Elsevier Editorial System(tm) for Archives of Physical Medicine and Rehabilitation Manuscript Draft
Manuscript Number: ARCHIVES-PMR-D-10-00494R1
Title: Kinematic features of rear-foot motion using anterior and posterior AFOs in stroke patients with hemiplegic gait
Article Type: Original Article
Keywords: Orthotic Devices; Stroke; Biomechanics; Gait Corresponding Author: Dr. Simon F.T. Tang,
Corresponding Author's Institution: First Author: Chih-Chi Chen
Order of Authors: Chih-Chi Chen; Wei-Hsien Hong; Chin-Man Wang; Chih-Kuang Chen; Katie Pei-Hsuan Wu; Chao-Fu Kang; Simon F.T. Tang
Abstract: Title: Kinematic features of rear-foot motion using anterior and posterior AFOs in stroke patients with hemiplegic gait
Running head: A-AFO and P-AFO use in hemiplegic gait Key Words: Orthotic devices, Stroke, Biomechanics, Gait.
Objective: To evaluate the kinematic features of rear-foot motion during gait in hemiplegic stroke patients, using anterior ankle foot orthoses (A-AFOs), posterior AFOs (P-AFOs), and no orthotic assistance.
Design: Crossover design with randomization for the interventions. Setting: A rehabilitation centre for adults with neurological disorders.
Participants: Fourteen patients with hemiplegia due to stroke and eleven able-bodied subjects. Interventions: Subjects with hemiplegia were measured walking under 3 conditions with randomized sequences: (1) with an A-AFO, (2) with a P-AFO, and (3) without an AFO. Control subjects were measured walking without AFO to provide a normative reference.
Main Outcome Measures: Rear-foot kinematic change in the sagittal, coronal, and transverse planes. Results: In the sagittal plane, as compared to walking with an A-AFO or without an AFO, the P-AFO significantly decreased plantarflexion to neutral at initial heel contact (P = 0.001) and the swing phase (P < 0.001), and increased dorsiflexion at the stance phase (P = 0.002). In the coronal plane, the A-AFO significantly increased maximal eversion to neutral (less inversion) at the stance phase (P = 0.025), and decreased the maximal inversion angle at the swing phase when compared with using no AFO (P = 0.005). The P-AFO also decreased the maximal inversion angle at the swing phase as compared to no
AFO (P = 0.005). In the transverse plane, when compared with walking without an AFO, the A-AFO and P-AFO decreased the adduction angle significantly at initial heel contact (P = 0.004).
Conclusions: For post-stroke hemiplegic gait, the P-AFO was better than the A-AFO in enhancing rear-foot dorsiflexion during the whole gait cycle. The A-AFO was superior to the P-AFO in correcting excessive rear-foot inversion at the stance phase. Both the A-AFOs and P-AFOs helped correct an inverted foot at the swing phase.
Dear Dr. Rodgers,
Thank you for your email telling me that the Editorial Board sees merit in my manuscript. Also I would like to thank Archives of PMR for finding two such outstanding and reasonable reviewers for me. Comments from the two reviewers were indeed very helpful. Revising the manuscript according to the comments from reviewers certainly made the manuscript more presentable.
We revised the manuscript as suggestion and focused on the areas as you pointed out, 1. Clarify comparison of kinematic variables between conditions, 2. Provide additional information about subjects and 3. Provide more description of the A-AFO.
The manuscript has been read by a native English speaker and edited for grammar errors. I hope you and the reviewers will like the revisions I have done. It will certainly be my greatest honor if this manuscript can be published in the renowned Archives of PMR.
Enclosed below you will find our replies to both reviews. We also made detailed comparison lists before and after revision for reviewers to easily review. Please allow us let one of our members as co-authors (Chao-Fu Kang, MD) because he helped a lot in revised this manuscript.
Thank you again. Please feel free to contact me at anytime if I can be of any further assistance. Take care!
Simon FT Tang
Professor and Program Director
Department of Physical Medicine and Rehabilitation, Chang Gung Memorial Hospital
5, Fu-Hsin ST., Kwei-Shan, Tao-Yuan County, 333, Taiwan Cover Letter
1 Replies to Reviewer 1
As suggested by reviewer 1, we have checked all manuscript, clarified the comparisons
and modulate those confusing statements.
Methods: We have added a more detailed description about the A-AFO. We have also
corrected the typing errors about the P-AFO. We also added a description to explain why we
let subjects walking barefoot with AFO.
Results: A table is now constructed as suggested. The table clearly provides information
on the sex, age, time since stroke, involved side, Brunnstrom stage, muscle tone, use of
assistive device, and prior AFO use.
A detailed comparison list before and after revision for reviewer 1 is listed in the following
page.
2 Comparison List for Reviewer 1
Suggestion 1:
The comparison of kinematic variables between conditions often is not clear. Often times, the variable is described as "increased" or decreased" , but it is not clear what the value is being compared to. Examples are: page 7, line114-115; 116-117; 119; p8 129-130, and abstract. These are specific examples but the authors should check and clarify all comparisons.
Reply: We have checked all manuscript and clarify the comparison as following:
Before Revision After revision
Abstract Results
At initial heel contact, the rear-foot showed increased dorsiflexion while wearing P-AFOs (P=0.001). During the stance phase, wearing the P-AFO increased the dorsiflexion angle more significantly than wearing the A-AFO or nothing (P=0.002). The A-AFO lessened inversion and increased the maximal eversion angle (P=0.025). During the swing phase, decreased maximal plantarflexion and an increased dorsiflexion angle were noted only wearing the P-AFO (P<0.001). With both the A-AFO and P-AFO, the inversion angle was significantly decreased as compared to wearing nothing (P=0.005).
Conclusions
A-AFOs were superior in correcting excessive rear-foot inversion, while P-AFOs had the advantage in enhancing rear-foot dorsiflexion. P-AFOs also helped correct an inverted foot at the swing phase.
Abstract Results
In the sagittal plane, as compared to walking with an A-AFO or without an AFO, the P-AFO significantly decreased plantarflexion to neutral at initial heel contact (P = 0.001) and the swing phase (P < 0.001), and increased dorsiflexion at the stance phase (P = 0.002). In the coronal plane, the A-AFO significantly increased maximal eversion to neutral (less inversion) at the stance phase (P = 0.025), and decreased the maximal inversion angle at the swing phase when compared with using no AFO (P = 0.005). The P-AFO also decreased the maximal inversion angle at the swing phase as compared to no AFO (P = 0.005). In the transverse plane, when compared with walking without an AFO, the A-AFO and P-AFO decreased the adduction angle significantly at initial heel contact (P = 0.004).
3
Before Revision After revision
Abstract-Conclusions
A-AFOs were superior in correcting excessive rear-foot inversion, while P-AFOs had the advantage in enhancing rear-foot dorsiflexion. P-AFOs also helped correct an inverted foot at the swing phase.
Abstract-Conclusions
For post-stroke hemiplegic gait, the P-AFO was better than the A-AFO in enhancing rear-foot dorsiflexion during the whole gait cycle. The A-AFO was superior to the P-AFO in correcting excessive rear-foot inversion at the stance phase. Both the A-AFOs and P-AFOs helped correct an inverted foot at the swing phase.
