Increased Risk of Stroke Among The Patients with Hip Fracture: A Nationwide Cohort Study
Running title: Hip Fracture and Stroke
Chun-Hao Tsai 1,2 E-mail address: ritsai8615@gmail.com
Cheng-Li Lin 3,4 E-mail address: orangechengli@gmail.com
Horng-Chang Hsu 1,2 E-mail address: D4749@mail.cmuh.org.tw
1 Graduate Institute of Clinical Medicine, China Medical University, Taichung, Taiwan
2 Department of Orthopedics, China Medical University Hospital, Taichung, Taiwan
3 Management Office for Health Data, China Medical University Hospital, Taichung, Taiwan
4 Department of Public health, China Medical University, Taichung, Taiwan
Correspondence to:
E-mail address:
Phone No.: +886-4-22053366 ext. 6505; Fax No.: +886-4-22070429
ABSTRACT
Aims: Hip fractures are associated with increased risk of major morbidity. However, little data are available on the risk of stroke after hip fracture. Therefore, we investigated whether hip fracture increased the risk of stroke in a large nationwide cohort study.
Methods: Using universal insurance claims data, we identified a study cohort of 6013 participants with hip fracture newly diagnosed in 2000–2010 and a non-hip fracture cohort of 23 802 participants. Incidence and risk of stroke were estimated for both cohorts until the end of 2011.
Results: The stroke incidence was 1.69-fold (95% confidence interval [CI] = 1.56–1.83) higher in the hip fracture cohort than in the non-hip fracture cohort with an adjusted hazard ratio (HR) of 1.54 (95% CI = 1.42–1.67) for the hip fracture cohort. The patients with hip fracture carried a higher risk of developing ischemic and hemorrhagic stroke, with adjusted HRs of 1.55 and 1.48 (95% CI = 1.42-1.69 and 1.16-1.89), respectively. With an incidence of 64.6 per 1000 person-years, the adjusted HR of stroke increased to 3.10 (95% CI = 2.47–3.90) for patients with coexistence of diabetes, hypertension, and heart failure, compared with those without diabetes, hypertension, and heart failure. With an incidence of 60.4 per 1000 person-years, the adjusted HR of stroke increased to 2.92 (95% CI = 2.43–3.51) for hip fracture patients with medication of diuretic, and ARB, compared with those without hip fracture, diuretic, and ARB.
Conclusion: Hip fracture is independently associated with a subsequent risk of stroke. Keywords: hip fracture, stroke, cohort study
Introduction
Hip fracture is a devastating event that causes major morbidity and mortality, particularly in elderly populations. 123 Worldwide, the total number of hip fractures is expected to surpass 6
million by a year. 4 Previous studies have shown that the lifetime risk of hip fracture is 17.5% for
women and 6% for men.5 The association between cardiovascular disease and hip fracture has
attracted attention in recent years. 6, 7 Several factors are thought to concurrently affect the vascular system and regulation of bone formation. 8, 9 Bone and vasculature are regulated by
several shared factors, and calcification of the vascular walls resembles the bone formation process in many ways. 9 One recent study reported that hip fracture is associated with an
increased risk of subsequent acute myocardiac infraction. 10 Stroke is a well-known risk factor for
hip fracture. However, there is only one article assess the risk of stroke among patients within one year of hip fracture. Long term medication after hip fracture also plays a role in stroke risk, so we also want to assess the risk in different medication. This study investigated the frequency and risk of stroke after hip fracture using a nationwide population-based cohort study.
Methods Data source
In 1995, Taiwan launched the National Health Insurance (NHI) program that covers approximately 99% of the Taiwanese population. The Bureau of NHI made patient data available electronically through the National Health Insurance Research Database (NHIRD) project. The NHIRD contains comprehensive patient information, including demographic characteristics, diagnoses, medical expenditures, and prescription claims that include the date and duration of prescriptions, type of medications, dosages. Diseases are coded according to the International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM). Previous studies have indicated that the high accuracy and validity of ICD-9-CM diagnoses in the NHIRD.11, 12 In
this study, we used the Longitudinal Health Insurance Database 2000 (LHID 2000) from 1996 to 2011 obtained from the NHIRD. The LHID 2000 contains 1,000,000 beneficiaries randomly sampled from the original NHIRD. The NHRI has reported that there were no statistically
significant differences in age, sex, or healthcare costs between the sample group and all enrollees. The NHIRD consists of personally unidentifiable secondary data released for research purposes. The study was approved by the Institutional Review Board (IRB) of China Medical University and Hospital (CMU-REC-101-012).
