A retrospective survey of patients with malignant gliomas treated in the neuro-oncological care system under the Universal National Health Insurance program in Taiwan
Yin-Cheng Huanga,
Kuo-Chen Weia,
Chin-Hong Changb,
Jen-Tsung Yangc,
Jih-Tsun Hod,
Chiung-Chyi Shene,
Chain-Fa Suf,
Der-Yang Chog,
Hsin-I Mah,
Jia-Wei Lini,
E-Jian Leej,
Jionn-Jong Wuk,
Ming-Dar Tsail,
Cheng-Kuei Changm,
Shen-Long Howngn,
Chen-Nen Changa, ,
a Department of Neurosurgery, Chang Gung Memorial Hospital at Linkou & Chang Gung University, Taoyuan, Taiwan
b Department of Neurosurgery, Chi Mei Medical Center, Tainan, Taiwan
c Department of Neurosurgery, Chang Gung Memorial Hospital, Chia-Yi, & Chang Gung University, Tao-Yuan, Taiwan
d Department of Neurosurgery, Chang Gung Medical Foundation, Kaohsiung Branch, Taiwan
e Department of Neurosurgery, Taichung Veterans General Hospital, & School of Medicine, National Yang-Min University, Taipei, Taiwan
f Department of Neurosurgery, Buddhist Tzu Chi General Hospital-Hualien Tzu Chi Medical Center, & Tzu Chi University, Hualien, Taiwan
g Department of Neurosurgery, China Medical University, China Medical University Hospital, Taichung, Taiwan
h Department of Neurosurgery, Tri-Service General Hospital, National Defense Medical Centre, Taipei, Taiwan
i Department of Neurosurgery, Shuang-Ho Hospital – Taipei Medical University, Taiwan
j Department of Neurosurgery, National Cheng Kung University Medical Hospital, Tainan, Taiwan
k Department of Neurosurgery, Far Eastern Memorial Hospital, Taipei, Taiwan
l Department of Neurosurgery, Shin Kong Wu Ho-Su Memorial Hospital, Fu-Jen Catholic University, Taipei, Taiwan
m Department of Neurosurgery, Mackay Memorial Hospital, Graduate Institute of Injury Prevention and Control, Taipei Medical University, Taipei, Taiwan
n Department of Neurosurgery, Kaohsiung Medical University Hospital, Taiwan
Abstract
In 1995 a government-supported Universal National Health care system was implemented in Taiwan, which in 2008 was available to 98% of the population.
This system offers affordable, rapid medical attention. A multi-center retrospective study was conducted to assess the prognosis of malignant glioma patients under this system. In 2005 and 2006, patients at 14 independent neuro- oncology centers with newly diagnosed malignant glioma were enrolled. The patient profile, pathology, treatment modalities, and prognosis were collected by questionnaire at each center. The Taiwan Neuro-Oncology Society was responsible for the data analysis. The overall median survival period, 1-year survival rate, and 2-year survival rate for patients with World Health Organization grade III glioma were 33.8 months, 81.4%, and 58.2%, respectively, and 15 months, 57.3%, and 33.9% in patients with grade IV glioma. The median survival period, 1-year survival rate, and 2-year-survival rate in patients receiving temozolomide adjuvant therapy was 36 months, 84.2%, and 61.8%, respectively, for patients with grade III glioma and 19.8 months, 73.1%, and 43.7%, for patients with grade IV glioma. The universal health care system in Taiwan offers a comparable prognosis with an affordable premium relative to other large series in developed countries.
Keywords
Chemotherapy;
Malignant glioma;
Radiation therapy;
Surgery;
Universal health insurance
1. Introduction
Insurance policy has a great impact on the medical care system. Taiwan established a universal health policy system in 1995 that was available to almost 98% of 23 million people in 2008.1 An overall improvement in health compared to pre-1995 has been reported.2 It is also critical to examine this system with respect to oncology care quality, due to the high cost and poor prognosis associated with cancer.
Malignant gliomas are a common primary malignancy with a grave prognosis.
According to a multi-center prospective study.3 the expected survival is about 2 years for patients with World Health Organization (WHO) grade III tumors and 1 year for those with grade IV tumors. Few series have been published describing the details of glioma treatment strategies and prognosis in Taiwan,[4], [5] and [6]
especially under the universal health care system. The goal of this study is to evaluate the prognosis of patients newly diagnosed with malignant glioma between 2005 and 2006. Although Taiwan has a relatively low gross national product, it provides a low insurance premium and unlimited lifetime medical coverage, offering affordable health care.