4
Before Revision After revision
Results (Page 7, line 114-119)
At initial heel contact, the rear-foot showed increased dorsiflexion while wearing P-AFOs. The subjects showed a trend in decreasing the inversion rear-foot angle after wearing A-AFOs, but it was not significant (P=0.064). Wearing the A-AFO and the P-AFO decreased the adduction angle significantly. During the stance phase, wearing the P-AFO increased the dorsiflexion angle more significantly than wearing the A-AFO or nothing. The A-AFO lessened inversion and increased the maximal eversion angle. There was no significant difference in the maximal abduction angle in any of the AFO trials. During the swing phase, decreased maximal plantarflexion and an increased dorsiflexion angle were noted only wearing the P-AFO. With both the A-AFO and P-AFO, the inversion angle was significantly decreased as compared to wearing nothing. No significant difference could be seen in the abduction and adduction angles with or without the A-AFO or P-AFO.
Results (page 8, line 136-146)
In the sagittal plane, as compared to walking with an A-AFO or without an AFO, the P-AFO significantly decreased plantarflexion to neutral at initial heel contact and the swing phase and increased dorsiflexion at the stance phase. In the coronal plane, the A-AFO significantly increased maximal eversion to neutral (less inversion) at the stance phase and decreased the maximal inversion angle at the swing phase when compared with not using an AFO. The P-AFO also decreased the maximal inversion angle at the swing phase when compared with not using an AFO. In the transverse plane, as compared to walking without an AFO, the A-AFO and P-AFO conditions decreased the adduction angle significantly at initial heel contact. There were no significant differences in maximal adduction and the maximal abduction angles among the three AFO conditions during the stance and swing phases respectively.
5
Before Revision After revision
Discussion (p8 125-131)
Our aim in this study was to assess the kinematic characteristics of rear-foot joint change during gait in hemiplegic stroke patients using A-AFOs, P-AFOs, and no orthotic assistance. Previously, the choice of anterior or posterior AFO was often based on the practitioner’s experience and the patients’ preference. In both the stance and the swing phases, our results showed that A-AFOs were superior in correcting excessive rear-foot inversion, while P-AFOs had the advantage in enhancing rear-foot dorsiflexion. P-AFOs also helped correct an inverted foot at the swing phase.
Discussion ( p9 148-158)
The incidence of equinovarus foot in stabilized vascular hemiplegia was reported to be about 18%.17 The equinovarus foot shifts weight bearing from the heel to the lateral plantar surface, which can cause loss of balance and reduce walking safety. This condition also has a strong correlation to the presence of claw toes.18, 19 An AFO has often been prescribed to facilitate ankle control for the equinus and/or varus foot. This study investigated the kinematic change in rear-foot joint control during gait in hemiplegic stroke patients using A-AFOs, P-AFOs, and no AFO assistance. As compared to using no AFO, the A-AFO decreased rear-foot inversion at the stance and swing phases. The P-AFO increased rear-foot dorsiflexion during the whole gait cycle in comparison with the A-AFO and P-AFO. The P-AFO also decreased rear-foot inversion at the swing phase as compared to using no AFO.
6 Suggestion 2:
In addition, in some locations, the comparison of the A-AFO to other conditions seems misleading. For example, the paper reads, 'our results showed that the A-AFOs were superior in correcting excessive rear foot inversion." (129-130; 171), but elsewhere (lines 134-136) the text indicates there were no differences in gait parameters between the brace conditions after statistical analysis.
Reply: We have clarified the comparison and modulate these confusing statements.
Before revision After revision
Discussion (line 134-136)
After wearing either A-AFOs or P-AFOs, we noted no significant difference in the gait parameters after statistical analysis.
Discussion (p10 line 161-162)
After wearing either A-AFOs or P-AFOs, we noted no significant difference in walking speed, step length and cycle time after statistical analysis.
Suggestion 3.
The paper correctly states in several locations that brace selection will be dependent upon the patient's motor control and gait patterns (i.e., line 198). However, the study does not adequately describe the clinical characteristics of the people with a history of stroke to allow interpretation of the results. The authors should provide additional information about subjects; for example, severity of deficits (some type of standardized measure), tone, use of assistive device, and prior AFO use.
Reply:
7 Suggestion 4, The A-AFO will not be familiar to many readers, and although it has been described elsewhere in the literature, it should be described in greater detail here; ie, specific anatomical boundaries of trim line, rationale for design.
Reply: We have added a more detailed description about the A-AFO.
Before revision After revision
Method
Nil (not mentioned before revision)
Method (p4 48-58)
The A-AFO was made of a low temperature 3.2 mm thick thermoplastic material, Orfit.a A piece of thermoplastic was cut in the shape of a bottle cap opener (fig 1). The pretibial and ankle parts were padded with closed-cell foam, Kushionflex padding.b Subjects were asked to sit with their knee in a 90 degree flexion and their ankle in a neutral position. After softening the thermoplastic in a hot water tank (60°C), the anterior AFO was molded directly to the subject’s lower limb, with her or his foot going through the hole in the bottle cap opener section. The sole part was 6 cm in width, with its anterior trim line just behind the metatarsal heads. The foot and ankle portions were folded to form the medial and lateral bars. The upper part was molded onto the ankle and lower half of the tibia without covering the medial and lateral malleoli. Velcro strapsc were placed at the ankle level and upper part of the orthosis (see fig 2). Usually, we can make an A-AFO within half an hour.
8 Suggestion 5, The paper states that P-AFO trim lines were anterior to both malleoli (line 55), but such a trim line seems quite restrictive and different from Fig 1. Please clarify.
Reply: We have corrected the typing errors and added more description about the P-AFO.
Before revision After revision
Method (p4 52-55)
The AFO extended distally under the toes and covered the mediolateral border of the foot. Proximally, it covered the posterior portion of the leg to 5 cm below the fibular head. The trim lines were anterior to both malleoli. Three straps crossed the anterior upper tibia, front of the ankle, and the mid-foot area (See fig 1).
Method (p4 59-67)
We used leaf-spring AFO in comparison with A-AFO not only because it is commonly used in clinical situations but it dose not cover malleoli, which is similar to the A-AFO. Each P-AFO was fabricated using polypropylene with the ankle in a neutral position. The footplate was cut to the metatarsal head. Proximally, it covered the posterior portion of the leg to 5 cm below the fibular head. The medial and lateral trim lines over the ankle were posterior to both malleoli. Three straps crossed the proximal end of shank, the front of the ankle, and the mid-foot area (see fig 2). We used three straps to hold the P-AFO instead of standard single strap at the upper shank because we let subjects walk barefoot with P-AFO without shoes assistance.
9 Suggestion 6, Why did subjects walk barefoot with P-AFO? In America, walking barefoot with a P-AFO would be very unusual.
Reply: We added a description to explain why we let subjects walking barefoot with P-AFO.
Before revision After revision
Nil (not mentioned before revision) Method. ( P5 68-70)
The decision to analyze subjects walking barefoot with AFOs was based upon: (1) our need to know the real function of the AFO without the assistance of a shoe; and, (2) our interest in conforming to the custom in Asia countries of walking barefoot indoors.
10 Replies to Reviewer 2
Introduction: As suggested by reviewer 2, we have added the suggested references to
expose the interest of AFOS.
Methods: We made a hole at P-AFO to allow calcaneal marker directly placed on the skin.
Thank you for reminding us to add the important description. We also added pictures to
clarify the marker position.
Results: We have corrected the typing error in table 3.
Discussions: Thank you for your kindly suggestion. We have added the references and a
discussion of risk of walking with equinovarus foot as your suggestion.
A detailed comparison list before and after revision for reviewer 2 is listed in the following
page.
11 Comparison List for Reviewer 2
Reviewer 2 Suggestion 1. Introduction:
Previous pertinent literature: page2, line15 to 24: The following article is missing in the references to expose the interest of AFOS: Ann Readapt Med Phys. 2008 Apr;51(3):147-53. Epub 2008 Jan 7.[Assessment of the Chignon dynamic ankle-foot orthosis using instrumented gait analysis in hemiparetic adults]. Bleyenheuft C, Caty G, Lejeune T, Detrembleur C.
