Life-threatening Cytomegalovirus-Induced Interstitial Pneumonitis in A Patient of Membranous Glomerulonephropathy with
Short-term Immune-Suppressant Therapy
Yen-Chung Lin
1, and Der-Cherng Tarng
2,31
Division of Nephrology, Department of Medicine, Su-Ao Veterans Hospital;
2
Division of Nephrology, Department of Medicine, Taipei Veterans General Hospital;
3
Department and Institute of Physiology, National Yang-Ming University, Taipei, Taiwan, R.O.C.
Abstract
Cytomegalovirus (CMV) disease is not uncommon upon an acquired immune compromised status like organ transplant recipients. However, the complication of short-term immunosuppressive therapy for non-transplant patients was not known very well. Here we reported a case of CMV pneumonitis presented with life threatening respiratory failure in a patient with diabetes and steroid-resistant membraneous glomer- ulonephropathy who underwent immunosuppressant therapy. Chest X-ray and high resolution computed tomography scan revealed interstitial pneumonitis over both lungs. A virus isolation culture of bronchoal- veolar lavage fluid and deoxyribonucleic acid polymerase chain reaction in peripheral blood showed positivity for CMV. After one month of ganciclovir therapy, the patient's symptoms improved and lung infil- tration resolved. However, post-infection sequela of severe restrictive lung disease occurred and oxygen therapy was maintained after his discharge. CMV lung infection may be mainly due to immune compromised status in the present case of diabetes, steroid-resistant glomerulopathy, and treatment with cyclosporine immunosuppressant. A high index of suspicion and early initiation of antivirus therapy are mandatory for the successful management of opportunistic CMV pneumonitis and the sequelae in patients receiving immuno- suppressive therapy. (J Intern Med Taiwan 2010; 21: 436-440)
Key words: Cytomegalovirus pneumonitis, Immunosuppressive therapy, Membranous glomerulone- phropathy
Introduction
Cytomegalovirus (CMV) infection is a frequent complication in patients who underwent organ transplantation. Most symptomatic CMV
infections are self-limited, but post-transplant graft dysfunction and new onset of diabetes mellitus or even severe fatal lung and gastrointestinal compli- cations have been reported. In review of the liter- ature, there is no CMV pneumonitis in non-trans-
Correspondence and requests for reprints : Dr. Der-Cherng Tarng
Address : Division of Nephrology, Department of Medicine, Taipei Veterans General Hospital and Department and Institute of Physiology, National Yang-Ming University, No. 201, Sec. 2, Shih-Pai Road, Taipei 112, Taiwan, R.O.C.
plant patients of primary glomerulonephropathy with immunosuppressant therapy. Herein, we report a case of diabetes and membranous glomerulone- phropathy presenting with fever and severe respi- ratory distress. CMV pneumonitis was confirmed when a virus isolation culture of bronchoal- veolar lavage (BAL) fluid and deoxyribonucleic acid (DNA) polymerase chain reaction (PCR) in peripheral blood showed positivity for CMV infection.
Case report
A 67-year-old Chinese man with newly diagnosed type 2 DM came to our hospital for help with the initial presentation of heavy proteinuria (7 g/day) and anasarca for more than half a year.
Initially, diabetic nephropathy induced stage III chronic kidney disease with an estimated creatinine clearance of about 36mL/min was presumed.
However, a renal biopsy was performed and the report showed stage II membranous glomerulo- nephropathy. The serology of the hepatic B and C markers, antinuclear antibody, rheumatoid factor, and syphilis VDRL were all negative, so secondary membraneous glomerulonephropathy was less likely. After several months of follow-up, oral methylprednisolone therapy (1 mg/kg) was prescribed and then cyclophosphamide was also added in order to lower the steroid dosage and side effects. However, the patient still suffered from lower leg edema and heavy proteinuria. Therefore, cyclosporine (200 mg/day) was chosen as rescue therapy and methylprednisolone and cyclophos- phamide were discontinued at the same time. He responded well to the cyclosporine therapy and urinary protein excretory rate decreased from 14 g/
day to 2.6 g/day within one month. Unfortunately, he developed progressive shortness of breath and excertional dyspnea and was sent to our emergency department for help.