The Taiwan Neuro-Oncology Society, founded in 2006, appreciates the importance of nationwide multi-center surveys for future health improvements. Our society is the first in Taiwan to attempt a retrospective study to obtain a basic profile of treatment modalities and prognoses for glioma patients. This multi-center, retrospective study collected information on the versatile treatment strategies and patient outcomes in 14 independent medical centers in Taiwan for patients with malignant glioma.
2. Methods and materials
The insurance plan under this medical care system is universal and lacks maximal lifetime limits; no limitations regarding previous existing illnesses are imposed, and the differential premium is determined by monthly income, ranging from 20 to 200 US dollars (USD) per month. There is a 10% co-payment for hospitalized patients; however, for patients with confirmed malignancy, all medical costs, including surgery, chemotherapy and radiation therapy, are waived. The referral to the tertiary medical center is encouraged but not enforced. In short, this health
care system encourages patients to receive extensive and multi-modal treatments.
More than half (14 out of 25) of the neurosurgical centers in Taiwan participated in this study. The enrolment criteria were patients newly diagnosed with WHO grade IV and III malignant gliomas, including classic grade IV glioblastoma multiforme (GBM), anaplastic astrocytoma (AA), and anaplastic oligodendroglioma (AOG), as diagnosed by a certified pathologist at each center between 2005 and 2006. To obtain a full profile from each patient, those who did not receive follow-up were excluded from the database. Preoperative and consecutive postoperative imaging was mandatory and reviewed by radiologists.
The data were collected according to questionnaires completed by physicians in each center at the end of 2009. All the questionnaires were sent to the Taiwan Neuro-Oncology Society for data processing. For the protection of patient privacy, all identifiable personal information was removed at every institute, except for the variables necessary for this study. Inter-institutional comparisons were not included in this retrospective study.
This retrospective study was approved by the Institutional Review Board of every institute. The basic information for each patient included age, gender, preoperative Karnofsky performance scale (KPS) score, operative procedures, postoperative KPS score, radiation therapy, chemotherapy, re-operation, adjuvant therapy after re-operation, stabilization period, recurrence-free survival, survival after recurrence, and overall survival.
3. Results
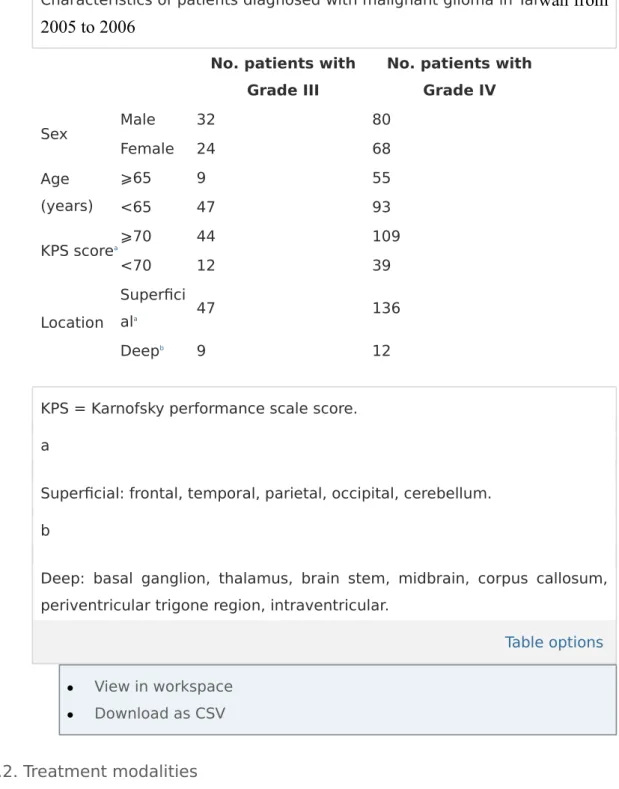
3.1. Demographic data
From 2005 to 2006, 204 patients newly diagnosed with malignant glioma were enrolled. There were 56 patients with grade III and 148 with grade IV glioma. The demographic data are listed in Table 1. The number of patients enrolled from each of the 14 participating institutes ranged from 2 to 44 (mean, 14.6 patients/center over 2 years). These institutes were geographically distributed throughout Taiwan, representing a low - bias patient source.
