Title: Prevalence and location of maxillary sinus septa
in the Taiwanese population and relationship to the
absence of molars
Abstract
Objectives: Understanding the septum structure of the sinus is necessary for correct implant placement in the maxilla if sinus encroachment is required. The exact mechanism that controls septum development is unclear, although a role for the irregular pneumatization of the sinus floor following tooth loss has been suggested. The aims of this study were to examine the prevalence and location of sinus septa in the Taiwanese population and to determine whether there is a relationship between the presence of septa and the absence of molars.
Materials and Methods: Using computed tomography (CT) scans of sinuses obtained from 423 subjects (216 women and 207 men, mean age 53.65 years), septum
morphology and its correlation with the presence of molars was examined.
Results: About 30% of subjects (124/423) had sinus septa, corresponding to 20.45% of all sinus segments detected (173/846). Fifty-nine patients had multiple septa, giving a prevalence of septa of 22.93%. Septa were located most frequently in the regions of the first and second molars. The prevalence was not related to tooth loss (edentulous, partially edentulous, or dentate maxillary segments). Logistic regression analysis showed that men were significantly more likely to have septa than were women (OR = 1.67; P = 0.019).
Conclusions: In the 423 Taiwanese subjects tested, the prevalence of septum was 29.31% according to the subjects and 22.93% according to the sinus segments. The most frequent location of septa was in the region of the first and secondary molars. No correlation was observed between the presence of septa and the absence of molars.
Introduction
Implant restoration is used increasingly in cosmetic and oral functional
rehabilitation. Following tooth loss, the edentulous alveolar process of the posterior maxilla often undergoes atrophy-related resorption (Kim, et al. 2006), which causes loss of vertical bone volume and marked sinus pneumatization. The extent of these changes varies between individuals. The atrophy-related resorption often leaves inadequate bone height for anchorage of dental implants. In such cases, sinus augmentation to elevate the sinus floor is required before the placement of an endosseous implant (van den Bergh, et al. 2000).
Detailed knowledge about maxillary sinus anatomy and the possible anatomic variations is required before surgical intervention can be performed in the posterior maxillary region. Complications of sinus augmentation, including soft tissue
perforation, hemosinus, oroantral fistula, and sinusitis, have been reported (Jensen, et al. 1998, Bhattacharyya 1999, Misch 1987, Timmenga, et al. 1997, Chanavaz 1990, Regev, et al. 1995, Ziccardi & Betts 1999). The anatomic variation in the maxillary sinus such as the septa can increase the risk of sinus membrane perforation during sinus augmentation (van den Bergh, et al. 2000, Jensen, et al. 1998, Chanavaz 1990, Krennmair, et al. 1999, Tatum 1986, Betts & Miloro 1994). The presence of septa may make it difficult to prevent tearing of the Schneiderian membrane while elevating it from the sinus floor and can limit the creation of a lateral window (Boyne & James 1980, Tidwell, et al. 1992).
skulls (90 sinuses), corresponding to a prevalence of 33.33%, and the direction of the septa radiated out from the medial wall toward the lateral wall of the sinus. He further described the septa as arising between areas of two adjacent teeth and as presenting usually in three specific regions of the sinus floor. Each basin corresponds to three defined periods of tooth development and eruption separated by time. It was thought that this pattern reflects the later occurrence of eruption and that the size of the septa is accentuated by further pneumatization of the alveolar process.
Vinter et al. in 1993 observed that atrophy of the maxillary alveolar process proceeds irregularly in different regions and leaves bony crests on the maxillary sinus floor (Vinter, et al. 1993). In 1999, Krennmair et al. proposed a classification of congenital and acquired septa into primary septa, which arise during development of the maxilla, and secondary septa, which arise from irregular pneumatization of the sinus floor following tooth loss (Krennmair, et al. 1999). In 2000, van den Bergh proposed that the septa provide a masticatory force by carrying the struts during the dentate phase of life but that they seem to disappear slowly when teeth are lost (van den Bergh, et al. 2000). However, the exact mechanism responsible for maxillary septum development is still uncertain.