Study population
We conducted a retrospective cohort from January 1, 2000, to December 31, 2010. We identified patients aged 20 years and older with a newly diagnosis of hip fracture (ICD-9-CM code 820) as hip fracture cohort. The first hospitalization for hip fracture served as the index date of a medical service for hip fracture. Patients those with a history of stroke prior to the index date, with a diagnosis of pathological fracture (ICD-9-CM 733.1), fractures from transport-related accidents (E800-E848), aged less than 20 years, and with incomplete information on demographics were excluded. Subjects without any records of hip fracture were used as the non-hip fracture cohort and were randomly selected from the NHI beneficiaries in the LHID 2000. For each hip fracture case was frequency matched with 4 controls by gender, age (per 5 years span), and index year. The same exclusion criteria were also applied to non-hip fracture subjects. Baseline variables
We obtained baseline variables, including age, sex, comorbidities of diabetes (ICD-9-CM code 250), hypertension (ICD-9-CM codes 401- 405), hyperlipidemia (ICD-9-CM code 272),
osteoporosis (ICD-9-CM code 733.0), coronary artery disease (CAD; ICD-9-CM codes 410-414), and heart failure (ICD-9-CM code 428), and medications including aspirin, clopidogrel, warfarin, proton pump inhibitors (PPIs), statins, estrogen (only women), prednisolone, bisphosphonates
and antihypertensive agents. Antihypertensive agents included calcium channel blockers (CCBs), angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs), alpha blocker, beta blocker, and diuretics.
Outcome measurement
The endpoint of interest in the study was development of stroke (ICD-9-CM codes 430-438). Stroke was classified into 2 subtypes: ischemic (ICD-9-CM codes 433-438) and hemorrhagic (ICD-9-CM codes 430-432). All subjects were followed from the index date to occurrence of endpoint, withdrawal from the insurance program, or until December 31, 2011, whichever was first.
Statistical analysis
The SAS statistical package (SAS System for Windows, Version 9.1.3, SAS Institute Inc., Cary, NC, USA) was used to perform all statistical analyses. A 2-tailed probability was
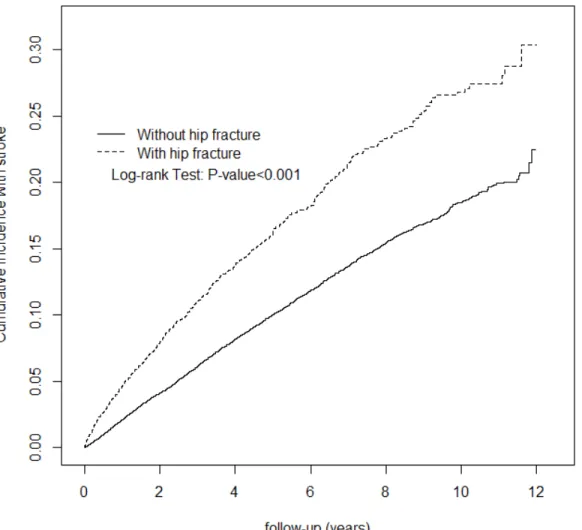
considered statistically significant for p values < 0.05. Distribution of gender, age (20-49, 50-64, 65-79 and 80+), comorbidities, and medications were compared between the hip fracture cohort and the non-hip fracture cohort, and were examined using the Chi-square test for categorical variables and t-test for continuous variables. We then estimated cumulative incidence curves of stoke during the follow-up period using the Kaplan-Meier method, and the differences between the 2 cohorts were examined by using the log-rank test. The sex-, age-, comorbidity-, and follow-up years-specific incidence densities of stroke were estimated for both cohorts. Univariable and multivariable Cox proportional hazards regression models estimate hazard ratios (HRs) and 95% confidence intervals (CIs) for stroke in patients with hip fracture in a relationship to the non-hip fracture cohort. Baseline characteristics variables such as sex, age, comorbidities and medications were included in the multivariate model for adjustment. Because the comorbidities included diabetes, hypertension, and heart failure in the multivariable model were significant. Further data
analysis was performed to evaluate the interaction pattern among diabetes, hypertension, and heart failure on stroke risk. In the multivariable model, antihypertensive agents including
diuretics and ARB attained significance. Further data analysis was also performed to evaluate the interaction among hip fracture, diuretics and ARB.
