Re: Manuscript ID CMAJ-12-0230 R1
Revision 2: Association between hypertensive disorders in pregnancy
and future end-stage renal disease: a population-based study
I-Kuan Wang, MD1, 2,3, Chih-Hsin Muo, MS4,5, Yi-Chih Chang, PhD6, Chih-Chia Liang, MD2, Chiz-Tzung Chang, MD, PhD2, Shih-Yi Lin2, MD, Tzung-Hai Yen, MD, PhD7, Feng-Rong Chuang8, MD, Pei-Chun Chen, PhD1,4*, Chiu-Ching Huang, MD1, Chi-Pang Wen, MD, PhD 9, Fung-Chang Sung, PhD4,5*, Donald E. Morisky, ScD10
Running title: Hypertension disorders in pregnancy and ESRD
1Graduate Institute of Clinical Medical Science, China Medical University, Taichung, Taiwan
2Department of Internal Medicine, College of Medicine, China Medical University, Taichung, Taiwan
3Division of Kidney Disease, China Medical University Hospital, Taichung, Taiwan 4Management Office for Health Data, China Medical University Hospital, Taichung, Taiwan
5Department of Public Health, China Medical University, Taichung, Taiwan
6Department of Medical Laboratory Science and Biotechnology, China Medical University, Taichung, Taiwan
7Division of Nephrology, Chang Gung Memorial Hospital-Taipei Medical Center, Chang Gung University College of Medicine, Taoyuan, Taiwan
8Division of Nephrology, Chang Gung Memorial Hospital-Kaohsiung Medical Center, Chang Gung University College of Medicine, Kaohsiung, Taiwan
9Institute of Population Science, National Health Research Institute, Zhuan, Taiwan 10UCLA Fielding School of Public Health, Los Angeles, CA
*Corresponding author: Fung-Chang Sung, PhD, MPH Professor
China Medical University Department of Public Health 91 Hsueh Shih Road
Taichung 404, Taiwan Tel: 886-4-2206-2295 Fax: 886-4-2201-9901
Author Contributors: Wang, Chang YC, Chang CT, Liang, Lin, Yen, Chuang and Huang designed the study. Muo carried out the statistical analysis. Wang drafted the manuscript. Chen, Huang, Wen, Sung and Morisky revised the manuscript.
Financial Disclosure: No conflict of financial interest was declared.
Funding/Support: The present study was supported by the National Sciences Council, Executive Yuan (grant numbers NSC 97-2625-M-039-003, NSC 100-2621-M-039-001), China Medical University Hospital (grant number 1MS1), Department of Health, Taiwan, Clinical Trial and Research Center for Excellence (grant number DOH101-TD-B-111-004), and Cancer Research Center of Excellence (DOH101-TD-C-111-005).
Ethical approval: The identifications of all insured subjects were scrambled to ensure confidentially to prevent ethical violation. The study was approved by the institutional review board at China Medical University Hospital.
Word count: 237 words in the Abstract, 2486 words in the text; 4 tables, 1 figure and
Abstract Background:
Studies on the association between hypertensive disorders in pregnancy and end-stage renal disease (ESRD) are limited. This study investigated the ESRD risk after delivery
for women with hypertensive disorders in pregnancy. .
Methods: We used insurance claims data of 1998-2009 to identify 26,651 women aged 19-40 years old with hypertensive disorders in pregnancy, without the baseline history of hypertension, diabetes, kidney disease, or lupus. We further randomly selected 213,397 women without thedisorders in pregnancy as the comparison cohort, withfrequency matched by age and the index year of pregnancy. Incidence rates of ESRD were compared between the two cohorts by the end 2009. Hazard ratios (HRs) were calculated with controlling for demographics and clinical factors.
