Kidney Cancer and Diabetes Mellitus: A Population-based
Case-control Study in Taiwan
Shih Wei Lai,1,2MD, Kuan Fu Liao,3,4,5MD, MS, Hsueh Chou Lai,6,7MD, MS, Pang Yao Tsai,8,9MPH, Fung Chang Sung,8,9PhD, MPH, Pei Chun Chen,10PhD, MSPH
(The first two authors contributed equally to this study.)
1School of Medicine, China Medical University, Taichung, 404, Taiwan
2Department of Family Medicine, China Medical University Hospital, Taichung, 404, Taiwan
3Department of Internal Medicine, Taichung Tzu Chi General Hospital, Taichung, 427, Taiwan
4School of Medicine, Tzu Chi University, Hualien, 970, Taiwan
5Department of health care administration, Central Taiwan University of Science and Technology, Taichung, 406, Taiwan
6School of Chinese Medicine, China Medical University, Taichung, 404, Taiwan 7Department of Internal Medicine, China Medical University Hospital, Taichung, 404, Taiwan
8Department of Public Health, China Medical University, Taichung, 404, Taiwan 9Management Office for Health Data, China Medical University Hospital, Taichung, 404, Taiwan
10Graduate Institute of Epidemiology and Preventive Medicine, College of Public Health, National Taiwan University, Taipei, 100, Taiwan
Address for correspondence: Dr Pei-Chun Chen, Graduate Institute of Epidemiology and Preventive Medicine, College of Public Health, National Taiwan University, 5Fl. No. 17, Hsu Chow Road, Taipei, 100, Taiwan
E-mail: eliz0118@gmail.com
ABSTRACT
Introduction: The purpose of this study was to explore whether diabetes mellitus
(DM) correlates with the risk of kidney cancer in Taiwan. Materials and Methods: We designed a population-based case-control study from the Taiwan National Health Insurance Database, which consisted of 116 patients with newly diagnosed kidney cancer as cases and 464 subjects without kidney cancer as controls in 2000 to 2009. Both cases and controls were aged ≥ 20 years. Baseline comorbidities were compared between kidney cancer cases and controls. Results: Multivariable analysis showed no association was detected between DM and kidney cancer (OR 1.06, 95% CI 0.58-1.94). Hypertension (OR 2.05, 95% 1.23-3.42), chronic kidney diseases (OR 2.57, 95% 1.23-5.37), cystic kidney diseases (OR 18.6, 95% CI 1.84-187.6) and kidney stones (OR 4.02, 95% CI 2.43-6.66) were significant comorbidities associated with increased risk of kidney cancer. Use of alpha-glucosidase inhibitor was associated with increased risk of kidney cancer (OR 4.31, 95% CI 1.07-17.3). Conclusions: DM does not correlate with the risk of kidney cancer. Hypertension, chronic kidney diseases, cystic kidney diseases, kidney stones and use of alpha-glucosidase inhibitors are associated with kidney cancer.
Keywords: Chronic kidney disease; Cystic kidney disease; Diabetes mellitus; Hypertension; Kidney cancer; Kidney stone
INTRODUCTION
Kidney cancer accounts for 3% to 4% of all cancers.1 In a systematic review by Mathew and et al,2 the incidence of kidney cancer was the highest in France (16.1 per 100,000 man-years) and the lowest in India (0.9 per 100,000 woman-years) during 1988 to 1992. A trend analysis in North America by Sun et al3 showed that the age-adjusted incidence of renal cell carcinoma rose from 7.6 per 100,000 person-years in 1988 to 11.7 per 100,000 person-years in 2006. This incidence has been increasing substantially in the world, but varies markedly. In Taiwan, kidney cancer ranked the eighteenth leading cause of cancer death in 2010 and the current mortality rate was around 2.0 to 2.3 per 100,000 persons in 2006 to 2010.4
Kidney cancer includes renal cell carcinoma arising from renal parenchyma (accounting for 90% of kidney cancer), and transitional cell carcinoma arising from renal pelvis. Although the real cause of kidney cancer remains unclear, to date, epidemiologic studies have shown that smoking, obesity, hypertension, end-stage renal disease, occupational exposure to chemical agents and genetic factors are the risk factors that contribute to development of kidney cancer worldwide.6-9 On the other hand, accumulating evidence has suggested that diabetes mellitus (DM) may affect the cancer risks of colon-rectum, liver and pancreas. In 2 large cohort studies in Japan and in the United States, men with DM may have an increase of 1.1 to 1.9-fold risk of kidney cancer. In a systematic review by Larsson et al,14 DM might also
increase 1.4-fold risk of kidney cancer (95% CI = 1.06-1.91), compared with non-diabetes.
