UNCORRECTED
PROOF
1
2
Original Contribution
3
Pigtail catheter for the management of pneumothorax in
4
mechanically ventilated patients
☆
5
Yu-Chao Lin MD, Chih-Yen Tu MD, Shinn-Jye Liang MD, Hung-Jen Chen MD,
6
Wei Chen MD
⁎
, Te-Chun Hsia MD, Chuen-Ming Shih MD, PhD, Wu-Huei Hsu MD
7 Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, China Medical University Hospital,
8 Taichung
Q1 , Taiwan
9 Received 16 December 2008; revised 16 January 2009; accepted 27 January 2009
10 11
12 Abstract
13 Purpose: There has been a paucity of data regarding the efficacy and safety of small-bore chest tubes
14 (pigtail catheter) for the management of pneumothorax in mechanically ventilated patients.
15 Methods: We conducted a retrospective review of mechanically ventilated patients who underwent
16 pigtail catheter drainage as their initial therapy for pneumothorax in the emergency department and
17 intensive care unit from January 2004 through January 2007 in a university hospital.
18 Results: Among the 62 enrolled patients, there were 41 men (66%) and 21 women (34%), with a mean
19 age of 63.8 ± 20.3 years. A total of 70 episodes of pneumothoraces occurred in the intensive care unit,
20 and 48 episodes of pneumothoraces (68.6%) were successfully treated with pigtail catheters. The
21 average duration of pigtail drainage was 5.9 days (1–27 days). No major complications occurred
22 through use of this procedure, except for pleural infections (n = 3, 4.2%) and clogged tube (n = 1, 1.4%).
23 Comparing the variables between the success and failure of pigtail treatment, the failure group had a
24 significantly higher proportion of FIO2 b60% requirement (45.5% vs. 14.6%, P = .005) and higher
25 positive end-expiratory pressure levels (8.7 ± 3.0 vs. 6.2± 2.3 mm Hg, P = .001) at the time of
26 pneumothorax onset than the success group. Further comparing the efficacy of pigtail drainage between
27 barotraumas and iatrogenic pneumothorax, pigtail catheters for management of iatrogenic
pneumothor-28 ax had a significantly higher success rate than barotraumas (87.5% vs. 43.3%, Pb .0001).
29 Conclusion: Pigtail catheter drainage is relatively effective in treating iatrogenic but less promising for
30 barotraumatic pneumothoraces.
31
© 2009 Published by Elsevier Inc.
32
1. Introduction
33
Pneumothorax is a potentially life-threatening
complica-34
tion in the emergency department and intensive care unit
35
(ICU), which usually requires prompt management. Previous
36
studies have reported that the incidence of pneumothorax in
37
the ICU ranges from 4% to 15% [1-4] and that most
38
pneumothoraces can be classified into 2 categories:
☆ Conflicts of interest: The authors have no actual or potential conflicts
of interest.
⁎ Corresponding author. Tel.: +886 4 2205 2121x2010; fax: +886 4 2203 8883.
E-mail address:peteralfa2004@yahoo.com.tw(W. Chen).
www.elsevier.com/locate/ajem
0735-6757/$– see front matter © 2009 Published by Elsevier Inc. doi:10.1016/j.ajem.2009.01.033
American Journal of Emergency Medicine (2009)xx, xxx–xxx
UNCORRECTED
PROOF
39 procedure-related pneumothoraces and mechanicalventila-40 tion-related barotraumas [5,6]. The procedure that most
41 commonly causes pneumothoraces is thoracentesis, followed
42 by vein/pulmonary artery catheterization and transbronchial
43 lung biopsy[5,7]. Barotrauma is usually associated with the
44 patients' underlying lung diseases, such as acute respiratory
45 distress syndrome (ARDS)[8-11], aspiration pneumonia[3],
46 Pneumocystis carinii pneumonia [12], and chronic
obstruc-47 tive pulmonary disease [4,13]. Overall, patients with
48 procedure-related pneumothoraces have better outcomes
49 than barotrauma-related pneumothoraces [5]. In addition,
50 tension pneumothorax, concurrent septic shock, and
pro-51 longed ICU stay were significant independent risk factors for
52 mortality[5,6].