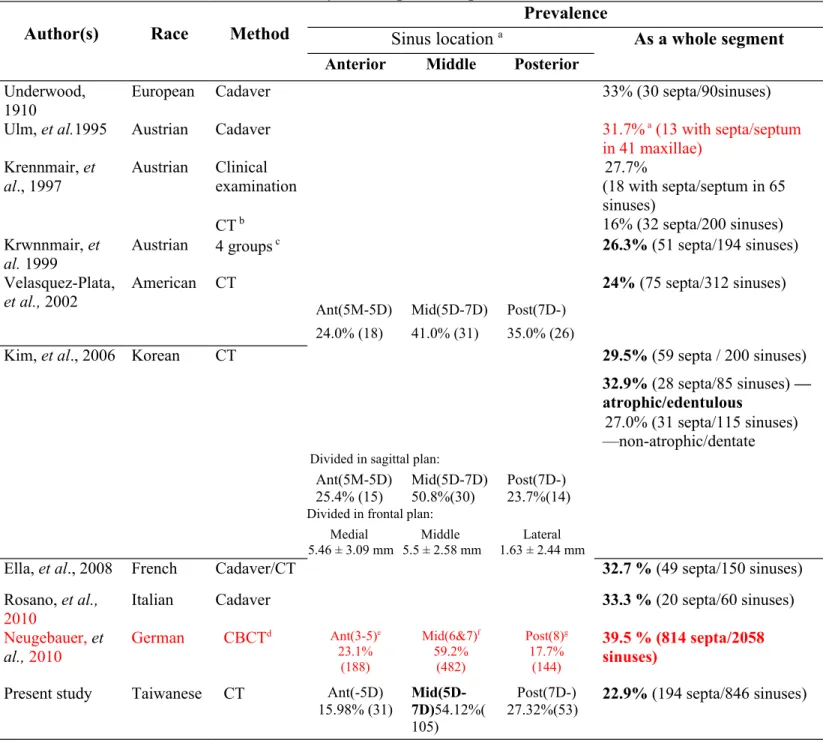
The prevalence of multiple septa in the maxillary sinus varies from 16% to 39.5% in the literature (Table 1) (Kim, et al. 2006, Krennmair, et al. 1999,
Underwood 1910, Krennmair, et al. 1997, Velasquez-Plata, et al. 2002, Ella, et al. 2008, Rosano, et al. 2010, Maestre-Ferrin, et al. 2010, Ulm, et al. 1995, Neugebauer, et al. 2010). The definition of “prevalence of septa” varies between reports. To calculate prevalence, previous reports have expressed the denominator as per subject,
maxilla, or sinus, and the numerator as the number of subjects with a septum or the number of septa (Maestre-Ferrin, et al. 2010). In addition, the observation
methodology varies between studies; data were obtained from direct clinical
observation, human autopsy, or various forms of radiography, and the classifications differed.
The location of septum was mainly in the posterior position distal to the third molar roots, according to the observation by Underwood; however, most septa were found in the anterior (premolar) region in the study by Krennmair et al.(Krennmair, et al. 1999, Underwood 1910). Recent studies further reported a higher prevalence (41.0%) of septa in the middle region, from the distal aspect of the second premolar to the distal aspect of the second molar (Kim, et al. 2006, Velasquez-Plata, et al. 2002, Rosano, et al. 2010). Possible differences between ethnic groups may contribute to these differences. The literature has focused on Caucasian populations in Europe and North America, but an Asian population (Korean) was included in only one study (Table 1). The purposes of this study were to estimate the prevalence and location of maxillary sinus septa in the Taiwanese population and to evaluate further the
relationship between the presence of septa and the absence of molars. We used radiographic (computed tomography, CT) imaging in 423 Taiwanese people.