There is no updated evidence about the association between DM and kidney cancer in Taiwan. Identifying the risk factors of kidney cancer is of importance to prevent this disease and further improve its prognosis. Therefore, we conducted this
population-based case-control study using data from the National Health Insurance (NHI) program in Taiwan to explore the following questions: (i) whether there is an association between DM and kidney cancer (ii) what the roles of other comorbidities on the risk of kidney cancer are (iii) what the impact of anti-diabetic drugs on the risk of kidney cancer is.
MATERIALS AND METHODS Data sources
This case-control study used the research database of the NHI program of Taiwan, which contains claims data of one million subjects randomly selected from all NHI beneficiaries. Details of the insurance program and the research database can be found in previous studies.15-18
Design
This was a population-based case-control study. Cases were the subjects who were newly diagnosed with kidney cancer (renal cell carcinoma, ICD-9 189.0) during the period of 2000 to 2009 and aged 20 years and above at the date of diagnosis. The index date for each case was the date of diagnosis with kidney cancer, and we defined the index date of control subjects as the date of kidney cancer diagnosis of their corresponding cases. For each kidney cancer case, 4 controls were randomly selected from the same dataset, after excluding the subjects with kidney cancer, any other cancer (ICD-9 140-208 and A-code A08x-A14x) or kidney transplant (ICD-9 V42.0) before the index date. In order to explore the potential comorbidities associated with the risk of kidney cancer, we retrospectively screened the medical history for each subject. Comorbidities prior to the index date included are as follows: DM (ICD-9 250.xx and A-code A181), obesity (ICD-9 278.00, 278.01, and A-code A183), hypertension (ICD-9 401-405, and A-code A260, A269), tobacco use (ICD-9 305.1),
alcoholism (ICD-9 303, 305.00, 305.01, 305.02, 305.03 and V11.3), kidney infections (ICD-9 590.x, and A-code A351), chronic kidney diseases (ICD-9 585, 586, 588.8 and 588.9), cystic kidney diseases (ICD-9 753.1x), and kidney stones (ICD-9 592.0, 592.1, 592.9, and A-code 352).
Statistical analysis
We compared the difference in sex, age, and comorbidities between the kidney cancer cases and the controls using the Chi-square test and t test. The significant variables were further included in the multivariable logistic regression analysis to measure odds ratio (OR) and 95% confidence interval (CI) for kidney cancer. The statistical
significance level was set at probability value of < 0.05 (SAS software version 9.1, SAS Institute Inc., Cary, North Carolina, USA).
Ethical considerations
All types of personal identification on files connected with the present study were scrambled using surrogate identification numbers to secure patient privacy. The present study was exempted from a full review by the Institutional Review Board at College of Public Health, China Medical University.
RESULTS
Baseline characteristics of the study population
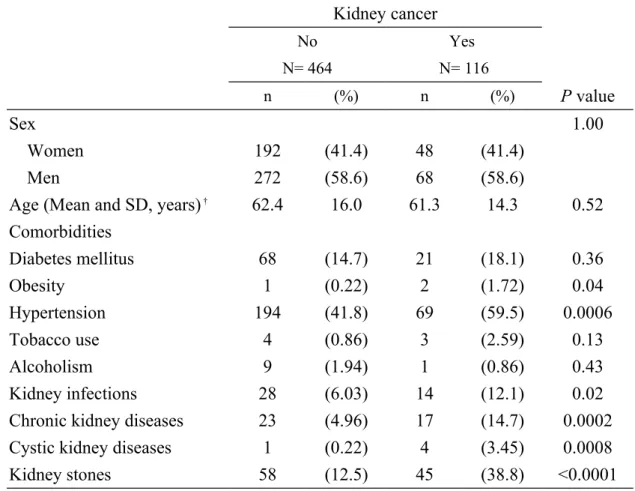
From 2000 to 2009, we identified 116 new cases of kidney cancer. Table 1
compares the demographic characteristics and comorbidities between kidney cancer cases and controls. The cases were more likely to have obesity, hypertension, kidney infections, chronic kidney diseases, cystic kidney diseases and kidney stones.