53 Reviewing the literature, there has been a paucity of data
54 regarding the management of pneumothorax in mechanically
55 ventilated patients [14,15]. The US guidelines recommend
56 use of larger (24F-28F) chest drains for patients with
57 spontaneous pneumothorax who may later need mechanical
58 ventilation, which is to allow a high flow state to manage
59 large air leaks generated by positive pressure ventilation
60 [15]. However, few data are available with regard to
small-61 bore chest tubes in the management of pneumothorax in
62 patients receiving positive pressure ventilation.
63 We have previously reported our experience in treating
64 patients in a general ward with primary and secondary
65 spontaneous pneumothorax using small-caliber chest tube
66 (pigtail) drainage with excellent outcomes [16-18]. We
67 also had experience in draining pleural effusions in
68 critically ill patients using ultrasound-guided pigtail
69 catheters [19]. The aim of this study was to evaluate
70 the clinical outcome, efficacy, and safety of pigtail
71 catheters in the treatment of pneumothorax in
mechani-72 cally ventilated patients in the ICU and to investigate
73 whether there are any differences between treating
74 iatrogenic or barotraumatic pneumothoraces.
75
2. Materials and methods
76
2.1. Patients
77 From January 2004 through January 2007, the medical
78 records and chest roentgenograms of all mechanically
79 ventilated patients whose conditions were diagnosed as
80 pneumothorax in the emergency room and medical ICU of
81 China Medical University Hospital (a 1700-bed tertiary
82 medical center with a 44-bed medical ICU) were reviewed
83 carefully. Patients who required mechanical ventilation and
84 underwent insertion of a pigtail catheter as their initial
85 therapy for pneumothorax were enrolled in the study. The
86 diagnosis of pneumothorax required that the following
87 criteria were met: evidence of air accumulation in the
88 pleural space by chest roentgenograms or chest
tomogra-89 phy, and air drainage by thoracentesis or chest tube
90
thoracostomy. All patients with mechanical ventilation
91
were screened daily by the intensivists, respiratory
92
therapists, and nursing staff according to the weaning
93
protocol [20]. The ventilator settings, including tidal
94
volume and positive end-expiratory pressure (PEEP)
95
titrated for patients with acute lung injury or ARDS were
96
guided by a protocol that included a lung protection
97
strategy [21]. In mechanically ventilated patients, tidal
98
volume was set to maintain a plateau pressure below 30 cm
99
H2O in most cases and no greater than 35 cm H2O in all
100
patients. Sedation and neuromuscular blockers were also
101
used according to protocol [22]. The institutional review
102
board at China Medical University Hospital approved the
103
study protocol.
104
2.2. Data collection
105
The following information was collected for each patient
106
receiving mechanical ventilation: demographic data (age,
107
sex, height, weight, smoking history, and underlying
108
diseases), acute physiology and chronic health evaluation
109
(APACHE) II scores [23] at the time of ICU admission,
110
primary indication for mechanical ventilation, type of
111
pneumothorax, location and size of pneumothorax, ARDS
112
event [24], ventilator setting; primary and secondary
113
management for pneumothorax, length of stay in the ICU
114
and total hospitalization, duration of pigtail drainage, and
115
management outcomes. Ventilator parameters including peak
116
inspiratory pressure, plateau pressure, PEEP, fraction of
117
inspired oxygen (FIO2), and tidal volume were recorded
118
during the onset of the pneumothorax.
119
2.3. Definition
120
The pneumothoraces were classified as “barotraumatic”