Results
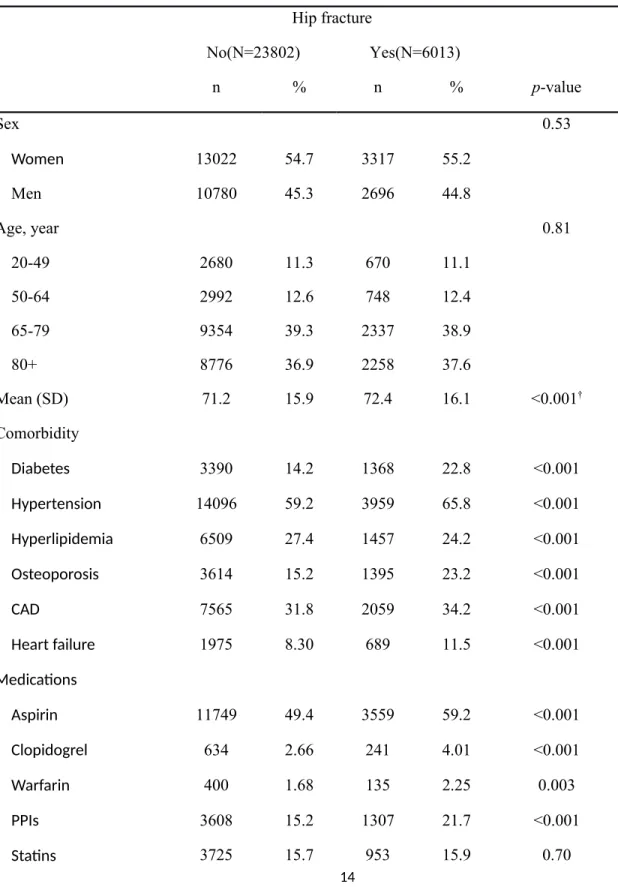
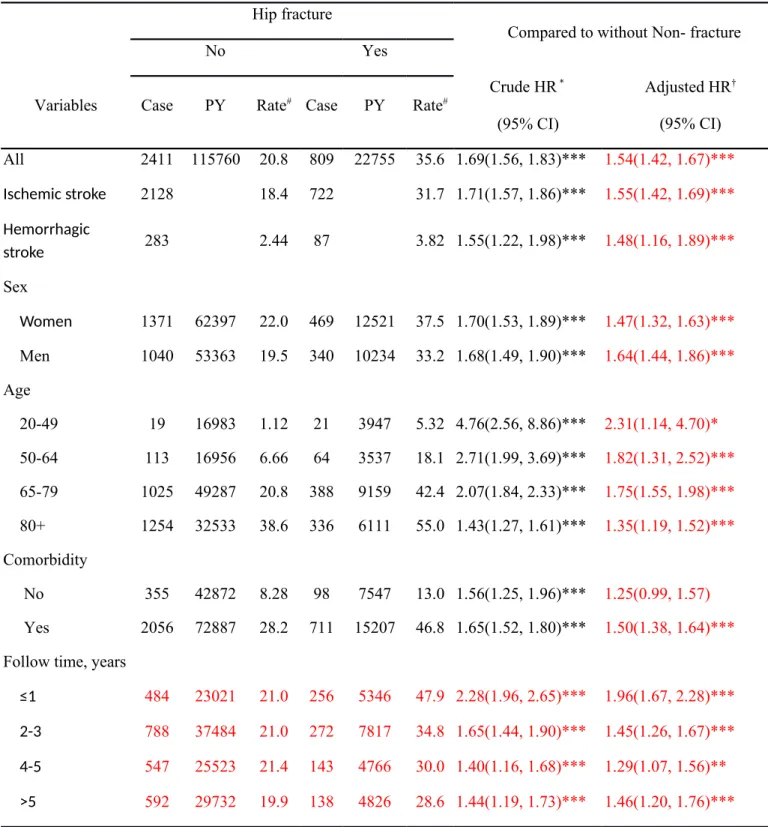
The study includes a cohort of 6013 patients with hip fracture and a non-hip fracture cohort of 23802 patients (Table 1). Of the hip fracture subjects, 55.2% were women and most were more than 65 years of age (76.5%). Mean age for the hip fracture cohort and non-hip fracture cohort were 72.4 (SD=16.1) and 71.2 (SD=15.9) years, respectively. Patients with hip fracture were more likely to have diabetes, hypertension, osteoporosis, CAD, and heart failure (p<0.001). All of medications were more prevalent in the hip fracture cohort at the baseline (p-value <0.001), compared to non-hip fracture cohort. During the mean follow-up of 3.78 years for the hip fracture cohort and 4.86 years for the non- hip fracture cohort, the overall incidence of stroke (per 1000 person-years) was 35.6 and 20.8, respectively (Table 2). Figure 1 shows the cumulative stroke incidence curve for the 2 cohorts and incidences that the hip fracture incidence curve is significantly higher than the non-hip fracture cohort (log-rank test p<0.001). After we adjusted for age, sex and comorbidities of diabetes, hypertension, hyperlipidemia, osteoporosis, CAD and heart failure and medication of aspirin, clopidogrel, warfarin, PPIs, statins, estrogen (only women), prednisolone, bisphosphonates, CCB, ACEI, ARB, alpha blocker, beta blocker, and diuretics, hip fracture patients compared to patients without hip fracture had a 1.54-fold risk of stroke (95% CI = 1.42-1.67). Hip fracture patients also had higher obvious incidence of
ischemic and hemorrhagic stroke. The stroke incidence was greater in women than in men in both cohorts. The sex-specific hip fracture cohort to non-hip fracture cohort relative incidence of stroke were significant for both women (adjusted HR=1.47, 95% CI=1.32-1.63) and men
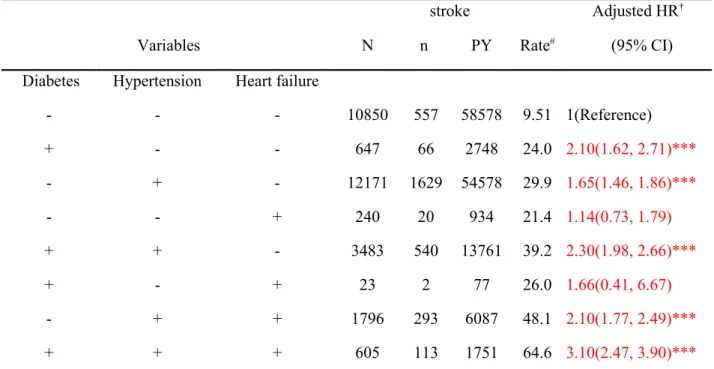
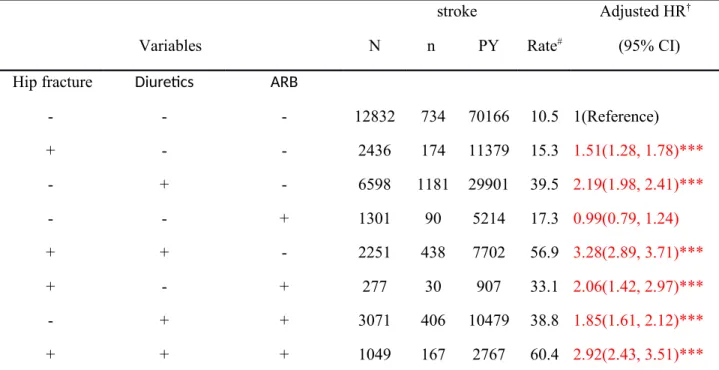