Reply: We have added the suggested references to expose the interest of AFOS.
Before revision After revision
Introduction (P2 19-22)
Several studies evaluated the effects of posterior AFOs (P-AFOs) on stroke patients and demonstrated improvement in gait parameters including stride length, gait velocity and cadence,4-6 gait stability,4 balance control,7 energy cost of walking,8 and functional status.5
Introduction (P2 19-22)
Several studies evaluated the effects of P-AFOs on stroke patients and demonstrated improvement in gait parameters including stride length, gait velocity and cadence,4-6 gait stability,4 balance control,7 energy cost of walking,8, 9 and functional status.5
Reference
9.Bleyenheuft C, Caty G, Lejeune T, Detrembleur C. Assessment of the Chignon dynamic ankle-foot orthosis using instrumented gait analysis in hemiparetic adults. Ann Readapt Med Phys 2008;51(3):154-60.
12 Suggestion 2.
Methods : p5 line 63-65. it seems the posterior marker is placed on the p-AFO. In this condition, are the authors sure that the kinematic data show the mobility of the foot rather the mobility of the P-AFO. Please discuss this point.
Reply:
We made a hole at P-AFO to allow calcaneal marker directly placed on the skin. We have added the picture and statement in the methods.
Before revision After revision
Method –Equipment (p5 62-64)
A marker was placed on the midline of the calcaneal posterior process, and, with the subject standing, individual markers were also placed on the medial and lateral sides of the calcaneus in a plane parallel to the ground (fig 2).
Method –Equipment (p5 80-81)
We made one hole in each P-AFO to allow placement of the calcaneal markers directly onto the skin (fig 2).
13 Suggestion 3.
P7 line 111 : the authors wrote that the stroke patients showed less maximal plantarflexion than the healthy control group, but the table 3 does not show that. Is there an error in the table 3?
14 Suggestion 4. Discussion: P8 line126-132 : Since the main result is the importance of the varus-foot stabilization with A-AFO it could be interesting to discuss the incidence of varus equinus and value its consequences on gait (see references below): Claw toes in hemiplegic patients after stroke.Laurent G, Valentini F, Loiseau K, Hennebelle D, Robain G.Ann Phys Rehabil Med. 2010 Mar;53(2):77-85. Epub 2010 Jan 13. English, French. PMID: 20097630 [PubMed - indexed for MEDLINE]
Epidemiology of pes varus and/or equinus one year after a first cerebral hemisphere stroke: apropos of a cohort of 86 patients] Verdié C, Daviet JC, Borie MJ, Popielarz S, Munoz M, Salle JY, Rebeyrotte I, Dudognon P. Ann Readapt Med Phys. 2004 Mar;47(2):81-6.
Reply: We have added the references and a discussion of risk of walking with equinovarus foot.
Before revision After revision
Discussion (p8 126-132)
Nil (not mentioned before revision)
Discussion (p9 148-151)
The incidence of equinovarus foot in stabilized vascular hemiplegia was reported to be about 18%.17 The equinovarus foot shifts weight bearing from the heel to the lateral plantar surface, which can cause loss of balance and reduce walking safety. This condition also has a strong correlation to the presence of claw toes.18, 19
Reference
17. Verdie C, Daviet JC, Borie MJ, Popielarz S, Munoz M, Salle JY et al. [Epidemiology of pes varus and/or equinus one year after a first cerebral hemisphere stroke: apropos of a cohort of 86 patients]. Ann Readapt Med Phys 2004;47(2):81-6. 19. Laurent G, Valentini F, Loiseau K, Hennebelle D, Robain G. Claw toes in hemiplegic patients after stroke. Ann Phys Rehabil Med 2010;53(2):77-85.
15 Suggestion 5. Moreover, since the A-AFO is superior in correcting excessive rear-foot inversion, a discussion of risk of walking with a varus-equinus foot could be interesting.
Reply:
Besides the discussion of altered rear-foot kinematics in hemiplegic gait and its consequences in altered gait pattern (p11 181-184). We have added a discussion of risk of walking with equinovarus foot as your suggestion.
Before revision After revision
Nil (not mentioned before revision) Discussion (p9 149-151)
The equinovarus foot shifts weight bearing from the heel to the lateral plantar surface, which can cause loss of balance and reduce walking safety. This condition also has a strong correlation to the presence of claw toes.18, 19
1 Word counts for the main text: 2969, Word counts for Abstract: 333.
1
Title: Kinematic features of rear-foot motion using anterior and posterior AFOs in 2
stroke patients with hemiplegic gait 3
Names and affiliations of the authors: Chih-Chi Chen, MD1, Wei-Hsien Hong, PHD2, 4
Chin-Man Wang MD1,Chih-Kuang Chen, MD1, Katie Pei-Hsuan Wu, MD1 , Chao-Fu Kang, 5
MD1 & Simon F.T. Tang, MD1 6
From the 1. Department of Physical Medicine and Rehabilitation, Chang Gung Memorial 7
Hospital and Chang Gung University, Linkou and 2. School of Sports Medicine, China 8
Medical University, Taichung, Taiwan 9
Running head: A-AFO and P-AFO use in hemiplegic gait 10
Grant & Financial Support: National Science Council, Republic of China (Grant No. NSC 11
98-2119-M-009-019). 12
Financial Disclosure: We certify that no party having a direct interest in the results of the 13
research supporting this article has or will confer a benefit on us or on any organization with 14
which we are associated AND, if applicable, we certify that all financial and material 15
support for this research (eg, NIH or NHS grants) and work are clearly identified in the title 16
page of the manuscript. 17
Corresponding author: 18
Professor Simon F.T. Tang, MD 19
2 Department of Physical Medicine & Rehabilitation
20
Chang Gung Memorial Hospital & Chang Gung University Taoyuan, Taiwan 21
5, Fu-Hsin St, Kwei-Shan, Tao-Yuan, 333, Taiwan 22 Tel: +886-3-328-1200 ext. 3846 23 Fax:+886-3-327-4850 24 E-mail: fttang@adm.cgmh.org.tw 25 bluegirl5477@yahoo.com.tw 26
1 Title: Kinematic features of rear-foot motion using anterior and posterior AFOs in 1
stroke patients with hemiplegic gait 2
Running head: A-AFO and P-AFO use in hemiplegic gait 3
Key words: Orthotic Devices, Stroke, Biomechanics, Gait. 4
5
2 Introduction
6
Stroke patients often have upper motor neuron syndrome with a resultant loss of strength 7
and dexterity, impaired motor control, increased spasticity, hyperreflexia, co-contraction, 8
and spastic dystonia in the affected limbs. These conditions result in inappropriate and 9
involuntary posturing and contribute to abnormal gait pattern and impaired walking ability.1 10
Clinically, we can identify more than one type of gait pattern across stroke patients, such as 11
the equinus and equinovarus gaits, indicating that people who have suffered strokes need to 12
use different strategies to achieve the goal of walking.2 13
AFOs are often prescribed to stroke patients and are designed to provide mediolateral 14
ankle stability during stance and adequate toe clearance during swing and to promote heel 15
strike.3 Conventional plastic AFOs have a posterior leaf-type design, and are fabricated by a 16
lamination or vacuum-forming technique over a positive plaster model of the limb.4 17
A-AFOs are low-temperature ankle foot orthoses commonly used in Asian countries for 18
convenience when walking indoors. Several studies evaluated the effects of P-AFOs on 19
stroke patients and demonstrated improvement in gait parameters including stride length, 20
gait velocity and cadence,4-6 gait stability,4 balance control,7 energy cost of walking,8, 9 and 21
functional status.5 Some studies evaluated the A-AFO function and suggested that A-AFOs 22
also work effectively for gait parameters,10 walking ability,11 and balance control12 in 23
hemiplegic stroke patients. 24