121
and “iatrogenic.” Iatrogenic pneumothorax was defined as
122
the development of extrapulmonary air resulting from an
123
invasive procedure to the chest, such as thoracentesis, central
124
venous catheterization, bronchoscopy, and
pericardiocent-125
esis[5,7]. Ventilator-associated barotrauma was defined as
126
the development of air outside the tracheobronchial tree
127
resulting from presumptive alveolar rupture and manifested
128
by at least one of the following: interstitial emphysema,
129
pneumothorax, pneumomediastinum, pneumoperitoneum, or
130
subcutaneous emphysema [6,8]. The occurrence of
venti-131
lator-associated barotrauma is increased in patients with
132
severe underlying lung disease, especially in patients with
133
ARDS, pneumonia, or chronic obstructive lung disease. The
134
pigtail catheter was removed if the lung expanded well after
135
drainage with no more air drained from the tube. Pigtail tube
136
removal was considered successful if no more residual air
137
was seen in the follow-up chest radiographs. On the other
138
hand, treatment failure was defined as progression of
139
pneumothorax size despite pigtail drainage or no significant
140
improvement in chest radiographs with persistent air leak in
2 Y.-C. Lin et al.
UNCORRECTED
PROOF
141 the 48 hours of follow-up. If resolution of the pneumothorax142 failed using pigtail drainage, insertion of a large-bore chest
143 tube (24F-32F) was performed.
144
2.4. Procedure for pigtail catheter insertion
145 The entire procedure, including examination by chest
146 ultrasound and insertion of the pigtail catheter, was
147 performed by an experienced emergency physician or
148 intensivist (also a pulmonologist) at the bedside in the
149 emergency room or ICU. Percutaneous pigtail catheters
150 (SKATER, PBN Medicals, Denmark
Q2 ) were all single-lumen
151 polyurethane coiled catheters, sized 12F to 16F, used in
152 conjunction with a wire and dilator and connected to a
153 negative-pressure drainage system with 10 cm H2O pressure
154 applied. Before inserting the catheter, a chest ultrasonic
155 examination was performed to locate the puncture site and
156 further confirm the diagnosis of pneumothorax by
ultra-157 sonographic pattern (gliding sign, lung point sign, and comet
158 tail artifact)[25-29]. After determining the insertion site, the
159 catheter was inserted using the modified Seldinger
techni-160 que, with insertion of the needle and syringe over a rib and
161 gentle aspiration of a syringe to locate the pneumothorax in
162 the pleural space. Finally, the pigtail catheter was attached to
163 a water seal chest drain system. The pigtail tubes were
164 secured properly, and the nursing staff was trained to monitor
165 the tubes vigilantly and to continuously inspect to prevent
166 tension pneumothorax. A chest radiograph was performed
167 immediately after the procedure. Generally, a chest
radio-168 graph was performed every day for the first 3 days.
169 Thereafter, chest radiographs were obtained every 3 days
170 or when clinical conditions changed.
171
2.5. Statistical analysis
172 Demographic and descriptive data are given as mean ± 1
173 SD and were compared using a two-tailed Student t test.
174 Categorical variables were compared using the chi-square or
175 Fisher's exact test, when appropriate (SPSS statistical
176 software for Windows, Chicago, Ill; statistical significance,
177 Pb .05). The clinical outcomes of the treatments with the
178 pigtail catheters were determined by evaluating resolution of
179 the pneumothorax.
180
3. Results
181 From January 2004 through January 2007 (3-year
182 interval), a total of 5358 patients were admitted to our
183 ICU. Eighty mechanically ventilated patients (1.5%)
184 received diagnoses of pneumothorax in the emergency
185 room and the ICUs during this period of time. In our
186 hospital, physicians routinely perform insertion of a pigtail
187 catheter as initial treatment for pleural disease
(pneu-188 mothorax or pleural effusions) in the emergency room and
189
medical ICUs [19], and surgeons customarily perform the
190
insertion of large-bore chest tubes for pleural diseases. As a
191
result, 71 ventilated patients received pigtail catheters as
192
initial therapy for pneumothorax in the emergency room
193
and medical ICUs, and the other 9 patients received
large-194
bore chest tubes as their initial therapy for pneumothorax in
195
the surgical ICU. Among the 71 mechanically ventilated
196
patients who received the pigtail catheter as the initial
197
therapy, 9 patients were excluded because the patients
198
expired as a result of their underlying diseases on the same
199
day as the pigtail insertion and, thus, could not be
200
evaluated. All these 9 patients died of shock, and their
201
follow-up chest radiographs all showed full lung expansion.
202
Eventually, 62 patients were enrolled in this study, and
203
there were a total of 70 episodes of pneumothorax
204
occurring during the emergency room and ICU stay.
