ContentslistsavailableatSciVerseScienceDirect
International
Journal
of
Antimicrobial
Agents
j o ur na l ho me p ag e :ht t p : / / w w w . e l s e v i e r . c o m / l o c a t e / i j a n t i m i c a g
Review
Does
empirical
treatment
of
community-acquired
pneumonia
with
fluoroquinolones
delay
tuberculosis
treatment
and
result
in
fluoroquinolone
resistance
in
Mycobacterium
tuberculosis?
Controversies
and
solutions
Gwan-Han
Shen
a,
Thomas
Chang-Yao
Tsao
b,
Shang-Jyh
Kao
c,
Jen-Jyh
Lee
d,
Yen-Hsu
Chen
e,
Wei-Chung
Hsieh
f,
Gwo-Jong
Hsu
g,
Yen-Tao
Hsu
h,
Ching-Tai
Huang
i,
Yeu-Jun
Lau
j,
Shih-Ming
Tsao
k, Po-Ren
Hsueh
l,∗aDivisionofRespiratoryandCriticalCareMedicine,DepartmentofInternalMedicine,TaichungVeteransGeneralHospital,Taichung,Taiwan
bDivisionofRespiratoryandCriticalCareMedicine,DepartmentofInternalMedicine,SchoolofMedicine,ChungShanMedicalUniversity,andUniversityHospital,Taichung,Taiwan cPulmonaryDivision,DepartmentofInternalMedicine,ShinKongWuHo-SuMemorialHospital,Taipei,Taiwan
dTBLaboratorySection,DepartmentofInternalMedicine,BuddhistTzuChiGeneralHospital,HualienandTzuChiUniversity,Hualien,Taiwan
eDivisionofInfectiousDiseases,DepartmentofInternalMedicine,KaohsiungMedicalUniversityHospital,GraduateInstituteofMedicine,KaohsiungMedicalUniversity,Kaohsiung, Taiwan
fDivisionofRespiratoryandCriticalCareMedicine,DepartmentofInternalMedicine,DaChienGeneralHospital,Maioli,Taiwan
gDivisionofInfectiousDiseases,DepartmentofInternalMedicine,DitmansonMedicalFoundationChia-YiChristianHospital,Chia-Yi,Taiwan hDivisionofPulmonaryandCriticalCareMedicine,DepartmentofInternalMedicine,TaipeiCityHospital,HepingFuyouBranch,Taipei,Taiwan iDivisionofInfectiousDiseases,DepartmentofMedicine,ChangGungUniversityandMemorialHospital,Taiwan
jInfectiousDiseases,DepartmentofInternalMedicine,ShowChwanMemorialHospital,Taichung,Taiwan
kInfectiousSection,InternalMedicineDepartment,InstituteofMicrobiologyandImmunology,ChungShanMedicalUniversity,andUniversityHospital,Taichung,Taiwan lDepartmentsofLaboratoryMedicineandInternalMedicine,NationalTaiwanUniversityHospital,NationalTaiwanUniversityCollegeofMedicine,No.7Chung-ShanSouthRoad, Taipei100,Taiwan
a
r
t
i
c
l
e
i
n
f
o
Keywords: Community-acquiredpneumonia Fluoroquinolones Tuberculosis Fluoroquinoloneresistance Multidrug-resistantMycobacterium tuberculosisa
b
s
t
r
a
c
t
Theroleoffluoroquinolones (FQs)asempiricaltherapyforcommunity-acquiredpneumonia(CAP) remainscontroversialincountrieswithhightuberculosis(TB)endemicityowingtothepossibilityof delayedTBdiagnosisandtreatmentandtheemergenceofFQresistanceinMycobacteriumtuberculosis. Althoughtheratesofmacrolide-resistantStreptococcuspneumoniaeandamoxicillin/clavulanic acid-resistantHaemophilusinfluenzaehaverisentoalarminglevels,theratesofrespiratoryFQ(RFQ)resistance amongsttheseisolatesremainrelativelylow.Itisreportedthatca.1–7%ofCAPcasesarere-diagnosed aspulmonaryTBinAsiancountries.Alongerduration(≥7days)ofsymptoms,ahistoryofnightsweats, lackoffever(>38◦C),infectioninvolvingtheupperlobe,presenceofcavitaryinfiltrates,opacityinthe lowerlungwithoutthepresenceofair,lowtotalwhitebloodcellcountandthepresenceoflymphopenia arepredictiveofpulmonaryTB.AmongstpatientswithCAPwhoresideinTB-endemiccountrieswho aresuspectedofhavingTB,imagingstudiesaswellasaggressivemicrobiologicalinvestigationsneedto beperformedearlyon.PreviousexposuretoaFQfor>10daysinpatientswithTBisassociatedwith theemergenceofFQ-resistantM.tuberculosisisolates.However,ratesofM.tuberculosisisolateswithFQ resistancearesignificantlyhigheramongstmultidrug-resistantM.tuberculosisisolatesthanamongst sus-ceptibleisolates.Consequently,inTaiwanandalsoinothercountrieswithTBendemicity,ashort-course (5-day)regimenofaRFQisstillrecommendedforempiricaltherapyforCAPpatientsifthepatientisat lowriskforTB.