(adjusted HR=1.64, 95% CI=1.44-1.86). The incidence of stroke increased with age in both cohorts. The age-specific analysis showed that hip fracture patients had a greater incidence of stroke development than the non-hip fracture cohort in all age groups. In patients with any comorbidity, the risk of stroke was 1.50-fold greater in the hip fracture cohort than in the non-hip fracture cohort (95% CI=1.38-1.64). The highest risk occurred during the first 1 year of follow-up period (adjusted HR=1.96, 95% CI=1.67-2.28), and reduced with increasingly longer period to 1.29 for 4-5 years of follow-up. The risk remained for >5 years of follow-up. Table 3 shows the stroke incidence associated with the interaction of diabetes, hypertension, and heart failure. The stroke incidence was much higher in patients with diabetes, hypertension, and heart failure. Compared with those without diabetes, hypertension, and heart failure, patients with diabetes, hypertension, and heart failure exhibited an adjusted HR of 3.10 (95% CI = 2.47–3.90). We listed the interactions of hip fracture, diuretics and ARB on stroke risk in Table 4. Compared with patients who lacked hip fracture, diuretics and ARB, patients with both hip fracture, and diuretics demonstrated a significantly higher risk of stroke (adjusted HR = 3.28, 95% CI = 2.89-3.71), followed by simultaneous hip fracture, diuretics and ARB exhibited an adjusted HR of 2.92 (95% CI = 2.43–3.51).
Discussion
The results of the current study indicate that, after adjustment for potential confounding factors, patients with hip fracture are at a 1.54-fold risk of developing stroke compared with the comparison cohort. The finding is consistent with previous studies.13, 14 However, the studies by Kang et al and Popa et al, reported that there was increased risk of stroke within one year after hip fracture. 13, 14 Our study displayed the risk of stroke persisted during follow-up periods even more than 5 years. The highest risk of stroke occurred during the first 1 year of follow-up period
(adjusted HR=1.96, 95% CI=1.67-2.28), and followed by a 1.45-fold risk for 2-3 years follow-up, a 1.29-fold risk for 4-5 years follow-up, and a 1.46-fold risk for more than 5 years of follow-up.