205
3.1. Characteristics and underlying diseases
206
Among the enrolled 62 patients, there were 41 men (66%)
207
and 21 women (34%), with ages ranging from 17 to 91 years
208
(mean, 63.8 years). The mean APACHE II score on the first day
209
of ICU admission was 19.6 ± 8.3. Thirty-five patients (56.5%)
210
had right-side pneumothoraces, 19 patients (30.6%) had
left-211
side, and 8 patients (12.9%) had bilateral pneumothoraces. The
212
most common primary indication for endotracheal intubation
213
was pneumonia (n = 37, 59.7%), followed by sepsis (n = 7,
214
11.3%), and neurological disorder (n = 8, 12.9%). Concomitant
215
underlying diseases were frequently found at the time of
216
admission, and the most common was malignancy (n = 18,
217
29.0%) followed by hypertension (n = 15, 24.2%) and diabetes
218
mellitus (n = 15, 24.2%) (Table 1).
219
3.2. Treatment outcome, complications,
220
and mortality
221
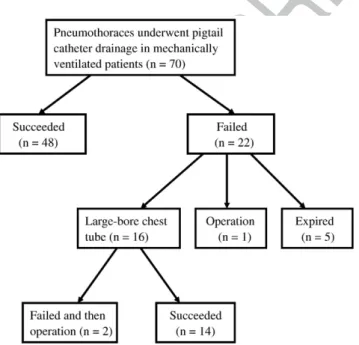
As shown in Fig. 1, 48 episodes of pneumothorax
222
(68.6%) were successfully treated with pigtail catheters.
223
Among 22 of the 70 episodes that were not resolved with
224
pigtail catheter drainage, one patient subsequently underwent
225
thoracoscopy with pleurodesis, five patients later died of
226
complications from their underlying disease, and 16 patients
227
underwent large-bore chest tube drainage. Of these 16
228
patients who underwent large-bore chest tube drainage, 2
229
patients also failed a subsequent 28F to 32F thoracostomy
230
tube and were required to undergo surgical pleurodesis. The
231
average duration of pigtail drainage was 5.9 days (1-27
232
days). Overall, 37 patients (59.7%) died during their ICU
233
stay, but none of them died of pneumothorax. No major
234
complications occurred through the use of this procedure,
235
except for 3 patients who developed pleural infections and 1
236
patient in whom the tube was occluded by a blood clot. The
237
pathogens associated with the 3 pleural infections were all
238
Staphylococcus aureus, and these patients were all
immu-239
nocompromised (2 malignancies and 1 uremia). Complica-3 Pigtail catheter for pneumothorax
UNCORRECTED
PROOF
240 tion events were managed with adequate drainage, antibiotic241 use, correct coagulopathy, and replacement or adjustment of
242 the tube by a physician. Analyzing the variables between the
243
2 groups (Table 2), more of the patients who failed the pigtail
244
drainage required FIO2b60% (45.5% vs 14.6%, P = .005),
245
and they had higher PEEP setting (8.7 ± 3.0 vs 6.2 ± 2.3, P =
246
.001) at the time of pneumothorax onset than patients whose
247
pigtail drainage was successful.
248
3.3. Barotraumatic and iatrogenic pneumothoraces
249
Among the 70 episodes of pneumothorax, 30 (42.9%)
250
were associated with barotraumas and the other 40 were
251
iatrogenic pneumothoraces. Underlying lung diseases for
252
patients with barotraumas included pneumonia (n = 25,
253
83%), chronic obstructive pulmonary disease (n = 3, 10%),
254
interstitial lung disease (n = 1, 3%), and asthma (n = 1,
255
3%). The 40 episodes of iatrogenic pneumothorax were
256
caused by transbronchial lung biopsy (n = 3, 7.5%), central
257
venous/pulmonary artery placement (n = 31, 77.5%), and
258
thoracentesis (n = 6, 15%). Comparing the efficacy of
259
pigtail drainage between barotraumatic and iatrogenic
260
pneumothorax, use of pigtail catheters for management of
261
iatrogenic pneumothorax had a significantly higher success
262
rate than for barotraumatic (87.5% vs. 43.3%, P b .0001).