© 2012 Elsevier B.V. and the International Society of Chemotherapy. All rights reserved.
1. Introduction
Community-acquired pneumonia (CAP) is one of the lead-ingcausesofdeathworldwide.Themortalityratehasincreased
∗ Correspondingauthor.
E-mailaddress:hsporen@ntu.edu.tw(P.-R.Hsueh).
significantlyoverthepast10yearsnotonlyinTaiwanbutalsoin othercountriesintheAsia-Pacificregion[1–3].Thekeycausative pathogens of CAP are Streptococcus pneumoniae, Haemophilus influenzaeandatypicalpathogens[1–3].Accordingtothe antimi-crobialtreatmentguidelinesoftheInfectiousDiseasesSocietyof America, theAmerican ThoracicSociety, the European Respira-torySocietyandtheInfectiousDiseasesSocietyofTaiwan[1–3], thedrugsofchoiceforCAPinoutpatientsarepenicillin-related
0924-8579/$–seefrontmatter © 2012 Elsevier B.V. and the International Society of Chemotherapy. All rights reserved. doi:10.1016/j.ijantimicag.2011.11.014
agents if urine cultures are positive for pneumococcal antigen, andmacrolide-ortetracycline-relatedagentsifurineculturesare negativeforpathogens.However,therateofpenicillin,macrolide andtetracyclineresistanceamongstS.pneumoniaeisolatesishigh inTaiwan[4].TheantibioticoptionsforinpatientswithCAPare -lactams or respiratory fluoroquinolones (RFQs) (levofloxacin, moxifloxacinandgemifloxacin).IntheIntensiveCareUnit(ICU), a-lactamantibioticcombinedwitha macrolideorwitha flu-oroquinolone(FQ)isappropriate[1–3].However,theincreasing resistanceofkey pathogens to-lactamantibiotics posesgreat challengestophysiciansinTaiwan.RFQscanbeusedinthe treat-ment of CAP in outpatients[5], inpatients and patients in the ICU.RFQshavebeenshowntohaveexcellentactivityagainstkey causativepathogensofCAPaswellasatypicalpathogens; how-ever,useofRFQsforempiricaltreatmentofCAPmightmaskthe diagnosisoftuberculosis(TB),leadingtodelayedtreatmentandFQ resistanceamongstsubsequentlyisolatedMycobacterium tubercu-losisstrains.
Thisarticle brieflyreviews thecommon microbial causesof CAP,theresistanceratesamongstkeypathogens,andtheproper administrationofFQsinthetreatmentofCAP.Theincidenceofand mortalityassociatedwithTBandthestatusofmultidrug-resistant M.tuberculosis(MDR-TB)inTaiwanarealsodescribed.Inaddition, wereviewthecontroversiessurroundingtheempiricaluseofFQs totreatpatientswithCAP,treatmentoptionsforpatientswitha delayedTBdiagnosis,andtheemergenceofFQresistanceamongst M.tuberculosisisolates.
2. Community-acquiredpneumonia
2.1. Aetiologyofcommunity-acquiredpneumoniainTaiwan Lauderdaleetal.collected168isolatesfrom468patientsfrom December2001toApril2002inTaiwanandfoundthatthemost commoncauseof CAPamongst adultpatientsinTaiwanwasS. pneumoniae(24%), followed byatypicalpathogens (Mycoplasma pneumoniae, Chlamydophila pneumoniae and Legionella pneu-mophila),H.influenzaeandKlebsiellapneumoniae[6].Theaetiology ofCAPwasundeterminedinca.40%ofCAPcases[6,7]. Staphylo-coccusaureuswasthecausativepathogenin2%ofCAPcases,and theoverallmortalityrateofpatientswithCAPwas8.3%[6]. 2.2. Antimicrobialsusceptibilityprofilesamongstrespiratory pathogens
Lin et al. foundthat amongst all S.pneumoniae strains that caused bacteraemia, only 29.2% were susceptible to penicillin, 15.1% to erythromycin, 18% to tetracycline and 33.7% to clin-damycin [8]. However, 96.4% were susceptible to cefotaxime, 97.3%tolevofloxacin and 98.4%tomoxifloxacin. Amongst non-bacteraemicstrains,only23.8%weresusceptibletopenicillin,5% toerythromycin,30%totetracyclineand30%toclindamycin. How-ever,theratesofsusceptibilityamongstS.pneumoniaeisolatesto cefotaxime,levofloxacinandmoxifloxacinwereeach100%[8].