3 Since ankle motor control in stroke patients is variable, and the designs of A-AFOs and 25
P-AFOs are different, we speculated that different post-stroke gait patterns could benefit 26
from different AFO types. We analyzed the shank-calcaneus rotation angle, as 27
representative of rear-foot movement, by means of a 3-dimensional motion analysis 28
system.13 To our knowledge, this is the first study to compare the kinematic changes in 29
rear-foot movement during gait in hemiplegic stroke patients using either A-AFOs or 30 P-AFOs. 31 Methods 32 Subjects 33
For this study, we recruited 14 stroke subjects with hemiplegia. The inclusion criteria for 34
the study group were as follows: (1) diagnosis of unilateral hemiplegia caused by either 35
hemorrhagic or ischemic stroke; (2) ability to follow simple verbal commands or 36
instructions; and, (3) ability to ambulate independently. Subjects were excluded if they had 37
any of the following conditions: (1) medical problems other than stroke that would interfere 38
with their gait; or, (2) foot-related premorbid or comorbid orthopedic problems. All patients 39
underwent neuroimaging studies, including computed tomography or magnetic resonance 40
imaging of the brain to confirm the diagnosis of stroke at an early stage. We also recruited 41
11 normal subjects, who had no known neurological and orthopedic impairments, to serve 42
as our control group. This study was approved by the local medical ethics and the human 43
4 clinical trial committees (Chang Gung Memorial Hospital, Taiwan), and all participants 44
signed the informed consent. 45
AFO design 46
A-AFOs and P-AFOs for the study were custom-made for each subject by a certified 47
orthotist. Fabrication of an anterior AFO was well documented in our previous study.11 The 48
A-AFO was made of a low temperature 3.2 mm thick thermoplastic material, Orfit.a A 49
piece of thermoplastic was cut in the shape of a bottle cap opener (fig 1). The pretibial and 50
ankle parts were padded with closed-cell foam, Kushionflex padding.b Subjects were asked 51
to sit with their knee in a 90 degree flexion and their ankle in a neutral position. After 52
softening the thermoplastic in a hot water tank (60°C), the anterior AFO was molded 53
directly to the subject’s lower limb, with her or his foot going through the hole in the bottle 54
cap opener section. The sole part was 6 cm in width, with its anterior trim line just behind 55
the metatarsal heads. The foot and ankle portions were folded to form the medial and lateral 56
bars. The upper part was molded onto the ankle and lower half of the tibia without covering 57
the medial and lateral malleoli. Velcro strapsc were placed at the ankle level and upper part 58
of the orthosis (see fig 2). Usually, we can make an A-AFO within half an hour. 59
The P-AFO used in this study was the plastic leaf-spring AFO14. We used leaf-spring 60
AFO in comparison with A-AFO not only because it is commonly used in clinical situations 61
but it dose not cover malleoli, which is similar to the A-AFO. Each P-AFO was fabricated 62
5 using polypropylene with the ankle in a neutral position. The footplate was cut to the 63
metatarsal head. Proximally, it covered the posterior portion of the leg to 5 cm below the 64
fibular head. The medial and lateral trim lines over the ankle were posterior to both malleoli. 65
Three straps crossed the proximal end of shank, the front of the ankle, and the mid-foot area 66
(see fig 2). We used three straps to hold the P-AFO instead of standard single strap at the 67
upper shank because we let subjects walk barefoot with P-AFO without shoes assistance. 68
The decision to analyze subjects walking barefoot with AFOs was based upon: (1) our need 69
to know the real function of the AFO without the assistance of a shoe; and, (2) our interest 70
in conforming to the custom in Asia countries of walking barefoot indoors. 71
Equipment 72
A Vicon motion analysis systemc was used to collect the kinematic data. The Vicon MS 73
system included 8 infrared cameras for acquiring, at a rate of 100Hz, the kinematic 74
trajectories of the reflective markers attached to the subject’s lower limbs. We placed 7 75
spherical retro-reflective markers (diameter 1.4 cm) directly on the subject’s affected-side 76
calcaneus and shank. Two markers were placed on the medial and lateral tibial condyles, 77
and 2 markers were also placed on the medial and lateral malleoli. A marker was placed on 78
the midline of the calcaneal posterior process, and, with the subject standing, individual 79
markers were also placed on the medial and lateral sides of the calcaneus in a plane parallel 80
to the ground. We made one hole in each P-AFO to allow placement of the calcaneal 81
6 markers directly onto the skin (fig 2). Three-dimensional marker trajectories were used to 82
determine the rear-foot motion angles in the sagittal (dorsiflexion–plantarflexion), coronal 83
(inversion–eversion), and transverse (abduction–adduction) planes. 84
Data collection 85
We evaluated and recorded stroke participants’ motor recovery and ankle muscle tone 86
using a Brunnstrom stage15 and modified Ashworth Scale (MAS),16 respectively. All 87
subjects practiced walking with and without the orthosis before we performed the gait 88
analysis. Each subject was asked to stand still for one second to allow all of the cameras to 89
record the markers to analyze the subject’s initial anatomical position. Each subject was 90
then measured walking at a self-selected, comfortable speed in each of three orthotic trials 91
(barefoot without an AFO, with a P-AFO, and with an A-AFO) during the same session. 92
The order of the three trials was randomized. Subjects were allowed to rest for 5 minutes 93
between trials. The walkway was carpeted to avoid any discomfort when the subjects 94
walked barefoot without an AFO. To reduce measurement errors during gait analysis, data 95
were collected from three successful trials. The data from these three trials were averaged 96
and the results were used for the statistical analysis. 97
Data analysis 98
A LabView software packaged was designed to analyze rear-foot motion. A joint 99
coordinate system examined the relative rotation matrices of the marker reference frames 100
7 on the calcaneus with respect to those on the shank. The neutral position was defined as the 101
standing position. The calculated rotation matrices in the neutral position were used to 102
correct the joint. Euler angles were used to define the three-dimensional relative joint 103
angular motion. From this neutral position, the distal segment was assumed to move 104
through three successive finite rotations to attain its new configuration. The first rotation 105
was dorsiflexion–plantarflexion about the z-axis of the proximal segment, followed by 106
inversion–eversion about a rotated floating x-axis. Finally, the third rotation was the 107
abduction–adduction rotation about the distal to proximal direction (y-axis) of the distal 108
segment. The temporal and spatial gait parameters were computed, including walking speed, 109
step length, cycle time, and angles of the rear-foot joint. 110
Statistical Analysis 111
We used SPSS version 12 softwaree for the statistical analysis. Group differences in age, 112
body height, and body mass were compared using an independent t-test. Gender differences 113
between the groups were determined using a χ2 test. The gait parameters were compared 114
using repeated measures analysis of variance (ANOVA) to determine significant differences 115
among the AFOs and groups. Post hoc Bonferroni tests were used to evaluate the 116
significance of pairwise comparisons between the AFOs. The level of significance used was 117
P < 0.05.
