Efficacy of home based virtual cycling training on bone mineral density in ambulatory children with cerebral palsy
Chia-Ling Chen,1,2 MD, PhD; Chung-Yao Chen,3,4 MD; Mei-Yuan Liaw,5 MD; Chia-Ying Chung,1,4 MD; Chao-Jan Wang,6 MD; Wei-Hsien Hong,7,* PhD
1Physical Medicine and Rehabilitation, Chang Gung Memorial hospital, 5 Fu-Hsing St. Kwei-Shan, Tao-Yuan 333, Taiwan
2Graduate Institute of Early Intervention, Chang Gung University, 259 Wen-Hwa 1st Rd, Kwei-Shan, Tao-Yuan 333, Taiwan
3Department of Physical Medicine and Rehabilitation, Chang Gung Memorial Hospital, Keelung, 222 Maijin Rd, Keelung 204, Taiwan
4School of Medicine, College of Medicine, Chang Gung University, 259 Wen-Hwa 1st Rd, Kwei-Shan, Tao-Yuan 333, Taiwan
5Department of Physical Medicine and Rehabilitation, Chang Gung Memorial Hospital, Kaohsiung, 123, Ta-Bei Rd., Niao-sung, Kaohsiung, Taiwan
6Department of Radiology, Chang Gung Memorial Hospital, Taoyuan, 5 Fu-Hsing St. Kwei-Shan, Tao-Yuan 333, Taiwan
7Department of Sports Medicine, China Medical University, 91 Hsueh-Shih Road, Taichung 40402, Taiwan
*Address correspondence to: Wei-Hsien Hong, PhD;
Department of Sports Medicine, China Medical University, 91 Hsueh-Shih Road, Taichung 40402, Taiwan
Tel.: +886-4-22053366 ext 7603; Fax: +886-4-22061724
Running title: Training and aBMD in CP Word count of the text: 4138
The number of figures and tables in the article: one figure and 2 tables
FINANCIAL DISCLOSURE/CONFLICT OF INTEREST
All funding sources supporting the work and all institutional or corporate affiliations of mine are acknowledged in an acknowledgement section.
I assert that there are no conflicts of interest (both personal and institutional) regarding specific financial interests that are relevant to the work conducted or reported in this manuscript. There are no potential conflicts of interest related to individual authors' commitments, no potential conflicts of interest related to project support, and no potential conflicts of interest related to commitments of editors, journal staff, or reviewers.
Mini Abstract
The 12-week home based virtual cycling training (hVCT) improved lower limb muscle strength and aBMD than the control program in children with CP. A muscle-strengthening program, rather than general physical activity, is more specific in enhancing aBMD for these children. A novel hVCT is an effective and efficient strategy that enhances lower limb bone density in these children.
Abstract
Purpose: This is the first study to assess the efficacy of a novel home based virtual cycling training (hVCT) program on bone density for children with spastic CP using a well-designed randomized controlled trial.
Methods: Twenty-seven ambulatory children with spastic CP, aged 6–12, were randomly assigned to the hVCT group (n=13) or control group (n=14). Outcome measures—motor function (Gross Motor Function Measure-66 (GMFM-66)), muscle strength (curl up scores and isokinetic torque of knee extensor and flexor muscle) and areal bone mineral density (aBMD) of the lumbar and distal femur—were administered before and immediately after the 12-week intervention.
Results: Analysis of covariance (ANCOVA) results show that the hVCT group had greater distal femur aBMD and isokinetic torques of knee extensor and flexor muscles than the control group at post treatment (p<0.05). However, curl up scores, GMFM-66, and lumbar aBMD at post treatment did not differ between the two groups.
Conclusions: Analytical findings suggest that the muscle-strengthening program is more specific in enhancing bone density for children with CP than general physical activity. Thus, the proposed 12-week hVCT protocol is an effective and efficient strategy for improving lower limb aBMD in these children.
Introduction
Cerebral palsy (CP) describes a group of movement and posture disorders that limit physical activity . The motor-related limitations of spastic CP range from ambulatory to non-ambulatory abilities. Many children with CP are at increased risk of low bone density. Bone densities vary in different skeletal regions in children with CP, as do motor limitations . Some children with moderate or severe CP have low or suboptimal areal bone mineral density (aBMD) and broadband ultrasound attenuation . Even ambulatory children with CP had lower aBMD in some skeletal regions than healthy children . The aBMD of distal femur was lower in ambulatory children with CP than in normal children, while the aBMD of lumbar regions did not differ between two groups . Consequently, the fractures in children with CP generally involve the limbs, especially the femur, and virtually never arise in the spine . Thus, fracture risk is increased in CP children with low bone density .