The causality mediating stroke occurrence among patients with hip fracture remains unclear. A number of factors maybe involve the association of hip fracture and stroke. The genetic factor that might explain the association of hip fracture and stroke includes not only telomere length but also specific genes involved in cellular mechanisms shared by the vasculature and bone. 15, 16 Matrix proteins supporting bone, vessel walls, and the myocardium can be of special relevance.17, 18Other potential factors are calcification regulatory hormones, sex steroids, proteins related to
lipid metabolism, oxidative stress, and chronic inflammation.9, 19 Physical inactivity,
psychological distress, and pain are common after a hip fracture. 20 Disruption or deterioration of
pre-existing cardiovascular risk could be triggered in such circumstances. Studies have
demonstrated systemic migration of emboli to the brain through intracardiac or extracardiac right to left shunts resulting in stroke is more common than thought earlier. 21,22 In addition, the
hospitalization and surgery required for hip fracture treatment are associated with unfavorable physiological changes that exacerbate the predisposing factor in patients to cerebrovascular events.
In the current study, the risk of stroke after hip fracture was more prominent among young patients, male, those with diuretics, ABR and comorbid disorders. The higher risk observed for the presence of hip fracture and comorbid medical disorders might reflect a synergistic effect between these risk factors. The higher risk of younger age may be contributed to the genetic factor.15, 16 The relationship between gender differences and stroke risk remain controversial.23, 24 Antihypertensive medications were associated with an increased risk of a hip fracture.25 It is also indicated to increase a stroke risk with diuretics and ABR in the current study. It may be related to the dehydration and hypercoagulative status after hip fracture, which is a documented
complication which could trigger a stroke. 26 We did not investigate the impact of type of hip
fracture, anesthesia, or surgery in the current study. Dehydration is common in the elderly, dehydration before surgery nearly quadrupled the number of postoperative complications after hip fracture surgery.27 Be aware of the hydration status is the key to prevent the subsequent
complication risk. Embolic events from fat embolism, deep vein thrombosis, and pulmonary embolism are not uncommon in patients with hip fracture during acute and postoperative periods.28 Our study revealed the highest risk of stroke is within the first year after hip fracture,
and the risk is still high in the following years. It notices not only the need of short term prophylaxis for cerebrovascular event in primary care after fracture, but also long term prevention would be assigned.
The strength of our study is the use of a population-based data set with enrollment of a large number of subjects. The current cohort study confirms that hip fractures are associated with an increased risk of stroke development. However, several limitations must be considered when interpreting these findings. First, because a claims database was used, our study was unable to investigate the effects of risk factors such as body mass index, dietary habits, exercise capacity, and cigarette smoking in the regression model, which potentially compromise our findings. Because nutritional supplements were not covered by the national insurance project in Taiwan, information on vitamin D and calcium supplements is also lacking. We could not adjust our estimates for severity of stroke and comobidity. Bisphosphonate is widely used in treatment of osteoporosis and after hip fracture. The current study adjusts the risk between bisphosphonates and stroke. Although bisphosphate use is not related to the stroke risk in our study, the
cardiovascular safety of bisphosphonates for the treatment of osteoporosis is still in concern.29-32. Further study of dosage and course of different bisphosphonate and risk of stroke after hip
fracture and surgery is warrant in the future. After adjusting for these cofounders, hip fracture is still independently associated with increased risk of stroke in following years in our study.
In conclusion, hip fracture is independently associated with increased risk of developing stroke compared with controls. In addition, the risk of stroke after hip fracture is more prominent in younger patients, male, more cardiovascular comorbidities and in patients specific mediation use such as diuretics and ABR. Our study suggests that physicians should be proactive to prevent strokes given the subsequent higher risk of stroke among patients with hip fracture. A multidisciplinary approach, including medical, orthopedic, and rehabilitative specialty collaboration, is suggested to address any level of stroke risk, both short-term and long-term risks. Controlling cerebrovascuar risks, early mobilization, hyertension medication adjustment, and adequate hydration may become pivotal roles to decrease the risk of stroke after hip fracture.