Therateofnon-susceptibilityofS.pneumoniaetolevofloxacinin amedicalcentreinTaiwanwas1.2%in2005,peakedat4.2%in2007 andthengraduallydecreasedto3%in2010[9].Formoxifloxacin, thenon-susceptibleratewas1.3%in2005,4%in2008andthen graduallydecreasedto1%in2009and2010.Hsiehetal.alsoshowed thattheprevalenceofFQ-resistantS.pneumoniaeisolatesinTaiwan waslow,even thoughFQs arewidelyused inthat country[9]. AmongsttheFQ-non-susceptibleisolatesinthatstudy,serotype 9V(20%)wasthemostcommon,followedby19F(6.8%),23F(3.9%) and14F(1.8%)[10].Theseserotypesareallvaccine-typeS. pneumo-niae.Fig.1showstheproportionoflevofloxacinresistanceamongst
Fig.1.Proportionoflevofloxacin-susceptibleStreptococcuspneumoniae isolates obtainedfrom12majorteachinghospitalsindifferentpartsofTaiwan,2010.N1–N5, fivehospitalsinNorthTaiwan;M1–M2,twohospitalsincentralTaiwan;S1–S4,four hospitalsinsouthernTaiwan;andE1,onehospitalineasternTaiwan.
S.pneumoniaeisolatedfrom12majorteachinghospitalslocatedin differentpartsofTaiwanin2010.Themajority(81–100%)oftheS. pneumoniaeisolatesweresusceptibletolevofloxacin[9].
ThesusceptibilityrateofH.influenzaetoamoxicillin/clavulanic acid(AMC)decreasedmarkedlyfrom95%in2002to88%in2009 inamedicalcentreinTaiwan[11].AMCshouldbeadministered withcautiontopatientswithCAP.Inaddition,Jean and Hsueh showedthattherateofextended-spectrum-lactamase (ESBL)-producing K.pneumoniae strainsin Taiwan was26% [4]. Wang etal.foundthattheresistanceratestoAMC,cefuroxime,cefaclor, ceftazidime, ceftriaxone and levofloxacin amongst K. pneumo-niaeisolatesassociatedwithcommunity-acquiredrespiratorytract infectionwereall≤10%[12].Amongst101community-acquired meticillin-resistant S. aureus (CA-MRSA) isolated in a medical centreinTaiwan,96%weresusceptibletolevofloxacinand mox-ifloxacin[13].
RegardingatypicalpathogensinTaiwan,theratesof suscepti-bilitytolevofloxacinwerereportedtobe93.9%forM.pneumoniae, 85.7%forC.pneumoniaeand100%forL.pneumophila[14]. 2.3. Roleofrespiratoryfluoroquinolonesinthetreatmentof community-acquiredpneumonia
InTaiwan,patientswithCAPwhowerepreviouslyhealthyand havenotusedantibioticsinthe3monthspriortodiseaseonset arenormallygivenamacrolideordoxycyclineasoutpatient treat-ment [3]. However,the rates of non-susceptibilityto penicillin anderythromycinamongstclinicalisolatesofS.pneumoniaehave increasedmarkedlyinrecentyears[4].Therefore,cautionshouldbe exercisedbeforeadministeringmacrolidesforCAPunlessatypical pathogensarehighlysuspected.Forpatientswithco-morbidities, aRFQora-lactamantibioticplusmacrolideissuggested[3].For inpatientswithco-morbidities,especiallyintheICU,a-lactam antibioticpluseitherazithromycinoraFQissuggested[1–3].For atypicalpathogens,FQsareaseffectiveasmacrolides.Thelength ofstayinhospitalandthetimetoclinicalstabilityfavourtheuseof FQs[15].Dragoetal.showedthatthecombinationoflevofloxacin withceftriaxoneproducedthehighestrateofsynergy(54%),mainly againstmacrolide-resistantisolates,whereasclarithromycin com-binedwithAMCwasshowntobeantagonisticin22%ofisolates
[16].NoantagonismwasnotedbetweenFQand-lactam antibi-otics[16].Theprevalenceoflevofloxacin-resistantS.pneumoniae increasedmarkedlyduringtheperiod2001–2007inHongKong, especiallyamongsttheelderly[17].Themostcommonaetiologyof levofloxacinresistancewassuboptimaluseofaFQinwhichsmall
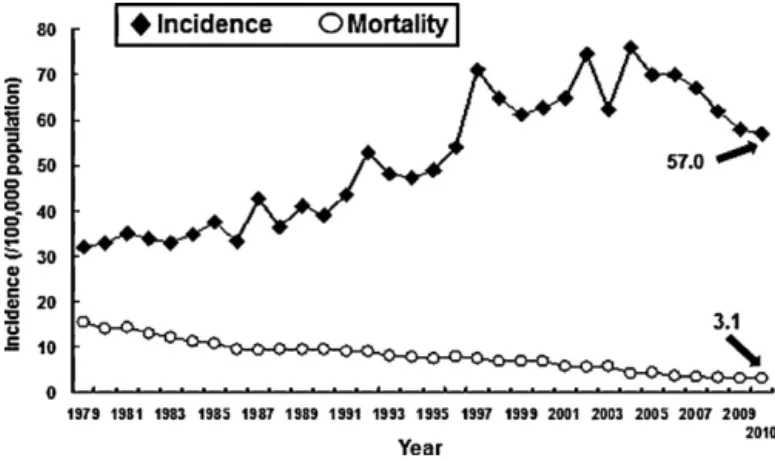
Fig.2. Incidenceofandmortalityrates(per100000population)associatedwith tuberculosisinTaiwan,1979–2010.