263
In addition, patients who developed ventilator-associated
264
barotraumatic pneumothoraces had a significantly longer
265
interval from the start of mechanical ventilation to
266
occurrence of pneumothorax (10.4 ± 8.4 vs 4.3 ±
267
7.5 days, P b .05), a higher incidence of ARDS events
268
(67% vs 10%, Pb .05), and a longer ICU stay (19.5 ± 9.3
Table 1
t1:1 Characteristics of 62 patients with pneumothoraces in the emergency department and ICU
t1:2
t1:3 Characteristics Patient no. (%) t1:4 Age (y) (mean ± SD) 63.8 ± 20.3 t1:5 Sex (male/female) 41/21
t1:6 Smoking 23 (37.1)
t1:7 APACHE II score (mean ± SD) 19.6 ± 8.3 t1:8 Primary indication for intubation
t1:9 Pneumonia 37 (59.7)
t1:10 Sepsis 7 (11.3)
t1:11 Neurological disorder 8 (12.9) t1:12 Upper airway obstruction 4 (6.5)
t1:13 Post-surgery 3 (4.8) t1:14 COPD 3 (4.8) t1:15 Miscellaneous 1 (1.6) t1:16 Underlying diseases t1:17 Malignancya 18 (29.0) t1:18 Hypertension 15 (24.2) t1:19 Diabetes mellitus 15 (24.2) t1:20 Chronic airway diseaseb 13 (21.0) t1:21 Congestive heart failure 7 (11.3)
t1:22 Uremia 6 (9.7)
t1:23 Cerebral vascular disease 6 (9.7) t1:24 Previous tuberculosis 5 (8.1) t1:25 Hepatic cirrhosis 5 (8.1)
t1:26 AIDS 2 (3.2)
COPD indicates chronic obstructive pulmonary disease. t1:27
a
Included lung cancer (n = 2), extra-pulmonary cancer (n = 16). t1:28
b
Included asthma (n = 1), chronic obstructive pulmonary disease (n = 11), and bronchiectasis (n = 1).
t1:29
Fig. 1 Flow chart representing the treatment outcomes of 62 patients with 70 episodes of pneumothoraces undergoing pigtail catheter as their initial management in the ICU.
Table 2 Comparison of successful and failed pigtail treatment t2:1 in 70 episodes of pneumothoraces in the ER and ICU
t2:2 t2:3 Success (n = 48) Failure (n = 22) P t2:4 Age 63.3 61.7 .765 t2:5 Sex (male/female) 27/21 20/2 .004 t2:6 Body mass index 19.6 ± 4.0 19.2 ± 3.6 .726
t2:7 APACHE II scores 20.0 ± 9.0 19.0 ± 7.4 .637 t2:8 Smoking 15 12 .063 t2:9 Pneumothorax side (right/left) 30/18 13/9 .221 t2:10 Days from start of
mechanical ventilation to pneumothorax 5.5 ± 7.5 10.1 ± 9.6 .034 t2:11 ARDS event 13 (27.1) 11 (50.0) .061 t2:12 Ventilator setting t2:13 Fio2b60% 7 (14.6) 10 (45.5) .005 t2:14 PEEP 6.3 ± 2.3 8.7 ± 3.0 .001 t2:15 Tidal volume 520.7 ± 105.3 483.8 ± 115.1 .207 t2:16 PIP 30.7 ± 5.9 32.3 ± 5.7 .329 t2:17 Plateau pressure 25.4 ± 3.9 24.7 ± 3.7 .548 t2:18 ICU stay (d) 12.4 ± 8.2 18.8 ± 10.3 .007 t2:19 Total hospitalization (d) 34.1 ± 30.4 42.3 ± 39.5 .346 t2:20 Pigtail intubation time (d) 6.0 ± 5.3 5.8 ± 6.3 .901
t2:21 Complications 3 (6.3) 1 (4.5) .775
t2:22 Mortality 28 (57) 13 (61) .952
PIP indicates peak inspiratory pressure. t2:23
4 Y.-C. Lin et al.
UNCORRECTED
PROOF
269 vs 10.6 ± 7.3 days, P b .05) than patients who had270 iatrogenic pneumothoraces (Table 3).