118
Results 119
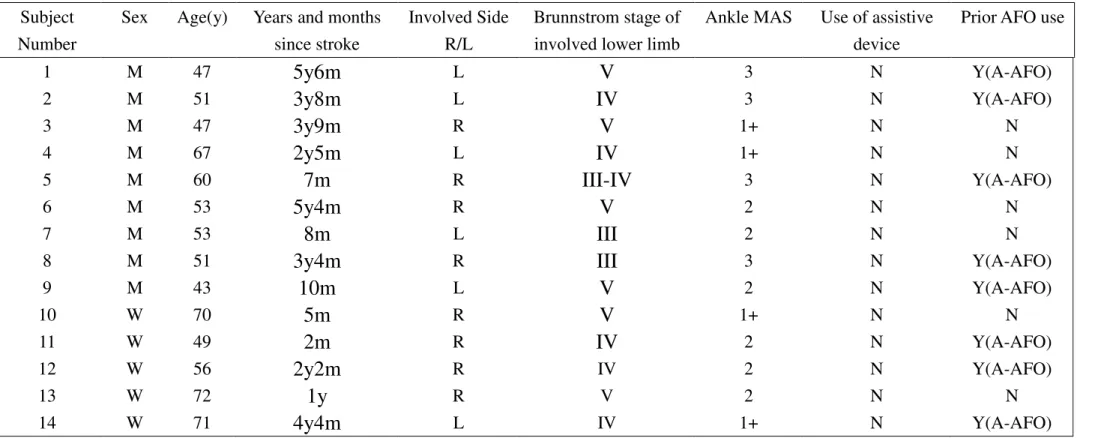
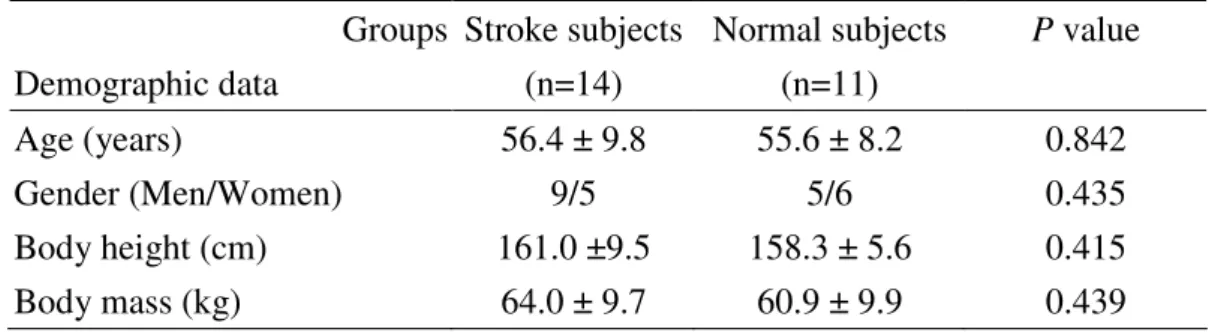
8 Descriptive information regarding the 14 participants with hemiplegia is listed in table 1. 120
Comparisons of demographic data, including age, gender, body height, and body weight 121
between the stroke and normative subjects are listed in table 2. The hemiplegic stroke 122
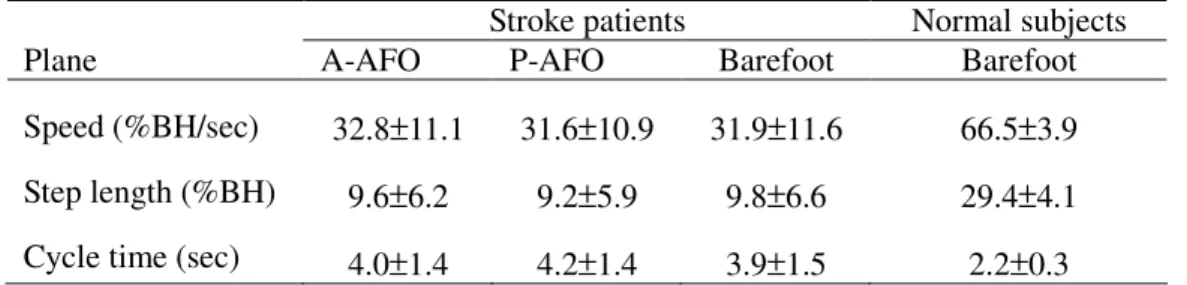
subjects walked at a significantly slower, self-selected, comfortable walking speed, had 123
decreased step length, and longer cycle times than the control group. When comparing the 124
A-AFO, P-AFO, and barefoot conditions in the hemiplegic stroke subjects, there was no 125
significant difference in the self-selected, comfortable walking speeds, step lengths, and 126
cycle times (see table 3). 127
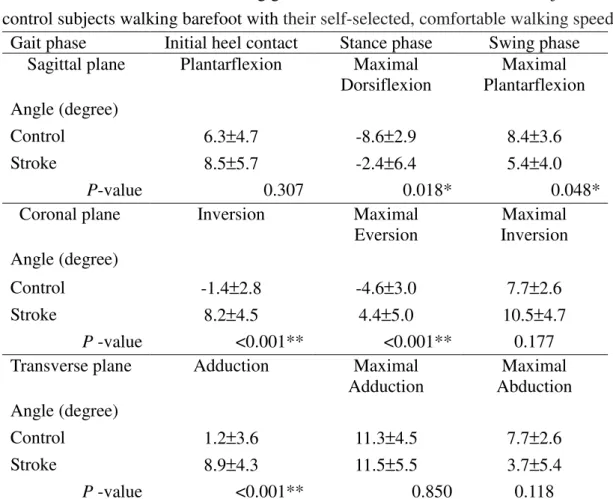
Rear-foot kinematic changes during gait in both the stroke and normal subjects when 128
barefoot are shown in table 4 and figure 3. At initial heel contact, the rear-foot movement 129
of the stroke patients showed increased inversion and adduction in comparison with the 130
healthy control subjects. During the stance phase, the stroke patients showed less 131
dorsiflexion and more inversion in the rear-foot angle. During the swing phase, the 132
rear-foot of the stroke patients showed less maximal plantarflexion and less dorsiflexion 133
than the healthy control group. Actually, they all showed the gait pattern as equinovarus 134
gait. 135
Comparisons of the rear-foot angular motions in hemiplegic stroke subjects in the 136
A-AFO, P-AFO, and without AFO conditions are shown in figures 3 and 4. In the sagittal 137
plane, as compared to walking with an A-AFO or without an AFO, the P-AFO significantly 138
9 decreased plantarflexion to neutral at initial heel contact and the swing phase and increased 139
dorsiflexion at the stance phase. In the coronal plane, the A-AFO significantly increased 140
maximal eversion to neutral (less inversion) at the stance phase and decreased the maximal 141
inversion angle at the swing phase when compared with not using an AFO. The P-AFO also 142
decreased the maximal inversion angle at the swing phase when compared with not using 143
an AFO. In the transverse plane, as compared to walking without an AFO, the A-AFO and 144
P-AFO conditions decreased the adduction angle significantly at initial heel contact. There 145
were no significant differences in maximal adduction and the maximal abduction angles 146
among the three AFO conditions during the stance and swing phases respectively. 147
Discussion 148
The incidence of equinovarus foot in stabilized vascular hemiplegia was reported to be 149
about 18%.17 The equinovarus foot shifts weight bearing from the heel to the lateral plantar 150
surface, which can cause loss of balance and reduce walking safety. This condition also has 151
a strong correlation to the presence of claw toes.18, 19 An AFO has often been prescribed to 152
facilitate ankle control for the equinus and/or varus foot. This study investigated the 153
kinematic change in rear-foot joint control during gait in hemiplegic stroke patients using 154
A-AFOs, P-AFOs, and no AFO assistance. As compared to using no AFO, the A-AFO 155
decreased rear-foot inversion at the stance and swing phases. The P-AFO increased 156
rear-foot dorsiflexion during the whole gait cycle in comparison with the A-AFO and 157
10 P-AFO. The P-AFO also decreased rear-foot inversion at the swing phase as compared to 158
using no AFO. 159
In comparison with the normal controls in our study, the stroke subjects showed 160
significantly decreased gait parameters including walking speed, step length, and cycle time. 161
After wearing either the A-AFOs or P-AFOs, we noted no significant differences in the 162
walking speed, step lengths, and cycle times after statistical analysis. Such results were not 163
compatible with the previously mentioned studies,4-6 but were similar to other studies.1, 20, 21 164
The relatively small number of cases, variable improvement in patients’ wearing different 165
types of AFO, (improvement in gait speed when wearing A-AFOs as opposed to decreases 166
in gait speed when wearing P-AFOs or vice versa), may explain the insignificant statistical 167
results. According to the study of Perry et al, a difference of 20 cm/s in walking speed was 168
defined as clinically significant.22 Even though some studies showed an improvement in 169
gait speed in stroke patients after wearing AFOs, most of the improvements were too small 170
to reach clinical significance.5 171
In healthy subjects, the rear-foot tended to plantarflex at initial heel contact, and then 172
dorsiflex during the stance phase and mid-swing phase in the sagittal plane. In the coronal 173
plane, the rear-foot inverted at initial heel contact and then everted until terminal stance 174
when it inverted. These findings are compatible with previous studies.12,15 W. Liu et al 175
evaluated rear-foot kinematic changes in healthy subjects and found that repeatable patterns 176
11 between subjects can be observed in dorsiflexion/plantarflexion and inversion/eversion, 177
suggesting that these characteristic changes are essential for efficient level walking. The 178
inconsistent kinematic changes in the abduction/adduction angle between the studies may 179
be explained by the angle’s secondary importance to level walking. Each individual may 180
adopts his/her own strategy and his/her specific motion characteristics.23 181
We noted that hemiplegic stroke subjects have altered rear-foot kinematics during gait, 182
such as rear-foot inversion and adduction at initial heel contact. It has been suggested that 183
foot eversion during the stance phase provides shock absorption on floor impact.24 184
Increased rear-foot inversion at initial heel contact only offers shock absorption from the 185
toe and lateral border of the foot, but increases the stress on the contact area.25 During the 186
