bs_bs_banner
Nephrology19 (2014)699–707
Original
Article
Multidisciplinary
care
improves
clinical
outcome
and
reduces
medical
costs
for
pre-end-stage
renal
disease
in
Taiwan
YUE-REN
CHEN,
1YU
YANG,
2SHU-CHUAN
WANG,
1WEN-YU
CHOU,
1PING-FANG
CHIU,
1CHING-YUANG
LIN,
3,4WEN-CHEN
TSAI,
5JER-MING
CHANG,
6,7TZEN-WEN
CHEN,
8SHYANG-HWA
FERNG
9and
CHUN-LIANG
LIN
101DivisionofNephrology,InternalMedicine,ChanghuaChristianHospital,ChanghuaCity,2SchoolofMedicine,ChungSangMedicalUniversity,3Collegeof
Medicine,5DepartmentofHealthServicesAdministration,ChinaMedicalUniversity,4DivisionofPediatricNephrologyandClinicalImmunologyCenter,China
MedicalUniversityHospital,TaichungCity,6DepartmentofInternalMedicine,KaohsiungMunicipalHsiao-KangHospital,7DivisionofNephrology,Kaohsiung
MedicalUniversityHospital,Kaohsiung,8DivisionofNephrology,InternalMedicine,TaipeiMedicalUniversityHospital,9DivisionofNephrology,Internal
Medicine,CathayGeneralHospital,TaipeiCity,and10DivisionofNephrology,InternalMedicine,ChiayiChangGungMemorialHospital,Chiayi,Taiwan
KEYWORDS:
chronickidneydisease,hospitalization,medical
costs,mortality,multidisciplinarycare.
Correspondence:
DrYuYang,DivisionofNephrology,Internal
Medicine,ChanghuaChristianHospital,Chung
SangMedicalUniversity,SchoolofMedicine,
135NanhsiaoStreet,ChanghuaCity,500
Taiwan.Email:2219@cch.org.tw
Acceptedforpublication9July2014.
Acceptedmanuscriptonline27July2014.
doi:10.1111/nep.12316
Disclosure: Theauthors have no conflicts o
f
interesttodisclose.
SUMMARY ATAGLANCE
Thisretrospectivestudyclearly
demonstratesthatmultidisciplinarycareby
nephrologistsindialysispatientsprovided
bettervariousoutcomesandlessmedical
costs.However,thepatientmortalitywas
notdifferent.
ABSTRACT:
Aim: Multidisciplinarycare(MDC)forpatientswithchronickidneydisease (CKD) mayhelp tooptimize disease care and improve clinical outcomes. Ourstudyaimedtoevaluatetheeffectivenessofpre-end-stagerenaldisease (ESRD)patientsunderMDCandusualcareinTaiwan.
Method: Inthis 3-yearretrospectiveobservational study,we recruited822 ESRDsubjects,aged18yearsandolder,initiatingmaintenancedialysismore than3monthsfromfivecooperatinghospitals.TheMDC(n=391)groupwas caredforbyanephrologists-basedteamandtheusualcaregroup(n=431) wascared forby sub-specialists or nephrologists alonemorethan 90 days beforedialysisinitiation.Patientcharacteristics,dialysismodality,hospital utilization,hospitalizationatdialysisinitiation,mortalityandmedicalcost wereevaluated.Medicalcostswerefurtherdividedintoin-hospital, emer-gencyservicesandoutpatientvisits.
Results: TheMDCgrouphadabetterprevalenceinperitonealdialysis(PD) selection,lesstemporarycatheteruse,alowerhospitalizationrateatdialysis initiationand 15%reductionin therisk of hospitalization(P0.05). After adjustingforgender,ageandCharlsonComorbidityIndexscore,therewere lowerin-hospital and higheroutpatient costsin the MDC group during 3 monthsbefore dialysisinitiation(P0.05).Incontrast,medicalcosts(NT$ 146038 vs 79022) and hospitalization days (22.4 vs 15.5 days) at dialysis initiation were higher in the usual care group. Estimated medical costs during 3 months before dialysis till dialysis initiation, the MDC group yieldedareductionofNT$59251foreachpatient(P0.001).Patient mor-talitywasnotsignificantlydifferent.
Conclusion: Multidisciplinarycareinterventionforpre-ESRDpatientscould not only significantly improve the quality of disease care and clinical outcome,butalsoreducemedicalcosts.
The rapid increased incidence and prevalence of chronic kidney diseases (CKD) have been recognized as a global publichealth problemthat consumesa largeproportionof health carebudgets.In Taiwan, thenationalprevalence of CKDishigh,butdiseaseawarenessisinadequate.Only3.5 %
ofCKDpatientsareabletoreporttheirstageofdisease,and awarenessratesarecloselyrelatedtodiseaseseverity.1,2A s
oneofthe mostrapidlyaging countrieswith anincreasing prevalence of diabetes mellitus, hypertension and
subse-quentlyCKD, Taiwan hasthe highest prevalenceand inci-dence of end-stage renal disease (ESRD) in the world.3 According to the Bureau of National Health Insurance (BNHI)annualreport,thedialysiscostsofESRDpatientsin Taiwan accounted for 5.0–7.52% of the total health-care resourcesinrecentyears.4
Medicalresourceutilizationhasbecomemorefrequentas disease progression and ESRD approach. According to a
recent study, the medical cost of pre-ESRD patients
©2014TheAuthors.NephrologypublishedbyWileyPublishingAsiaPtyLtdonbehalfofAsianPacificSocietyofNephrology.