271
4. Discussion
272 To the best of our knowledge, this is the first retrospective
273 study reporting the efficacy and safety of drainage using a
274 small-bore chest tube (pigtail catheter) as the initial treatment
275 in mechanically ventilated patients who developed
pneu-276 mothoraces in the emergency room and medical ICUs. Our
277 study showed that the overall success rate was 68.6%,
278 (barotraumatic: 43.3%, iatrogenic: 87.5%), and the
compli-279 cation rate was 5.7%. Therefore, in our series, the use of
280 pigtail catheters with a water seal drainage system appears to
281 be a safe and promising technique in the treatment of
282 pneumothoraces under positive pressure ventilation.
283 In this study, patients who failed pigtail catheter
284 drainage seemed to have significantly higher PEEP levels
285 (8.7 ± 3.0 vs. 6.3 ± 2.3 mm Hg, P = .001) than patients
286 who were successfully treated with pigtail catheters.
287 According to our ventilator setting protocol for ARDS
288 [30], high PEEP levels were usually applied for those
289 patients. Therefore, higher PEEP levels may reflect more
290 severe underlying pulmonary conditions. In this vicious
291 cycle, the effects of PEEP may raise airway pressures and
292 aggravate air leakage[31].
293 The interval from start of mechanical ventilation to
294 occurrence of pneumothorax caused by barotrauma was
295 10.4 days, which was significantly longer than that in
296 the iatrogenic pneumothoraces (4.3 days). This was
297
because most invasive procedures were performed within
298
the first three days of ICU admission, but the patients
299
with ARDS usually developed pneumothorax in the late
300
stages (N2 weeks) [32].
301
Little is known about the small-bore chest tube for
302
treating iatrogenic pneumothoraces in patients under positive
303
pressure ventilation. Reviewing the literature, the success
304
rate of small-bore chest tubes for treating iatrogenic
305
pneumothoraces was about 71% to 85% [33-35]. Our data
306
showed an 87.5% success rate for treatment with the pigtail
307
catheter in patients who developed iatrogenic
pneu-308
mothoraces in the ICU. Thus, we strongly suggest that the
309
pigtail catheter can be used as first-line therapy for iatrogenic
310
pneumothoraces under positive pressure ventilation.
311
Traditional large-bore chest tubes usually produce much
312
more chest wall trauma than pigtail catheters because the
313
physician must make an incision into the chest wall, bluntly
314
dissect the intercostal tissues, and place the tube into the
315
pleural space. Furthermore, insertion requires significant
316
force, which may cause inadvertent damage to the chest wall
317
and the underlying organs. The advantage of the pigtail
318
method is that it is easy and simple to perform for the
319
physician and involves less trauma and discomfort for the
320
patient. To further enhance safety, we performed this
321
procedure under ultrasonic guidance. A chest ultrasonic
322
examination was performed before the procedure for the
323
following reasons: (1) to confirm the diagnosis of
pneu-324
mothorax with an echo finding (lung sliding or gliding sign,
325
lung point sign, comet tail artifact) [25-29] and (2) to
326
evaluate the presence of pleural effusion and locate the solid
327
organ positions to prevent hollow organ perforation.
328
There were some limitations to our study. First, this was a
329
retrospective study, and we do not have comparative results
330
from large-bore chest tubes in mechanically ventilated
331
patients with pneumothoraces. However, the results in our
332
series are still promising and similar to those of a previous
333
study that showed a success rate of 55% when large-bore
334
chest tubes were inserted to treat pneumothoraces in the ICU
335
[5]. Second, the number of enrolled patients in our series was
336
too small to further analyze possible factors predicting
337
treatment failure. A larger prospective and randomized trial
338
is necessary to confirm our results.
339
In conclusion, this is the first report of the utility of pigtail
340
catheters in the management of mechanically ventilated
341
patients with pneumothoraces. Our study shows that
342
drainage using pigtail catheters is relatively effective in
343
iatrogenic pneumothoraces but less promising in
barotrau-344
matic pneumothoraces.
345
References
346
[1] Strange C. Pleural complications in the intensive care unit. Clin Chest
347
Med 1999;20:317-27.
348
[2] Petersen GW, Baier H. Incidence of pulmonary barotrauma in a
349
medical ICU. Crit Care Med 1983;11:67-9.