Results: The women with hypertensive disorders in pregnancy had a greater risk of chronic kidney disease and ESRD , with adjusted HRs of 9.38 (95% CI 7.09-12.4) and
12.4 (95% CI 8.54-18.0), respectively, after controlling for urbanization, coronary artery disease, congestive heart failure, hyperlipidemia and abruption. The HR for ESRDdecreased to 2.72 (95% CI 1.76-4.22) after further controlling for hypertension and diabetes. Women with preeclampsia/eclampsia had a higher adjusted HR of 14.0 (95% CI 9.43-20.7)than those with only gestational hypertension (adjusted HR 9.03, 95% CI 5.20-15.7).
Interpretation: Women with hypertensive disorders in pregnancy are at a high risk of subsequent ESRD. The risk increase much higher for women with
preeclampsia/eclampsia, compared with those with only gestational hypertension.
Keywords: End-stage renal disease, gestational hypertension, preeclampsia, pregnancy.
Introduction
Hypertensive disorders in pregnancy are major causes of maternal and fetal morbidity and mortality, affecting 5% to 10% of pregnancies. Both gestational
hypertension and preeclampsia are the spectra of hypertensive disorders in pregnancy. Gestational hypertension is referred to as the new onset of hypertension (over 140/90 mmHg) without proteinuria after 20-week gestation in pregnant women. Preeclampsia characterizes the new onset of hypertension (over 140/90 mmHg) with proteinuria of at least 300 mg in a 24-hour urine sample after 20-week gestation. Gestational
hypertension may progress into preeclampsia in 10% to 20% of pregnant women. The risk factors associatedwith preeclampsia include family history of preeclampsia, first pregnancy, multiple gestation, old maternal age, obesity, preexisting hypertension, renal disease, and diabetes mellitus. Women with a history of hypertensive disorders in pregnancy are at higher risk of encountering hypertension, diabetes mellitus, and cardiovascular disease in later life. Hypertensive disorders in pregnancy and
cardiovascular disease share several common risk factors, such as obesity, preexisting hypertension, renal disease, and insulin resistance. Hypertensive disorders in
pregnancy also increases the risk of emerging cardiovascular disease because of long-term metabolic and vascular changes.
Hypertensive disorders in pregnancy affects the function and morphology of the kidney. Previous studies have reported increased prevalence of microalbuminuria
after pregnancy in women with previous hypertensive disorders in pregnancy. In a case control study, women with biopsy-proven renal disease are associated with a past history of preeclampsia. However, studies on whether hypertensive disorders in pregnancy is associated with subsequent end-stage renal disease (ESRD) in later life are limited. Only one study from Norway linking birth and renal registries has
demonstrated that women with preeclampsia during their first pregnancy is associated with a 3.2-fold increased risk of ESRD. The present study investigated the risk of ESRD for Asian women with hypertensive disorders in pregnancy using the universal insurance claim data of Taiwan.
Methods
Data sourceWe obtained a dataset consisting of health care reimbursement claims established for the 1996-2009 period by the National Health Research Institutes for the Taiwan National Health Insurance program. Taiwan National Health Insurance program was reformed from 13 insurance systems in March 1995 with a coverage rate of 93.1% for the 23 million residents in 1996 and rising to 99% in 1999. Patient identifications that were used for linking files had been scrambled before the data set was released to secure patient privacy. The present study was approved by the Research Ethic Committee of China Medical University Hospital. The International Classification of
Disease Revision 9th Clinical Modification (ICD-9-CM) in databases of National Health Research Institutes was used to define diseases.
Study subjects
We identified 28,724 women with hypertensive disorders in pregnancy (ICD-9-CM: 642.3, 642.4–642.6, 642.9) in the first pregnancy who were 19 to 40 years old during 1998 to 2009. This pregnancy was defined as the index pregnancy. The date when the hypertensive disorder in pregnancy was diagnosed was used as the index date for estimating the follow-up time. We excluded women with the history of
hypertension (N = 447), diabetes (N = 1194), renal disease (N = 396), and systemic
lupus erythematous (N = 36) before the index date. We selected the remaining 26,651 women with hypertensive disorders in pregnancy as the study cohort of hypertensive disorders in pregnancy.