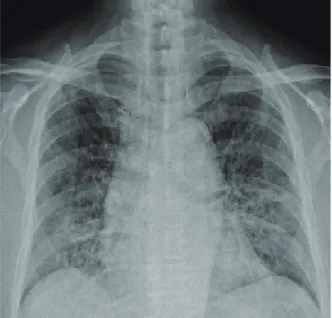
Physically, diffuse moist crackles were found
bilaterally and chest plain film showed interstitial infiltrations over both lung fields (Fig.1). Initially, congestive heart failure was highly suspected;
however, fluid overload and cardiomegaly were less evident. Later on, fever and severe hypoxemia developed. Besides, ground glass opacities in bilateral lung parenchyma were shown by high resolution computed tomography (HRCT) of the chest (Fig.2). White blood cell count was normal but shifted to the left. There was no thrombocy- topenia or elevation of the creatine kinase level.
Finally, rapid progressing interstitial pneumonitis
Fig. 1. Cytomegalovirus pneumonitis. Bilateral reticulo- interstitial infiltrations especially at lower lung fields shown in chest X-ray film.
Fig. 2. Cytomegalovirus pneumonitis. Diffuse reticular interstitial thickening of the intra- and interlobular septa with patchy ground glass opacities over both lungs shown in high resolution computed tomography of the chest.
9
Figure 1 Authors: Lin and Tarng
10
Figure 2 Authors: Lin and Tarng
by atypical virus infection was suspected. BAL for bacteriology including Gram stains for bacteria, acid-fast stain for Mycobacterium tuberculosis, Toluidine blue O stain for Pneumocystis carinii and india ink for Cryptococcus neoformis all revealed negative findings. There were no bacteria or fungus growth in BAL fluid culture. However, a CMV virus isolation culture of BAL fluid showed a positive result and quantitative PCR for CMV DNA in the peripheral blood showed 325 copies/
µl (normal reference value <10 copies/µL). In addition, serology enzyme-linked immunosorbent assay of the anti-CMV examination showed positive IgG and borderline IgM. Although BAL cytology did not show a cytoplasmic inclusion body, CMV pneumonitis was diagnosed based on the results of CMV isolation from BAL culture and positive PCR report.
Intravenous ganciclovir (350 mg twice a day) was administered immediately for several days until fever decreased, followed by oral valganciclovir (900 mg twice a day) as maintenance therapy for four weeks. In addition, cyclosporine was replaced by mycophenolate mofetil with a dose of 1 g per day. Symptoms of dyspnea and shortness of breath improved gradually. Chest plain film also showed regressive change. However, the flow volume curve of pulmonary function test displayed a restrictive pattern with FEV1 of 1.18 liter (46% prediction rate) and carbon monoxide diffusing capacity revealed a severe reduction of gas exchange (6.6 mL/min/mmHg, 25% prediction rate). Meanwhile, his renal function improved to an estimated creat- inine clearance of 65 mL/min. After discharge, the patient still depended on oxygen therapy at home.
Mycophenolate mofetil (1 g/day) and low dose methylprednisolone (10 mg/day) were continu- ously administered for nearly one year. Till now, there is no recurrence of CMV pneumonitis and his membranous glomerulonephropathy remains in the state of complete remission.
Discussion
Cytomegalovirus is a prevalent viral pathogen, and it remains in a latent status among immuno- competent hosts with 40% to 100% seroprevalence of anti-CMV antibody in the adult population
1. In addition, CMV infection is the most dominant cause of interstitial pneumonitis in immunocompromized renal transplant recipients
2. The definite diagnosis of CMV pneumonitis requires a biopsy for the histo- logical identification of the cytomegalic inclusion body. However, transbronchial biopsies are rarely performed because of uncontrolled bleeding in patients with thrombocytopenia. Serology of the anti-CMV antibody is not a specific marker of CMV infection in immunosuppressed patients, and chest CT scan findings of CMV pneumonitis is neither specific. CMV virus isolation culture has a low positive predictive rate in immunosuppressed AIDS patients and virus copy load does not seem to be related to the degree of lung damage
3. Recently, CMV DNA viremia by real-time PCR is widely used in clinical practice. A reactivation of CMV occurs frequently in ill immunocompetent patients and is correlated with hospitalization rate
4.
Cytomegalovirus infection is more common in patients of glomerulonephritis with nephrotic- range proteinuria than in the normal population
5. Imbalance system of immunity in the infected patients manifested by a rise in number of T-helper cells and activities of complement may play a role in the mechanism of membranous glomeru- lonephropathy. Patients with pre-diabetes or post- transplant diabetes mellitus have an increased risk for CMV infection compared to non-diabetic patients with renal transplant
6. Therefore, diabetes and chronic GN are important predisposing factors of CMV infection. This is the reason for a severe CMV infection occurred in our patient.