doses(100–200mg)ofofloxacinandlevofloxacinwere adminis-teredtwoorthreetimesdaily.Accordingly,appropriatedosesof aRFQ(levofloxacin,750mg/day;moxifloxacin, 400mg/day;and gemifloxacin,320mg/day)arerecommended[1–3].
3. Tuberculosisandcommunity-acquiredpneumonia
3.1. TuberculosisinTaiwan
TheincidenceofTBwas75casesper100000populationin2002, butdecreasedto62casesper100000populationin2003becauseof thesevereacuterespiratorysyndrome(SARS)outbreak(Fig.2).In 2004,theincidencereboundedto76casesper100000population (16784newcases)[18].In2005,theTaiwanCentersforDisease Control(CDC)performeda‘StopTBProgram’totrytoreducethe incidencebyone-half.From2005to2010theTBincidencerate decreasedfrom70to57per100000populationandthemortality ratedecreasedfrom4.3to3per100000population(Fig.2).The overallnumberofpatientswhodieddecreasedfrom970in2005 to700in2010.Thelong-termtrendinTBmortalityalsodecreased from294per100000populationin1947to3per100000in2010. 3.2. Proportionoftuberculosisamongstpatientswith
community-acquiredpneumonia
Fig.3demonstratestheproportionsofTBamongstpatients ini-tiallydiagnosed as havingCAPin differentcountries. The rates rangedfrom1–3%inTaiwanto7%inIndia[6,7,19,20].Themajority (>50%)ofthosepatientswithCAPduetoTBwereofadvancedage (>65years)andhadvariousco-morbidities[6].
Fig. 3.Proportion of Mycobacterium tuberculosis as the causative agent of community-acquiredpneumonia(CAP)inseveralcountries.
3.3. Antimicrobialresistanceandmultidrugresistanceamongst Mycobacteriumtuberculosisisolates
TheTaiwanCDCreportedthattherewasamarkeddifferencein antimicrobialresistanceratesbetweenpatientswithincidentTB andpatientswithrecurrentTB[21];theratesofresistancewere, respectively,9%and18%toisoniazid,2%and10%torifampicin,2% and7%toethambutol,8%and12%tostreptomycinand14%and23% toanyfirst-linedrugduring2009–2010(http://www.cdc.gov.tw). Theratesofresistancetofirst-linedrugstendedtodecrease dur-ing2000–2010exceptfortherateofresistancetostreptomycin, which remainedstable.TherateofincidentMDR-TBwas1%in 2010.Therateofresistancetoanydrugclassaswellasthe inci-dence of MDR-TB also showeda downward trend during that decade[22].
3.4. FluoroquinoloneresistanceamongstMycobacterium tuberculosisisolatesinTaiwan
Duringtheperiod2000–2006,theFQresistancerateamongst non-MDR-TBisolatesinTaiwanwas0.1%,thatamongstisolates frompatientswithpreviousanti-TBtreatmentwas7.9%andthat amongstMDR-TBisolateswas16.7%[23].Wangetal.evaluated FQ susceptibilityaswell asgeneticmutationsamongst isolates frompatientswhohadbeenexposedtoFQsfromJanuary2004 toDecember2005[24].Theyfoundthatmultipledrugresistance hadthestrongestcorrelationwithFQresistance(19%ofisolates)
[24].NeitherprevioususeofFQsnorthedurationofFQexposure wascorrelatedwithFQsusceptibility.Amongst theFQ-resistant isolates,35.7%hadagyrAmutation(D94GandA90V)and7.1%had agyrBmutation(N538)[24].
Amongstthe215MDR-TBisolatesfromTaiwanreportedbyYu etal., 42.8%wereresistanttoofloxacin[21].Therateof exten-sively drug-resistant TB (XDR-TB) was 10.3% in 2004 (12/116 isolates)and10.1%in2005(10/99isolates)[21].Accordingtothe annual reportfrom TaiwanCDC,therate ofFQ-resistant MDR-TB isolateswas29.1% (144/494)fromJuly2009toMarch2009 (http://www.cdc.gov.tw).In total,43MDR-TBisolateswerealso resistanttocapreomycin,amikacinorkanamycin.Therateof XDR-TBamongstMDR-TBisolateswas8.7%.NearlyallFQ-resistantM. tuberculosisisolateswerefoundamongstMDR-TBisolates(Fig.4)
[20–26].ThemostcommonsitesfromwhichFQ-resistantM. tuber-culosisisolateswereobtainedwerethegenitourinarytract(5.1%), pulmonarytract(1.5%)andpleuralcavity(1.0%)[22].