Multiple complex variables contribute to bone density variations in different skeleton areas in these children . Growth variables are mainly related to femoral and lumbar bone densities, while muscular endurance is mainly related to femoral bone densities . Increasing evidence indicates that bone density is strongly related to muscle function in healthy children and children with CP . The poor bone status or physiologic osteopenia in children with CP is primarily due to a lack of normal musculature loading . The bone density of children with CP is adversely affected by abnormal modeling and remodeling due to decreased muscle strength during mechanical loading. A strong relationship exists between bone strength and muscle force or size , such as isokinetic knee strength in healthy children and ambulatory children with CP . Hence, poor musculature development of children with CP causes abnormal bone development . However, to date, no study has investigated the effects of muscle-strengthening programs on bone density in children with CP.
It is important issue that designs an effective and efficient program to enhance the bone density for children with CP. The home based virtual cycling training (hVCT) integrates the
pedal cycling movement through the virtual reality (VR) exercises at home environment. Home based programs can also provide exercise in a natural environment, thereby increasing participant and caregiver compliance. A previous study showed that a 10-week bicycle ergometer training program, i.e., repetitive cycling, positively affected physical fitness and neuromuscular adaptation in muscles by improving maximal oxygen uptake and muscle efficiency . Furthermore, VR fitness can be fun and motivational, further encouraging users to workout . Therefore, the hVCT program designed for muscle strengthening in this work is home based, requires repetitive and progressive-resistance movement, and is VR based.
This is the first study to investigate the effects of a novel hVCT protocol, home based and VR based muscle-strengthening program, on bone density for children with spastic CP using a randomized controlled trial (RCT). Outcome measures were muscle strength, motor function, and bone density. We hypothesize that children with spastic CP who complete the 12-week hVCT program will have better muscle strength, motor function, and bone density than the control group. Furthermore, cycling and progressive-resistance lower limb muscle strengthening can increase knee muscle strength and femur aBMD, but not trunk muscle strength or lumbar aBMD. Findings obtained by this work may have clinical implications for children with CP at risk of low bone density.
Material and Methods Participants
Children with spastic CP from the Physical Medicine and Rehabilitation Department of a tertiary hospital were recruited for this study. Inclusion criteria were diagnosed CP with Gross Motor Function Classification System (GMFCS) levels I–II , age of 6–12, in pre-pubertal stage, ability to walk independently, ability to undergo a motor function and isokinetic muscle test, and ability to comprehend commands and cooperate during an examination. Exclusion criteria were as follows: 1) children with recognized chromosomal abnormalities; 2) children with a progressive neurological disorder or severe concurrent illness or disease that is not typically associated with CP; 3) children with active medical conditions such as pneumonia; 4) children who had undergone any major surgery or nerve block in the preceding 3 months; 5) children with hormonal disturbance; and, 6) children with poor tolerance for performing the isokinetic test or a poor ability to cooperate during assessment. The Institutional Review Board for Human Studies at Chang Gung Memorial Hospital approved this protocol, and caregivers of all participants or participants provided informed consent.
Figure 1 shows a flow diagram of the randomization procedure. Among the 65 children who underwent an eligibility assessment, 30 were deemed eligible for the randomization procedure. Participants were randomly assigned to the hVCT group or control group. One child in the control group and one child in the hVCT group dropped out due to a lack of available time to complete this study. One child in the control group with incomplete data during follow up was excluded from final analysis. In total, data for 27 children with spastic CP, hVCT group (n=13) and control group (n=14), were analyzed.
Design and Procedures
All participants underwent a series of tests to assess muscle strength, gross motor function, and bone density. Tests were administered before and immediately after the 12-week intervention. A physical therapist, who was not blinded to group allocation, was trained
to use an isokinetic dynamometer and the Gross Motor Function Measure (GMFM) as a precondition of study participation. Motor severities, GMFCS scores, were graded by the same physiatrist. Participant characteristics, including demographic, growth, and clinical data were recorded.