Currently, one of the substitute therapy in
patients with steroid-resistant membranous glomer-
ulonephropathy and nephrotic-range proteinuria is cyclosporine
7. In a meta-analysis study, the remission rate observed after the use of cyclo- sporine was 70.5%, being complete in 52.9% of patients
8. However, about 40% of the patients with membranous glomerulonephropathy relaped after discontinuation of cyclosporine. Maintanence cyclosporine therapy is one of the major risk factors to CMV disease
9. Mycophenolate mofetil (MMF) is an alternative immunosuppressive agent due to well tolerated adverse effects and similar efficacy as cyclosporine for patients with nephrotic syndrome
10. In this case, urine protein and serum creatinine levels were decreased successfully after a three- month period of MMF treatment.
In the present case, we draw attentions to the CMV infection in patients with diabetes mellitus and those treated with cyclosporine for the steroid-resistant glomerulonephropathy. It is difficult to diagnose CMV pneumonitis immedi- ately and accurately unless transbronchial biopsy is performed. To improve the diagnostic rate of CMV infection, firstly, we should pay more attention to the high-risk patients such as post-organ transplant or HIV status. Diabetes and glomerulonephropathy, as well as receiving long-term immunosuppressive agents all increase the risk for serious CMV infec- tions. Secondly, in immunocompromised patients initially presented with dyspnea and interstitial pneumonitis in chest plain films or HRCT, CMV viremia by PCR should be performed in order to facilitate diagnosis other than four times serocon- version of CMV IgG and positive CMV BAL culture. Finally, early initiation of an empiric therapy with ganciclovir is also important since immunocompromised patients are very vulnerable
and easily prone to the catastrophes of severe CMV infection. Stopping currently-used immunosup- pressive therapy is not mandatory, but shifting to other alternatives is a treatment of choice. In facing the wide usage of potent immunosuppressive agents in patients of glomerulonephropathy and diabetes, we should keep alert in the clinical aspects of CMV pneumonitis.
References
1. Rafailidis PI, Mourtzoukou EG, Varbobitis IC, et al. Severe cytomegalovirus infection in apparently immunocompetent patients: a systematic review. Virol J 2008 27; 5:47.
2. Heurlin N, Brattstrom C, Tyden G, et al. Cytomegalovirus the predominant cause of pneumonia in renal transplant patients. A two-year study of pneumonia in renal transplant recipients with evaluation of fiberoptic bronchoscopy. Scand J Infect Dis 1989; 21: 245-53.
3. Uberti-Foppa C, Lillo F, Terreni MR, et al. Cytomegalovirus pneumonia in AIDS patients: value of cytomegalovirus culture from BAL fluid and correlation with lung disease.
Chest 1998; 113: 919-23.
4. Limaye AP, Kirby KA, Rubenfeld GD, et al. Cytomegalo- virus reactivation in critically ill immunocompetent patients.
JAMA 2008; 300: 413-22.
5. Semidotskaia ZhD, Artemova SN. Cytomegalovirus infection and glomerulonephritis. Lik Sprava 1999; 4:77-83.
6. Hjelmesæth J, Hartmann A, Leivestad T, et al. The impact of early-diagnosed new-onset post-transplantation diabetes mellitus on survival and major cardiac events. Kidney Int 2006; 69: 588-95.
7. Cattran DC, Appel GB, Hebert LA, et al. North America Nephrotic Syndrome Study Group. Cyclosporine in patients with steroid-resistant membranous nephropathy: A randomized trial. Kidney Int 2001; 59: 1484-90.
8. CBCFP Frassinetti, DSG Bezerra Jr, BFA De Sousa, et al.
Treatment of steroid-resistant nephrotic syndrome with cyclosporine: Study of 17 cases and a literature review. J Nephrol 2005; 18: 711-20.
9. Kanter J, Pallardó L, Gavela E, et al. Cytomegalovirus infection in renal transplant recipients: risk factors and outcome. Transplant Proc 2009; 41: 2156-8.
10. Choi MJ, Eustace JA, Gimenez LF, et al. Mycophenolate mofetil treatment for primary glomerular disease. Kidney Int 2002; 61: 1098-114.
短期使用免疫抑制劑在慢性腎絲球腎炎病患身上 產生之嚴重巨細胞肺病
林彥仲
1唐德成
2,31
蘇澳榮民醫院 腎臟內科
2
台北榮民總醫院 內科部腎臟科
3