Fig.4. Proportionofquinoloneresistanceamongstmultidrug-resistant Mycobac-teriumtuberculosis(MDR-TB)andnon-MDR-TBisolatesinTaiwan[21–24,26].
3.5. Empiricaluseoffluoroquinolonesamongst community-acquiredpneumoniapatientsanddelayed tuberculosisdiagnosisandtreatment
Dooley et al. wasthe first topoint out the possibility that empiricaltreatmentwitha FQ mightdelay thediagnosisof TB
[27].AmongstpatientswhoreceivedempiricalFQtreatment,the mediantimebetweensymptomonsetandreceiptofanti-TB med-ication was 21 days compared with a median time of 5 days amongstthosewhodidnotreceiveFQs[27,28].However,the sam-plesizeintheirstudywassmall.Ofthe17patientswhodidnot receive FQs,7 receivedanti-TB therapy and 3 patientsdid not receiveantibiotictreatment.The initialacid-fast bacillussmear waspositivein8ofthosepatients.TBwassuspectedinatleast one-halfofthepatientswhodidnot receiveFQs,soantibiotics werenot prescribed and anti-TB treatmentwas given directly. Interestingly, of those patients who received FQ monotherapy, 83%experiencedimprovementinthesymptomsofTB,and clini-calimprovementoccurredanaverageof3daysaftertheinitiation oftherapy.Otherstudieshavealsoreportedthatthedelayin ini-tiationofanti-TBmedicationwaslongeramongst patientswho receivedFQsthanamongstpatientswhodidnotreceiveFQ-based antibiotics(43.1±40.0daysvs.18.7±16.9days;P=0.04)[28–30]. Medianhealthcaredelayforpatientswhoreceivedantibioticsfor non-TBdiagnoses/indicationsprior toTBdiagnosiswas39 days versus15days (P<0.01)for patientswho hadinitiallyreceived TB therapy [26]. Notonly didadministration of a FQ result in adelayeddiagnosisofTB (median29 days),but administration ofotherantibiotics(suchas-lactams,macrolidesor carbapen-ems)hadasimilareffect(median31days).InthestudybyGolub etal.,only57%ofpatientsinitiallydiagnosedashavingpneumonia hadachestradiograph[31].Interestingly,34%ofthechest radio-graphssuggesteda diagnosisofTB;however,thepatientswere stillsubsequently prescribedempiricalantibiotics.More impor-tantly,bothantibioticuseandnothavingachestradiographtaken during thefirst healthcare visit were independently related to longerhealthcaredelaysintheoverallcohort.Mathuretal.showed that ca. 44–55% of active TB patients were given an incorrect diagnosisattheinitialpresentation,mainlybecauseof atypical radiographicmanifestations [32].A studyfromMalaysiaclearly demonstratedthat a duration ofsymptoms of>2 weeksbefore hospitaladmission [oddsratio (OR)=25.1;P<0.001), history of nightsweats(P=0.038),a chestradiographshowingupperlobe involvement(P=0.012)or cavitaryinfiltrates (P=0.002),a total whitebloodcellcountof≤12×109/Lonadmission(P=0.029)and
lymphopenia(P=0.040)]wassignificantlyassociatedwith culture-positivepulmonaryTB(Fig.5)[19].Inaddition,lowerlungfieldTB (LLFTB)isdifficulttodifferentiatefrompneumonia andisoften
Fig.5.Clinicalandlaboratorypredictorsofpatientswithtuberculosiswhowere initiallydiagnosedashavingcommunity-acquiredpneumonia[19].CXR,chest radiography;WBC,whitebloodcellcount.
misdiagnosedbecauseof atypicalfindingsonchest radiographs
[33,34].InTaiwan,ca.20%ofpulmonaryTBpatientshaveLLFTB
[33]. Multivariateanalysis conductedby Lin et al. showedthat prolongedduration ofsymptoms ≥7 days(OR=4.57; P=0.038), lackoffever >38◦C (OR=9.04;P=0.001)and theabsenceofair bronchograms(OR=12.08;P=0.007)weresignificantpredictorsof LLFTBinpatientswithLLFpneumonia[35].Acalculatedprobability of>0.36suggestsLLFTBwithasensitivityof81.8%andaspecificity of86.1%[35].