Intervention
The hVCT group cycled for 40 min per day, 3 times a week, for 12 weeks. The hVCT program consisted of a 5 min warm up exercise, loaded sit-to-stand exercises for 20 times, progressive-resistance cycling for 20 min, and a cool down exercise for 5 min. The Eloton SimCycle Virtual Cycling System (Eloton, Inc., NV, USA), a lightweight and portable stationary cycling system, was used for cycling and progressively increasing resistance movements for the lower limbs based on the participant’s ability. This system provides an exercise experience that is both motivational and convenient, allowing participants to cycle at home. The system provides a cycling machine with a video workout library to guide users through virtual exercises. The Eloton Theater CD-ROMs link participants to virtual worlds through a personal computer (PC). Participants can enter the world of virtual fitness via one of the interactive workouts on the CD-ROMs. SimCycle detects pedal movement and adjusts the simulation on the PC monitor. The cycling resistance is primarily from an adjustable nylon tension belt, which can be adjusted from a knob above. The warm up and cool down exercises involved stretching and relaxing the, head, neck, and the upper and lower body, such as hip adductors/hip abductors, knee flexors/knee extensors, and ankle dorsiflexors/ ankle plantar flexors for lower limb, and shoulder flexors/ extensors, shoulder adductors / abductors, elbow flexors/ extensors, wrist flexors/ extensors, and finger flexors/ extensors. One sit-to-stand exercises consisted of one stand up and one sit down. The children performed the loaded sit-to-stand exercises for 10 repetitions for 2 sets with 2-miniute rest between 2 sets . The load was adjusted by adding weight bags to a backpack worn by the participant, and the range of bags were from 0.5 kg–3kg. After 3 min rest, participants performed
progressive-resistance cycling for 20 min. The entire cycling workout included 2 minutes of warm up at a comfortable speed, 16 minutes of cycling at a fast speed, and followed by a 2 minute cool down at a comfortable speed. At the first time, the therapist determined the loads for sit-to-stand training and adjusted the optimal resistance for cycling training. The training load for the loaded sit-to-stand exercises was established according to the individual 1 repetition maximum (1 RM) test. Children were trained with the loads determined by a 75% of 1 RM . The initial cycling resistance was determined by the resistance that allowed children need an effort to cycle for 20 minutes. The cycling resistance was adjusted depending on the
participant’s ability and was progressively increased if the participants found their feet were flying off the pedals.
Participants in control groups were encouraged to perform usual and general physical activity at home under parental supervision. The usual and general physical activity in control group involved walking, running, jogging, or sports or recreational exercises at school or at home for 30–40 min/day, 3 days/week for 12 weeks. To increase the optimal adherence in the protocol for participants, the participants and caregivers were interviewed about the
implementing the programs by research assistant via telephone every 1-2 week. Furthermore, the participants and caregivers were followed up at the rehabilitation clinic every month. The research assistant recorded the compliance of home based programs of the participants. All children had good compliance for performing home based programs except one child of the hVCT group and one child of the control group. They have no available time to continue this study due to heavy school work. No adverse effects or harmful events related to either intervention occurred during the study period.
Assessment
Demographic and growth data
Demographic and growth data were age, gender, body height, body weight, and body mass index (BMI). Weight and height were measured by the same seated weight scale (Model
ACSMIN) and stadiometer, respectively, at Rehabilitation Science and Engineering Service Laboratory. Height was the maximum distance from the feet to the highest point on the head while standing; the subject’s heels, knees, buttocks, and the back were placed in contact with a wall with the help of assistants. The BMI was calculated by dividing weight by height squared.
Clinical data
Clinical data covered motor severity and anticonvulsant usage. The severity of motor limitation associated with CP was classified using the GMFCS . The GMFCS grades self-initiated movement of patients with CP, particularly their functional abilities (e.g., sitting, crawling, standing, and walking), and need for assistive devices (e.g., walkers, crutches, and canes) and wheeled mobility. The GMFCS utilizes a five-point scale, ranging from I for “independent” to V for “dependent.” Anticonvulsant usage was categorized as using or not using anticonvulsant drugs. Only one child in the hVCT group and one child in the control group took anticonvulsants.
