Indian Journal of Surgery
Lower Limb Pain Caused by Insufficient Muscular Microcirculation
--Manuscript
Draft--Manuscript Number: IJOS-D-12-00166R1
Full Title: Lower Limb Pain Caused by Insufficient Muscular Microcirculation
Article Type: Original Article
Keywords: Lower limb perfusion insufficiency; Microcirculation; Neurogenic claudication; Failed back surgery syndrome
Corresponding Author: Yung-Hsiang Chen, Ph.D. China Medical University
Taichung, TAIWAN, REPUBLIC OF CHINA Corresponding Author Secondary
Information:
Corresponding Author's Institution: China Medical University Corresponding Author's Secondary
Institution:
First Author: Jung-Tung Liu, M.D., D.M.S., Ph.D. First Author Secondary Information:
Order of Authors: Jung-Tung Liu, M.D., D.M.S., Ph.D. Wen-Jui Liao
Cheng-Siu Chang Yung-Hsiang Chen, Ph.D. Order of Authors Secondary Information:
Abstract: Lumbar spinal surgery is a common procedure to treat low back pain. To remark that lower limb perfusion insufficiency may induce the similar syndrome as neuropathic pain, it was surveyed 1,076 cases post spinal surgery within 5 years, in which 51 cases had no obvious improvement 3 months after surgery, 27 cases received second operation because of instability, inadequate decompression and wrong level, and the other 27 cases including 3 cases after twice spinal surgeries were enrolled. Physical examinations were presented with atypical neuropathic pain and muscle wasting at single lower limbs which deteriorated with long distance walking. Computed tomography or magnetic resonance imaging scan were studied including the neural structure and lower limbs angiography. The picture showed degenerative change without definite neural structural compression or vascular occlusion. There is also no significant finding of electrodiagnostic study. Rest radionuclide study of lower limb muscle and myocardium was performed in these 27 cases using Thallium-201. All patients presented 9 - 24% (avg. 14%) muscle perfusion difference compared with two legs. Most of peripheral arterial occlusion disease cases present the symptoms with ischemic pain and vascular claudication. In the study, the patients present not only ischemic limb but also the bizarre symptoms, such as low back pain with or without radiating root pain and sensory disturbance. Physicians should be aware of the possibility of lower limb pain caused by lower perfusion syndrome.
Response to Reviewers: To: Professor Editor Indian Journal of Surgery
E-mail: angie.malanday@springer.com Dear Professor Editor,
Your further editorial consideration will be very much appreciated. Best regards,
Yung-Hsiang Chen, Ph.D.
Graduate Institute of Integrated Medicine China Medical University
Taichung 40402, Taiwan
E-mail: yhchen@mail.cmu.edu.tw Reviewer(s)’ Comments to the Author: Reviewers’ comments:
The Indian Journal of Surgery is not a specialized Spine journal. Please modify your manuscript to include vascular component and exclude majority of spine content. We would appreciate a trim manuscript, with vascular focus.
Response:
Thank you so much for the comments, we fully agree with your opinion. We have tried to revise our manuscript in response to the comments as attachment. Your further consideration will be very much appreciated.
Indian Journal of Surgery
(Ms. No. IJOS-D-12-00166.R1)
Lower Limb Pain Caused by Insufficient Muscular Microcirculation
Jung-Tung Liu,1,2 Wen-Jui Liao,1 Cheng-Siu Chang,1 and Yung-Hsiang Chen3,4
1
Department of Neurosurgery, Department of Nuclear Medicine, Department of Radiology, Chung Shan Medical University Hospital, Taichung, Taiwan; 2School of Medicine, College of Medicine, Chung Shan Medical University, Taichung, Taiwan; 3Graduate Institute of Integrated Medicine, Graduate Institute of Clinical Medical Science, China Medical University, Taichung, Taiwan; 4
Department of Medical Research, Department of Neurosurgery, China Medical University Hospital, Taichung, Taiwan
Address correspondence to: Yung-Hsiang Chen, Ph.D., Graduate Institute of
Integrated Medicine, China Medical University, No. 91, Hsueh-Shih Road, Taichung 40402, Taiwan. Tel: +886-4-22063366 #3512, Fax: +886-4-22037690, E-mail: yhchen@mail.cmu.edu.tw.