References
1. Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761-1767
2. Fisher AA, Davis MW, Rubenach SE, Sivakumaran S, Smith PN, Budge MM. Outcomes for older patients with hip fractures: The impact of orthopedic and geriatric medicine cocare. J Orthop Trauma. 2006;20:172-178; discussion 179-180
3. Bentler SE, Liu L, Obrizan M, Cook EA, Wright KB, Geweke JF, Chrischilles EA, Pavlik CE, Wallace RB, Ohsfeldt RL, Jones MP, Rosenthal GE, Wolinsky FD. The aftermath of hip fracture: Discharge placement, functional status change, and mortality. Am J
Epidemiol. 2009;170:1290-1299
4. Kannus P, Parkkari J, Sievanen H, Heinonen A, Vuori I, Jarvinen M. Epidemiology of hip fractures. Bone. 1996;18:57S-63S
5. Melton LJ. Who has osteoporosis? A conflict between clinical and public health perspectives. Journal of Bone and Mineral Research. 2000;15:2309-2314
6. Sennerby U, Melhus H, Gedeborg R, Byberg L, Garmo H, Ahlbom A, Pedersen NL, Michaelsson K. Cardiovascular diseases and risk of hip fracture. JAMA. 2009;302:1666-1673
7. Batsis JA, Huddleston JM, Melton LJt, Huddleston PM, Lopez-Jimenez F, Larson DR, Gullerud RE, McMahon MM. Body mass index and risk of adverse cardiac events in elderly patients with hip fracture: A population-based study. J Am Geriatr Soc. 2009;57:419-426
8. McFarlane SI. Bone metabolism and the cardiometabolic syndrome: Pathophysiologic insights. J Cardiometab Syndr. 2006;1:53-57
9. McFarlane SI, Muniyappa R, Shin JJ, Bahtiyar G, Sowers JR. Osteoporosis and cardiovascular disease: Brittle bones and boned arteries, is there a link? Endocrine. 2004;23:1-10
10. Chiang CH, Liu CJ, Chen PJ, Huang CC, Hsu CY, Chen ZY, Chan WL, Huang PH, Chen TJ, Chung CM, Lin SJ, Chen JW, Leu HB. Hip fracture and risk of acute myocardial infarction: A nationwide study. J Bone Miner Res. 2013;28:404-411
11. Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML. Validation of the national health insurance research database with ischemic stroke cases in taiwan. Pharmacoepidemiology and drug
safety. 2011;20:236-242
12. Chung WS, Lin CL, Peng CL, Chen YF, Lu CC, Sung FC, Kao CH. Rheumatoid arthritis and risk of acute myocardial infarction--a nationwide retrospective cohort study.
International journal of cardiology. 2013;168:4750-4754
13. Kang JH, Chung SD, Xirasagar S, Jaw FS, Lin HC. Increased risk of stroke in the year after a hip fracture: A population-based follow-up study. Stroke; a journal of cerebral
circulation. 2011;42:336-341
14. Popa AS, Rabinstein AA, Huddleston PM, Larson DR, Gullerud RE, Huddleston JM. Predictors of ischemic stroke after hip operation: A population-based study. J Hosp Med. 2009;4:298-303
15. Wong LS, de Boer RA, Samani NJ, van Veldhuisen DJ, van der Harst P. Telomere biology in heart failure. Eur J Heart Fail. 2008;10:1049-1056
16. Valdes AM, Richards JB, Gardner JP, Swaminathan R, Kimura M, Xiaobin L, Aviv A, Spector TD. Telomere length in leukocytes correlates with bone mineral density and is shorter in women with osteoporosis. Osteoporos Int. 2007;18:1203-1210
17. Baldini V, Mastropasqua M, Francucci CM, D'Erasmo E. Cardiovascular disease and osteoporosis. J Endocrinol Invest. 2005;28:69-72
18. Hofbauer LC, Brueck CC, Shanahan CM, Schoppet M, Dobnig H. Vascular calcification and osteoporosis--from clinical observation towards molecular understanding.
Osteoporos Int. 2007;18:251-259
19. Theill LE, Boyle WJ, Penninger JM. Rank-l and rank: T cells, bone loss, and mammalian evolution. Annu Rev Immunol. 2002;20:795-823
20. Dharmarajan TS, Banik P. Hip fracture. Risk factors, preoperative assessment, and postoperative management. Postgrad Med. 2006;119:31-38
21. Tateishi Y, Iguchi Y, Kimura K, Kobayashi K, Shibazaki K, Eguchi K. Right-to-left shunts may be not uncommon cause of tia in japan. J Neurol Sci. 2009;277:13-16 22. Bannan A, Shen R, Silvestry FE, Herrmann HC. Characteristics of adult patients with
atrial septal defects presenting with paradoxical embolism. Catheter Cardiovasc Interv. 2009;74:1066-1069
23. Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Au R, Kannel WB, Wolf PA. The lifetime risk of stroke: Estimates from the framingham study. Stroke; a journal of
cerebral circulation. 2006;37:345-350
24. Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, Haase N, Ho M, Howard V, Kissela B, Kittner S, Lloyd-Jones D, McDermott M, Meigs J, Moy C, Nichol G, O'Donnell CJ, Roger V, Rumsfeld J, Sorlie P, Steinberger J, Thom T, Wasserthiel-Smoller S, Hong Y. Heart disease and stroke statistics--2007 update: A report from the american heart association statistics committee and stroke statistics subcommittee.