ThisisanopenaccessarticleunderthetermsoftheCreativeCommonsAttribution-NonCommercial-NoDerivsLicense,whichpermitsuseanddistributioninany medium,
providedtheoriginalworkisproperlycited,theuseisnon-commercialandnomodificationsoradaptationsaremade.
Y-RChenetal.
increased sharplyinthe last6monthsprior todialysis ini-tiation.5 Service utilization and hospitalizations were the major components of cost during the period immediately before and after dialysis initiation.6 Co-morbidity, such as cardiovascular disease, is the major cause of mortalit y
among CKD patients, and CKD patients with increasing co-morbiditymayberesponsible fortherapidescalationof medicalexpenditures.7,8
Optimal management of CKD may improve clinical
outcome and decrease mortality, thus resultingin reduced hospitalization and medicalcost. In 2002,the US National KidneyFoundationlaunchedthepromotionofclinical prac-ticeguidelinesforthediagnosis,evaluationandmonitoring ofCKDwithintheKidneyDiseaseOutcomesQuality Initia-tive(NKFK/DOQI)inanefforttoincreasetheawarenessof optimal CKD care.9 Recent trials and studies also have proven the efficacy of several interventions such as earl y
detection of CKD,10 prevention of kidney disease pro-gression, early referral to nephrologists,11 promotion of pre-dialysiseducations,12timelypreparationofrenal
replace-ment therapy (RRT), and care by a comprehensive,
nephrology-based,multi-disciplinaryteam.13–15
Thepurposeof ourstudyistoevaluatethe effectiveness andassociationofclinicaloutcome,impactofdialysis
modal-ityselection,medicalutilizationandcostsbetweenpre-ESRD patientsreceivingMDCandusualcareinTaiwan.
MATERIALS
AND
METHODS
Study design and subjects
Ourretrospectivestudy wasdirectlylinkedto theNationalHealth
Insurance(NHI)systemwithitsoutpatientandin-hospitaldatabase
intheperiodfromJanuary2005toDecember2009.Patientsaged18
yearsorolderwhowereonmaintenancerenalreplacementtherapy
(includinghaemodialysisandPD)andwhohadcatastrophicillness
cardshadtheirmedicalexpensecoveredbytheNHIandwerecared
forinfivecooperatinghospitalsinthenorthern,centraland
south-ernareas ofTaiwan.Initially,854 subjectswereenrolled, butwe
excluded patients who received temporary dialysis due to acute
deterioration ofrenalfunction,andthosewho diedinthefirst3
months after dialysis initiation. In the end, 822 subjects were
recruitedandfurtheranalyzed.
Atotalof391subjectswereplacedintotheMDCgroupwhohad
receivednephrologists-basedCKDteamcareformorethan90days
beforedialysisinitiation.Theother431subjects,whowereunder
theintervention of sub-specialistsalone suchasendocrinologists,
cardiologistsandnephrologistswithoutreferringtotheMDC,were
definedastheusualcaregroup(Fig.1).
Fig.1 Participantflowchart.
700
©2014TheAuthors.NephrologypublishedbyWileyPublishingAsiaPtyLtdonbehalfofAsianPacificSocietyofNephrolog y
patient management
Themultidisciplinarycare(MDC)consistedofanephrologist,
neph-rologynurseeducator,renaldietician,socialworker,pharmacy
spe-cialists,andsurgeonforvascularaccesscreation,tenchoffcathete
r
implantation.ForthestandardizedinterventionofCKDintheMDC
group,themanagementandeducationwasdependentonthe
dif-ferent stage of CKD and followed the NKF K/DOQI guidelines,
Taiwanpre-ESRD care programand reimbursementpolicy ofthe
NHI.CKDmanagementintheMDCgroupfocusedbothonmedical
management and lifestyle modification. The
case-management
nephrologynursecontactedpatientstoensureregularfollow-ups.
The members of the MDC team met with and followed up on
patients regularly to review and discuss patients’ individualized
therapy,medicalrecommendationsformetabolicabnormality,diet
assessmentandco-morbidity.
Criteria for dialysis initiation
CriteriafordialysisinitiationweremandatedbytheBNHIinTaiwan
including:
1Absolute criteria ofserum creatinine levels above10mg/dL or
creatinineclearanceoflessthan5mL/min.
2Relative criteria of serum creatinine levels above 6mg/dL or
creatinineclearanceoflessthan15mL/min,anduremicconditions
whichthreatenlifeorimpairqualityoflife(notlistedindetail).
Data collection and initial dialysis modality definition
Patients’basiccharacteristicswereprovidedbythefivecooperating
hospitals.WedirectlylinkedtotheNHIsystemandclaimdatato
confirm 1st dialysis medicalrecords and admission data to avoi
d
incorrectdatacollection.IfpatientshadeverexperiencedPDduring
thefirst3monthsafterdialysis initiation,initialdialysismodalit
y
wasdefinedasPD.
Definitionof comorbidity diseases
Based on the definition of Dartmouth-Manitoba’s Charlson
ComorbidityIndex(D-M’sCCI),16weusedtheInternational
Classi-fication ofDiseases (ICD-9)code on thein-hospitaldatabase and
double records in outpatient database to identify co-morbidities
withinoneyearbeforedialysisinitiation.Subsequently,anyinstanc
e
ofICD-9codeoncepresentedintheNHIdatabasewascountedas
co-morbidityandweightedintheCCIscore.