Running Title: Lower Limb Perfusion Insufficiency and FBSS *Title Page
Indian Journal of Surgery
(Ms. No. IJOS-D-12-00166.R1)
Lower Limb Pain Caused by Insufficient Muscular Microcirculation
Abstract
Lumbar spinal surgery is a common procedure to treat low back pain. To remark
that lower limb perfusion insufficiency may induce the similar syndrome as
neuropathic pain, it was surveyed 1,076 cases post spinal surgery within 5 years, in
which 51 cases had no obvious improvement 3 months after surgery, 27 cases
received second operation because of instability, inadequate decompression and
wrong level, and the other 27 cases including 3 cases after twice spinal surgeries were
enrolled. Physical examinations were presented with atypical neuropathic pain and
muscle wasting at single lower limbs which deteriorated with long distance walking.
Computed tomography or magnetic resonance imaging scan were studied including
the neural structure and lower limbs angiography. The picture showed degenerative
change without definite neural structural compression or vascular occlusion. There is
also no significant finding of electrodiagnostic study. Rest radionuclide study of lower
limb muscle and myocardium was performed in these 27 cases using Thallium-201.
All patients presented 9 – 24% (avg. 14%) muscle perfusion difference compared
Blinded Manuscript
Click here to view linked References
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
with two legs. Most of peripheral arterial occlusion disease cases present the
symptoms with ischemic pain and vascular claudication. In the study, the patients
present not only ischemic limb but also the bizarre symptoms, such as low back pain
with or without radiating root pain and sensory disturbance. Physicians should be
aware of the possibility of lower limb pain caused by lower perfusion syndrome.
Keywords: Lower limb perfusion insufficiency; Microcirculation; Neurogenic
claudication; Failed back surgery syndrome
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
Introduction
Lower limb perfusion insufficiency, the most common form of peripheral arterial
occlusion disease (PAOD) [1], due to atherosclerosis is a clinical problem that has no
effective medical therapy [2]. When significant atherosclerotic peripheral arterial
disease and neurogenic claudication occur together in the lower limb, neuropathy may
mask the typical symptoms and signs of lower limb ischemia, thus confounding
diagnosis [3]. The diagnostic information gained from symptom enquiry, including
claudication, as well as clinical findings (e.g. absent pulses and prolonged capillary
refill times) can often be misleading in patients [4].
Failed back surgery syndrome (FBSS) is clinically defined as persistent or
recurrent pain, mainly in the lower back and/or legs, even after previous anatomically
successful spinal surgery [5]. Some of the anatomic pain source is unclear, but lower
limb perfusion insufficiency may induce the similar syndrome as neuropathic pain [6].
Because the success can be measured in a variety of ways, reports of surgical failure
rates vary widely. In many series, the overall success rate exceeds 80%. However,
some degree of back pain can persist for years in up to 70% of patients after
discectomy [7]. The success rates fall to around 30% after a second back surgery, 15%
after the third, and to 5% after the fourth surgery [8]. It is a disabling condition that
affecting approximately 30% of spinal surgery patients and it is difficult to treat these
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
patients with conservative therapy [5, 9]. Patients with FBSS typically suffer many
associated problems, including operations of the lumbosacral area, depression and
sleeping problems, family and economic problems, high-dose opioid dependence, and
low probability that further surgery will result in pain relief [10]. Although FBSS
involves many controversies, it defines a common and difficult clinical situation that
deserves particular attention.
Many physicians have declared that pathophysiologic and anatomic diagnosis is
critical to the success in FBSS [8, 11, 12], however, diagnostic algorithms generally
fall into two integrated approaches including temporal and anatomic. Immediate
failure or continuation of preoperative symptoms is ascribed to wrong diagnosis,
technical error, or poor patient selection primarily because of psychosocial factors
[13]. Temporary relief followed by pain recurrence within a few weeks of surgery
suggests infection. Longer-term failures may be caused by loss of intervertebral
stability or spinal stenosis, either at the previous surgical site or at adjacent levels [8].
Data on the causes of failed back surgery are limited. When applying these principles
of diagnosis to the various reviews of causes of FBSS, it is clear that most of the time
an exact diagnosis is unclear. Many authors have advised against a monolithic, solely
anatomic diagnosis and favor a biopsychosocial assessment that includes anatomy
with considerations of behavioral elements ranging from fear avoidance to secondary
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
gain [14].
There are few papers to remark that lower limb perfusion insufficiency may
induce the similar symptom as neuropathic pain [15]. Patients and primary physicians
now need a more sophisticated understanding of diagnostic possibilities, treatment
options, range of surgical techniques, and expected results. The aim of this study is
addressed on the symptom similarity between lower limb insufficient perfusion and
neurogenic claudication for the prevention of following possible FBSS.