stance phase, rear-foot control in the hemiplegic stroke patients became more plantarflexed 187
and still inverted. This plantarflexion and rear-foot inversion may interfere with adequate 188
pushing motion generation during propulsion.26 During the swing phase of stroke subjects, 189
the rear-foot remained in the plantarflexion position and could not accomplish dorsiflexion 190
well. Inadequate dorsiflexion may interfere with foot clearance. Perry found that the 191
hemiplegic stroke patients had inadequate shock absorption at heel strike, poor control of 192
momentum during stance, and inadequate excursion of the paretic limb during swing.27 Our 193
study suggests that these observations may be explained by the abnormal kinematic 194
changes in rear-foot control in our stroke patients. 195
12 After hemiplegic stroke subjects wore the two types of AFOs, their rear-foot control at 196
initial heel contact was in a more dorsiflexed position with P-AFOs as compared to the 197
A-AFOs and no AFO, and was less adducted with both the A-AFOs and P-AFOs when 198
compared to using no AFO. During the stance phase, the P-AFO increased the dorsiflexion 199
angle when compared with the A-AFO and no AFO, while the A-AFO corrected an inverted 200
rear-foot more effectively when compared with not using an AFO. At the swing phase, the 201
P-AFO kept the rear-foot in the dorsiflexion position in comparison with the A-AFO and no 202
AFO, and both the A-AFO and P-AFO decreased the inverted angle as compared to using 203
no AFO. The kinematic findings for the P-AFO in the sagittal plane were compatible with 204
Stefania Fatone et al’s study, which showed that all patients tested with P-AFOs with 205
different AFO alignments and foot-plate lengths were able to decrease their plantar flexion 206
of the ankle at initial contact and mid-swing.1 Our study also suggested that the A-AFOs 207
had a greater effect on inverted rear-foot control than the P-AFOs and going barefoot, 208
especially in the stance phase. 209
We speculated that the different effects of AFO type on the rear-foot kinematic change 210
may relate to the design differences. The P-AFO, with its sole extending the length from 211
heel to sulcus and posterior reinforcement to stiffen its plantar flexion resistance feature, 212
may prevent ankle plantarflexion effectively. Their medial and lateral trim lines posterior to 213
both malleoli allowed sufficient flexibility and helped dorsiflexion effectively but helped 214
13 less in controlling inverted ankle. The A-AFO, with its small sole band just under the 215
metatarsal and lack of posterior reinforcement, may have limited its ability to prevent 216
plantarflexion. However, its continuous coverage from the metatarsal and tarsal to shank 217
may fix the subtalar joint and prevent rear-foot inversion more effectively. Although the 218
rear-foot kinematics after AFO correction were still different from those of the normal 219
subjects, the A-AFOs and P-AFOs did play a role in correcting and normalizing the 220
rear-foot angle of hemiplegic subjects after statistical analysis. Such change may contribute 221
to the functional improvement noted in previously mentioned studies in gait stability, 222
balance control, energy cost, and patients’ function. Other integrated strategies are still 223
needed to improve stroke patients’ gait pattern.28
224
There are some limitations in this study. First, a relatively small number of cases were 225
recruited for this study. Second, the healthy control group did not walk as slowly as the 226
stroke subjects, given that forcing such a slow speed on a healthy person would result in 227
unnatural gait patterns and thereby increase the variables. Third, we studied the rear-foot 228
kinematic change as representative of the ankle joint, since it can be easily marked and 229
compared well with the typical ankle gait analysis 13. Fourth, we only analyzed the 230
posterior leaf-spring AFO, which provide little effects in controlling inverted ankle, in 231
representative of P-AFO in this study. Further study should evaluate the rear-foot, mid-foot, 232
and fore-foot motions under different AFO designs and conditions. 233
14 Conclusions
234
The results of our study suggested that for post-stroke hemiplegic gait, the P-AFO was 235
better than A-AFO in enhancing rear-foot dorsiflexion during the whole gait cycle. The 236
A-AFO was superior to the P-AFO in correcting excessive rear-foot inversion at the stance 237
phase. Both the A-AFOs and P-AFOs helped correct inverted foot at the swing phase. The 238
choice between A-AFO and P-AFO should not only be made by considering the patients’ 239
preference and the practitioners’ expertise, but should also be based on the patients’ motor 240
control and resultant gait characteristics. We report our results here in anticipation that they 241
will be applied to AFO selection in hemiplegic stroke patients. 242
Acknowledgement: 243
This research was supported by the National Science Council, R. O. C. (grant no.: 244
NSC-95-2221-E-033-027) 245
15 References
247
1. Fatone S, Gard SA, Malas BS. Effect of ankle-foot orthosis alignment and foot-plate 248
length on the gait of adults with poststroke hemiplegia. Arch Phys Med Rehabil 249
2009;90(5):810-8. 250
2. Kim CM, Eng JJ. Magnitude and pattern of 3D kinematic and kinetic gait profiles in 251
persons with stroke: relationship to walking speed. Gait Posture 2004;20(2):140-6. 252
3. Lehmann JF, Condon SM, Price R, deLateur BJ. Gait abnormalities in hemiplegia: 253
their correction by ankle-foot orthoses. Arch Phys Med Rehabil 1987;68(11):763-71. 254
4. Abe H, Michimata A, Sugawara K, Sugaya N, Izumi S. Improving gait stability in 255
stroke hemiplegic patients with a plastic ankle-foot orthosis. Tohoku J Exp Med 256
2009;218(3):193-9. 257
5. de Wit DC, Buurke JH, Nijlant JM, Ijzerman MJ, Hermens HJ. The effect of an 258
ankle-foot orthosis on walking ability in chronic stroke patients: a randomized controlled 259