Material & Methods:
Five hundred sets of CT images were screened initially based on the CT examination of paranasal sinuses in Otorhinolaryngology section of Taipei Tzu-Chi General Hospital in 2005 and 2006. The study received Institutional Review Board approval. CT images with inadequate information (e.g., the field of CT images did not extend to maxillary alveolar bone or molars) or that showed signs of a previous operation or injury (e.g., fractured sinus) were excluded. A total of 423 CT images obtained from 216 females and 207 males (age range 13–89 years, mean age 53.65 years), were finally included in this study. The sinus CT scans were performed using a 64-slice multidetector CT system (LightSpeed VCT 64; GE Healthcare, Milwaukee, WI, USA). The scan parameters were: helical pitch, 0.531; gantry rotation time, 1 s; tube voltage, 120 kV, and tube current, 250 to 400 mA. At 2.5-mm intervals, 2.5-mm axial images were obtained from the level of the apex of the maxillary teeth to the level of the top of the frontal sinus.
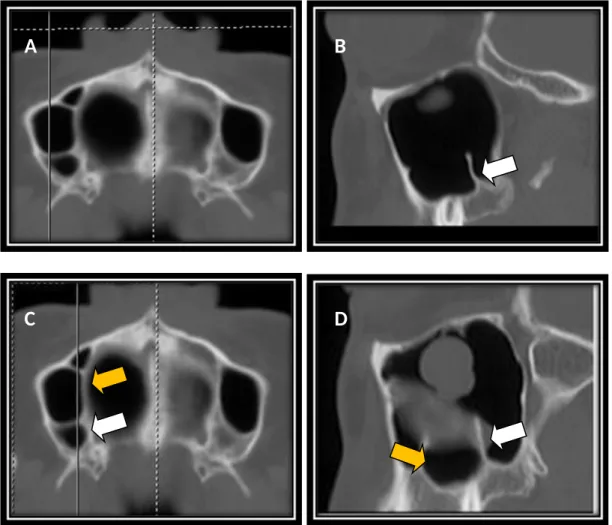
The CT images were examined for the presence of antral septa using the axial planes and the subsequently reconstructed sagittal planes of each section. The following criteria were used to identify the presence of a septum or septa on the maxillary sinus floor. First, the images showed separated complete compartments that were divided by a bony structure on the axial view. Second, the images showed a crest- or ridge-like bony structure in the related position on the sagittal view (Figure 1).
To examine the relationship between the presence of teeth and the occurrence of septa, the anatomic location of the septa was recorded in relation to the maxillary posterior teeth inferior to the septum on consecutive sagittal views. The septum was
classified on the basis of the location and its relationship to the existing tooth or teeth. Three regions were identified using a modification of a previous study(Kim, et al. 2006) as anterior (mesial to the distal aspect of the second premolar; mesial to 5D), middle (from the distal aspect of the second premolar to the distal aspect of the second molar; 5D–7D), and posterior (distal to the distal aspect of the second molar; distal to 7D). An atrophic maxillary dental ridge was defined according to the presence or absence of teeth as: missing (6, 7, and 8 missing), nonatrophic (6 and 7 present), and partially atrophic (between atrophic and nonatrophic) (Kim, et al. 2006, Krennmair, et al. 1999, Krennmair, et al. 1997, Velasquez-Plata, et al. 2002). In addition, a septum located apically to the maxillary root at the dentate site was defined as a primary septum and that located apically to an edentulous ridge was classified as an other septum because it is impossible to label a septum located apical to an edentulous ridge as either primary or secondary without a radiographic history of the sinus in question (Kim, et al. 2006). The age and sex of the subjects, the presence of a septum or septa, and the number and locations of the septa on each maxillary sinus floor were
recorded. The condition of the existing molar(s) was also recorded.
Statistical analysis
In the present study, the chi-square test was selected to examine the relationship between the distribution of sinus septa and the variables of the absence of molars, the sex and the age (with thirty year intervals) of subjects examined. For testing the effect of each variable on the presence of sinus septum, the logistic regression analysis was further used. The odds ratio (OR) and 95% confidence interval (CI) were estimated. The P < 0.05 was selected as the statistical significance.