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
Methods
Patients
The study was approved by the Institutional Review Board of Chung Shan
Medical University Hospital. All patients provided were informed the written consent
before participating. 1,076 cases with post spinal surgery within 5 years were
surveyed. 51 cases had no obvious improvement 3 months after surgery; 27 cases
received second operation because of instability, inadequate decompression, or wrong
level; and the other 27 cases including 3 cases after twice spinal surgeries were
enrolled in this study. The mean age and body mass index (BMI) of these patients
were 62.4 10.0 (range 41 – 82) years and 27.9 3.5 (range 23 – 39) kg/m2,
respectively. Males comprised 51.9% of these patients. The demographic data
including mean age, gender, BMI, diabetes, smoking, other related diseases, and
surgical area are shown in Table 1. Physical examination presented with atypical
neuropathic pain and muscle wasting at single lower limbs which deteriorated with
long distance walking. Computational tomography (CT) or magnetic resonance
imaging (MRI) scan was utilized for studying the neural structure and lower limbs
angiography. Radiographic measurements were made by technicians “blind” to
treatment group status, with variability controlled via inter- and intra-observer
comparisons [16]. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
Myocardial and Lower Limb Scintigraphy
Stress Thallium-201 myocardial scintigraphy was performed on all patients.
Briefly, ECG was performed during graded exercise testing on a bicycle ergometer.
The results of exercise ECG were interpreted as negative if there were no ischemic
changes during exercise [17]. Single-photon emission computed tomography (SPECT)
imaging was performed within 5 – 10 min after the injection of Thallium-201, with
the patient in the supine position, using a single-head, wide-angle-lens gamma camera
and a low-energy, high-resolution collimator.
Additionally, patients were instructed to remain in the supine position for lower
limb Thallium-201 scanning in the same run after exercise myocardial SPECT
imaging [18]. Three irregular areas of interest were drawn using a trackball around the
entire buttock, thigh, and calf on one side. Symmetrical areas of interest were
automatically generated. No correction was made for background activity. Total
counts in each of the three levels were then determined by computer, and right-to-left
ratios were calculated at each level. A ratio < 0.9 or > 1.1 at one or several levels
defined an abnormal result of lower limb scintigraphy for the level considered, as
reported previously [17, 19]. The perfusion defects were obvious in some patients, but
counting was always performed.
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
Statistical Analysis
The statistical analyses were performed using SPSS software (SPSS, Chicago,
IL). The data were expressed as n or means SD, and the correlations with the
scintigraphy variable were tested by the Mann-Whitney nonparametric test. P values
were two-sided; a value <0.05 was considered statistically significant.
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