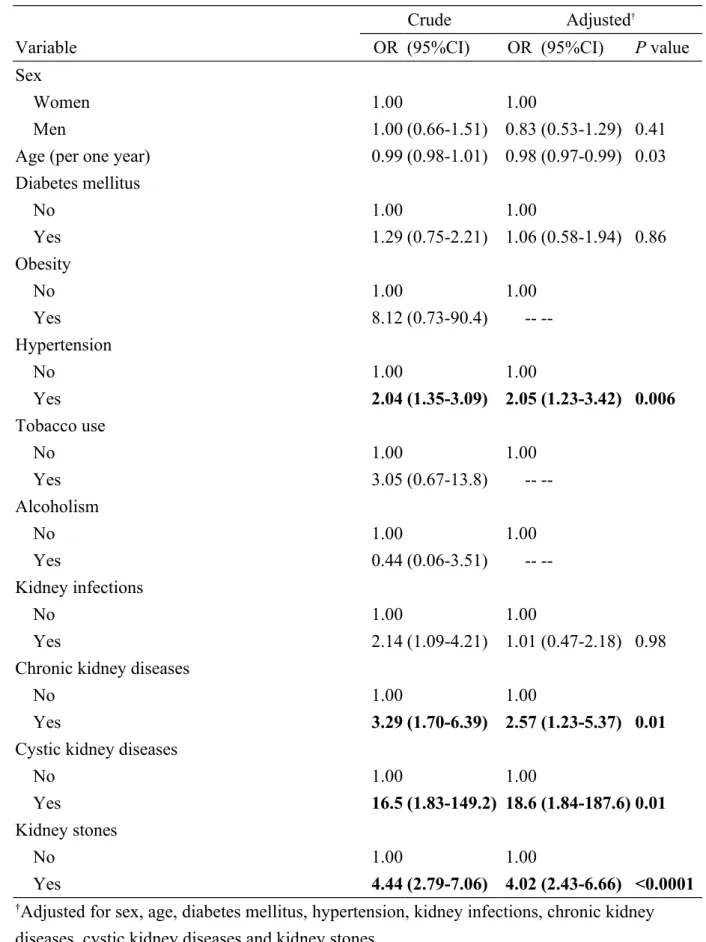
Related factors for kidney cancer by multivariable logistic regression
The results of multivariable logistic regression analysis showed no association was observed between DM and kidney cancer (OR 1.06, 95% CI 0.58-1.94) after adjusting for variables that were significantly related to kidney cancer from the crude analysis (Table 2). Hypertension (OR 2.05, 95% 1.23-3.42), chronic kidney diseases (OR 2.57, 95% 1.23-5.37), cystic kidney diseases (OR 18.6, 95% CI 1.84-187.6) and kidney stones (OR 4.02, 95% CI 2.43-6.66) were independent comorbidities
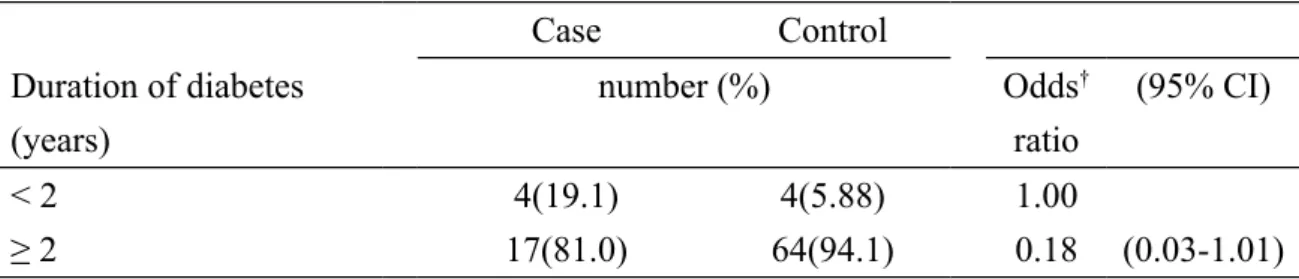
significantly associated with kidney cancer. The further analysis was performed using only the diabetic cases. After adjusting for variables, diabetic duration was not
significantly related to the risk of kidney cancer (Table 3).