Table 3
t3:1 Clinical characteristics and outcomes of barotrauma and iatrogenic pneumothoraces undergoing pigtail catheter drainage in the ER and ICU
t3:2 t3:3 Barotrauma (n = 30) Iatrogenic (n = 40) P t3:4 Age 56.6 67.5 .027 t3:5 Sex 23/7 24/16 .142 t3:6 BMI 20.2 ± 3.2 18.9 ± 4.2 .199 t3:7 Smoking 15 (50) 12 (30) .089 t3:8 Pneumothorax side (right/left) 15/15 28/12 .089 t3:9 Pneumothorax size (large) 25 (83) 34 (85) .683 t3:10 APACHE II score 17.5 ± 6.8 21.4 ± 9.3 .054 t3:11 Successful pigtail treatment 13 (43.3) 35 (87.5) .001 t3:12 Days from start of mechanical
ventilation to pneumothorax 10.4 ± 8.4 4.3 ± 7.5 b.05 t3:13 FIO2b60% 9 (30) 8 (20) .334 t3:14 ICU stay (d) 19.5 ± 9.3 10.6 ± 7.3 b.05 t3:15 Total hospitalization (d) 41.1 ± 34.7 33.3 ± 32.5 .337 t3:16 Duration of pigtail intubation (d) 6.2 ± 5.2 5.8 ± 5.9 .742 t3:17 Mortality 20 (67) 21 (52.5) .234
BMI indicates body mass index.
t3:18 *Pb .05 compared with the pneumonia subgroup.
t3:19 Q3
5 Pigtail catheter for pneumothorax
UNCORRECTED
PROOF
350 [3] de Latorre FJ, Tomasa A, Klamburg J, et al. Incidence of351 pneumothorax and pneumomediastinum in patients with aspiration
352 pneumonia requiring ventilatory support. Chest 1977;72:141-4.
353 [4] Zwillich CW, Pierson DJ, Creagh CE, et al. Complications of assisted
354 ventilation. A prospective study of 354 consecutive episodes. Am J
355 Med 1974;57:161-70.
356 [5] Chen KY, Jerng JS, Liao WY, et al. Pneumothorax in the ICU: patient
357 outcomes and prognostic factors. Chest 2002;122:678-83.
358 [6] Anzueto A, Frutos-Vivar F, Esteban A, et al. Incidence, risk factors and
359 outcome of barotrauma in mechanically ventilated patients. Intensive
360 Care Med 2004;30:612-9.
361 [7] de Lassence A, Timsit JF, Tafflet M, et al. Pneumothorax in the
362 intensive care unit: incidence, risk factors, and outcome.
Anesthesiol-363 ogy 2006;104:5-13.
364 [8] Weg JG, Anzueto A, Balk RA, et al. The relation of pneumothorax and
365 other air leaks to mortality in the acute respiratory distress syndrome.
366 N Engl J Med 1998;338:341-6.
367 [9] Amato MB, Barbas CS, Medeiros DM, et al. Effect of a
protective-368 ventilation strategy on mortality in the acute respiratory distress
369 syndrome. N Engl J Med 1998;338:347-54.
370 [10] Stewart TE, Meade MO, Cook DJ, et al. Evaluation of a ventilation
371 strategy to prevent barotrauma in patients at high risk for acute
372 respiratory distress syndrome. Pressure- and Volume-Limited
Ventila-373 tion Strategy Group. N Engl J Med 1998;338:355-61.
374 [11] Brochard L, Roudot-Thoraval F, Roupie E, et al. Tidal volume
375 reduction for prevention of ventilator-induced lung injury in acute
376 respiratory distress syndrome. The Multicenter Trail Group on Tidal
377 Volume reduction in ARDS. Am J Respir Crit Care Med 1998;158:
378 1831-8.
379 [12] Sepkowitz KA, Telzak EE, Gold JW, et al. Pneumothorax in AIDS.
380 Ann Intern Med 1991;114:455-9.
381 [13] Kumar A, Pontoppidan H, Falke KJ, et al. Pulmonary barotrauma
382 during mechanical ventilation. Crit Care Med 1973;1:181-6.
383 [14] Henry M, Arnold T, Harvey J. BTS guidelines for the management of
384 spontaneous pneumothorax. Thorax 2003;58(Suppl 2):ii39-52.