Outcome Measures
Gross motor function
The GMFM in clinical practice and international rehabilitation research is the gold standard for evaluating quantitative changes in gross motor function . The GMFM-66, which consists of a subset of 66 items, is a one-dimensional hierarchical scale . The GMFM-66 score was obtained from the GMFM-88 total score using Gross Motor Ability Estimator software . Muscle strength
Trunk muscle strength was assessed using curl ups. The curl up test measures the ability of abdominal muscles to generate tension repeatedly. These muscles are utilized for postural control. The dependent variable was maximum number of curl ups performed correctly in 1 min. The knee extension and flexion torque of the more-affected lower limb that was
(Cybex NORM®, Humac, CA, USA). Participants were positioned on the Cybex testing chair with a trunk-to-thigh angle of approximately 95°. The dynamometer input shaft was aligned with the knee and the dynamometer lever arm was strapped just above the malleoli of the tested leg. Straps were used to stabilize each participant’s involved thigh, pelvis, and trunk. Each participant performed warm-up contractions and practiced concentric knee extension and flexion twice before the test. After resting for 10 seconds, a participant performed five consecutive cycles of concentric knee extension and flexion. Knee extension-flexion comprised a maximal voluntary knee extension, followed immediately by a maximal voluntary knee flexion. Testing velocity was set to 90°/s, and range of motion was 70°, starting with the knee flexed at 80° and ending in an extension at -10°. Measured variables were isokinetic peak torque of the knee extensor and knee flexor. High intraclass correlation coefficient (ICC) values (range, 0.93–0.98) existed for peak torque of absolute isokinetic muscle strength of the knee extensor and flexor at different angular velocities using Cybex . Bone density
The aBMD (g/cm2) was measured at the lumbar spine (L1 to L4) and the distal femur of the more-affected limb using dual X-ray absorptiometry (DXA) (Hologic Delphi QDR, Bedford, MA, USA). The lumbar spine was scanned using standard scanning procedures. The procedure for assessing aBMD of the distal femur projected in the lateral plane has been described previously . Lateral distal femur aBMD was measured by DXA using fan-beam forearm scan mode. Patients were positioned on the ipsilateral side of the leg to be scanned. The aBMD was analyzed from the metadiaphysis of the distal femur, including the trabecular and cortical bones. The physis and zone adjacent to provisional zone calcification were not analyzed because of potential variability with age. This approach was developed specifically to handle significant hip and knee contractures that are commonly limited by CP, and impede measurements at the standard proximal femur site. Ten children received the DXA
3.8%, derived from opposite side. Statistical Analyses
Descriptive and univariate analyses were conducted using the Statistical Package for the Social Sciences (SPSS) version 12.0 (SPSS, Inc., Chicago, IL, USA). To determine
comparability at baseline of demographic and clinical characteristics, the independent two-sample t-test was applied to continuous variables and the chi-square test was applied to categorical variables. To investigate whether the hVCT group improved more than the control group at post treatment, analysis of covariance (ANCOVA) was applied to each outcome variable. Pre treatment performance was the covariate; group was the independent variable; and post treatment performances were separate dependent variables. Significance was set at 0.05 (one-tailed). Effect size, η2, was calculated for each outcome variable to index the magnitude of group differences. A large effect is represented by an η2 of at least 0.138, a moderate effect by an η2 of 0.059 , and a small effect by an η2 of 0.01 .
Results
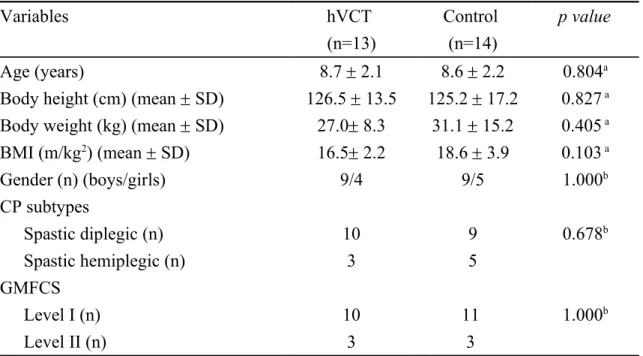
Demographic data did not differ significantly between both groups (Table 1). Before the intervention, the two groups did not significantly differ in any outcome measure, including motor function, muscle strength, and aBMD (Table 2).
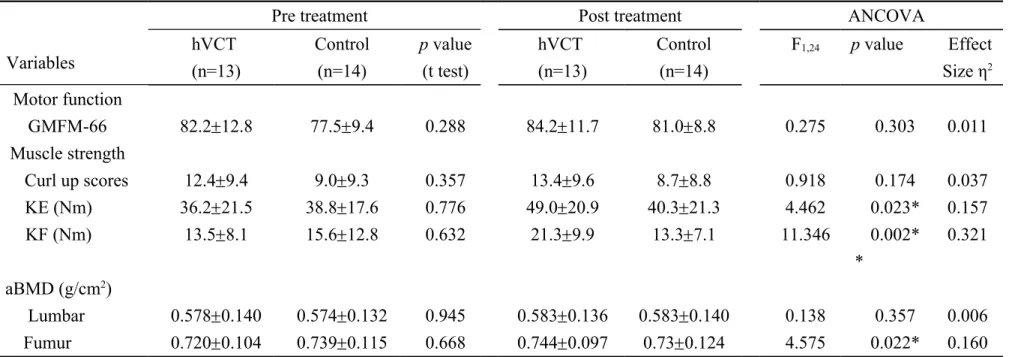
Both groups had improvement in the GMFM-66 scores at post treatment. The ANCOVA results show that no significant differences existed in GMFM-66 scores between both groups after intervention. The hVCT group had improvement in the curl up score and knee muscle strength at post treatment. The control group had improvement in the knee extensor strength, but not knee flexor strength and curl up score, at post treatment. The ANCOVA results show significant and large effect on knee muscle strength, but no significant difference existed in curl up scores at post treatment (Table 2). The hVCT group had higher peak torque of the knee extensor (F1,24=4.462, p=0.023, η2=0.157) and flexor (F1,24=11.346, p=0.002, η2=0.321) than the control group after intervention.