Results
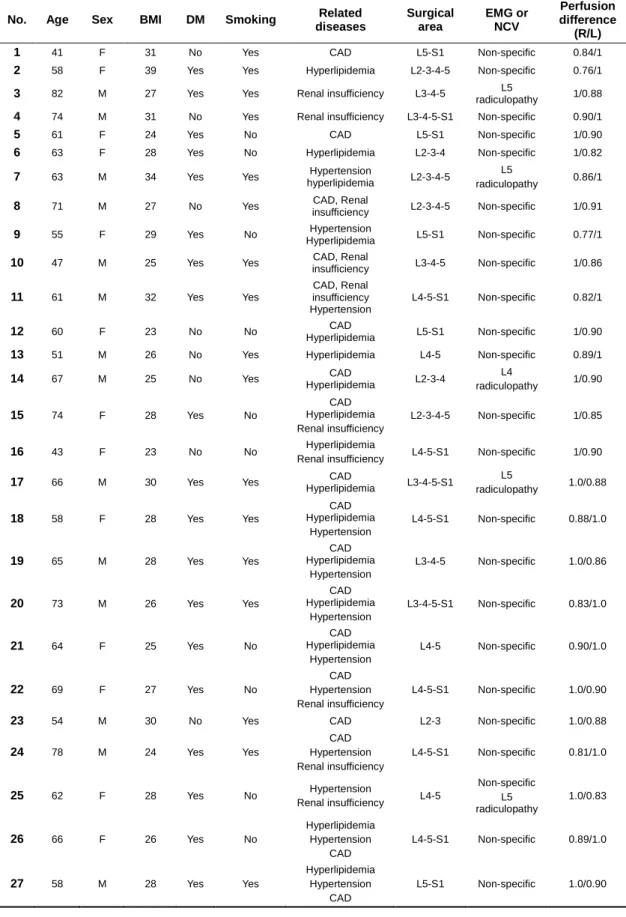
Table 1 presents the demographic data and clinical characteristics for patients
with FBSS. The demographic data includes mean age, gender, BMI, diabetes,
smoking, other related diseases, and surgical area. There is also no significant finding
of electro-diagnostic electromyography (EMG) and nerve conduction velocity (NCV)
study (Table 1). In the quantified rest radionuclide study of lower limb muscle and
myocardium using Thallium-201, it was compared the muscle perfusion difference
between two lower limbs each other. All patients presented 9 – 24% (average 14%)
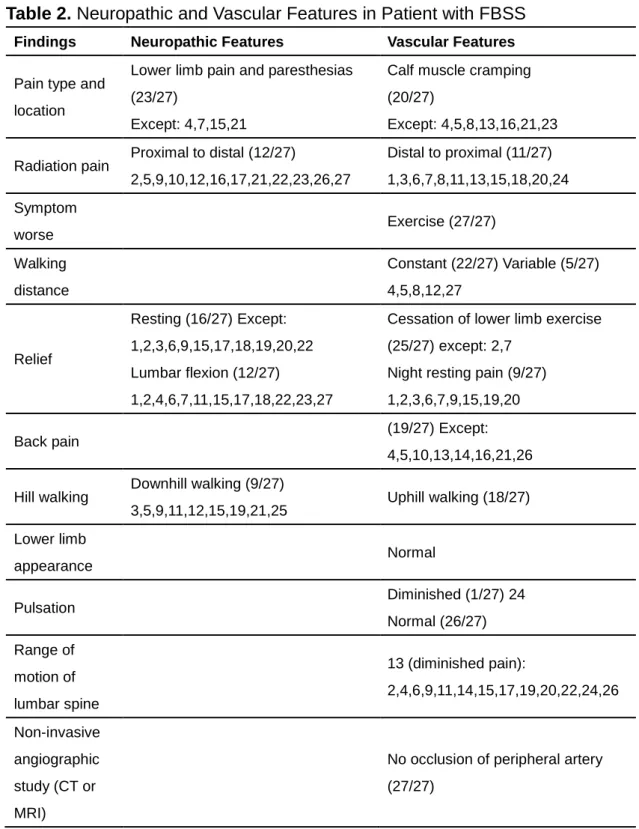
muscle perfusion difference compared with two legs. Table 2 shows the neuropathic
and vascular features that were found from the patients.
Angiograms of the superficial femoral artery from a 61 years-old male (patient
No. 11) with right lower limb pain were shown in Figure 1A. No vascular occlusion
was found in Angiography. However, mean total counts of lower limb Thallium-201
scanning and regional right-to-left ratio were shown. The right-to-left ratio for
perfusion difference of legs was 0.82/1. The test showed a defect of perfusion in the
right calf (arrow) (Figure 1B). The lower limb scintigraphy Thallium-201 scanning
was abnormal in almost 27 patients. Figure 1C shows degenerative change without
definite neural structural compression or vascular occlusion.
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
Discussion
This present study addressed on the symptom similarity between lower limb
insufficient perfusion and neurogenic claudication for the prevention of following
possible FBSS. For the past two decades, researchers and practitioners have used the
phrase FBSS to describe patients with chronic disabling lower back pain with or
without leg pain after one or more spinal surgeries [5]. However, studies with relevant
outcome are rarely diagnosis specific, and high level research studies comparing
surgical and nonsurgical approaches to FBSS studies have not been published to date
[20].
Most of PAOD cases present the symptoms with ischemic pain and vascular
claudication [21]. However, these symptoms, usually, happen in the stage of
significant loss of vascular patency. Sonogram and angiogram are good modalities for
diagnosis of PAOD. The majority of patients with early stage atherosclerotic vascular
change developed similar symptom as well, although blood circulation is normal.
Skeletal muscle perfusion scan provides the information at the level of a
microcirculation (in fact at tissue oxygenation). In the present study, the patients
present not only ischemic limb but also the bizarre symptoms, such as low back pain
with or without radiating root pain and sensory disturbance. These symptoms are hard
to discriminate spinal problem from neuropathy. Many spinal surgeons try to
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
emphasize the discrepancy between two categories; nevertheless, the clear-cut
separation is not so easy [22]. The peak incidence of patients with insufficient lower
limb perfusion is 6th - 7th decay, but they probable have spinal disorder as well.