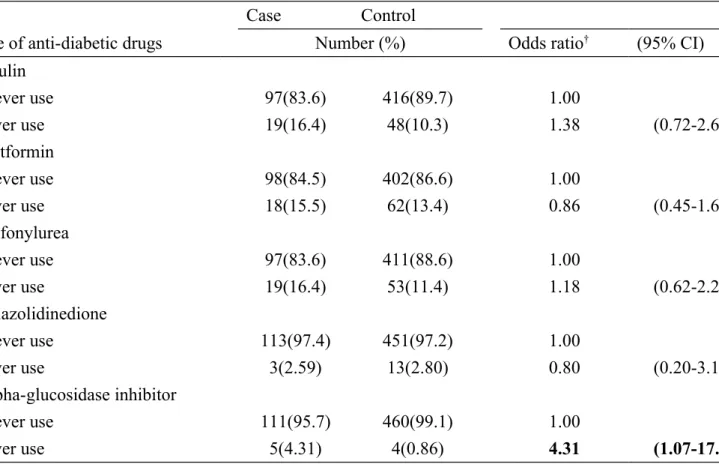
Influence of anti-diabetic drugs on the risk of kidney cancer
Table 4 shows the effects of anti-diabetic drugs on the risk of kidney cancer. After adjustments for potential confounders, the OR for use of alpha-glucosidase inhibitor vs. no use was 4.31 (95% CI 1.07-17.3). No significant association was found
between other anti-diabetic drugs and the risk of kidney cancer. .
DISCUSSION
Though not novel, to the best of our knowledge, this is the first case-control study to discuss the association between DM and kidney cancer in Taiwan, making this a timely contribution to the growing literature on diabetes and cancers. A large cohort study in Japan by Inoue et al12 found that after exclusion of kidney cancer diagnosed within 5 years of baseline, the hazard ratio of kidney cancer remained high in diabetic patients (HR 2.41, 95% CI =1.22-4.78). A large cohort study in US by Atchison et al13 showed that the relative risk of kidney cancer was 1.24 after 2 to 5 years between diagnoses of DM and kidney cancer (95% CI 1.11–1.38), 1.09 after 6 to 10 years (95% CI 0.97–1.22) and decreasing to 1.00 after >10 years (95% CI 0.91–1.10). However, a cohort study in Japan by Washio et al19 showed that though DM showed an increased risk of kidney cancer death in age- and sex-adjusted model (HR 2.22, 95% CI 1.04-4.70), after controlling for covariates, it did not achieve statistical significance (HR 1.52, 95% CI 0.60–3.85).19 In the present study, we did not observe
an association between DM and kidney cancer, irrespective of diabetic duration. Because this was an observational study, we do not have a plausible explanation why no association was detected between DM and kidney cancer in Taiwan. However, the different populations may partially account for the conflicting results between the present study and the others.
The other medical conditions significantly associated with kidney cancer found in the present study are consistent with the established evidence in literature. These
conditions include hypertension (OR 2.05), chronic kidney diseases (OR 2.57), cystic kidney diseases (OR 18.6) and kidney stones (OR 4.02). This further confirms that the etiology of kidney cancer is multi-factorial. However, detection bias should be
considered, because patients with these above conditions would receive much more attention such as frequent kidney imaging, and small renal masses that might not otherwise be discovered could be identified and treated.
In the present study, use of alpha-glucosidase inhibitor was found to be associated with the risk of kidney cancer (OR 4.31). Because there was no similar report previously and the case number was small in the present study, we could not make a plausible explanation why the use of alpha-glucosidase inhibitor is associated with the increased risk of kidney cancer.
It should be noted that there were some limitations in the present study. First, because there was an inherent limitation of using health insurance dataset, a number of suspected risk factors of kidney cancer were not available in this dataset, such as
included these covariates by using ICD-9 codes, only small case numbers could be found. Third, the information about tumour stage, tumour size, kidney function, blood glucose level, and HbA1c were also not available because of the inherent limitation of this dataset. Further studies including these related factors are needed to clarify the issue of kidney cancer.
CONCLUSION
This study suggests that: (1) DM does not correlate with the risk of kidney cancer (2) Hypertension, chronic kidney diseases, cystic kidney diseases and kidney stones are associated with kidney cancer (3) Use of alpha-glucosidase inhibitor is associated with kidney cancer.
Funding
This study was supported in part by grants from Taiwan Department of Health Clinical Trial and Research Center of Excellence (DOH101-TD-B-111-004), the Cancer Research Center of Excellence (DOH 101-TD-C-111-005), and the National Science Council (NSC 100-2621-M-039-001). The funding agencies did not
influence the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Acknowledgements
The authors thank the National Health Research Institute in Taiwan for providing the insurance claims data.