Service utilizations and medical costs,
clinical outcome
Service utilization and patients’ mortality were our clinical
outcomes.Datawerefollowedupuntil31December2009.Medical
serviceutilizationandcosts wereanalyzed from3monthsbefore
dialysisuntil6monthsafterdialysisinitiation(definedasthe
obser-vationperiod).Accidentinjuriesorsurgicalconditionsnotrelatedto
CKDwereexcluded.Medicalcostswerefurtheranalyzedinto
out-patientvisits,in-hospital,andemergencyservices.Serviceutilizatio
n
included frequency ofoutpatient visitsandhospitalization before
MDCimprovesoutcomesandreducescosts
andafterdialysisinitiation,percentageofhospitalizationatdialysis
initiation,andaveragelengthofstay(LOS).Serviceutilizationand
medicalcostduringobservationperiodwerefurtherdividedinto‘3
monthsbeforedialysis’,‘atdialysisinitiation’and‘6monthsafter
dialysisinitiation’.‘Atdialysisinitiation’wasdefinedastheperiodof
first time dialysis prescription (through hospitalization or
outpa-tient). Dialysis costs were excluded in our study (there was no
comparisonofcostofPDvshaemodialysis).
Statistical analysis
Frequency(n) and percentage (%) were used to determine the
distributionof gender,dialysis modality selection, andtemporary
catheteruse,hospitalizationatdialysisinitiation,frequencyof
hos-pitalization,co-morbidityandmortality.Meanandstandard
devia-tion(SD)wereusedtodescribethedistributionofage,hospitaldays,
andmedicalcostson outpatientvisits,in-hospitaland emergency
services.Wealsousedmediantodescribethedistributionofmedical
costs.Thedifferencesincategoricalvariableswereanalyzedby2test
(orFisher’sexacttest).Ageneralizedlinearmodel(GLM)wasused
toevaluatemedicalcostsbetweentheMDCand usualcaregroup
afteradjustingforgender,ageandCCIscore.TheTobitregression
modelwasusedto estimatetheadjusted medicalcosts associated
with the MDC and usual care group after controlling for other
covariates.TheKaplan–Meiersurvivalcurveandlog-rankstatistics
wereused todescribe hospitalization riskandpatientsurvival. A
multivariateCoxregressionmodelwasperformedtopredict
hospi-talizationriskandpatientmortalityafteradjustingforgender,age
andCCIscore.Atwo-tailedP-valuelessthan0.05wasconsidered
statisticallysignificant.Allstatisticalanalyseswereconductedusing
thestatisticalpackageforWindow,SAS9.2(SASInstitute,Cary,NC,
USA)andSPSS16.0(SPSS,Chicago,IL,USA).
RESULTS
Patient characteristics and co-morbidity
In total,822 subjects (usual care, n431; MDC, n391) withmeanageof62.8years(male,51.5%)wereincludedin ourstudy.Patient’scharacteristics,dialysismodality, percent-ageofhospitalizationatdialysisinitiationandco-morbidity areshowninTable1.TheMDCgrouphadahigher percent-ageofPDmodalityselection,lowertemporarycatheteruse, and a lower hospitalization rate at dialysis initiation (P0.05). The CCI scorein the MDCgroup was loweras comparedtotheusualcaregroup(P0.02).
Decline of renal function and eGFR at
dialysis initiation
Table2furtherillustratesthebaselineestimatedglomerular filtrationrate (eGFR) oneyear beforedialysis initiation,at dialysisinitiation,andthedeclineofrenalfunctionbasedon thevalidsubjectsprovidedbyfivecooperatinghospitals.We foundthepatientsoftheMDCgrouphadmorecompliance to outpatients follow-up and more detail laboratory data record(datanotshown).Thedeclineofrenalfunctionwas
©2014TheAuthors.NephrologypublishedbyWileyPublishingAsiaPtyLtdonbehalfofAsianPacificSocietyofNephrology 701
Y-RChenetal.
Table1 Generalcharacteristicofoursubjects DC
Us
ualcare
(n=391) (n=431)
P
P0.001)(Table3).The MDCgrouphada shorterLOSof hospitalization forboth ‘at dialysis initiation’ (15.5days vs 22.4days,P0.001)and‘6monthsafterdialysisinitiation’ (11.2daysvs16.0days,P0.05)(Table3).
Gender,male 210 53.7 213 49.4 0.22
Dialysischoice,PD† 120 30.7 67 15.6 0.001
Temporarycatheteruse 222 56.8 328 76.1 0.001
Initialdialysisadmission 0.05
In-hospital 327 83.6 369 85.6 Outpatient 42 10.7 28 6.5 Emergency 22 5.6 34 7.9 Hospitalizationrate‡ 347 88.7 402 93.3 0.03 CCIscore§ (2.01.6) (2.21.8) 0.02 Age (63.013.9) (62.615.5) 0.72
†Ifpatientshadtheexperienceoftheperitonealdialysis(PD)modelfro
m
dialysisinitiationtoaftera3monthsperiod,itwascalculated.‡Ifpatientsw ere
transferredfromoutpatientservicesoremergencyservicestohospitalizatio
n
atdialysisinitiation,itwascalculated.§Comorbiditydiseaseswerebasedo
n
Dartmouth-Manitoba’sCCI(D-M’sCCI).Valuesareexpressedas(meanSD).