Results
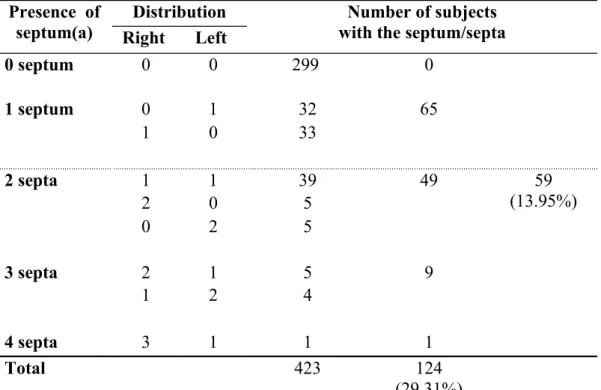
A total of 124 of the 423 subjects examined exhibited one or more sinus septa (29.31%) (Table 2A), corresponding to the presence of a septum or septa in 20.45% of sinus segments (173/846 sinuses, 86 in the right and 87 in the left) (Table 2B). In the 124 subjects who exhibited a septum or septa, 49 (39.52%) exhibited symmetrical septa (Table 2A). A total of 194 septa (98 in the right and 96 in the left) was recorded, and the prevalence of septa was 22.93% (194/846) (Table 2B). Fifty-nine subjects had multiple septa (59/423 = 13.95%): 49 had two septa, nine patients had three septa, and one had four septa (Table 2A). The presence and the prevalence of septum/septa in the right and left maxillary sinuses were similar (Table 2C). Morphologically, the septa observed in this study population all showed the transverse direction (bucco-palatal orientation) (Figure 1), radiating out from the medial wall toward the lateral wall of the maxillary sinus. The height of the septa varied.
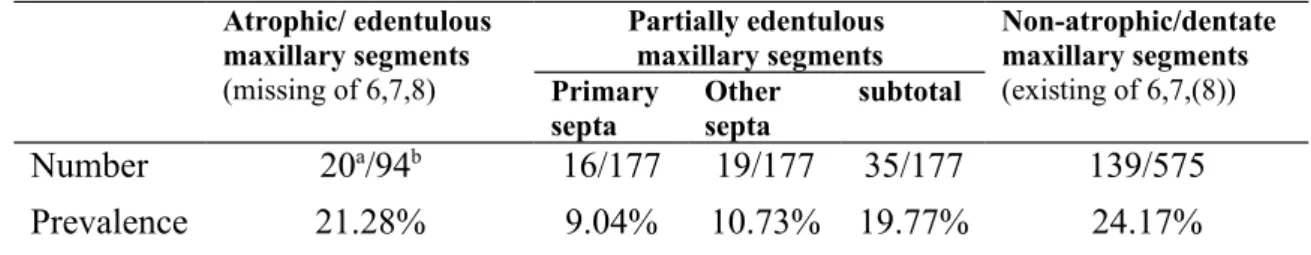
Thirty-one septa (15.98%) were located in the anterior region, 105 (54.12%) in the middle region, and 53 (27.32%) in the posterior region. Three septa (1.55%) were located across the anterior and middle regions and two septa (1.03%) were located across the middle and posterior regions (Table 3). The septa prevalence in the
atrophic, partially atrophic, and nonatrophic maxillary segments was 21.28%, 19.77%, and 24.17%, respectively (Table 4). In the partially atrophic maxillary segments (n = 177), the prevalence of primary and other septa was 9.04% for primary septa and 10.73% for other septa (Table 4).
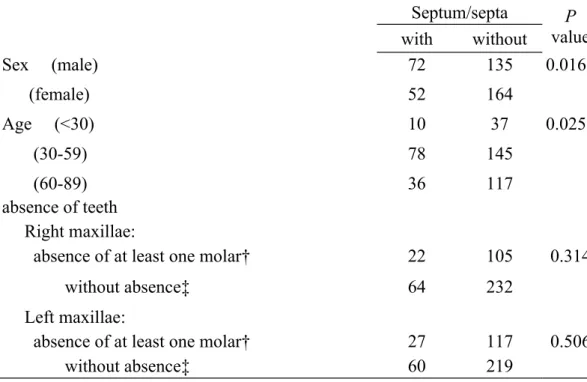
The distribution of septum/septa was not significantly related to the presence or absence of teeth (chi-square test). The distribution of septum/septa differed
significantly between males and females (P = 0.016) and between ages when grouped by 30-year intervals (P = 0.025) (Table 5A). After adjusting for sex, age, and the absence of teeth, logistic regression analysis showed that only sex was associated with septa occurrence (OR = 1.67; 95% CI = 1.09–2.55; P = 0.019) (Table 5B).