The femur aBMD in the hVCT group was increased at post treatment, however, that was decreased in the control group at post treatment. The ANCOVA results show a significant and large effect on distal femur aBMD (F1,24=4.575, p=0.022, η2=0.160) at post treatment (Table 2); that is, the hVCT group had more improved femur aBMD after intervention than the control group. However, no difference existed between the two groups in lumbar aBMD at post treatment.
Discussion
This is the first work, to the best of our knowledge, to design a novel hVCT protocol to enhance the bone density for children with spastic CP. Analytical results are partially
consistent with our hypothesis. The hVCT protocol in this study is an effective and efficient strategy for improving aBMD. The hVCT group had better muscle strength and bone density at post treatment than the control group. Thus, the 12-week hVCT program improved
isokinetic strength of knee muscles to a greater extent (measured by isokinetic torques of knee muscles) and generated greater gains in bone density of the lower limbs (measured by distal femur aBMD) than the control program at post treatment. These analytical findings suggest that the hVCT program generated better muscle strength and greater lower limb bone density than the general physical activity.
The hVCT induced greater gains in muscle strength and aBMD of the lower limbs, but not motor functions, in children with CP than the general physical activity. In this study, at post treatment, the GMFM-66 scores in the hVCT and control groups were increased by 2 points and 3.5 points, respectively. Wang and Yang recommended the GMFM-66 change scores of 3.7 points for great improvement, 1.6 points for clinically meaningful improvement, and <1.6 points for no clinically meaningful improvement . That is, both interventions
induced clinically meaningful improvement in the gross motor function. Non-significant differences in GMFM-66 scores at post treatment between the two groups likely existed because the hVCT focus is muscle strengthening, not general motor function training. These
analytical results supported that muscle strength, not GMFM-66 scores, was correlated with bone density in children with CP . These findings may suggest the muscle-strengthening program is more specific in enhancing bone density for children with CP than general physical activity.
In this study, hVCT increased femur aBMD, but not lumbar aBMD, in children with spastic CP more than the control program. The likely reason is that knee muscle strength, but not trunk muscle strength, increased after hVCT intervention. The hVCT uses repetitive cycling, further providing low mechanical loading on lower limb bones. Low magnitude mechanical loading is osteogenic in children with disabling conditions . An RCT showed that low-magnitude and high-frequency mechanical stimuli are anabolic for the trabecular bone in children, possibly by providing a surrogate for suppressed muscular activity in the disabled . High-level physical activity, such as jumping, which generates reaction forces eight times one’s body weight, is a simple method of improving bone mass at the hip and spine in healthy children . Although the loads on bones during postural muscle activity are much lower (< 100 microstrains) than those during peak loading (> 2,000 microstrains) . Analytical findings suggest that even relatively low mechanical loading on bone induced by repetitive muscle contractions can also improve lower limb bone density in ambulatory children with spastic CP. Hence, muscle-strengthening program is the choice of treatment to enhance lower limb bone density when high-level physical activity is a safety concern for children with spastic CP.
In this study, the aBMD change was similar to the value of least significant change in the opposite femur (3.8%), although the change in the femur aBMD after 12-week hVCT
intervention was relatively small (0.024 g/cm2, 3.3%). The BMD changes in response to therapy are relatively small, and similar in magnitude to the measurement precision error , although the change equals or exceeds the least significant change can be considered to be genuine biological change . Expressed as smallest detectable difference, it can be considered a
significant change if aBMD change should exceed 0.02 g/cm2 at the total hip and 0.04 g/cm2 at the spine . When monitoring an individual patient, the increases in BMD with therapy are often less than the least significant change . The small gains in BMD are in fact statistically significant when considering group data from clinical trials . Some have even misinterpreted such discussion to mean that some medications do not produce a significant increase in BMD, because the increases in BMD with therapy are often small . These findings may support that even the small gains in femur aBMD after 12-week hVCT intervention are in fact statistically significant.
Furthermore, in this study, distal femur aBMD at post treatment was increased in the hVCT group and decreased in the control group. Analytical results are compatible with those obtained by a previous study . Chad et al. demonstrated that femoral neck-bone mineral content (BMC), volumetric bone mineral density (vBMD), and total proximal femur BMC were increased in an intervention group after an 8-month weight-bearing physical activity intervention in children with CP; however, the femoral neck BMC and vBMD decreased in the control group .
In this work, hVCT induced greater increases in muscle strength of knee muscles, but not in the trunk muscle, in children with CP than the control therapy. The likely reason is the specificity of muscle strengthening by hVCT; that is, the hVCT focus is lower limb muscle strengthening, not trunk muscle strengthening. A previous RCT demonstrated that significant improvements in some measures of strength existed for a stationary cycling group of children with CP . The enhanced motor control strategy after hVCT may result from forced use, repetitive movement, and progressive-resistance movement of more-affected lower limbs. The reciprocal pedal movement can reinforce use of the more-affected limb. Cycling provides massive and repetitive practice and progressive-resistance training of lower limb muscles. Accordingly, the hVCT can overcome learned non-use of the more-affected limb, further enhancing muscle strength of the more-affected limb.