Table 1.
Characteristics of patients diagnosed with malignant glioma in Tai
wan from 2005 to 2006
No. patients with Grade III
No. patients with Grade IV
Sex Male 32 80
Female 24 68
Age (years)
⩾65 9 55
<65 47 93
KPS scorea⩾70 44 109
<70 12 39
Location
Superfici
ala 47 136
Deepb 9 12
KPS = Karnofsky performance scale score.
a
Superficial: frontal, temporal, parietal, occipital, cerebellum.
b
Deep: basal ganglion, thalamus, brain stem, midbrain, corpus callosum, periventricular trigone region, intraventricular.
Table options
View in workspace
Download as CSV
3.2. Treatment modalities
Although craniotomy followed by chemotherapy and radiation therapy is considered standard for the first complete treatment, there are variations that depend on the individual neuro-oncology team. During the 2 years of the study, new treatments such as temozolomide (TMZ), Gliadel® Wafer (polifeprosan 20 with carmustine implant, MGI Pharma, Maryland, USA), radiosurgery for a local booster, immunotherapy, and carmustine were attempted in certain patients. The multi-disciplinary modalities are listed in Table 2.
Table 2.
Treatment modalities of all patients diagnosed with malignant glioma in Taiwan from 2005 to 2006
Grade III (n = 56
)
Grade IV (n = 14
8)
Surgery 5 18
Surgery + external radiationa 19 42
Surgery + radiation + chemotherapy 27 71
Adjuvant TMZb 9 41
CCRT TMZ 15 19
BCNUc 1 4
Gliadel 2 4
Gliadel+ adjuvant TMZd 2
CCRT TMZ + BCNU 1
Surgery + adjuvant TMZ 2 9
Surgery + radiation + immunotherapye 1 1
Surgery + radiation + immunotherapye + adjuvant TMZ 1 1
Surgery + radiosurgery 1 1
Surgery + radiation + radiosurgery + adjuvant TMZ 3 Surgery + radiation + radiosurgery + immunotherapye +
adjuvant TMZ 1
Radiation + adjuvant TMZ 1
a
External radiation: intensity modulated radiation therapy-based (IMRT).
b
TMZ = temozolamide, adjuvant and concomitant chemotherapy and radiation therapy (CCRT) protocol are described.9
c
BCNU = carmustine (150–200 mg/m2 every 6 weeks).
d
Gliadel® wafer.
e
Immunotherapy: dendritic cell-based autologous vaccination, a completed clinical trial including grade III and IV glioma.
Table options
View in workspace
Download as CSV
The extent of surgical resection was recorded according to the answers on the questionnaire form. The gross total resection rate was 48.2% in patients with grade III and 53.3% in patients with grade IV glioma. A stereotactic navigation system, which helps to increase the extent of resection, was used in about 25% of the surgical procedures.
Of the patients with grade III glioma, 30 received chemotherapy (53.6%), as did 86 patients (58.1%) with grade IV glioma (Table 2). The modalities differed according to decisions made by the individual neuro-oncology team. An immunotherapy trial using dendritic cell-based tumor vaccines was attempted in two grade III and three grade IV patients during this period.
For external radiation treatment, 169 out of 204 patients (82.8%) received intensity-modulated radiation therapy. A total of six patients received gamma knife radiation for an initial local booster (one with grade III glioma, and five with grade IV glioma). In addition, the number of patients with a good KPS score (⩾70) dropped from 44 to 21 in patients with grade III glioma and 109 to 41 in patients with grade IV glioma after complete primary treatment (Supplementary Table 1), indicating the severity of glioma in these patients.
3.3. Stabilization and progression-free survival
The progression-free interval describes the median, 6-month and 12-month progression-free interval in different patient subgroups based on age, gender, baseline KPS score, and location (Table 3). For patients with grade III tumors, the median overall progression-free survival was 10.6 months, the 6-month progression-free rate was 67.8%, and the 12-month progression-free rate was 45.8%; for patients with grade IV tumors, the median overall progression-free
survival was 6.3 months, 6-month rate was 53.6%, and the 12-month rate was 21.3%, respectively. In a multiple regression analysis, it was shown that the extent of resection remained the main predictive variable for progression-free survival (Table 3).
Table 3.