3.6. Empiricaluseoffluoroquinolones(FQs)amongst
community-acquiredpneumoniapatientsandtheemergenceof FQresistanceinMycobacteriumtuberculosis
Recently,Laietal.reportedthattheFQresistancerateinM. tuberculosiswasonly1.3%inTaiwanduring2005–2010[25].Prior tothattimeperiod,FQresistanceincreasedmarkedlyfrom7.7% in1995–1997to22.2% in1998–2000[26].Laiet al.foundthat approximatelytwo-thirdsofofloxacin-resistantM.tuberculosis iso-lateswereMDRand,surprisingly,theratesofFQresistancewere highestamongstadultsaged34–44years[25].Only22.2%of FQ-resistantTBisolates(8/36)weresusceptibletoallfirst-lineanti-TB agents.Theirresultsweresimilartothosereportedbyvanden Boogaard et al., who showed that the rate of FQ-resistant TB waslowinTBpatientsandwasnotrelatedtopreviousbriefFQ exposure[36].Parketal.evaluatedtheimpactofshort-term expo-suretoFQonofloxacin resistanceinhumanimmunodeficiency virus(HIV)-negativepatientswithTBandfoundthattherateof ofloxacin-resistantM.tuberculosiswaslowandthatmostcasesof ofloxacinresistancewereassociatedwithMDR-TB[37].Theyalso foundthatthefrequencyofofloxacin-resistantM.tuberculosiswas lowamongstpatientswhowereexposedtoFQsforashortperiod oftime[37].ThesefindingsfavourtheapplicationofFQsinthe regimenforCAPorTBinpatientswithshorterdiseasedurations.
4. Solutions
InTaiwan,only1–2%ofpatientswithCAPreceiveafinal diag-nosisofTB.ItisimportanttodifferentiatebetweenCAPandTBin theinitialpresentation.Ifthelesionislocatedintheupperlung field,clinicalspecimencollectionorrapidnucleicacid amplifica-tioncouldshortenthedelaytoTBdiagnosisratherthanrestrictthe empiricaltreatmentwithFQsinCAP.Ifthelesionisinthelower lobe,riskfactorsincludingadvancedage,prolongeddurationofthe lesion,lackoffeverandabsenceofairbronchogramsshouldraise thesuspicionofLLFTB.
AlthoughuseofFQsinTaiwanishigh,theincidenceofTB,the mortalityrateassociatedwithTBandtherateofdrugresistance havedecreased.TherateofFQresistanceinS.pneumoniaeislow andtherateofsusceptibilitytoFQsishighamongstH.influenzae,K. pneumoniae(includingESBL-producingstrains),atypicalpathogens andCA-MRSAinTaiwan.
Because of the high incidence of CAP caused by atypical pathogensinTaiwan,coverageofatypicalpneumoniamustbe con-sideredintheempiricaltreatmentofCAPbothinoutpatientsand inpatients.Macrolidesshouldbeusedwithcautionbecauseofhigh ratesofresistancetothatantimicrobialclassinS.pneumoniae.FQs haveagoodsynergisticeffectwithotherantimicrobialagents,with theexceptionof amacrolide combinedwitha-lactam, which mightshowsomeantagonistproperties.
5. Conclusions
Empirical treatment of CAP with a FQ might mask active TB, delay treatment and contribute to the development of FQ
resistance.FQresistanceinM.tuberculosisisrelatedtoFQ dura-tionandthetimingofexposure.ExposuretoaFQ for>10days andexposurefor>60daysbeforeTBdiagnosiswerebothshown tobeassociatedwithasignificantriskofdevelopingFQresistance. Consequently,inTaiwanaswellasinothercountrieswith endemic-ity ofTB, a short-course(5-day) regimenof a FQ(levofloxacin, moxifloxacinandgemifloxacin)isstillrecommendedforempirical therapyforCAPpatientsifthepatientisatlowriskforTB. Further-more,FQresistanceislesslikelytooccuramongstM.tuberculosis strainsisolatedfrompatientswithshort-termexposure(<10days) toFQ.
Funding:Nofundingsources. Competinginterests:Nonedeclared. Ethicalapproval:Notrequired.
References
[1]MandellLA,WunderinkRG,AnzuetoA,BartlettJG,CampbellGD,DeanNC,etal. InfectiousDiseasesSocietyofAmerica/AmericanThoracicSocietyconsensus guidelinesonthemanagementofcommunity-acquiredpneumoniainadults. ClinInfectDis2007;44(Suppl.2):S27–72.
[2] WoodheadM,BlasiF,EwigS,HuchonG,IevenM,OrtqvistA,etal.Guidelines forthemanagementofadultlowerrespiratorytractinfections.EurRespirJ 2005;26:1138–80.