trial. Clin Rehabil 2004;18(5):550-7. 260
6. Tyson SF, Thornton HA. The effect of a hinged ankle foot orthosis on hemiplegic gait: 261
objective measures and users' opinions. Clin Rehabil 2001;15(1):53-8. 262
7. Wang RY, Lin PY, Lee CC, Yang YR. Gait and balance performance improvements 263
attributable to ankle-foot orthosis in subjects with hemiparesis. Am J Phys Med Rehabil 264
2007;86(7):556-62. 265
16 8. Corcoran PJ, Jebsen RH, Brengelmann GL, Simons BC. Effects of plastic and metal 266
leg braces on speed and energy cost of hemiparetic ambulation. Arch Phys Med Rehabil 267
1970;51(2):69-77. 268
9. Bleyenheuft C, Caty G, Lejeune T, Detrembleur C. Assessment of the Chignon 269
dynamic ankle-foot orthosis using instrumented gait analysis in hemiparetic adults. Ann 270
Readapt Med Phys 2008;51(3):154-60. 271
10. Park JH, Chun MH, Ahn JS, Yu JY, Kang SH. Comparison of gait analysis between 272
anterior and posterior ankle foot orthosis in hemiplegic patients. Am J Phys Med Rehabil 273
2009;88(8):630-4. 274
11. Wong AM, Tang FT, Wu SH, Chen CM. Clinical trial of a low-temperature plastic 275
anterior ankle foot orthosis. Am J Phys Med Rehabil 1992;71(1):41-3. 276
12. Chen CK, Hong WH, Chu NK, Lau YC, Lew HL, Tang SF. Effects of an anterior 277
ankle-foot orthosis on postural stability in stroke patients with hemiplegia. Am J Phys Med 278
Rehabil 2008;87(10):815-20. 279
13. Leardini A, Benedetti MG, Berti L, Bettinelli D, Nativo R, Giannini S. Rear-foot, 280
mid-foot and fore-foot motion during the stance phase of gait. Gait Posture 281
2007;25(3):453-62. 282
14. Ragnarsson KT. Lower extremity orthotics, shoes, and gait aids. In: JA Delisa, editor. 283
Physical medicine & rehabilitation:principles and practice 4th ed. Philadelphia: Lippincott, 284
17 Williams & Wilkins; 2005. p 1383-5.
285
15. Brunnstrom S. Motor testing procedures in hemiplegia: based on sequential recovery 286
stages. Phys Ther 1966;46(4):357-75. 287
16. Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of 288
muscle spasticity. Phys Ther 1987;67(2):206-7. 289
17. Verdie C, Daviet JC, Borie MJ, Popielarz S, Munoz M, Salle JY et al. [Epidemiology 290
of pes varus and/or equinus one year after a first cerebral hemisphere stroke: apropos of a 291
cohort of 86 patients]. Ann Readapt Med Phys 2004;47(2):81-6. 292
18. Reiter F, Danni M, Lagalla G, Ceravolo G, Provinciali L. Low-dose botulinum toxin 293
with ankle taping for the treatment of spastic equinovarus foot after stroke. Arch Phys Med 294
Rehabil 1998;79(5):532-5. 295
19. Laurent G, Valentini F, Loiseau K, Hennebelle D, Robain G. Claw toes in hemiplegic 296
patients after stroke. Ann Phys Rehabil Med 2010;53(2):77-85. 297
20. Beckerman H, Becher J, Lankhorst GJ, Verbeek AL. Walking ability of stroke patients: 298
efficacy of tibial nerve blocking and a polypropylene ankle-foot orthosis. Arch Phys Med 299
Rehabil 1996;77(11):1144-51. 300
21. Cruz TH, Dhaher YY. Impact of ankle-foot-orthosis on frontal plane behaviors 301
post-stroke. Gait Posture 2009;30(3):312-6. 302
22. Perry J, Garrett M, Gronley JK, Mulroy SJ. Classification of walking handicap in the 303
18 stroke population. Stroke 1995;26(6):982-9.
304
23. Liu W, Siegler, S., Hillstrom, H. and Whitney, K. Three-dimensional, 305
six-degrees-of-freedom kinematics of the human hindfoot during the stance phase of level 306
walking. Human Movement Science 1997;16:283-98. 307
24. Perry J. Gait analysis: normal and pathological function. NJ: SLACK Incorporated, 308
Thorofare; 1992. 309
25. Turner DNCaMS. An Atlas of Lower Limb Orthotic Practice. London: Chapman& 310
Hall; 1997. 311
26. Levinger P, Gilleard W. Tibia and rearfoot motion and ground reaction forces in 312
subjects with patellofemoral pain syndrome during walking. Gait Posture 2007;25(1):2-8. 313
27. Perry J. The mechanics of walking in hemiplegia. Clin Orthop Relat Res 314
1969;63:23-31. 315
28. Dickstein R. Rehabilitation of gait speed after stroke: a critical review of intervention 316
approaches. Neurorehabil Neural Repair 2008;22(6):649-60. 317
19 Supplier
319
a. Orfit Industries n.v., Vosveld 9a, B-2110 Wijnegem, Belgium. 320
b. Sammons Preston, PO Box 93040 Chicago, IL 60673-3040 USA. 321
c. VICON, Oxford Metrics Limited, 14 Minns Estate, West Way, Oxford, OX2 OJB UK. 322
d. National Instruments 11500 N. Mopac Expwy. Austin, TX 78759-3504. USA. 323
e. SPSS Inc, 233 S Wacker Dr, 11th Fl, Chicago, IL 60606 USA. 324
20 Figure Legends
326
Figure 1. A piece of thermoplastic was cut in the shape of a bottle cap opener 327
Figure 2. The arrangement of markers on the shank and calcaneus in anterior AFO (A, B) 328
and posterior AFO (C, D) conditions 329
Figure 3. Angular motion of rear-foot in both groups: plantarflexion (+); dorsiflexion (-); 330
inversion (+); eversion (-); adduction (+); abduction (-); Asterisks (*) indicate points in the 331
gait cycle where the difference in angles with and without AFOs was significantly different. 332
Vertical lines indicate mean toe-off for each cycle with and without AFOs. The solid line 333
shows toe-off for the A-AFO trial, the dash line for the P-AFO trial, and the dot line for 334
toe-off without an AFO. 335
Figure 4. Angular comparisons of rear-foot with and without AFOs. *: P<0.05; 336
plantarflexion (+), dorsiflexion (-); inversion (+), eversion (-); adduction (+), abduction (-). 337
Table 1: Information about stroke subjects with hemiplegia
Subject Number
Sex Age(y) Years and months since stroke
Involved Side R/L
Brunnstrom stage of involved lower limb
Ankle MAS Use of assistive device
Prior AFO use
1 M 47
5y6m
LV
3 N Y(A-AFO) 2 M 513y8m
LIV
3 N Y(A-AFO) 3 M 473y9m
RV
1+ N N 4 M 672y5m
LIV
1+ N N 5 M 607m
RIII-IV
3 N Y(A-AFO) 6 M 535y4m
RV
2 N N 7 M 538m
LIII
2 N N8 M 51
3y4m
RIII
3 N Y(A-AFO)9 M 43
10m
LV
2 N Y(A-AFO) 10 W 705m
RV
1+ N N 11 W 492m
RIV
2 N Y(A-AFO) 12 W 562y2m
R IV 2 N Y(A-AFO) 13 W 721y
R V 2 N N 14 W 714y4m
L IV 1+ N Y(A-AFO)MAS:Modified Ashworth Scale. N: no, Y: yes.