Discussion
In the present study, septa were observed in 29.31% of subjects and in 20.45% of sinus segments. The prevalence of septa was 22.93% because 59 patients had multiple septa (Table 1). The prevalence of septa in this selected Taiwanese population is similar to that reported in other populations (Table 1). In the present study, all of the septa were incomplete and appeared as residues on the sinus floor. In the present study, we observed a greater prevalence of septa in the middle region (5D–7D) (54.12%), followed by the posterior region (distal to 7D) (27.32%) and the anterior region (mesial to 5D) (15.98%). Other studies have reported a similar finding of a higher prevalence in the middle region (Kim, et al. 2006, Krennmair, et al. 1999, Underwood 1910, Velasquez-Plata, et al. 2002, Neugebauer, et al. 2010). The exact mechanism responsible for of septum development is uncertain. Septa appear from developmental or acquired malformations, and congenital septa, also referred to as “primary septa,” can develop in all maxillary sinus regions (e.g., sinus floor or anterior wall). By contrast, incomplete septa on the sinus floor, also known as
“secondary septa,” are considered to result from tooth loss and atrophy (Krennmair, et al. 1997).It is impossible to classify a septum located apically to an edentulous ridge as either primary or secondary without a radiographic history of the sinus in question. Thus, septa located apically to dentate regions can be classified as primary
(developmental) septa, whereas those located apically to an edentulous region can be defined as other septa (Kim, et al. 2006). In the present study, analysis of the partially dentate population showed similar proportions of septa located superior to a maxillary tooth (primary septa) (9.04%) as those located superior to an edentulous ridge (other septa) (10.73%). Moreover, the percentages of septa were also similar between atrophic maxillary segments (21.28%) and nonatrophic segments (24.17%). Logistic
regression showed that the absence of a tooth or teeth was not associated with higher septa occurrence, at least in this selected population in Taiwan. The absence of teeth might not increase the occurrence of so-called the secondary septa or the prevalence of septa.
In the present study, the distribution of septa prevalence differed between the three age groups grouped into 30-year intervals (P = 0.025) (Table 5). The prevalence was highest in the 30- to 59-year-olds (34.98%). However, after adjusting for other factors such as sex, age, and the absence of a tooth or teeth, only sex remained significant (P = 0.037). A recent study also found no correlation between age or sex and the prevalence of septa (Neugebauer, et al. 2010). In the present study, however, the presence of septum/septa was higher in males than in females: 34.8% (72/207) of males and 24.1% (52/216) of females exhibited a septum or septa, while 28.26% (117/414) and 17.82% (77/432) in the prevalence of septa according to sinus
segments, for male and female, respectively. After adjustment, the logistic regression showed that males had a higher occurrence of septa than females (P = 0.019) (Table 5B). The reason for the difference between this result and the results of previous studies is uncertain. However, van den Bergh et al. proposed that septa provide a masticatory force (van den Bergh, et al. 2000), which might offer a reason for higher septa prevalence in males.
In this study, the CT scans of the sinuses of 423 Taiwanese were selected to examine septum morphology and to determine whether this correlates with the presence and absence of molars. CT allows high-resolution imaging of delicate bony
maxillary sinus. In the 1999 study by Krennmair et al., panoramic radiography led to a false diagnosis of 21.3% (13/61) of subjects, and the authors proposed that CT is a better method for visualizing maxillary septa (Krennmair, et al. 1999). Others have made similar suggestions (Alder, et al. 1995, Dula, et al. 2001, Schwarz, et al. 1987). A routine CT examination before implant surgery may provide better information for dentists and may help avoid unexpected complications.