For each woman with hypertensive disorders in pregnancy, 8 women without hypertensive disorders in pregnancy were randomly selected, as the comparison cohort, from women with the first normal pregnancy and with frequency matched by
age and the index year. Aside from the similar exclusion criteria as the cohort of
hypertensive disorders in pregnancy, women with any history of hypertensive disorders in pregnancy before the development of ESRD or by the end of 2009 were illegible in the comparison cohort.
chronic kidney disease and ESRD. Subjects who died or withdrew from the National Health Insurance program were censored. The ESRD patients were defined from the registry for catastrophic illness patients who required long-term renal replacement therapy, such as dialysis or renal transplantation.
Covariables
The demographic data used included age at the index pregnancy (19 to 24, 25 to 29, 30 to 34, and 35 to 40 years old) and urbanization level. The baseline disorders, including coronary artery disease, congestive heart failure, and hyperlipidemia were identified before the index date. The postpartum coronary artery disease, congestive heart failure, hypertension, hyperlipidemia and diabetes were also identified before the end-point or December 31, 2009. Preterm delivery and abruption were referred to the outcome of index pregnancy. These disorders were considered as comorbidities that were potentially associated with the development of ESRD. The Taiwan National Health Research Institutes has divided the urbanization of Taiwan into 7 levels, with the level 1 reflected the highest urban areas and the level 7 reflected the lowest urban areas. We combined the level 5 to 7 as the level 5 because of the low population in those areas. The subtypes of hypertensive disorders in pregnancy were classified into gestational hypertension only and preeclampsia.
Data analyses first compared the demographic data and comorbidities between cohorts with and without hypertensive disorders and examined using Chi-square test for categorical variables and t-test for continuous variables. The incidence rates of ESRD were estimated for both cohorts. Cox proportional hazards regression analysis was used to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) of
chronic kidney disease and ESRD for the cohort with hypertensive disorders in pregnancy compared with the cohort without hypertensive disorders in pregnancy.
The Cox proportional hazards assumption was examined using the likelihood test. The assumption was not violated (p = 0.18). We performed four models to estimate crude
HRs and adjusted HRs for evaluating the ESRD risk. We used univariate analysis for model 1. Model 2 controlled for urbanization, coronary artery disease, congestive heart failure, hyperlipidemia, and abruption. We further added hypertension and diabetes to model 3 for the adjustment. Model 4 was a time-dependent Cox proportional hazards regression with hypertension and diabetes as time-dependent variables, also adjusted for variables in model 3. We also examined how postpartum hypertension and diabetes altered the chronic kidney disease and ESRD risk. Kaplan-Meier analysis was used to assess the ESRD-free proportion for both cohorts. The SAS software (version 9.1 for windows; SAS Institute Inc., Cary, NC, USA) was used for all statistical analyses.
Results
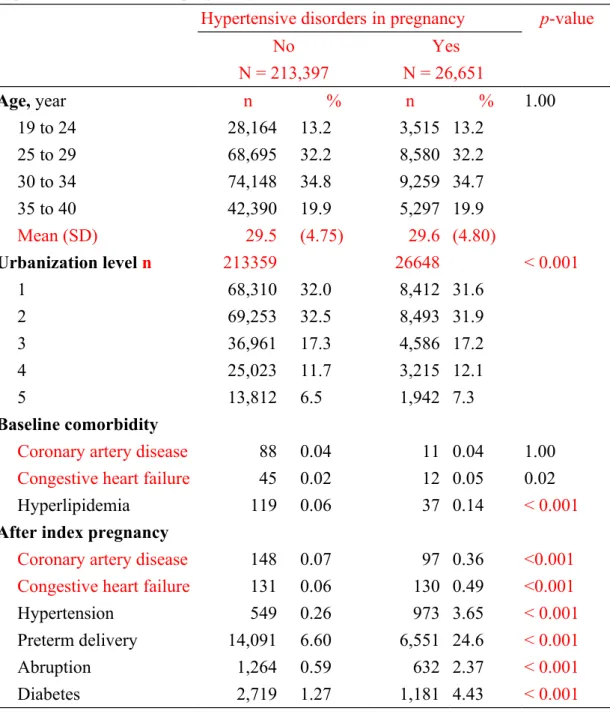
Compared with the cohort withouthypertensive disorders in pregnancy (N = 213 397), the cohort with hypertensive disorders in pregnancy (N = 26651) had less urbanized residents but was more prevalent with congestive heart failure and hyperlipidemia before the index date and comorbidities after the index date (Table 1).