CCI,CharlsonComorbidityindex;GFR,glomerularfiltrationrate;SD,standa
rd deviation.
slowerintheMDCgroup(7.6vs11.1mL/minper1.73m2, P0.001),alsoeGFR atthedialysis initiationwas lowera s
compared to the usual care group (5.1 vs5.9mL/min per 1.73m2,P
0.001).
Hospitalization risk and patient mortality
Duringanaveragefollow-uptimeof33.6months,atotalof 104 (24.1%) patients in the usual care and 67 (17.1% )
patients in theMDC groupdied (P0.01).The usualcare grouphadahigherhospitalizationrateduringthe observa-tionperiods(usualcare75.4%vsMDC69.3%,P0.05),an d
even6monthsafterdialysisinitiation(usualcare58.7%v s
MDC50.6%, P0.02).TheMDCgroup hadbetterpatient survival and lower risks of hospitalization in the Kaplan– Meier analysis (log-rank test, P0.05) (Figs2,3). After adjustingforgender,ageandCCI,theMDCgroupwasstill associatedwitha15%reductionintheriskofhospitalization (hazard ration [HR], 0.85; 95% confidence interval [CI] ,
0.72–0.99,P0.05).However,therewasnosignificant
dif-ference in patient mortality between the two groups (HR, 0.79;95%CI,0.58–1.08,P0.14).
Medical costs and frequencyof service utiliza
tion
The average medicalcostfor‘3months beforedialysis ini-tiation’, ‘at dialysis initiation’ and ‘6 months after dialysis initiation’wereNT$43329,NT$114161andNT$224624, respectively(datanotshown).ThemeanLOSof‘atdialysis
initiation’and‘6monthsafter dialysisinitiation’were19.1 daysand13.7days,respectively(datanotshown).
Medicalcostfortheusualcaregroup‘atdialysisinitiatio n’
was significantly higher (NT$ 146038 vs NT$ 7902 2 NT,
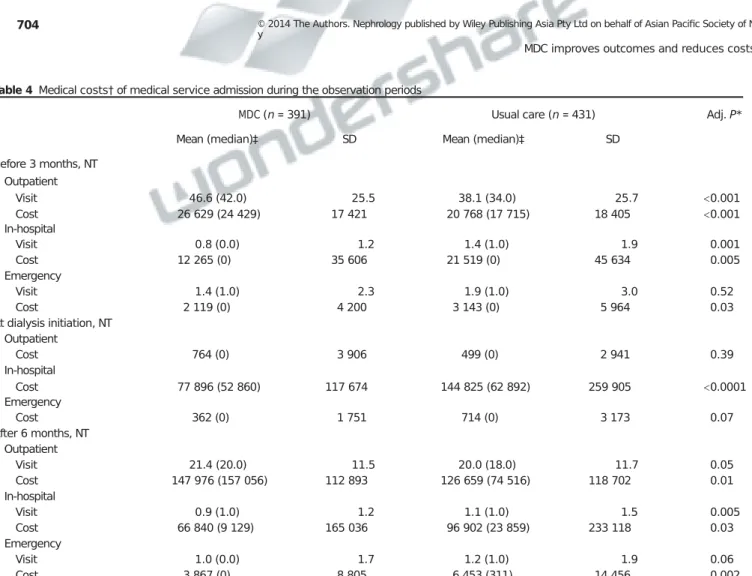
3 months before dialysis initiation
There was a higher frequency of outpatient visits (46.6 vs 38.1, P0.001) and higher average medical costs in the
MDC group (NT$ 26629 vs NT$ 20768, P0.001);
however,frequencyofhospitalization(0.8vs1.4,P0.001) andin-hospital(NT$12265vsNT$21519,P0.01), emer-gencycosts(NT$2119vsNT$3143,P0.05)werelowerin theMDCgroup(Table4).
At dialysisinitiation
Medicalcostsatdialysisinitiationweremainlyattributedto in-hospitalcosts.TheMDCgroupincurredlowerin-hospital costs after adjusting for gender, age and CCI score (NT$ 77896vsNT$144825,P0.05)(Table4).However,there
was no difference on outpatient and emergency costs
betweenthetwogroups.
6 months after dialysis initiation
Outpatient visits (21.4 vs 20.0, P0.05) and costs (NT$ 147976dollarsvsNT$126659,P0.01)werehigherinthe MDCgroup,whereasfrequencyofhospitalization(0.9vs1.1, P0.005) and in-hospital (NT$ 66840 vs NT$ 96902, P0.03) and emergency costs (NT$ 3867 vs NT$ 6453,
P0.002) were lower in the MDC group (Table4 and Fig.4).
Medical costs by Tobit regression
Age,CCIscore,temporarycatheteruseandhospitalizationat dialysisinitiationhadsignificantlypositiveeffectsonmedical costs (Table5). Adjusted medical costs were significantly lowerintheMDCgroupandwerereduceduptoNT$59251 foreachpatientduring3monthsbeforedialysisuntildialysis initiation(P0.001).