Through the symptomatic expression and image finding even MRI or CT scan,
surgeons might make incorrect diagnoses and subsequent wrong decisions. The cause
of vascular stenosis even obstructs related systemic disorder such as hyperlipidemia,
obesity, DM, hypertension or renal insufficiency. Neuropathic pain can happen in any
age, it is not closed to systemic disease. Once aged patients suffer from lower limb
disability and no sufficient evidence to support the lesion originated from neural
structure, muscle perfusion assessment should be considered for study.
The FBSS label has been used primarily to connote poor prognosis and to warn
patient and practitioner accordingly in making further treatment choices. In one
review, initial success rates exceeding 50% fell to around 30% after the second
surgery, to 15% after the third, and to 5% after the fourth [23]. From the nonoperative
perspective, rehabilitation may have less success in reducing pain reports in
postsurgical patients compared to their nonoperated peers, even when most physical
capacities improve equally [8]. Although diminished prognosis after an unsuccessful
operation may be conceded, some authors caution against inappropriate
discouragement and even distraction from the critical clinical tasks of diagnosis and
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
treatment [24, 25].
Back surgery is not the final common pathway for everyone with persistent back
pain. It offers specific therapy for specific anatomical derangements associated with
specific complexes of symptoms [26], When surgery ranges beyond carefully defined
situations, disappointed patients are likely to be expected. A generation ago, “back surgery” usually meant removing the offending portion of a herniated disk [10], Time has changed, and both the indications and the surgical techniques have expanded
enormously. Indeed, clinical science has struggled to keep pace with innovation,
creating uncertainties about the efficacy and safety of some new surgical techniques.
Often, internists are asked for advice by these challenging patients but are unfamiliar
with the conditions leading to back surgery, the types of back surgery, and the best
approaches to diagnosis and management [13].
Conclusions
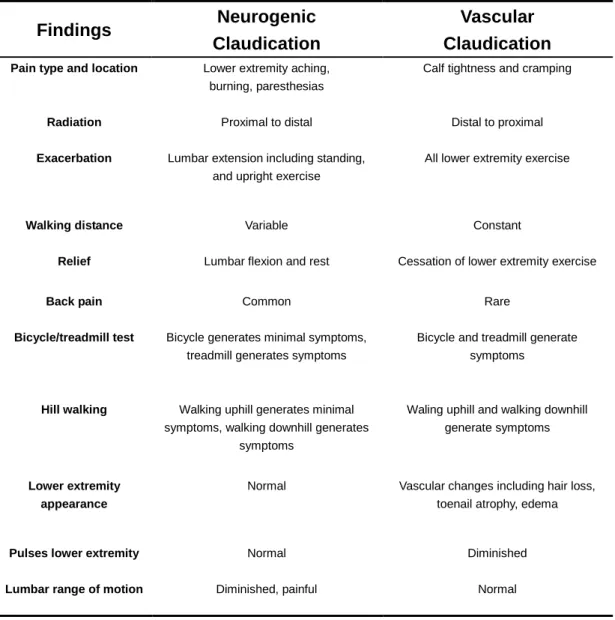
Muscle scan can demarcate the perfusion difference between two lower limbs.
Many Spinal surgeons perform the spinal surgery according to the complaints from
patients and the radiological finding. However, these symptoms are hard to demarcate
from ischemic pain (Table 3). Physicians should be aware of the possibility of lower
limb pain causing by lower perfusion syndrome.
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
Acknowledgements
This study is supported in part by Taiwan Department of Health Clinical Trial
and Research Center of Excellence (DOH101-TD-B-111-004) and National Science
Council (NSC 100-2320-B-039-008-MY2). We thank Miss Jin-Mei Wang and
Chi-Hsiang Wei for the manuscript preparation.
Conflict of interest statement
There are no conflicts of interest.