In conclusion, the prevalence of septa was 22.93% (194/846) in the 423
Taiwanese people examined, which is similar to that reported in other ethnic groups. The most frequent location of septa was in the region of the first and second molars. No relationship was observed between the presence of septa and the absence of molars. The prevalence of septa was higher in males than in females.
Kim, M.J., Jung, U.W., Kim, C.S., Kim, K.D., Choi, S.H., Kim, C.K. & Cho, K.S., (2006) Maxillary sinus septa: Prevalence, height, location, and morphology. A reformatted computed tomography scan analysis. J Periodontol 77: 903-908.
van den Bergh, J.P., ten Bruggenkate, C.M., Disch, F.J. & Tuinzing, D.B., (2000) Anatomical aspects of sinus floor elevations. Clin Oral Implants Res 11: 256-265. Jensen, O.T., Shulman, L.B., Block, M.S. & Iacono, V.J., (1998) Report of the sinus consensus conference of 1996. Int J Oral Maxillofac Implants 13 Suppl: 11-45. Bhattacharyya, N., (1999) Bilateral chronic maxillary sinusitis after the sinus-lift procedure. Am J Otolaryngol 20: 133-135.
Misch, C.E., (1987) Maxillary sinus augmentation for endosteal implants: Organized alternative treatment plans. Int J Oral Implantol 4: 49-58.
Timmenga, N.M., Raghoebar, G.M., Boering, G. & van Weissenbruch, R., (1997) Maxillary sinus function after sinus lifts for the insertion of dental implants. J Oral Maxillofac Surg 55: 936-939;discussion 940.
Chanavaz, M., (1990) Maxillary sinus: Anatomy, physiology, surgery, and bone grafting related to implantology--eleven years of surgical experience (1979-1990). J Oral Implantol 16: 199-209.
Regev, E., Smith, R.A., Perrott, D.H. & Pogrel, M.A., (1995) Maxillary sinus complications related to endosseous implants. Int J Oral Maxillofac Implants 10: 451-461.
Ziccardi, V.B. & Betts, N.K. (1999) Complications of maxillary sinus augmentation. In: O. T. Jensen, ed. The sinus bone graft, 201-208. Chiago: Quintessence.
Krennmair, G., Ulm, C.W., Lugmayr, H. & Solar, P., (1999) The incidence, location, and height of maxillary sinus septa in the edentulous and dentate maxilla. J Oral Maxillofac Surg 57: 667-671; discussion 671-662.
Tatum, H., Jr., (1986) Maxillary and sinus implant reconstructions. Dent Clin North Am 30: 207-229.
Betts, N.J. & Miloro, M., (1994) Modification of the sinus lift procedure for septa in the maxillary antrum. J Oral Maxillofac Surg 52: 332-333.
Boyne, P.J. & James, R.A., (1980) Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg 38: 613-616.
Tidwell, J.K., Blijdorp, P.A., Stoelinga, P.J., Brouns, J.B. & Hinderks, F., (1992) Composite grafting of the maxillary sinus for placement of endosteal implants. A preliminary report of 48 patients. Int J Oral Maxillofac Surg 21: 204-209.
Underwood, A.S., (1910) An inquiry into the anatomy and pathology of the maxillary sinus. J Anat Physiol 44: 354-369.
Vinter, I., Krmpotic-Nemanic, J., Hat, J. & Jalsovec, D., (1993) [does the alveolar process of the maxilla always disappear after tooth loss?]. Laryngorhinootologie 72: 605-607.
Krennmair, G., Ulm, C. & Lugmayr, H., (1997) Maxillary sinus septa: Incidence, morphology and clinical implications. J Craniomaxillofac Surg 25: 261-265.
Velasquez-Plata, D., Hovey, L.R., Peach, C.C. & Alder, M.E., (2002) Maxillary sinus septa: A 3-dimensional computerized tomographic scan analysis. Int J Oral Maxillofac Implants 17: 854-860.