DISCUSSION
Severalstudieshaveevaluatedtheeffectivenessof compre-hensive, nephrology-based, multi-disciplinary care (MDC) andhave affirmed their substantialbenefits,such as bette r
laboratory parameters and clinical outcomes, slower renal functiondeclines,morefunctionalvascularaccessandshorte r
LOSatdialysisinitiation,andreductioninmedicalcostsand serviceutilization.13–15,17However,onlyfewstudieshave sim-ultaneouslyfocusedonmedicalserviceutilization,costand clinicaloutcomesfortheMDConpre-ESRDpatients.17From ourlarge-scale population and multi-hospital collaborative
702 ©2014TheAuthors.NephrologypublishedbyWileyPublishingAsiaPtyLtdonbehalfofAsianPacificSocietyofNephrolog y
MDCimprovesoutcomesandreducescosts
Table2 Baselineestimatedglomerularfiltrationrate(eGFR)(mL/minper1.73m2)andeGFRchange(eGFR)betweenmultidisciplinarycare(MDC)andusual care
group
MDC(n=391) Usualcare(n=431) P AdjustedP
# MeanSD
n
# MeanSD
BaselineeGFR1yearbeforedialysis 315 12.17.0 218 17.011.7 0.001 0.001
eGFRatdialysisinitiation 315 5.10.7 218 5.90.7 0.001 0.001
eGFR 315 7.06.3 218 11.111.0 0.001 0.001
eGFR/month 315 0.60.6 218 1.11.4 0.001 0.001
eGFR(estimatedglomerularfiltrationrate)asbaselineeGFR1yearbeforedialysis–eGFRatdialysisinitiation.AdjustPforgender,ageandCCIscore;e
GFR
providedbyfivecooperatinghospitalsbasedonvalidsubjects(somesubjectslosttofollow-upandinitiationrenalreplacementtherapy[RRT]outsidethe
study hospitals).
Fig.2 Kaplan–Meiercurveoftimetofirsthospitalizationbetweenmultidisciplinarycare(MDC)andusualcaregroupinthefollow-upperiod.
studythatwasdirectlylinkedtotheNHIsystemanddatabas e
in Taiwan,we confirmed the effectivenessof theMDC for pre-ESRDpatientsnotonlyforimprovingclinicaloutcomes, butalsoforreducingmedicalcosts.
Declines of renalfunction and characteristic
at
dialysis initiation
ConsensusguidelinesforCKDmanagement emphasizethe administrationofnephroprotectiveagents(RAASblockade), reductionofcardiovascularrisk,screeningandintervention forCKD-MBDandanaemia.Unfortunately,somephysicians may be reluctant to prescribe renoprotective medications such as RAAS blockage due to hyperkalaemia or haemo-dynamicmediatedincreaseinserumcreatininelevel.MDC
membranes could help and support additional effort to conductmedicationssideeffectsfollow-up.Dueto combina-tion of lifestyle modifications and more effective medical prescriptionaccordingtoK/DOQIandconsensusguidelines, theneGFRdeclinesintheMDCgroupwasslowerthanthe usual care group. Also in our study, there was no earlier initiationof dialysistherapy andCKDpatientsin theMDC groupinTaiwanweremorelikelytoinitiate dialysisrather thanfacemortality.18,19
Previous researchhas shownthat areduction in tempo-rary catheter useis associated with a lowerinfection rate, avoidanceof emergencydialysis, lower riskof hospitaliza-tion,andadecreaseinmortality,whichresultsinareduction of medical cost.20,21 Also the timing of referral and pre-dialysiseducationhasbeenshowntoinfluencetheselection
©2014TheAuthors.NephrologypublishedbyWileyPublishingAsiaPtyLtdonbehalfofAsianPacificSocietyofNephrology 703
Y-RChenetal.
Fig.3 Kaplan–Meiercurveofpatientsurvivalbetweenmultidisciplinarycare(MDC)andusualcaregroupinfollow-upperiod.
Table3 Medicalcosts†andhospitalutilizationinoursubjects
MDC(n=391) Usualcare(n=431) P
Mean(median)‡ SD Mean(median)‡ SD
Medicalcosts,NT
Atdialysisinitiation 79022(53302) 117118 146038(63327) 259431 0.001
After6months 218684(197092) 185792 230014(195463) 243206 0.46
Hospitaldays
Atdialysisinitiation 15.5 12.9 22.4 24.2 0.001
After6months 11.2 21.8 16.0 31.2 0.01
†Excludingdialysiscost;before3monthsandafter6months,costswerebasedontotalsubjects,whileatdialysisinitiation,theywerebasedonthenu
mberof
validsubjects.‡Medianwascalculatedbasedonthenumberofallthesubjects.MDC,multidisciplinarycare;SD,standarddeviation.
of dialysis modality and compliance to therapy prescrip-tion.22,23InTaiwan,theproportionofdialysispatients under-going PD increased from 6.1 to 7.8% between 2001 and 2005, butthe proportionoptingforPD remainslow. MDC may helpCKD patients to receivewell-balanced presenta-tions ofallrenal replacementtherapyoptions.Educational intervention could increase in patient self-care ability and the provision of adequateandgood qualityinformationof dialysis,makingpatientswillingtoundergoPDandself-care dialysis.Ourstudydemonstratedthesameresultsasprevi
-ousstudiesinsofarastheMDCgrouphadlowertemporary catheter use(56.8% vs76.1%, P0.001), a lower rate of
emergencyvisitatdialysisinitiation(5.6%vs7.9%,P0.0 5)
anddoubletheoddsofselectingthePDmodality(30.7%vs 15.6%,P0.001).