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
References
1. Mehrabi Bahar M, Saeed Modaghegh MH, Soltani E (2010) Serum Lipid Changes after Short Term SIPC Therapy for Lower Limb Lymphedema. Indian J Surg 72:305-307
2. Powell RJ, Simons M, Mendelsohn FO, Daniel G, Henry TD, Koga M, Morishita R, Annex BH (2008) Results of a double-blind, placebo-controlled study to assess the safety of intramuscular injection of hepatocyte growth factor plasmid to improve limb perfusion in patients with critical limb ischemia. Circulation 118:58-65
3. Simonetti I, Pratesi C (2006) Intermittent claudication or neurogenic claudication? "Why don't you speak to me"? Intern Emerg Med 1:133; discussion 133-134
4. Varcoe RL, Taylor CF, Annett P, Jacobsen EE, McMullin G (2006) The conundrum of claudication. ANZ J Surg 76:916-927
5. North RB, Campbell JN, James CS, Conover-Walker MK, Wang H, Piantadosi S, Rybock JD, Long DM (1991) Failed back surgery syndrome: 5-year follow-up in 102 patients undergoing repeated operation. Neurosurgery 28:685-690; discussion 690-681
6. Rodrigues GS, Khan SA (2011) Pharmacovigilance among surgeons and in surgical wards: overlooked or axiomatic? Indian J Surg 73:4-8
7. Dvorak J, Gauchat MH, Valach L (1988) The outcome of surgery for lumbar disc herniation. I. A 4-17 years' follow-up with emphasis on somatic aspects. Spine (Phila Pa 1976) 13:1418-1422
8. Hazard RG (2006) Failed back surgery syndrome: surgical and nonsurgical approaches. Clin Orthop Relat Res 443:228-232
9. Javid MJ, Hadar EJ (1998) Long-term follow-up review of patients who underwent laminectomy for lumbar stenosis: a prospective study. J Neurosurg 89:1-7
10. Van Buyten JP (2006) Neurostimulation for chronic neuropathic back pain in failed back surgery syndrome. J Pain Symptom Manage 31:S25-29
11. Fritsch EW, Heisel J, Rupp S (1996) The failed back surgery syndrome: reasons, intraoperative findings, and long-term results: a report of 182 operative treatments. Spine (Phila Pa 1976) 21:626-633
12. Swiontkowski MF (1999) Current concepts review. Methods for locating missing patients for the purpose of long-term clinical studies. J Bone Joint Surg Am 81:142
13. Ragab A, Deshazo RD (2008) Management of back pain in patients with
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
previous back surgery. Am J Med 121:272-278
14. Waddell G (1987) 1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine (Phila Pa 1976) 12:632-644
15. Song J, Lee JB, Suh JK (2009) Clinicopathological considerations in patients with lumbosacral extraforaminal stenosis. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia 16:650-654
16. Liu JT, Liao WJ, Tan WC, Lee JK, Liu CH, Chen YH, Lin TB (2010) Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture: a prospective, comparative, and randomized clinical study. Osteoporos Int 21:359-364
17. Cosson E, Paycha F, Tellier P, Sachs RN, Ramadan A, Paries J, Attali JR, Valensi P (2001) Lower-limb vascularization in diabetic patients. Assessment by thallium-201 scanning coupled with exercise myocardial scintigraphy. Diabetes Care 24:870-874
18. White C (2007) Clinical practice. Intermittent claudication. N Engl J Med 356:1241-1250
19. Segall GM, Lennon SE, Stevick CD (1990) Exercise whole-body thallium scintigraphy in the diagnosis and evaluation of occlusive arterial disease in the legs. J Nucl Med 31:1443-1449
20. Onesti ST (2004) Failed back syndrome. Neurologist 10:259-264
21. McDermott MM, Greenland P, Liu K, Guralnik JM, Criqui MH, Dolan NC, Chan C, Celic L, Pearce WH, Schneider JR, et al. (2001) Leg symptoms in peripheral arterial disease: associated clinical characteristics and functional impairment. JAMA 286:1599-1606
22. Taylor RS, Van Buyten JP, Buchser E (2005) Spinal cord stimulation for chronic back and leg pain and failed back surgery syndrome: a systematic review and analysis of prognostic factors. Spine (Phila Pa 1976) 30:152-160 23. Nachemson AL (1993) Evaluation of results in lumbar spine surgery. Acta
Orthop Scand Suppl 251:130-133
24. Verbeek JH (2003) Label is unhelpful. BMJ 327:986-987
25. Talbot L (2003) "Failed back surgery syndrome". BMJ 327:985-986
26. Deyo RA (2007) Back surgery--who needs it? N Engl J Med 356:2239-2243
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
Figure Legends
Figure 1. A 61 year-old male with right lower limb pain. (A) The angiography shows
no vascular occlusion. (B) MRI shows the disc herniation at L4-5 and L5-S1. (C)
Muscle perfusion scan shows lower perfusion of right limb.