[3]InfectiousDiseasesSocietyofTaiwan;TaiwanSocietyofPulmonaryandCritical Medicine;MedicalFoundationinMemoryofDr.Deh-LinCheng;Foundation ofProfessorWei-ChuanHsiehforInfectiousDiseasesResearchandEducation; CYLee’sResearchFoundationforPediatricInfectiousDiseasesandVaccines. GuidelinesonantimicrobialtherapyofpneumoniainadultsinTaiwan,revised 2006.JMicrobiolImmunolInfect2007;40:279–83.
[4]JeanSS,HsuehPR.AntimicrobialdrugresistanceinTaiwan.JFormosMedAssoc 2011;110:4–13.
[5]WispelweyB,SchaferKR.Fluoroquinolonesinthemanagementof community-acquired pneumonia in primary care. Expert Rev Anti Infect Ther 2010;8:1259–71.
[6]LauderdaleTL,ChangFY,BenRJ,YinHC,NiYH,TsaiJW,etal.Etiologyof com-munityacquiredpneumoniaamongadultpatientsrequiringhospitalizationin Taiwan.RespirMed2005;99:1079–86.
[7] YenMY,HuBS,ChenYS,LeeSS,LinYS,WannSR,etal.Aprospective etio-logicstudyofcommunity-acquiredpneumoniainTaiwan.JFormosMedAssoc 2005;104:724–30.
[8] LinSH,LaiCC,TanCK,LiaoWH,HsuehPR.Outcomesofhospitalizedpatients with bacteraemic and non-bacteraemic community-acquired pneumonia causedbyStreptococcuspneumoniae.EpidemiolInfect2011;139:1307–16. [9]HsiehYC,ChangLY,HuangYC,LinHC,HuangLM,HsuehPR.Circulationof
internationalclonesoflevofloxacinnon-susceptibleStreptococcuspneumoniae inTaiwan.ClinMicrobiolInfect2010;16:973–8.
[10]HsiehYC,LinPY,ChiuCH,HuangYC,ChangKY,LiaoCH,etal.Nationalsurvey ofinvasivepneumococcaldiseasesinTaiwanunderpartialPCV7vaccination in2007:emergenceofserotype19Awithhighinvasivepotential.Vaccine 2009;27:5513–8.
[11]ChungKP,HuangYT,LeeLN,YuCJ,LaiCC,HsuehPR.Alarmingly decreas-ingratesofamoxicillin–clavulanatesusceptibilityamongclinicalisolatesof Haemophilusinfluenzaefrom2001to2009inamedicalcenterinTaiwan.J Infect2011;62:185–7.
[12]WangH,ChenM,XuY,SunH,YangQ,HuY,etal.Antimicrobial suscepti-bilityofbacterialpathogensassociatedwithcommunity-acquiredrespiratory tractinfectionsinAsia:reportfromtheCommunity-AcquiredRespiratoryTract InfectionPathogenSurveillance(CARTIPS)study,2009–2010.IntJAntimicrob Agents2011;38:376–83.
[13]ChenYH,LiuCY,LuJJ,KingCH,HsuehPR.Invitroactivityofnemonoxacin (TG-873870),anovelnon-fluorinatedquinolone,againstclinicalisolatesof Staphylococcusaureus,enterococciandStreptococcuspneumoniaewith var-ious resistancephenotypes inTaiwan.J AntimicrobChemother 2009;64: 1226–9.
[14]vanRensburgDJ,PerngRP,MithaIH,BesterAJ,KasumbaJ,WuRG,etal. Effi-cacyandsafetyofnemonoxacinversuslevofloxacinforcommunity-acquired pneumonia.AntimicrobAgentsChemother2010;54:4098–106.
[15]GriffinAT,PeyraniP,WiemkenT,ArnoldF.Macrolidesversusquinolones in Legionella pneumonia: results from the Community-Acquired Pneu-monia Organization internationalstudy. Int J Tuberc Lung Dis 2010;14: 495–9.
[16]Drago L, Nicola L, Rodighiero V, Larosa M, Mattina R, De Vecchi E. Comparativeevaluationofsynergyofcombinationsof-lactamswith flu-oroquinolones ora macrolide in Streptococcus pneumoniae. J Antimicrob Chemother2011;66:845–9.
[17]HoPL,ChengVC,ChowKH.Decreasingprevalenceoflevofloxacin-resistant StreptococcuspneumoniaeinHongKong,2001to2007.JAntimicrobChemother 2009;63:836–8.
[18] LoHY,ChouP,YangSL,LeeCY,KuoHS.TrendsintuberculosisinTaiwan, 2002–2008.JFormosMedAssoc2011;110:501–10.
[19] Liam CK,Pang YK, Poosparajah S.Pulmonary tuberculosis presenting as community-acquiredpneumonia.Respirology2006;11:786–92.
[20] SinghA.Fluoroquinolonesshouldnotbethefirst-lineantibioticsto treat community-acquiredpneumoniainareasoftuberculosisendemicity.Clin InfectDis2007;45:133.