Service utilizations and medical costs
Studieshaveindicatedthatresourceutilizationhasbecome morefrequentasESRDapproaches.6,24–26Asubstantial pro-portionofthesharpincreaseinhospitalizationratesinthe3 monthsbeforeandaftertheinitiationofdialysiswas attrib-utedtovascularaccess andrelatedcomplications.25Several otherfactorsalsoconfirmedtheincreasedriskof hospitali-zation, such as later referral, temporary catheter use, advancedage,loweralbuminandhematocritlevels,andan
704 ©2014TheAuthors.NephrologypublishedbyWileyPublishingAsiaPtyLtdonbehalfofAsianPacificSocietyofNephrolog y
MDCimprovesoutcomesandreducescosts
Table4 Medicalcosts†ofmedicalserviceadmissionduringtheobservationperiods
MDC(n=391) Usualcare(n=431) Adj.P*
Mean(median)‡ SD Mean(median)‡ SD
Before3months,NT Outpatient Visit 46.6(42.0) 25.5 38.1(34.0) 25.7 0.001 Cost 26629(24429) 17421 20768(17715) 18405 0.001 In-hospital Visit 0.8(0.0) 1.2 1.4(1.0) 1.9 0.001 Cost 12265(0) 35606 21519(0) 45634 0.005 Emergency Visit 1.4(1.0) 2.3 1.9(1.0) 3.0 0.52 Cost 2119(0) 4200 3143(0) 5964 0.03 Atdialysisinitiation,NT Outpatient Cost 764(0) 3906 499(0) 2941 0.39 In-hospital Cost 77896(52860) 117674 144825(62892) 259905 0.0001 Emergency Cost 362(0) 1751 714(0) 3173 0.07 After6months,NT Outpatient Visit 21.4(20.0) 11.5 20.0(18.0) 11.7 0.05 Cost 147976(157056) 112893 126659(74516) 118702 0.01 In-hospital Visit 0.9(1.0) 1.2 1.1(1.0) 1.5 0.005 Cost 66840(9129) 165036 96902(23859) 233118 0.03 Emergency Visit 1.0(0.0) 1.7 1.2(1.0) 1.9 0.06 Cost 3867(0) 8805 6453(311) 14456 0.002
*Adjustingforgender,ageandCharlsonComorbidityIndex(CCI)score.†Excludingdialysiscost;before3monthsandafter6months,costswerebasedontot
al
subjects,whileatdialysisinitiation,theywerebasedonthenumberofvalidsubjects.‡Medianwascalculatedbasedonthenumberofallthesubjects.SD,sta
ndard deviation.
increased number of co-morbidity.5,25,27,28 The MDC group couldfacilitatetheearlycreationoffunctionaldialysisacces s
intheoutpatientsetting,whichobviatedtherequirementof temporarycatheter useanddecreased associated complica-tions, thus decreasing medical service utilization and expenditure.
Inourretrospectivecohortstudyfrom2005to2009based ontheNHIdatabase,wefoundthattheMDCgroupdidhave a significantly lower risk of hospitalization and LOS. The majormedicalcostswerein-hospitalcostsatdialysis initia-tion,and therewasa50% reduction ofmedicalcostsafter theMDCintervention(NT$ 77896 vsNT$144825). Also, CCI score, temporary catheter use and hospitalization at dialysis initiation are major independent risk factors for medicalexpenditure.AftertheTobitmodelanalysis adjust-ment,the estimatedmedicalcostsreduction foreachMDC patientduring3monthsbeforeuntildialysisinitiationcould beuptoNT$59251.Inlight ofthe 8000incidentdialysis patients who allreceived carefromthe MDC in2009, we couldestimatethatsavedmedicalexpenditurecanreach47 5
millionNTdollarseachyear,whichaccountsfor1.4‰ofthe 400billionNT-dollarfiscalbudgetsfortheNHI.29
Clinical outcome
Nephrology care6months before dialysis and the consist-encyofcarearestrongpredictorsofmortality.30,31MDCcould provide pre-ESRD patients with enhanced disease knowl-edgeandawareness,amorepositiveattitude,betterlifestyle modificationswithcardiovascularriskreduction,and more effectivemedicalprescriptionaccordingtoK/DOQIand con-sensusguidelines;allofthesemaycontributetoadecreasein all-causesmortality.
As expected, our finding confirmed the effectiveness of MDCindecreasingtheriskofhospitalization,butindicated no significantly better survival benefits. We speculatethat ESRDpatientswhodiedwithin90daysafterdialysis initia-tionwereexcludedfromourstudy. Also duetothe acces-sibility of dialysis therapy in Taiwan, pre-ESRD patients underMDCinterventionaremostlikelytoinitiatethe dialy-siselectivelyandexperienceoptimaldialysistherapybefore reachingmortality.
Therearestillsomelimitationsinourstudy.First,dueto our study design, we could not provide detailed cause of hospitalizationandmortality(garbleddata providedbythe
©2014TheAuthors.NephrologypublishedbyWileyPublishingAsiaPtyLtdonbehalfofAsianPacificSocietyofNephrology 705
Y-RChenetal.
Fig.4 Medicalcosts(excludingdialysiscosts)ofmultidisciplinarycare(MDC)andusualcaregroupinobservationperiods.Before3monthsandafter6
months
werebasedonthetotalnumberofsubjects.Atdialysisinitiation,costswerebasedonthenumberofvalidsubjects(adjustingforgender,ageandCCIsco
re).
outpatient;
,in-hospital;■,emergency.