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59
Table 1. Demographic Data of Patients with FBSS
No. Age Sex BMI DM Smoking Related diseases Surgical area EMG or NCV Perfusion difference (R/L) 1 41 F 31 No Yes CAD L5-S1 Non-specific 0.84/1
2 58 F 39 Yes Yes Hyperlipidemia L2-3-4-5 Non-specific 0.76/1
3 82 M 27 Yes Yes Renal insufficiency L3-4-5 L5
radiculopathy 1/0.88
4 74 M 31 No Yes Renal insufficiency L3-4-5-S1 Non-specific 0.90/1
5 61 F 24 Yes No CAD L5-S1 Non-specific 1/0.90
6 63 F 28 Yes No Hyperlipidemia L2-3-4 Non-specific 1/0.82
7 63 M 34 Yes Yes Hypertension
hyperlipidemia L2-3-4-5
L5
radiculopathy 0.86/1
8 71 M 27 No Yes CAD, Renal
insufficiency L2-3-4-5 Non-specific 1/0.91
9 55 F 29 Yes No Hypertension
Hyperlipidemia L5-S1 Non-specific 0.77/1
10 47 M 25 Yes Yes CAD, Renal
insufficiency L3-4-5 Non-specific 1/0.86 11 61 M 32 Yes Yes CAD, Renal insufficiency Hypertension L4-5-S1 Non-specific 0.82/1 12 60 F 23 No No CAD Hyperlipidemia L5-S1 Non-specific 1/0.90
13 51 M 26 No Yes Hyperlipidemia L4-5 Non-specific 0.89/1
14 67 M 25 No Yes CAD Hyperlipidemia L2-3-4 L4 radiculopathy 1/0.90 15 74 F 28 Yes No CAD Hyperlipidemia Renal insufficiency L2-3-4-5 Non-specific 1/0.85 16 43 F 23 No No Hyperlipidemia
Renal insufficiency L4-5-S1 Non-specific 1/0.90
17 66 M 30 Yes Yes CAD
Hyperlipidemia L3-4-5-S1 L5 radiculopathy 1.0/0.88 18 58 F 28 Yes Yes CAD Hyperlipidemia Hypertension L4-5-S1 Non-specific 0.88/1.0 19 65 M 28 Yes Yes CAD Hyperlipidemia Hypertension L3-4-5 Non-specific 1.0/0.86 20 73 M 26 Yes Yes CAD Hyperlipidemia Hypertension L3-4-5-S1 Non-specific 0.83/1.0 21 64 F 25 Yes No CAD Hyperlipidemia Hypertension L4-5 Non-specific 0.90/1.0 22 69 F 27 Yes No CAD Hypertension Renal insufficiency L4-5-S1 Non-specific 1.0/0.90
23 54 M 30 No Yes CAD L2-3 Non-specific 1.0/0.88
24 78 M 24 Yes Yes CAD Hypertension Renal insufficiency L4-5-S1 Non-specific 0.81/1.0 25 62 F 28 Yes No Hypertension Renal insufficiency L4-5 Non-specific L5 radiculopathy 1.0/0.83 26 66 F 26 Yes No Hyperlipidemia Hypertension CAD L4-5-S1 Non-specific 0.89/1.0 27 58 M 28 Yes Yes Hyperlipidemia Hypertension CAD L5-S1 Non-specific 1.0/0.90 Table 1
Table 2. Neuropathic and Vascular Features in Patient with FBSS
Findings Neuropathic Features Vascular Features
Pain type and location
Lower limb pain and paresthesias (23/27)
Except: 4,7,15,21
Calf muscle cramping (20/27)
Except: 4,5,8,13,16,21,23
Radiation pain Proximal to distal (12/27)
2,5,9,10,12,16,17,21,22,23,26,27 Distal to proximal (11/27) 1,3,6,7,8,11,13,15,18,20,24 Symptom worse Exercise (27/27) Walking distance Constant (22/27) Variable (5/27) 4,5,8,12,27 Relief Resting (16/27) Except: 1,2,3,6,9,15,17,18,19,20,22 Lumbar flexion (12/27) 1,2,4,6,7,11,15,17,18,22,23,27
Cessation of lower limb exercise (25/27) except: 2,7
Night resting pain (9/27) 1,2,3,6,7,9,15,19,20
Back pain (19/27) Except: 4,5,10,13,14,16,21,26
Hill walking Downhill walking (9/27)