[21]YuMC,WuMH,JouR,Extensivelydrug-resistanttuberculosis,Taiwan.Emerg InfectDis2008;14:849–50.
[22] LaiCC,LiuWL,TanCK,HuangYC,ChungKP,LeeMR,etal.Differencesindrug resistanceprofilesofMycobacteriumtuberculosisisolatescausingpulmonary andextrapulmonarytuberculosisinamedicalcentreinTaiwan,2000–2010. IntJAntimicrobAgents2011;38:125–9.
[23]LaiCC,TanCK,HuangYT,ChouCH,HungCC,YangPC,etal.Extensively drug-resistantMycobacteriumtuberculosisduringatrendofdecreasingdrug resistancefrom2000through2006atamedicalcenterinTaiwan.ClinInfect Dis2008;47:e57–63.
[24]WangJY,LeeLN,LaiHC,WangSK,JanIS,YuCJ,etal.Fluoroquinolone resis-tanceinMycobacterium tuberculosisisolates:associatedgenetic mutations andrelationshiptoantimicrobialexposure.JAntimicrobChemother2007;59: 860–5.
[25]LaiCC,TanCK,HuangYT,LiaoCH,HsuehPR.Fluoroquinolone-resistant tuber-culosisatamedical centreinTaiwan,2005–10.JAntimicrobChemother 2011;66:2437–8.
[26] HuangTS, Kunin CM,Shin-Jung Lee S,Chen YS, TuHZ, Liu YC. Trends influoroquinoloneresistanceof Mycobacteriumtuberculosiscomplex ina Taiwanesemedical centre:1995–2003.J AntimicrobChemother2005;56: 1058–62.
[27] DooleyKE,GolubJ,GoesFS,MerzWG,SterlingTR.Empirictreatmentof community-acquiredpneumoniawithfluoroquinolones,anddelaysinthe treatmentoftuberculosis.ClinInfectDis2002;34:1607–12.
[28]ChenTC,LuPL,LinCY,LinWR,ChenYH.Fluoroquinolonesareassociated withdelayedtreatmentandresistanceintuberculosis:asystematicreview andmeta-analysis.IntJInfectDis2011;15:e211–6.
[29]YoonYS,LeeHJ,YoonHI,YooCG,KimYW,HanSK,etal.Impactof fluo-roquinolonesonthediagnosisofpulmonarytuberculosisinitiallytreatedas bacterialpneumonia.IntJTubercLungDis2005;9:1215–9.
[30] WangJY,HsuehPR,JanIS,LeeLN,LiawYS,YangPC,etal.Empiricaltreatment withafluoroquinolonedelaysthetreatmentfortuberculosisandisassociated withapoorprognosisinendemicareas.Thorax2006;61:903–8.
[31] GolubJE,BurS,CroninWA,GangeS,SterlingTR,OdenB,etal.Impactofempiric antibioticsandchestradiographondelaysinthediagnosisoftuberculosis.Int JTubercLungDis2005;9:392–7.
[32]Mathur P, Sacks L, Auten G, Sall R, Levy C, Gordin F. Delayed diagno-sisofpulmonarytuberculosisincityhospitals.ArchInternMed1994;154: 306–10.
[33]ChangSC,LeePY,PerngRP.Thevalueofroentgenographicandfiber bron-choscopicfindingsinpredictingoutcomeofadults withlower lungfield tuberculosis.ArchInternMed1991;151:1581–3.
[34]WangJY,LeeLN,HsuehPR.Factorschangingthemanifestationofpulmonary tuberculosis.IntJTubercLungDis2005;9:777–83.
[35]Lin CH, Chen TM, Chang CC, Tsai CH, Chai WH, Wen JH. Unilateral lowerlungfieldopacitiesonchestradiography:acomparisonofthe clin-ical manifestations of tuberculosis and pneumonia. Eur J Radiol 2011, doi:10.1016/j.ejrad.2011.03.028[Epubaheadofprint].
[36] vandenBoogaardJ,SemvuaHH,vanIngenJ,MwaigwisyaS,vanderLaan T,vanSoolingenD,etal.Lowrateoffluoroquinoloneresistancein Mycobac-teriumtuberculosisisolatesfromnorthernTanzania.JAntimicrobChemother 2011;66:1810–4.
[37]ParkIN,HongSB,OhYM,LimCM,LeeSD,LewWJ,etal.Impactofshort-term exposuretofluoroquinolonesonofloxacinresistanceinHIV-negativepatients withtuberculosis.IntJTubercLungDis2007;11:319–24.

![Fig. 5. Clinical and laboratory predictors of patients with tuberculosis who were initially diagnosed as having community-acquired pneumonia [19]](https://thumb-ap.123doks.com/thumbv2/9libinfo/8947081.272721/4.918.56.429.885.1097/clinical-laboratory-predictors-tuberculosis-initially-diagnosed-community-pneumonia.webp)