Table5 Tobitmodelanalysisonadjustedmedicalcosts†:before3monthstoinitialdialysisperiods
Total(n=822) MDC(n=391) Usualcare(n=431)
95%CI P 95%CI P 95%CI P
Low high Low High Low High
Intercept −81501 −177274 −4273 0.10 −53235 −125152 18682 0.15 −177367 −351407 −3327 0.05
MDCversusnon-MDC −59251 −91477 −27025 0.001 — — — — — — — —
Maleversusfemale 1299 −30303 32902 0.94 −2198 −27510 23114 0.86 5457 −49868 60783 0.85
CCIscore 28798 19255 38342
0.001 18799 10892 26706 0.001 36011 19743 52279 0.001
Temporarycatheteruse‡ 64479 28752
100206
0.001 65664 39294 92035 0.001 67096 −1453 135646 0.06
Hospitalizationrate‡ 76068 17858
134278 0.01 45657 4428 86885 0.03 124185 7024
241347 0.04
Scale 229560 218727
240929 125821 117304
134956 291996 273139
312154
†Excludingdialysiscost.‡Eventswereatdialysisinitiation.CCI,CharlsonComorbidityIndex;MDC,multidisciplinarycare.
NHI). Also this was a retrospective observational study of secondary data analysis, so we could not provide detailed biochemistry differences between the two groups. These limited items used as clinical parameters and incomplete informationduetoprimarydataerrorswereneitheravoided noroverlooked.Second,weonlyanalyzedmedicalcosts,and assuch,couldnotevaluatedifferencesinpatients’qualityof life,societyresourceutilizationandexpenditure.Third,the fixedreimbursementpolicyoftheNHIrestrainedlaboratory parameter measurement and medical utilization (such a s
haemoglobin correction by the ESA administration). Furthermore, theNHI systemin Taiwanis auniquehealth insurancecoveragesystem,andourresultsmaynotapplyt o
othercountriesthatconductsimilaranalyses.TheBureauof
Health Promotionin Taiwan has launched pre-ESRD care initiativessince2002.TheMDCprograminTaiwanproposed astandardcareprotocolandannualreportingsystem.Since 2008theTaiwanSocietyofNephrologycommitteealso con-ducted a surveillance program and improvement of the qualityofpre-ESRDcare.ThepropagationoftheMDCmight partially explain the stabilization of increase in incident ESRDpatientsinTaiwan.
CONCLUSION
Pre-ESRDpatients underthe MDCintervention,especially forthoseat3monthspriortoinitiatingdialysis,hadahigher percentage of functional vascular access and better
preva-706 ©2014TheAuthors.NephrologypublishedbyWileyPublishingAsiaPtyLtdonbehalfofAsianPacificSocietyofNephrolog y
lenceinPDselection.Moreover,bothLOSatdialysis initia-tionaswellastheriskofhospitalizationwasreduced.Finally ,
ourstudyconfirmed the effectivenessof MDCnot onlyin improving clinical outcome but also in reducing medical expenditure.
ACKNOWLEDGEMENTS
Thisstudywassupportedbythe Bureau ofHealth Promo-tion, Department of Health, R.O.C. (97-HP-1103, 98-HP-1112,99-HP-1108,100-HP-1104).YuYangwasresponsible for the study conception and execution. Chiou, Chang, Chen,LinandFerngwereresponsibleforplancoordination andcooperation.Wangwasresponsiblefordataanalysisand the drafting of the manuscript. Chou assisted with imple-menting the study and data collection. We thank the cooperationofthehospitalCKDnurses,e.g.Jui-HsinChen, Shu-ChiLu,Jay-JenLin,Ya-HsuehShih,Chih-YingHuang inthecollectionofthesubjects’data.
REFERENCES
1.WenCP,ChengTYD,TsaiMKetal.All-causemortalityattributable
tochronickidneydisease:Aprospectivecohortstudybasedon
462293adultsinTaiwan.Lancet2008;371:2173–82.
2.HsuC-C,HwangS-J,WenC-Petal.Highprevalenceandlow
awarenessofCKDinTaiwan:Astudyontherelationshipbetween
serumcreatinineandawarenessfromanationallyrepresentative
survey.Am.J.KidneyDis.2006;48:727–38.
3.HwangS-J,LinM-Y,ChenH-Cetal.Increasedriskofmortalityin
theelderlypopulationwithlate-stagechronickidneydisease:A
cohortstudyinTaiwan.Nephrol.Dial.Transplant.2008;23:3192–8.
4.DepartmentofHealth.NationalHealthInsuranceAnnualStatistical
Report1996.DepartmentofHealth,2004:Taiwan,2004.[Cited25
August2014.]AvailablefromURL:http://www.nhi.gov.tw
5.AroraP,KauszAT,ObradorGTetal.Hospitalutilizationamong
chronicdialysispatients.J.Am.Soc.Nephrol.2000;11:740–46.
6.StPeterWL,KhanSS,EbbenJP,PereiraBJG,CollinsAJ.Chronic
kidneydisease:Thedistributionofhealthcaredollars.KidneyInt.
2004;66:313–21.
7. KeithDS,NicholsGA,GullionCM,BrownJB,SmithDH.
Longitudinalfollow-upandoutcomesamongapopulationwith
chronickidneydiseaseinalargemanagedcareorganization.Arch.
Intern.Med.2004;164:659–63.