The hVCT protocol designed in this study is an effective and efficient strategy to
improve aBMD. That the relatively short training duration of 12 weeks for the hVCT protocol enhanced femur aBMD is a promising effect, as most studies have shown that the training durations required to increase bone density are longer . For children with CP, harnessing a bone’s sensitivity to mechanical stimuli over the course of a long treatment period (standing on active devices for 10 min/day, 5 days/week for 6 months) may be an effective strategy for fragile bones . After an 8-month physical activity intervention, the femoral neck and proximal femur bone density increased in children with CP . For healthy children, a simple pragmatic program of daily activity for 16 months enhanced distal tibia strength . However, a 9-week intervention (a high-impact exercise and lifestyle intervention) did not significantly increase bone mineral density at the femoral neck or lumbar spine sites compared with controls for children aged 10–11 .
The designed 12-week training protocol can increase lower limb bone density, likely because the hVCT protocol used VR based training in addition to capitalizing on the
advantages of home based programs, repetitive practice, and progressive-resistance training. VR environments allow creativity, and generate task persistence, pleasure, and some degree of control , further enhancing subject motivation to workout. A previous study showed that VR has many benefits, including reorganization/plasticity, increased motor capacity,
heightened visual and perceptual skills, and a high degree of social participation, for children with CP . For example, VR therapy may induce cortical reorganization for functional
improvement based on a functional Magnetic Resonance Imaging (fMRI) study of a child with hemiparetic CP .
The potential scan artifacts that may be precluding accurate aBMD assessment may occurs among children with CP. For example, joint contractures, hip dysplasia, and metallic implants usually prevent reliable measures of aBMD in the proximal femur, and scoliosis and spinal fusion instrumentation prevent DXA measures in the lumbar spine . Technical
difficulties generally occur when attempting to obtain an assessment of aBMD in these children . Overall, the coefficients of variation of aBMD in the distal femur projected in the lateral plane were similar to those for hip and spine . Therefore, the aBMD measures of the distal femur should be considered as an alternative for patients with CP if the whole-body, hip and spine aBMD are difficult to measure. Therefore, this study obtained bone measures of the distal femur projected in the lateral plane.
Findings are limited by study design. This work had a limited participant age range, sample size, and analysis of characteristics of interest. The primary enrollment criterion was ambulatory children with CP; those with limited ambulatory capability were excluded. To eliminate the influence of pubertal stage on the outcome, only pre-pubertal children were recruited in this study. Those with pubertal or post-pubertal stage were excluded.
Furthermore, this study did not assess vitamin D status among the participants, variables that could affect both bone density and functional outcomes. Only 2 participants received
anticonvulsants; thus, we cannot draw any conclusions about the potential effects of these
medications. Hence, study results cannot be generalized to all CP cases. Despite this
limitation, this work elucidated the positive effects of hVCT on bone densities in ambulatory children with spastic CP.
Conclusions
This work demonstrates that the designed 12-week hVCT protocol is an effective and efficient strategy for improve aBMD. The findings suggest that the hVCT group had better muscle strength and greater lower limb bone density than control group after intervention. The muscle-strengthening program is more specific in enhancing bone density for children with CP than general physical activity. Most importantly, experimental data may help clinicians plan preventive strategies in these children, who are at risk for low bone density. Future studies can focus on longitudinal follow up and the underlying brain mechanism of hVCT programs for bone density improvement in children with CP.
Acknowledgements
The authors would like to thank the National Science Council, Taiwan, for financially supporting this research under Contract No. NSC 93-2314-B-182A-201 and 96-2314-B-182A-044-MY2. Ted Knoy is appreciated for his editorial assistance.
References:
1. Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, Dan B, Jacobsson B (2007) A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl 109:8–14.
2. Chen CL, Ke JY, Wang CJ, Wu KP, Wu CY, Wong AM (2011) Factors associated with bone density in different skeletal regions in children with cerebral palsy of various motor severities. Dev Med Child Neurol 53:131–136.
3. Henderson RC (1997) Bone density and other possible predictors of fracture risk in children and adolescents with spastic quadriplegia. Dev Med Child Neurol 39:224–227. 4. Henderson RC, Kairalla J, Abbas A, Stevenson RD (2004) Predicting low bone density in
children and young adults with quadriplegic cerebral palsy. Dev Med Child Neurol 46:416–419.
5. Henderson RC, Kairalla JA, Barrington JW, Abbas A, Stevenson RD (2005) Longitudinal changes in bone density in children and adolescents with moderate to severe cerebral palsy. J Pediatr 146:769–775.