Table 2. Comparisons of demographic data between stroke and normative subjects Groups Demographic data Stroke subjects (n=14) Normal subjects (n=11) P value Age (years) 56.4 ± 9.8 55.6 ± 8.2 0.842 Gender (Men/Women) 9/5 5/6 0.435 Body height (cm) 161.0 ±9.5 158.3 ± 5.6 0.415 Body mass (kg) 64.0 ± 9.7 60.9 ± 9.9 0.439 . Table 2
Table 3. Gait parameters of AFO conditions in stroke subjects and normal subjects
Stroke patients Normal subjects
Plane A-AFO P-AFO Barefoot Barefoot
Speed (%BH/sec) Step length (%BH) Cycle time (sec)
32.8±11.1 9.6±6.2 4.0±1.4 31.6±10.9 9.2±5.9 4.2±1.4 31.9±11.6 9.8±6.6 3.9±1.5 66.5±3.9 29.4±4.1 2.2±0.3 Table 3
Table 4. Rear-foot kinematics during gait for the involved limb of stroke subjects and control subjects walking barefoot with their self-selected, comfortable walking speed.
Gait phase Initial heel contact Stance phase Swing phase Sagittal plane Plantarflexion Maximal
Dorsiflexion Maximal Plantarflexion Angle (degree) Control 6.3±4.7 -8.6±2.9 8.4±3.6 Stroke 8.5±5.7 -2.4±6.4 5.4±4.0 P-value 0.307 0.018* 0.048*
Coronal plane Inversion Maximal
Eversion Maximal Inversion Angle (degree) Control -1.4±2.8 -4.6±3.0 7.7±2.6 Stroke 8.2±4.5 4.4±5.0 10.5±4.7 P -value <0.001** <0.001** 0.177
Transverse plane Adduction Maximal
Adduction Maximal Abduction Angle (degree) Control 1.2±3.6 11.3±4.5 7.7±2.6 Stroke 8.9±4.3 11.5±5.5 3.7±5.4 P -value <0.001** 0.850 0.118
*: P <0.05; **: P <0.01; plantarflexio (+), dorsiflexion (-); inversion (+), eversion (-);
adduction (+), abduction (-).
A B C D
-10 -5 0 5 10 15 Plantarflexion At initial contact Max dorsiflexion At stance phase Max plantarflexion At swing phase A n g le ( d e g ) A-AFO P-AFO Without AFO 0 5 10 15 20 Inversion At initial contact Max eversion At stance phase Max inversion At swing phase A n g le ( d e g ) 0 5 10 15 20 25 Adduction At initial contact Max adduction At stance phase Max abduction At swing phase A n g le ( d e g ) Sagittal plane Coronal plane Transverse plane * * * * * * * * * * * Figure 4
CHECKLIST
Incomplete submissions will not be put into peer review until requirements are met.
A more complete description of each item that must be checked is provided under the appropriate heading in the Information for Authors.
General
The cover letter with essential information, including statement of information on
corresponding author and statement signed by corresponding author that written permission has been obtained from all persons named in the Acknowledgments.
All elements of the manuscript are printed in English and double-spaced with 1-inch margins at top, bottom, and sides. Right margins are unjustified.
All pages are numbered in the following order: title page, structured or standard abstract, body of the text, acknowledgments, references, legends, and tables.
The text is consecutively line numbered.
If this is a randomized controlled trial, provide the CONSORT flow diagram (http://www.consort-statement.org/Downloads/flowchart.doc).
The Disclosure Statements & Copyright Assignment form signed by the guarantor at original submission. If a resubmission, then all authors must submit the Disclosure Statements & Copyright Assignment form. In either case, the author uploading the
submission must insert the selected financial disclosure into the title page of the manuscript. Human experimentation has been approved by the local institutional review board or conforms to Helsinki Declaration as stated in the section Manuscript Preparation, Methods.
Guidelines for the care use of nonhuman animals or other species approved by the institution have been followed as indicated in the Methods. The species is named in the title, abstract, and Methods section.
Signed, written permission from both the copyright holder and the original author for the use of tables, figures, or quotations previously published and their complete references is on file with the author and can be submitted to the editorial office on request.
Signed, written permission for the use of quotations of personal communications and unpublished data has been obtained from the person(s) being quoted and is enclosed. It is recommended that a professional editor or a colleague fluent in English edit before submission of manuscripts by authors whose first language is not English.
When resubmitting a manuscript for further consideration, provide an itemized accounting of how the manuscript was changed in response to the original set of evaluations.
Similar Publication
Attached is a reprint of each article and/or abstract the author and/or coauthors have previously published or is “in press,” and each manuscript the author and/or coauthors have submitted for possible publication or have in manuscript form dealing with the same patients, animals, laboratory experiment, or data, in part or in full, as those reported in the submitted manuscript. Further explanation of the circumstances is included. Similarities and differences are explained in the cover letter.
Title Page
These elements are in the following sequence, and are typed double spaced.
Word counts for the main text (from opening paragraph through conclusions) and Abstract. Running head of no more than 40 character spaces.
Title.
Author(s) full name(s) and highest academic degree(s) are included.
The name(s) of the institution(s), section(s), division(s), and department(s) where the study was performed are provided and the institutional affiliation(s) of the author(s) at the time of the study is indicated.
Acknowledgment of any presentation of this material, to whom, when, and where. Acknowledgment of financial support.
Requisite financial disclosure as selected from the Disclosure Statements & Copyright Assignment form and an explanation of any conflicts of interest.
Name, address, business and home telephone numbers, fax number, and e-mail address of corresponding author and author from whom reprints can be obtained.
If reprints are not available, this is stated on the title page.
Clinical trial registration number. Abstract
A structured abstract (eg, Articles, Review Articles) with Key Words is on page 2 and is headed by the title.
A standard abstract of 200 words or fewer (eg, Clinical Notes) with Key Words is on page 2 and is headed by the title.
References
All references have been checked for accuracy and completeness.
Are numbered consecutively in the order they are cited in the text; all listed references have been cited in the text.
The format prescribed by the "Uniform Requirements for Manuscripts Submitted to Biomedical Journals" has been followed. Examples provided under Manuscript Preparation have been uploaded.
For any reference cited as "in press," a copy of the article is included.
Personal communications and unpublished observations are not used as numbered references but are mentioned in the text with the written approval of the person being quoted. Author must produce a copy of the approval if so required by the editors. Suppliers
Provide a list (after the Reference section) including all manufacturers and other nondrug products used directly in the study.
Provide names and complete mailing addresses for each Supplier.
Equipment and/or materials are identified in text, tables, and legends by superscript lower case letters.
Suppliers are listed consecutively in the order they are cited in the text.
Figures
Each is numbered with an Arabic numeral and cited in numeric sequence in the text.
Photographs of recognizable persons should be accompanied by a signed release from the patient or legal guardian authorizing publication. Masking eyes to hide identity is not sufficient.
Figure Legends
Are provided for each figure.
Are numbered and presented together in numeric order following Reference page(s). Tables
Each table is headed by a title and numbered in Arabic numerals on a separate page. Tables are cited in numeric sequence in the text.
In addition to the notice of informed consent and releases to publish photographs of recognizable persons, submit with the manuscript written permission to use nonoriginal material (quotations exceeding 100 words, any table or illustration) from both author and publisher of the original. No article will be accepted as a submission to Archives without all required permissions. Credit the source in a text or table footnote or in a legend. Reviewers
Submit the names of 3 potential reviewers and their addresses, telephone numbers, and email address (if known). Do not submit names of people affiliated with your institution. I have reviewed this Checklist and have complied with its requirements.
____Chih-Chi Chen_________________________ ____2010726______________ Type in name above Type in date above