Circulation. 2007;115:e69-171
25. Tinetti ME, Han L, Lee DS, McAvay GJ, Peduzzi P, Gross CP, Zhou B, Lin H. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med. 2014;174:588-595
26. Wilson D, Cooke EA, McNally MA, Wilson HK, Yeates A, Mollan RA. Altered venous function and deep venous thrombosis following proximal femoral fracture. Injury. 2002;33:33-39
27. Ylinenvaara SI, Elisson O, Berg K, Zdolsek JH, Krook H, Hahn RG. Preoperative urine-specific gravity and the incidence of complications after hip fracture surgery: A
prospective, observational study. Eur J Anaesthesiol. 2014;31:85-90 28. Rosencher N, Vielpeau C, Emmerich J, Fagnani F, Samama CM. Venous
thromboembolism and mortality after hip fracture surgery: The escorte study. Journal of
thrombosis and haemostasis : JTH. 2005;3:2006-2014
29. John Camm A. Review of the cardiovascular safety of zoledronic acid and other bisphosphonates for the treatment of osteoporosis. Clin Ther. 2010;32:426-436
30. Black DM, Reid IR, Boonen S, Bucci-Rechtweg C, Cauley JA, Cosman F, Cummings SR, Hue TF, Lippuner K, Lakatos P, Leung PC, Man Z, Martinez RL, Tan M, Ruzycky ME, Su G, Eastell R. The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: A randomized extension to the horizon-pivotal fracture trial (pft). J Bone
31. Sharma A, Chatterjee S, Arbab-Zadeh A, Goyal S, Lichstein E, Ghosh J, Aikat S. Risk of serious atrial fibrillation and stroke with use of bisphosphonates: Evidence from a meta-analysis. Chest. 2013;144:1311-1322
32. Huang WF, Tsai YW, Wen YW, Hsiao FY, Kuo KN, Tsai CR. Osteoporosis treatment and atrial fibrillation: Alendronate versus raloxifene. Menopause. 2010;17:57-63
Table 1. Comparison of demographics and comorbidity between hip fracture patients and controls Hip fracture No(N=23802) Yes(N=6013) n % n % p-value Sex 0.53 Women 13022 54.7 3317 55.2 Men 10780 45.3 2696 44.8 Age, year 0.81 20-49 2680 11.3 670 11.1 50-64 2992 12.6 748 12.4 65-79 9354 39.3 2337 38.9 80+ 8776 36.9 2258 37.6 Mean (SD) 71.2 15.9 72.4 16.1 <0.001† Comorbidity Diabetes 3390 14.2 1368 22.8 <0.001 Hypertension 14096 59.2 3959 65.8 <0.001 Hyperlipidemia 6509 27.4 1457 24.2 <0.001 Osteoporosis 3614 15.2 1395 23.2 <0.001 CAD 7565 31.8 2059 34.2 <0.001 Heart failure 1975 8.30 689 11.5 <0.001 Medications Aspirin 11749 49.4 3559 59.2 <0.001 Clopidogrel 634 2.66 241 4.01 <0.001 Warfarin 400 1.68 135 2.25 0.003 PPIs 3608 15.2 1307 21.7 <0.001 Statins 3725 15.7 953 15.9 0.70
Estrogen (only women) 3246 13.6 762 12.7 0.05 Prednisolone 12779 53.7 3428 57.0 <0.001 Bisphosphonates 456 1.92 243 4.04 <0.001 Calcium channel blocker (CCB) 12231 51.4 3772 62.7 <0.001 ACEI 8127 34.1 2436 40.5 <0.001 ARB 4372 18.4 1326 22.1 <0.001 Alpha blocker 4380 18.4 1340 22.3 <0.001 Beta blocker 11182 47.0 3197 53.2 <0.001 Diuretics 9669 40.6 3300 54.9 <0.001
Table 2. Incidence and adjusted hazard ratio of stroke stratified by sex, age and comorbidity compared between with hip fracture and without hip fracture
Hip fracture
Compared to without Non- fracture
No Yes