6. Henderson RC, Lark RK, Gurka MJ, Worley G, Fung EB, Conaway M, Stallings VA, Stevenson RD (2002) Bone density and metabolism in children and adolescents with moderate to severe cerebral palsy. Pediatrics 110:e5.
7. Henderson RC, Lin PP, Greene WB (1995) Bone-mineral density in children and adolescents who have spastic cerebral palsy. J Bone Joint Surg Am 77:1671–1681.
8. Jekovec-Vrhovsek M, Kocijancic A, Prezelj J (2005) Quantitative ultrasound of the calcaneus in children and young adults with severe cerebral palsy. Dev Med Child Neurol 47:696–698.
9. Chen CL, Ke JY, Lin KC, Wang CJ, Wu CY, Liu WY (2011) Anthropometric and fitness variables associated with bone mineral density and broadband ultrasound attenuation in ambulatory children with cerebral palsy. J Child Neurol 26:552–559.
10. Chen CL, Lin KC, Wu CY, Ke JY, Wang CJ, Chen CY (2012) Relationships of muscle strength and bone mineral density in ambulatory children with cerebral palsy. Osteoporos Int 23:715–721.
11. Lee JJ, Lyne ED (1990) Pathologic fractures in severely handicapped children and young adults. J Pediatr Orthop 10:497–500.
12. Ward KA, Caulton JM, Adams JE, Mughal MZ (2006) Perspective: cerebral palsy as a model of bone development in the absence of postnatal mechanical factors. J Musculoskelet Neuronal Interact 6:154–159.
13. Schoenau E, Fricke O (2008) Mechanical influences on bone development in children. Eur J Endocrinol 159 Suppl 1:S27–31.
14. Binkley TL, Specker BL (2008) Muscle-bone relationships in the lower leg of healthy pre-pubertal females and males. J Musculoskelet Neuronal Interact 8:239–243.
15. Chan DC, Lee WT, Lo DH, Leung JC, Kwok AW, Leung PC (2008) Relationship between grip strength and bone mineral density in healthy Hong Kong adolescents. Osteoporos Int 19:1485–1495.
16. Schonau E (1998) The development of the skeletal system in children and the influence of muscular strength. Horm Res 49:27–31.
17. Daly RM, Stenevi-Lundgren S, Linden C, Karlsson MK (2008) Muscle determinants of bone mass, geometry and strength in prepubertal girls. Med Sci Sports Exerc 40:1135– 1141.
18. Schoenau E (2005) From mechanostat theory to development of the "Functional Muscle-Bone-Unit". J Musculoskelet Neuronal Interact 5:232–238.
19. Wilmshurst S, Ward K, Adams JE, Langton CM, Mughal MZ (1996) Mobility status and bone density in cerebral palsy. Arch Dis Child 75:164–165.
20. Kaljumae U, Hanninen O, Airaksinen O (1994) Knee extensor fatigability and strength after bicycle ergometer training. Arch Phys Med Rehabil 75:564–567.
21. Snider L, Majnemer A, Darsaklis V (2010) Virtual reality as a therapeutic modality for children with cerebral palsy. Dev Neurorehabil 13:120–128.
22. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B (1997) Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 39:214–223.
23. Scholtes VA, Dallmeijer AJ, Rameckers EA, Verschuren O, Tempelaars E, Hensen M, Becher JG (2008) Lower limb strength training in children with cerebral palsy--a randomized controlled trial protocol for functional strength training based on progressive resistance exercise principles. BMC Pediatr 8:41.
24. Russell DJ, Rosenbaum PL, Avery L, Lane M (2002) Gross Motor Function Measure (GMFM-66 and GMFM-88): User’s Manual. MacKeith Press, London, United Kingdom. 25. Impellizzeri FM, Bizzini M, Rampinini E, Cereda F, Maffiuletti NA (2008) Reliability of
isokinetic strength imbalance ratios measured using the Cybex NORM dynamometer. Clinical physiology and functional imaging 28:113–119.
26. Harcke HT, Taylor A, Bachrach S, Miller F, Henderson RC (1998) Lateral femoral scan: an alternative method for assessing bone mineral density in children with cerebral palsy. Pediatr Radiol 28:241–246.
27. Cohen J (1988) Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates, Hillsdale.
28. Wang HY, Yang YH (2006) Evaluating the responsiveness of 2 versions of the gross motor function measure for children with cerebral palsy. Arch Phys Med Rehabil 87:51– 56.
29. Ward K, Alsop C, Caulton J, Rubin C, Adams J, Mughal Z (2004) Low magnitude mechanical loading is osteogenic in children with disabling conditions. J Bone Miner Res 19:360–369.
in prepubescent children: a randomized controlled trial. J Bone Miner Res 16:148–156. 31. Lenchik L, Kiebzak GM, Blunt BA (2002) What is the role of serial bone mineral density
measurements in patient management? J Clin Densitom 5 Suppl:S29–38.