Progression-free survival in patients with grade III and grade IV glioma in Taiwan from 2005 to 2006
No. patients with Grade III (n = 56;
progression = 46, 82.1%)
No. patients with Grade IV (n = 148;
progression = 124, 83.8%)
Progression events Progression events
Median (mths)
6 mths
(%) 12 mths
(%)
Median (mths)
6 mths
(%) 12 mths
(%)
Overall 10.6 67.8 45.8 6.3 53.6 21.3
Age ⩾65
years 7/9 7.4 53.2 26.7 81/93 6.8 55.9 22.3
<65 years
39/4
7 11.1 70.2 48.9 43/55 6.0 49.5 19.5
Sex Male 27/3
2 15.2 79.2 66.7 65/80 6.8 58.6 19.4
Female 19/2
4 6.5 59.1 29.5z 59/68 5.9 48 23
KPS ⩾70 34/4 11.1 72.7 49.2 93/109 6.6 55.3 21.6
No. patients with Grade III (n = 56;
progression = 46, 82.1%)
No. patients with Grade IV (n = 148;
progression = 124, 83.8%)
Progression events Progression events
Median (mths)
6 mths
(%) 12 mths
(%)
Median (mths)
6 mths
(%) 12 mths
(%)
score
baseline 4
<70 12/1
2 6.6 50 33.3 31/39 6.0 49.1 20.8
Location Superfici ala
40/4
9 15.2 82.4 58.8 114/13
8 6.5 57.4 57.4
Deepb 6/7 16 57.1 38.1 10/10 3.4 30 30
Cox regression model for progression-free survival
Progression events Grade III
Progression events Grade IV
Simple model
Multiple model
Simple model
Multiple model HR (95% CI) HR (95% CI)
Age ⩾65 vs. <65 years
0.70 (0.31–
1.58)
1.26 (0.50–
3.18)
0.94 (0.65–
1.36)
1.18 (0.77–
1.80)
Sex Male vs. female
0.57 (0.31–
1.02)
0.61 (0.30–
1.23)
1.02 (0.71–
1.45)
0.97 (0.68–
1.40) Baseline KPS
score ⩾70 vs. <70
0.47⁎ (0.24–
0.93)
0.43⁎ (0.21–
0.91)
0.96 (0.64–
1.44)
1.04 (0.67–
1.63) Extent of
surgery
Total resection vs.
partial + biopsy
0.62 (0.26–
1.48)
0.44 (0.16–
1.20)
0.70⁎ (0.49–
0.99)
0.59⁎ (0.41–
0.86)
ChemotherapycYes vs. no
0.88 (0.49–
1.57)
1.04 (0.55–
1.97)
0.46⁎ (0.32–
0.65)
0.41⁎ (0.28–
0.60)
CI = confidence interval, HR = hazards ratio, KPS = Karnofsky performance scale score, mths = months.
⁎
Statistically significant (p < 0.05).
a
Superficial: frontal, temporal, parietal, occipital, cerebellum.
b
Deep: basal ganglion, thalamus, brain stem, midbrain, corpus collosum, trigone, intraventericular.
c
Including any chemotherapy.