Variables Case PY Rate# Case PY Rate# Crude HR * (95% CI) Adjusted HR† (95% CI) All 2411 115760 20.8 809 22755 35.6 1.69(1.56, 1.83)*** 1.54(1.42, 1.67)*** Ischemic stroke 2128 18.4 722 31.7 1.71(1.57, 1.86)*** 1.55(1.42, 1.69)*** Hemorrhagic stroke 283 2.44 87 3.82 1.55(1.22, 1.98)*** 1.48(1.16, 1.89)*** Sex Women 1371 62397 22.0 469 12521 37.5 1.70(1.53, 1.89)*** 1.47(1.32, 1.63)*** Men 1040 53363 19.5 340 10234 33.2 1.68(1.49, 1.90)*** 1.64(1.44, 1.86)*** Age 20-49 19 16983 1.12 21 3947 5.32 4.76(2.56, 8.86)*** 2.31(1.14, 4.70)* 50-64 113 16956 6.66 64 3537 18.1 2.71(1.99, 3.69)*** 1.82(1.31, 2.52)*** 65-79 1025 49287 20.8 388 9159 42.4 2.07(1.84, 2.33)*** 1.75(1.55, 1.98)*** 80+ 1254 32533 38.6 336 6111 55.0 1.43(1.27, 1.61)*** 1.35(1.19, 1.52)*** Comorbidity No 355 42872 8.28 98 7547 13.0 1.56(1.25, 1.96)*** 1.25(0.99, 1.57) Yes 2056 72887 28.2 711 15207 46.8 1.65(1.52, 1.80)*** 1.50(1.38, 1.64)*** Follow time, years
≤1 484 23021 21.0 256 5346 47.9 2.28(1.96, 2.65)*** 1.96(1.67, 2.28)*** 2-3 788 37484 21.0 272 7817 34.8 1.65(1.44, 1.90)*** 1.45(1.26, 1.67)*** 4-5 547 25523 21.4 143 4766 30.0 1.40(1.16, 1.68)*** 1.29(1.07, 1.56)** >5 592 29732 19.9 138 4826 28.6 1.44(1.19, 1.73)*** 1.46(1.20, 1.76)***
Adjusted HR† : multivariable analysis including age, sex, co-morbidities of diabetes, hypertension, hyperlipidemia, osteoporosis, CAD, and heart failure, medications of aspirin, clopidogrel, warfarin, PPIs, statins, estrogen (only women), prednisolone, bisphosphonates, calcium channel blocker (CCB), ACEI, ARB, Alpha blocker, Beta blocker, and diuretics; *p<0.05, **p<0.01, ***p<0.001
Comorbidity‡: Only to have one of comorbidities (including diabetes, hypertension, hyperlipidemia, osteoporosis, CAD, and heart failure) classified as the comorbidity group
Table 3. Development of stroke in patients with hip fracture by interaction of diabetes, hypertension, heart failure
stroke Adjusted HR†
Variables N n PY Rate# (95% CI)
Diabetes Hypertension Heart failure
- - - 10850 557 58578 9.51 1(Reference) + - - 647 66 2748 24.0 2.10(1.62, 2.71)*** - + - 12171 1629 54578 29.9 1.65(1.46, 1.86)*** - - + 240 20 934 21.4 1.14(0.73, 1.79) + + - 3483 540 13761 39.2 2.30(1.98, 2.66)*** + - + 23 2 77 26.0 1.66(0.41, 6.67) - + + 1796 293 6087 48.1 2.10(1.77, 2.49)*** + + + 605 113 1751 64.6 3.10(2.47, 3.90)*** N, sample size; n, events of stroke; Rate#, incidence rate, per 1,000 person-years; Adjusted HR†:
multivariable analysis including age, sex, co-morbidities of hyperlipidemia, osteoporosis, and CAD, medications of aspirin, clopidogrel, warfarin, PPIs, statins, estrogen (only women), prednisolone, bisphosphonates, calcium channel blocker (CCB), ACEI, Alpha blocker, and Beta blocker; *p<0.05, **p<0.01, ***p<0.001
Table 4. Development of stroke in patients with hip fracture associated with Medications of Diuretics and ARB
stroke Adjusted HR†
Variables N n PY Rate# (95% CI)
Hip fracture Diuretics ARB
- - - 12832 734 70166 10.5 1(Reference) + - - 2436 174 11379 15.3 1.51(1.28, 1.78)*** - + - 6598 1181 29901 39.5 2.19(1.98, 2.41)*** - - + 1301 90 5214 17.3 0.99(0.79, 1.24) + + - 2251 438 7702 56.9 3.28(2.89, 3.71)*** + - + 277 30 907 33.1 2.06(1.42, 2.97)*** - + + 3071 406 10479 38.8 1.85(1.61, 2.12)*** + + + 1049 167 2767 60.4 2.92(2.43, 3.51)*** N, sample size; n, events of stroke; Rate#, incidence rate, per 1,000 person-years; Adjusted HR†:
multivariable analysis including age, sex, co-morbidities of diabetes, hypertension, hyperlipidemia, osteoporosis, CAD, and heart failure, medications of aspirin, clopidogrel, warfarin, PPIs, statins, estrogen (only women), prednisolone, bisphosphonates, calcium channel blocker (CCB), ACEI, Alpha blocker, and Beta blocker; *p<0.05, **p<0.01, ***p<0.001