3,5,9,11,12,15,19,21,25 Uphill walking (18/27) Lower limb appearance Normal Pulsation Diminished (1/27) 24 Normal (26/27) Range of motion of lumbar spine 13 (diminished pain): 2,4,6,9,11,14,15,17,19,20,22,24,26 Non-invasive angiographic study (CT or MRI)
No occlusion of peripheral artery (27/27)
Table 3. Clinical Features Differentiating Neurogenic Claudication and Vascular Claudication Findings Neurogenic Claudication Vascular Claudication
Pain type and location Lower extremity aching, burning, paresthesias
Calf tightness and cramping
Radiation Proximal to distal Distal to proximal
Exacerbation Lumbar extension including standing, and upright exercise
All lower extremity exercise
Walking distance Variable Constant
Relief Lumbar flexion and rest Cessation of lower extremity exercise
Back pain Common Rare
Bicycle/treadmill test Bicycle generates minimal symptoms, treadmill generates symptoms
Bicycle and treadmill generate symptoms
Hill walking Walking uphill generates minimal symptoms, walking downhill generates
symptoms
Waling uphill and walking downhill generate symptoms
Lower extremity appearance
Normal Vascular changes including hair loss, toenail atrophy, edema
Pulses lower extremity Normal Diminished
Lumbar range of motion Diminished, painful Normal
Figure 1
http://www.springer.com/journal/12262
﹉ASS● ●珀而●hUf﹉
S…
rg..ns.f﹏
●
一
c。
prr︳
ght
TransferStatement
thecopy府ghttU∥1sa〢ide:s transferedto then6UaH甜
。
nUfSvrgeonsUf︳nd:a
tf.rV.S.g.vemmente,n坤呼Ⅸ∫ tU好時 a燈e波tranSmmb(e,db由Ve好andWhen
theamde治aCceptedfUrpub::cat:on.theauthorwarrants thath:Srllercon㏑buIon
治o茁g㏑祕andthatheJshehasful︳ p-rt.make曲 治gran●.TheauthUrd°rlsfUr
andaccepts respUns弦琳好yf.rreleas:ngtll:smate㎡alUnbeharUfanyanda田 cU-authors.thecUpv∥ ghttFanSfercovers theexclus︳ ve㎡ghti.reprUduceand
dk如butethea大de,:ndt媌ngrep㎡ nts,tranS圮曲onS,phUtUgFaph沁 repFUd㏕●ns,
m油田b爾,deCtFUntfUrJnfUml聆,°n竹ne)。了anV°㏑eFrepFUdu田onsUf由m∥ar
natUre.
AnaUth●rmay“無a由盹 anamlUF_.eatedⅥ田當UnUf打glIera由deUnh怎加eF
Uwnwebs扣eandoΓ :nh淹伯q〢n㎝tutona:Γepo由t。n「Hersriemaya| sodepos比 th:S
晚 由 ㎝ Un馣純 r食㏕ 駢 S●rmders 曲 軸 ㏕ 田 了卵 叫 at扭色nd㎡s request oraSareSult ofa︳ ega︳ obIgaton,provided又 iSnUtmadepub︳:dy
availam日㏕田12硹撫 aner㎡磞 pUbI輛 .HJS1●emaYnUtuse臨
pvb∥ She′SPDFvers︳on,wh:ch︳SpUstedon唧 .SpHngeH:nk.oom,fUrthepurpUSe Ufself-蚴 Ur出眾憑由tFunemUFe,曲 盻au甘×盯 卿 Un)rpUsth曲 veFS;Un prUv︳dedacknUWedgement:Sg︳ven to theo︻g:na︳ sourceofpub田a戒:onanda︳ink
:s︳nseFtedtUthepubliSheda飆 eonSp府解 s㏑從由啗敵e.the︳ ㏑kmustbe
accompankK:bythefUlk四〢ngtext:︳喻 eoHg∥及“pvb︳ka市oniSavalableat
_ .spHngeH:nk.com‘.
了heauthor治 requestedtUuse廿贈 司阿田η 兩ateDUlfUrtheamde.Artides
dSSem磁艴d啪a-.Sp茁 nge〢 ㏑k.comaFeindeXed,abstractedandreferencedby
manyab┤㏑喊 ngandinfUrma臼°nServ:cesjb:b︳︳°gFaph︳cnemUrks,subScH”on agenc齒,︳bra的◤nemrks,andcUnso由 a.
AneFmbm蜘 ●f托 agreemmt由嘻nedbI純 cUrrespUndngamUr:changesUf
authorsh:poΓ ︳nt1.eordeΓ oftheauthoΓs︳:Sted㏑用|notbeaccepted.
Jo..ma:::Ⅱd:anJo▌ma︳ofSu四●呼
了:tle●faFt:c︳.:
∟owerL;了nbPainCausedby︳nsu爾 cientMuscu|arM:crUc:rcu︳a臼on ,
A●tho〢S9:
Jung-了ung∟︳u,Wen-Ju︳ L︳aU,Cheng-SiuChang,andYung-Hs︳angChen Aut●●o′sS㎏ nm.Π
= (由gn:ngonbeha什 Uf” :ntauthUrs)
「eb.23,2。 12