385 [15] Baumann MH, Strange C, Heffner JE, et al. Management of
386 spontaneous pneumothorax: an American College of Chest Physicians
387 Delphi consensus statement. Chest 2001;119:590-602.
388 [16] Chen CH, Chen W, Hsu WH. Pigtail catheter drainage for secondary
389 spontaneous pneumothorax. QJM 2006;99:489-91.
390 [17] Liu CM, Hang LW, Chen WK, et al. Pigtail tube drainage in the
391 treatment of spontaneous pneumothorax. Am J Emerg Med 2003;21:
392 241-4.
393 [18] Tsai WK, Chen W, Lee JC, et al. Pigtail catheters vs large-bore chest
394 tubes for management of secondary spontaneous pneumothoraces in
395 adults. Am J Emerg Med 2006;24:795-800.
396
[19] Liang SJ, Tu CY, Chen HJ, et al. Application of ultrasound-guided
397
pigtail catheter for drainage of pleural effusions in the ICU. Intensive
398
Care Med 2008.
399
[20] Ely EW, Baker AM, Dunagan DP, et al. Effect on the duration of
400
mechanical ventilation of identifying patients capable of breathing
401
spontaneously. N Engl J Med 1996;335:1864-9.
402
[21] Ventilation with lower tidal volumes as compared with traditional tidal
403
volumes for acute lung injury and the acute respiratory distress
404
syndrome. The Acute Respiratory Distress Syndrome Network. N
405
Engl J Med 2000;342:1301-8.
406
[22] Brook AD, Ahrens TS, Schaiff R, et al. Effect of a
nursing-407
implemented sedation protocol on the duration of mechanical
408
ventilation. Crit Care Med 1999;27:2609-15.
409
[23] Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of
410
disease classification system. Crit Care Med 1985;13:818-29.
411
[24] Bernard GR, Artigas A, Brigham KL, et al. The American-European
412
Consensus Conference on ARDS. Definitions, mechanisms, relevant
413
outcomes, and clinical trial coordination. Am J Respir Crit Care Med
414
1994;149:818-24.
415
[25] Lichtenstein D, Meziere G, Biderman P, et al. The“lung point”: an
416
ultrasound sign specific to pneumothorax. Intensive Care Med 2000;
417
26:1434-40.
418
[26] Lichtenstein D, Meziere G, Biderman P, et al. The comet-tail artifact:
419
an ultrasound sign ruling out pneumothorax. Intensive Care Med 1999;
420
25:383-8.
421
[27] Lichtenstein DA, Menu Y. A bedside ultrasound sign ruling out
422
pneumothorax in the critically ill. Lung sliding. Chest 1995;108:1345-8.
423
[28] Targhetta R, Bourgeois JM, Chavagneux R, et al. Diagnosis of
424
pneumothorax by ultrasound immediately after ultrasonically guided
425
aspiration biopsy. Chest 1992;101:855-6.
426
[29] Wernecke K, Galanski M, Peters PE, et al. Pneumothorax: evaluation
427
by ultrasound—preliminary results. J Thorac Imaging 1987;2:76-8.
428
[30] Gattinoni L, Caironi P, Cressoni M, et al. Lung recruitment in patients
429
with the acute respiratory distress syndrome. N Engl J Med 2006;354:
430
1775-86.
431
[31] Ricard JD. Barotrauma during mechanical ventilation: why aren't we
432
seeing any more? Intensive Care Med 2004;30:533-5.
433
[32] Gattinoni L, Bombino M, Pelosi P, et al. Lung structure and function in
434
different stages of severe adult respiratory distress syndrome. JAMA
435
1994;271:1772-9.
436
[33] Conces Jr DJ, Tarver RD, Gray WC, et al. Treatment of
pneu-437
mothoraces utilizing small caliber chest tubes. Chest 1988;94:55-7.
438
[34] Horsley A, Jones L, White J, et al. Efficacy and complications of
439
small-bore, wire-guided chest drains. Chest 2006;130:1857-63.
440
[35] Collop NA, Kim S, Sahn SA. Analysis of tube thoracostomy performed
441
by pulmonologists at a teaching hospital. Chest 1997;112:709-13.
442 443
6 Y.-C. Lin et al.