Ella, B., Noble Rda, C., Lauverjat, Y., Sedarat, C., Zwetyenga, N., Siberchicot, F. & Caix, P., (2008) Septa within the sinus: Effect on elevation of the sinus floor. Br J Oral Maxillofac Surg 46: 464-467.
Maestre-Ferrin, L., Galan-Gil, S., Rubio-Serrano, M., Penarrocha-Diago, M. & Penarrocha-Oltra, D., (2010) Maxillary sinus septa: A systematic review. Medicina oral, patología oral y cirugía bucal 15: e383-386.
Ulm, C.W., Solar, P., Krennmair, G., Matejka, M. & Watzek, G., (1995) Incidence and suggested surgical management of septa in sinus-lift procedures. Int J Oral Maxillofac Implants 10: 462-465.
Neugebauer, J., Ritter, L., Mischkowski, R.A., Dreiseidler, T., Scherer, P., Ketterle, M., Rothamel, D. & Zoller, J.E., (2010) Evaluation of maxillary sinus anatomy by cone-beam ct prior to sinus floor elevation. The International journal of oral & maxillofacial implants 25: 258-265.
Som, P.M., Sacher, M., Lanzieri, C.F., Lawson, W. & Shuger, J.M., (1984) The hidden antral compartment. Radiology 152: 463-464.
Alberti, P.W., (1976) Applied surgical anatomy of the maxillary sinus. Otolaryngol Clin North Am 9: 3-20.
Alder, M.E., Deahl, S.T. & Matteson, S.R., (1995) Clinical usefulness of two-dimensional reformatted and three-two-dimensionally rendered computerized tomographic images: Literature review and a survey of surgeons' opinions. J Oral Maxillofac Surg 53: 375-386.
Dula, K., Mini, R., van der Stelt, P.F. & Buser, D., (2001) The radiographic assessment of implant patients: Decision-making criteria. Int J Oral Maxillofac Implants 16: 80-89.
Schwarz, M.S., Rothman, S.L., Rhodes, M.L. & Chafetz, N., (1987) Computed tomography: Part ii. Preoperative assessment of the maxilla for endosseous implant surgery. Int J Oral Maxillofac Implants 2: 143-148.
Table 1. Prevalence of maxillary sinus septa in the previous literatures and this study.
Author(s) Race Method Sinus location a Prevalence As a whole segment
Anterior Middle Posterior
Underwood, 1910
European Cadaver 33% (30 septa/90sinuses)
Ulm, et al.1995 Austrian Cadaver 31.7% a (13 with septa/septum
in 41 maxillae) Krennmair, et al., 1997 Austrian Clinical examination 27.7% (18 with septa/septum in 65 sinuses) CT b 16% (32 septa/200 sinuses) Krwnnmair, et al. 1999
Austrian 4 groups c 26.3% (51 septa/194 sinuses)
Velasquez-Plata,
et al., 2002
American CT 24% (75 septa/312 sinuses)
Ant(5M-5D) Mid(5D-7D) Post(7D-) 24.0% (18) 41.0% (31) 35.0% (26)
Kim, et al., 2006 Korean CT 29.5% (59 septa / 200 sinuses)
32.9% (28 septa/85 sinuses) — atrophic/edentulous
27.0% (31 septa/115 sinuses) —non-atrophic/dentate
Divided in sagittal plan:
Ant(5M-5D)
25.4% (15) Mid(5D-7D)50.8%(30) Post(7D-) 23.7%(14)
Divided in frontal plan: Medial
5.46 ± 3.09 mm 5.5 ± 2.58 mmMiddle 1.63 ± 2.44 mmLateral
Ella, et al., 2008 French Cadaver/CT 32.7 % (49 septa/150 sinuses)
Rosano, et al.,
2010
Italian Cadaver 33.3 % (20 septa/60 sinuses)
Neugebauer, et al., 2010 German CBCTd Ant(3-5)e 23.1% (188) Mid(6&7)f 59.2% (482) Post(8)g 17.7% (144) 39.5 % (814 septa/2058 sinuses)
Present study Taiwanese CT Ant(-5D)
15.98% (31) Mid(5D-7D)54.12%(
105)
Post(7D-)
27.32%(53) 22.9% (194 septa/846 sinuses)
a: the prevalence of one or more septa per sinus b: computed tomography
c: group I: by using the images from panoramic radiography
group II: direct examination on cadavers
Table 2. Distribution of maxillary sinus septa in the CT images from 423 Taiwanese. A. The distribution of the presence of septum/septa in 423 subjects (the numbers with
underline and bold indicate the subjects presented septa in both right and left sinuses).