Table options
View in workspace
Download as CSV
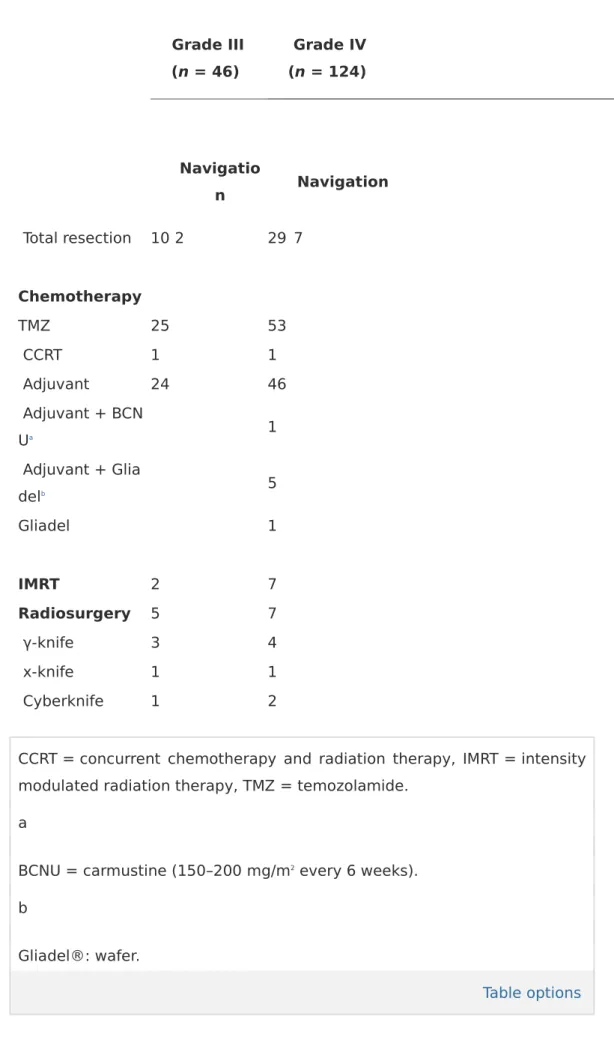
3.4. Treatment after recurrence
After tumor recurrence is confirmed with clinical and imaging studies, the therapy modalities (as opposed to those of primary treatment) are mainly re-operation, chemotherapy and booster radiation therapy (Table 4). For surgical methods, total resection was achieved in 10 of 46 patients with recurrent grade III glioma (21.7%), and 29 of 124 patients with recurrent grade IV glioma (23%). The navigation system was still used on about one-quarter of the re-operated patients.
Table 4.
Therapy modalities after tumor recurrence in patients diagnosed with malignant glioma in Taiwan from 2005 to 2006
Grade III (n = 46)
Grade IV (n = 124)
Navigatio
n Navigation
Surgery
All 16 4 38 9
Biopsy 0 0 1 1
Subtotal
resection 6 2 8 1
Grade III (n = 46)
Grade IV (n = 124)
Navigatio
n Navigation
Total resection 10 2 29 7
Chemotherapy
TMZ 25 53
CCRT 1 1
Adjuvant 24 46
Adjuvant + BCN
Ua 1
Adjuvant + Glia
delb 5
Gliadel 1
IMRT 2 7
Radiosurgery 5 7
γ-knife 3 4
x-knife 1 1
Cyberknife 1 2
CCRT = concurrent chemotherapy and radiation therapy, IMRT = intensity modulated radiation therapy, TMZ = temozolamide.
a
BCNU = carmustine (150–200 mg/m2 every 6 weeks).
b
Gliadel®: wafer.
Table options
View in workspace
Download as CSV
Chemotherapy with TMZ was prescribed in 54% of patients with grade III glioma and 42.7% of patients with grade IV glioma. Two patients with tumor recurrence received concurrent chemotherapy and radiation therapy (CCRT).
Some patients received local booster radiosurgery after recurrence due to the prior completion of radiotherapy. In total, 12 patients received radiosurgery (γ- knife, x-knife, or cyberknife) (Table 4).
3.5. Overall survival
For patients with grade III glioma, the median survival was 33.8 months, the 6- month survival rate was 81.4%, and the 12-month survival rate was 58.2%; for patients with grade IV glioma, the respective values were 15 months, 57.3%, and 33.9% (Table 5). A multiple regression analysis revealed that age (<65 years) and a baseline KPS score are positive prognostic factors for patients with grade IV glioma, but not for patients with grade III glioma. Patients with deep-seated tumors (thalamus, basal ganglion, brain stem) had a less favorable survival in either grade III or grade IV patients. Total excision may lead to longer survival (92.4% 1-year survival in grade III and 71.9% in grade IV; verified by simple and multiple regression models in Table 5). From 2005 to 2006, 53.6% of grade III and 58.1% of grade IV patients received initial chemotherapy. Due to the multi- disciplinary practice for patients receiving chemotherapy, the median survival period, 6-month survival rate, and 12-month survival rate are significantly higher than those for patients who did not receive chemotherapy (21.2 months, 73.3%, and 45.7% versus [vs.] 8.2 months, 33.1%, and 16.4%, respectively, p < 0.001).
Further delineating the treatment modalities, the survival period for patients who received Gliadel® did not differ compared to patients who did not receive it (1- year survival: 50% vs. 57%). However, either with CCRT TMZ or adjuvant TMZ, survival was significantly prolonged compared to those without TMZ (1-year- survival, 80.7%, 70.2% vs. 38.5%; p < 0.001).