8. GullionCM,KeithDS,NicholsGA,SmithDH.Impactof
comorbiditiesonmortalityinmanagedcarepatientswithCKD.
Am.J.KidneyDis.2006;48:212–20.
9. NationalKidneyF.K/DOQIclinicalpracticeguidelinesforchronic
kidneydisease:Evaluation,classification,andstratification.Am.J.
KidneyDis.2002;39:S1–266.
10.LevinA,StevensPE.EarlydetectionofCKD:Thebenefits,
limitationsandeffectsonprognosis.Nat.Rev.Nephrol.2011;7:
446–57.
11.SmartNA,TitusTT.Outcomesofearlyversuslatenephrology
referralinchronickidneydisease:Asystematicreview.Am.J.Med.
2011;124:1073–1080.e1072.
12.MasonJ,KhuntiK,StoneM,FarooqiA,CarrS.Educational
interventionsinkidneydiseasecare:Asystematicreviewof
MDCimprovesoutcomesandreducescosts
13. HemmelgarnBR,MannsBJ,ZhangJetal.Associationbetween
multidisciplinarycareandsurvivalforelderlypatientswithchronic
kidneydisease.J.Am.Soc.Nephrol.2007;18:993–9.
14. WuIW,WangS-Y,HsuK-Hetal.Multidisciplinarypredialysis
educationdecreasestheincidenceofdialysisandreducesmortality
–acontrolledcohortstudybasedontheNKF/DOQIguidelines.
Nephrol.Dial.Transplant.2009;24:3426–33.
15. CurtisBM,RavaniP,MalbertiFetal.Theshort-andlong-term
impactofmulti-disciplinaryclinicsinadditiontostandard
nephrologycareonpatientoutcomes.Nephrol.Dial.Transplant.
2005;20:147–54.
16. RomanoPS,RoosLL,JollisJG.Presentationadaptingaclinical
comorbidityindexforusewithICD-9-CMadministrativedata:
Differingperspectives.J.Clin.Epidemiol.1993;46:1075–9.
17. WeiS-Y,ChangY-Y,MauL-Wetal.Chronickidneydiseasecare
programimprovesqualityofpre-end-stagerenaldiseasecareand
reducesmedicalcosts.Nephrology2010;15:108–15.
18. ChenYR,YangY,WangSCetal.Effectivenessofmultidisciplinary
careforchronickidneydiseaseinTaiwan:A3-yearprospective
cohortstudy.Nephrol.Dial.Transplant.2013;28:671–82.
19. HwangS-J,YangW-C,LinM-Y,MauL-W,ChenH-C,Taiwan
SocietyofN.Impactoftheclinicalconditionsatdialysisinitiation
onmortalityinincidenthaemodialysispatients:Anationalcohort
studyinTaiwan.Nephrol.Dial.Transplant.2010;25:2616–24.
20. PisoniRL,ArringtonCJ,AlbertJMetal.Facilityhemodialysis
vascularaccessuseandmortalityincountriesparticipatingin
DOPPS:Aninstrumentalvariableanalysis.Am.J.KidneyDis.2009;
53:475–91.
21. PerlJ,WaldR,McFarlanePetal.Hemodialysisvascularaccess
modifiestheassociationbetweendialysismodalityandsurvival.
J.Am.Soc.Nephrol.2011;22:1113–21.
22.GoovaertsT,JadoulM,GoffinE.Influenceofapre-dialysis
educationprogramme(PDEP)onthemodeofrenalreplacement
therapy.Nephrol.Dial.Transplant.2005;20:1842–7.
23.MannsBJ,TaubK,VanderstraetenCetal.Theimpactofeducation
onchronickidneydiseasepatients’planstoinitiatedialysiswith
self-caredialysis:Arandomizedtrial.KidneyInt.2005;68:
1777–83.
24.SmithDH,GullionCM,NicholsG,KeithDS,BrownJB.Costof
medicalcareforchronickidneydiseaseandcomorbidityamong
enrolleesinalargeHMOpopulation.J.Am.Soc.Nephrol.2004;15:
1300–6.
25.MixTCH,StPeterWL,EbbenJetal.Hospitalizationduring
advancingchronickidneydisease.Am.J.KidneyDis.2003;42:
972–81.
26.HunsickerLG.Theconsequencesandcostsofchronickidney
diseasebeforeESRD.J.Am.Soc.Nephrol.2004;15:1363–4.
27.BessetteRW,CarterRL.PredictinghospitalcostinCKDpatients
throughbloodchemistryvalues.BMCNephrol.2011;12:65.
28.LaliberteF,BookhartBK,VekemanFetal.Directall-causehealth
carecostsassociatedwithchronickidneydiseaseinpatientswith
diabetesandhypertension:Amanagedcareperspective.J.Manag.
CarePharm.2009;15:312–22.
29.WuM-S,WuI-W,ShihC-P,HsuK-H.Establishingaplatformfor
battlingend-stagerenaldiseaseandcontinuingquality
improvementindialysistherapyinTaiwan.ActaNephrol.2011;25:
148–53.
30.DoganE,ErkocR,SayarliogluH,DurmusA,TopalC.Effectsof
latereferraltoanephrologistinpatientswithchronicrenalfailure.
Nephrology2005;10:516–19.
31.HuismanRM.Thedeadlyriskoflatereferral.Nephrol.Dial.
Transplant.2004;19:2175–80.