Presence of septum(a)
Distribution Number of subjects
with the septum/septa Right Left 0 septum 0 0 299 0 1 septum 0 1 32 65 1 0 33 2 septa 1 1 39 49 59 (13.95%) 2 0 5 0 2 5 3 septa 2 1 5 9 1 2 4 4 septa 3 1 1 1 Total 423 124 (29.31%)
B. The prevalence of sinus presenting one or more sinus septa and the prevalence of septa in all examined 846 sinuses.
Number (sinus or septa) All sinuses Prevalence Total sinuses with
septum/septa
173
(86 in right, 87 in left)
846
20.45% Total septa in all
examined sinuses (1 * 65 + 2 * 49 + 3* 9 + 4*1)194 22.93% C. The distribution of septum/septa occurred in right and left sides.
With septum/septa N of septa Right (N=423) 86 (20.3 %) 98 (23.17 %)
Table 3. Distribution of maxillary sinus septa according the location of tooth. Anterior (-5D) Middle (5D-7D) Posterior (7D-)
Crossing two zones
Total septa From Anterior to Middle (-5D)-(5D-7D) From Middle to Posterior (5D-7D)-(7D-) N septa 31 (15.98%) 105 (54.12%) 53 (27.32%) 3 (1.55%) 2 (1.03%) 194
Table 4. Distribution of sinus septa in atrophic, partially atrophic and non-atrophic maxillary segments in the 423 subjects examined.
Atrophic/ edentulous maxillary segments (missing of 6,7,8) Partially edentulous maxillary segments Non-atrophic/dentate maxillary segments (existing of 6,7,(8)) Primary
septa Other septa subtotal
Number 20a/94b 16/177 19/177 35/177 139/575
Prevalence 21.28% 9.04% 10.73% 19.77% 24.17%
Primary septa: septa located apical to maxillary root in dentate sites of partially dentate group.
Other septa: septa located apical to edentulous maxillary ridge in missing sites of partially dentate group.
a.: Number of septa b.: Number of sinuses
Table 5. The effect of the absence of molar, the sex, and the age of examined subject on the distribution of sinus septum/septa.
A. Sample characteristics Septum/septa P value with without Sex (male) 72 135 0.016* (female) 52 164 Age (<30) 10 37 0.025* (30-59) 78 145 (60-89) 36 117 absence of teeth Right maxillae:
absence of at least one molar† 22 105 0.314
without absence‡ 64 232
Left maxillae:
absence of at least one molar† 27 117 0.506
without absence‡ 60 219
*. Chi-squared test for count variables for difference in trend cross waves, statistical significance was noted if p < 0.05.
†: The absence of third molar was not included ‡: Presence of all molars or the first two molars B. Logistic regression analysis
Odds ratio Std. error z P>|z| 95% conf. interval
gender 1.67 0.36 2.35 0.02 1.09 2.55 age 0.99 0.01 -1.09 0.28 0.98 1.01 absence of molar (Right) 0.91 0.20 -0.43 0.67 0.60 1.39 absence of molar (Left) 0.89 0.18 -0.6 0.55 0.60 1.31
Figure 1. The CT images from the axial plane (A and C) and from the sagittal plane (B and D) - The presence of septum is determined by the observation of the complete compartments divided by bony structure on the axial view, and the finding of a crest- and ridge-like bony structure in the related position on subsequent sagittal views. (Yellow arrows indicate an anterior septum; white arrows indicate a posterior septum) From axial images, these two septa both showed transverse (bucco-palatally)
direction, connecting the lateral and medial walls of the maxillary sinus.