. 3. Analysis of multiple revision cases Total number of revisions
Case number 166 48 10 3 1 1 0 20 40 60 80 100 120 140 160 180 1 2 3 4 5 6
中華整形外科醫誌:民國 93 年/13 卷/2 期
Fig. 5. Survival curve of fresh/non-fresh fistula operation Fig. 4. Survival curve of primary fistula operation
Revision-Reshunt Free
by Loose Criteria
0 180 360 540 720 900 1080 1260 1440 1620 1800 Survival Time 0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0 Cum ulative Proportion Surviving
Cumulative Revision/Reshunt Free Ratio
Fresh vs NonFresh Cases
0 180 360 540 720 900 1080 1260 1440 Time 0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0
Cumulative Proportion Surviving
Complete Censored
Fresh Cases
NonFresh Cases
Discussions
This research is the first outcome analysis of AV fistula operation in Taiwan based on insurance claim database. Since NHI covers 96% of population, and end-stage renal disease (ESRD) is one of the “major diseases” (重大傷病) included in the initial setup of NHI, the high recruitment rate and coverage of various practice patterns of different hospitals are the most valuable part of this study. The data before year 2001 also avoid the effect of total budget control (總額預算). The other contribution of this study is validation of the methodology of case follow-up in insurance claim database by the relatively homogeneous problem of the subsequent vascular revisions. The different
selection criteria by strict or by loose sets of ICD procedural codes yielded consistent distribution of events, and suggested a stable underlying biological process. Although the study of NHRID is limited by the more detailed clinical procedures in inpatient datasets than in outpatient datasets, the large case base and the inclusion of various practice patterns of all hospital types still makes this methodology important for follow- up study of surgical disease or procedures. This data is limited mainly to the inpatients. The proportion performed in the medical center may be exaggerated. Accordingly, the severity of disease and the associated disease may be aggravated. Both factors may affect the patency rate and increase the complications, medical expenses, and length of hospital stay.
Fig. 6. Survival curve of primary fistula operation in different age groups
Cumulative Revision/Reshunt-Free Ratio
(by Loose Selection Criteria)
0 180 360 540 720 900 1080 1260 1440 Time 0.0 0.1 0.2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0
Cumulative Proportion Surviving
Complete Censored
30-39 y/o
40-49 y/o
50-59 y/o
60-69 y/o
70-79 y/o
中華整形外科醫誌:民國 93 年/13 卷/2 期
In addition to the inpatient-only approach, there are other limitations inherent in the secondary use of insurance claim database for clinical study such as ICD-only informa- tion and no control group.
Feldman et al. analyzed Medicare datasets and found that 15 to 16% of hospital stays among prevalent ESRD patients were associated with vascular access-related morbidity. They also found that women, blacks, the elderly, and diabetics appear to be at particularly high risk3. In our study, elder age and previous vascular procedure are risk factors for fistula revision, but sex and diabetics are not.
Failures of native fistulae usually occurred early in the postoperative period, secondary to attempts to use inadequate veins. 5 This may explain the first revision peak in 1-3 months after primary operation of our study. Thrombosis caused the secondary A-V fistula failures and was generally the result of venous stenosis. This may explain the second peak in 14-16 months.
Woods et al. used Medicare datasets to identify access failures or revisions among patients with A-V fistula or graft, and found that the relative risk of access failure for a patient with an AV fistula, compared with a patient of the same age with an AV graft, was 67% lower at the age of 40 years, 54% lower at the age of 50 years, and 24% lower at the age of 65 years.2 We tried to separate graft use from native fistula in the NHIRD, but not yet success due to no suitable code can be used to present graft use. We are working on it in our incoming studies.
Conclusion
By inpatient follow-up data, we concluded primary patency rate of AV fistula was between 90.56% and 81.78%. By loose criteria, the overall A-V fistula patency rate is 80% in the first year, 72% in the second, and 66% in the third year. If revisions at the outpatient service were added, the revision rate would double. The revision rates are 16.37% and 27.71% for fresh and non-fresh AV fistula respectively.
We demonstrate the validity of follow-up methodology in the claim database by ICD- code selections. The events before the primary surgery could help the differentiation between freshness of cases.
Reference
1. Hakim, Raymond, Himmelfarb, Jonathan. Hemodialysis access failure: A call to action. Kidney International. October 1998;54(4):1029- 1040.
2. Woods JD, Turenne MN. Vascular access survival among incident hemodialysis patients in the United States. Am J Kidney Dis. 1997 Jul;30(1): 50-7.
3. Feldman HI, Held PJ. Hemodialysis vascular access morbidity in the United States. Kidney Int. 1993 May;43(5):1091-6.
4. Bacchini, Giuseppe. Locatelli, Francesco. Survival of Prosthetic Grafts of Different Materials after Impairment of a Native Arteriovenous Fistula in Hemodialysis Patients. ASAIO Journal, January 2001;47(1):30-33.
5. Palder SB, Kirkman RL, Whittenmore AD et al. Vascular access for hemodialysis. Ann Surg, 1985; 202:235–239.
6. Brescia MJ, Cimino JE, Appel K et al. Chronic hemodialysis using venipuncture and asurgically created arteriovenous fistula. N Engl J Med, 1966;275:1089–1092.
7. Joseph, Swapna MD. Adler, Stephen MD. Vascular Access Problems in Dialysis Patients:
Pathogenesis and Strategies for Management. Heart Disease. July/August 2001;3(4):242-247. 8. Kinnaert P, Vereerstreaeten P, Toussaint C et al.
Nine years’ experience with internal AV fistulas for hemodialysis: a study of some factors influencing the results. Br J Surg 1977;64:242– 246.
9. Lee JJ, Liu CCH, Wu SJH et al. Overview of Extremity Replantation in Taiwan by the
National Health Insurance Database from 1996 to 2000. J Plast & Reoonstr Surg Asso ROC. 2001;10(4):217-230.
10. Yang YJ, Liu CCH, Wu SJH et al. Epidemiology of Burn Injury in Taiwan by the National Health Insurance Database. J Plast & Reoonstr Surg Asso ROC. 11(4), 2002.
11. National Health Insurance Research Database (NHIRD, http://www.nhri.org.tw/ nhird/)
Reprints request from: Dr. Chung-Yih Yan M.D.
Division of plastic surgery, Cathay General Hospital, Taipei, Taiwan Address: 280, Sec. 4, Jen-Gi Rd, Taipei 106, Taiwan
Tel and Fax: 886 2 2708 2121 ext 8810, 886 2 2708 9995