Conflict of Interest Statement
Table 1. Comparison by sociodemographic factors and other medical conditions between kidney cancer cases and controls
Kidney cancer No N= 464 Yes N= 116 n (%) n (%) P value Sex 1.00 Women 192 (41.4) 48 (41.4) Men 272 (58.6) 68 (58.6)
Age (Mean and SD, years) † 62.4 16.0 61.3 14.3 0.52
Comorbidities Diabetes mellitus 68 (14.7) 21 (18.1) 0.36 Obesity 1 (0.22) 2 (1.72) 0.04 Hypertension 194 (41.8) 69 (59.5) 0.0006 Tobacco use 4 (0.86) 3 (2.59) 0.13 Alcoholism 9 (1.94) 1 (0.86) 0.43 Kidney infections 28 (6.03) 14 (12.1) 0.02
Chronic kidney diseases 23 (4.96) 17 (14.7) 0.0002
Cystic kidney diseases 1 (0.22) 4 (3.45) 0.0008
Kidney stones 58 (12.5) 45 (38.8) <0.0001
data are presented as the number of subjects in each group, with percentages given in parentheses
Table 2. Crude and adjusted odds ratios and 95% confidence intervals of kidney cancer associated with diabetes and covariates
Crude Adjusted†
Variable OR (95%CI) OR (95%CI) P value
Sex
Women 1.00 1.00
Men 1.00 (0.66-1.51) 0.83 (0.53-1.29) 0.41
Age (per one year) 0.99 (0.98-1.01) 0.98 (0.97-0.99) 0.03 Diabetes mellitus No 1.00 1.00 Yes 1.29 (0.75-2.21) 1.06 (0.58-1.94) 0.86 Obesity No 1.00 1.00 Yes 8.12 (0.73-90.4) --Hypertension No 1.00 1.00 Yes 2.04 (1.35-3.09) 2.05 (1.23-3.42) 0.006 Tobacco use No 1.00 1.00 Yes 3.05 (0.67-13.8) --Alcoholism No 1.00 1.00 Yes 0.44 (0.06-3.51) --Kidney infections No 1.00 1.00 Yes 2.14 (1.09-4.21) 1.01 (0.47-2.18) 0.98
Chronic kidney diseases
No 1.00 1.00
Yes 3.29 (1.70-6.39) 2.57 (1.23-5.37) 0.01
Cystic kidney diseases
No 1.00 1.00
Yes 16.5 (1.83-149.2) 18.6 (1.84-187.6) 0.01
Kidney stones
No 1.00 1.00
Yes 4.44 (2.79-7.06) 4.02 (2.43-6.66) <0.0001
†Adjusted for sex, age, diabetes mellitus, hypertension, kidney infections, chronic kidney diseases, cystic kidney diseases and kidney stones
OR, odds ratio: CI, confidence interval
Table 3. Adjusted odds ratios of kidney cancer in relation to duration of diabetes
Case Control Duration of diabetes (years) number (%) Odds† ratio (95% CI) < 2 4(19.1) 4(5.88) 1.00 ≥ 2 17(81.0) 64(94.1) 0.18 (0.03-1.01)
†Adjusted for sex, age, hypertension, kidney infections, chronic kidney diseases, cystic kidney diseases and kidney stones
Table 4. Adjusted odds ratios of kidney cancer in relation to use of anti-diabetic drugs
Case Control
Use of anti-diabetic drugs Number (%) Odds ratio† (95% CI)
Insulin never use 97(83.6) 416(89.7) 1.00 ever use 19(16.4) 48(10.3) 1.38 (0.72-2.64) Metformin never use 98(84.5) 402(86.6) 1.00 ever use 18(15.5) 62(13.4) 0.86 (0.45-1.62) Sulfonylurea never use 97(83.6) 411(88.6) 1.00 ever use 19(16.4) 53(11.4) 1.18 (0.62-2.24) Thiazolidinedione never use 113(97.4) 451(97.2) 1.00 ever use 3(2.59) 13(2.80) 0.80 (0.20-3.19) Alpha-glucosidase inhibitor never use 111(95.7) 460(99.1) 1.00 ever use 5(4.31) 4(0.86) 4.31 (1.07-17.3)
†Adjusted for sex, age, hypertension, kidney infections, chronic kidney diseases, cystic kidney diseases and kidney stones