32. Baim S, Wilson CR, Lewiecki EM, Luckey MM, Downs RW, Jr., Lentle BC (2005) Precision assessment and radiation safety for dual-energy X-ray absorptiometry: position paper of the International Society for Clinical Densitometry. J Clin Densitom 8:371–378. 33. El Maghraoui A, Do Santos Zounon AA, Jroundi I, Nouijai A, Ghazi M, Achemlal L,
Bezza A, Tazi MA, Abouqual R (2005) Reproducibility of bone mineral density measurements using dual X-ray absorptiometry in daily clinical practice. Osteoporos Int 16:1742–1748.
34. Chad KE, Bailey DA, McKay HA, Zello GA, Snyder RE (1999) The effect of a weight-bearing physical activity program on bone mineral content and estimated volumetric density in children with spastic cerebral palsy. J Pediatr 135:115–117.
35. Fowler EG, Knutson LM, Demuth SK, Siebert KL, Simms VD, Sugi MH, Souza RB, Karim R, Azen SP (2010) Pediatric endurance and limb strengthening (PEDALS) for children with cerebral palsy using stationary cycling: a randomized controlled trial. Phys Ther 90:367–381.
36. Macdonald HM, Kontulainen SA, Khan KM, McKay HA (2007) Is a school-based physical activity intervention effective for increasing tibial bone strength in boys and girls? J Bone Miner Res 22:434–446.
37. McWhannell N, Henaghan JL, Foweather L, Doran DA, Batterham AM, Reilly T, Stratton G (2008) The effect of a 9-week physical activity programme on bone and body composition of children aged 10-11 years: an exploratory trial. Int J Sports Med 29:941– 947.
38. Reid D (2004) The influence of virtual reality on playfulness in children with cerebral palsy: a pilot study. Occup Ther Int 11:131–144.
39. You SH, Jang SH, Kim YH, Kwon YH, Barrow I, Hallett M (2005) Cortical reorganization induced by virtual reality therapy in a child with hemiparetic cerebral palsy. Dev Med Child Neurol 47:628–635.
40. Henderson RC, Berglund LM, May R, Zemel BS, Grossberg RI, Johnson J, Plotkin H, Stevenson RD, Szalay E, Wong B, Kecskemethy HH, Harcke HT (2010) The relationship between fractures and DXA measures of BMD in the distal femur of children and adolescents with cerebral palsy or muscular dystrophy. J Bone Miner Res 25:520–526.
Figure Legends:
Table 1 Demographic characteristics and clinical data of both groups Variables hVCT (n=13) Control (n=14) p value Age (years) 8.7 2.1 8.6 2.2 0.804a
Body height (cm) (mean SD) 126.5 13.5 125.2 17.2 0.827 a Body weight (kg) (mean SD) 27.0 8.3 31.1 15.2 0.405 a BMI (m/kg2) (mean SD) 16.5 2.2 18.6 3.9 0.103 a Gender (n) (boys/girls) 9/4 9/5 1.000b CP subtypes Spastic diplegic (n) 10 9 0.678b Spastic hemiplegic (n) 3 5 GMFCS Level I (n) 10 11 1.000b Level II (n) 3 3
at tests; bchi-square tests; hVCT home based virtual cycling training; BMI body mass index; CP cerebral palsy; GMFCS Gross Motor Function Classification System.
Table 2 Descriptive and inferential statistics for analysis of outcome measures of both groups
Variables
Pre treatment Post treatment ANCOVA
hVCT (n=13) Control (n=14) p value (t test) hVCT (n=13) Control (n=14) F1,24 p value Effect Size η2 Motor function GMFM-66 82.212.8 77.59.4 0.288 84.211.7 81.08.8 0.275 0.303 0.011 Muscle strength Curl up scores 12.49.4 9.09.3 0.357 13.49.6 8.78.8 0.918 0.174 0.037 KE (Nm) 36.221.5 38.817.6 0.776 49.020.9 40.321.3 4.462 0.023* 0.157 KF (Nm) 13.58.1 15.612.8 0.632 21.39.9 13.37.1 11.346 0.002* * 0.321 aBMD (g/cm2) Lumbar 0.5780.140 0.5740.132 0.945 0.5830.136 0.5830.140 0.138 0.357 0.006 Fumur 0.7200.104 0.7390.115 0.668 0.7440.097 0.730.124 4.575 0.022* 0.160
*p<0.05; **p<0.01; Values are expressed as meanSD; hVCT home based virtual cycling training; GMFM-66 Gross Motor Function Measure-66; aBMD areal bone mineral density; KE isokinetic torque of knee extensor; KF isokinetic torque of knee flexor.