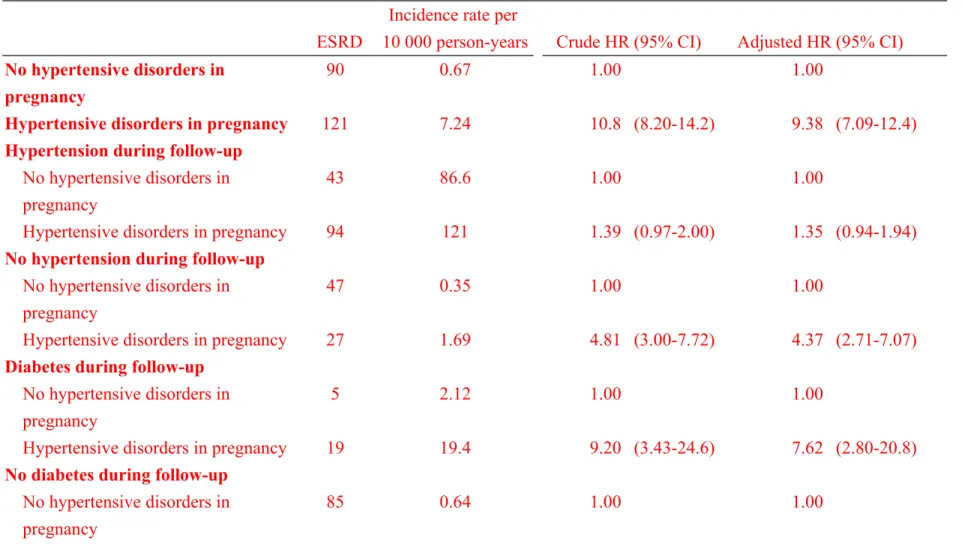
The incidence of chronic kidney disease was 10.8-fold higher in the cohort with hypertensive disorders in pregnancy than in the cohort without the disorders in pregnancy, with an adjusted HR of 9.38 (Table 2). Among women without hypertension during follow-up, women with hypertensive disorders in pregnancy had 4.37-fold higher hazard of chronic kidney disease compared with those without the disorders.
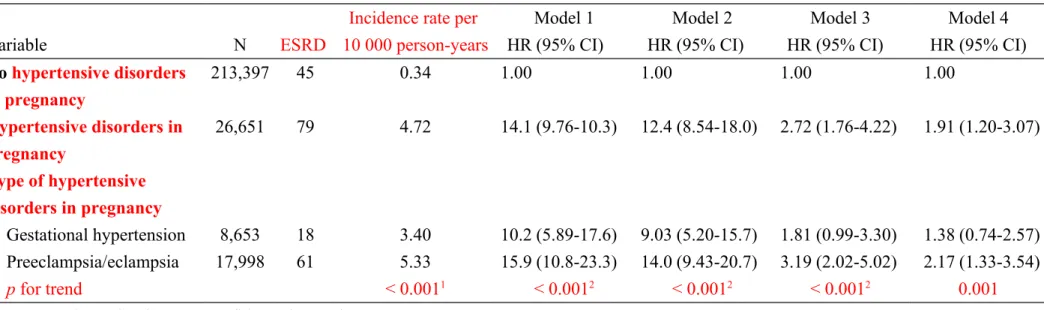
The incidence of ESRD was 14.1-fold higher in the cohort with hypertensive disorders in pregnancy than the cohort without hypertensive disorders in pregnancy, with a crude HR of 14.1 (Table 3). The HR decreased slightly after controlling for urbanization, coronary disease, congestive heart failure, hyperlipidemia, and abruption (model 2), and decreased further to 2.72 after adding hypertension and diabetes to model 3. In the time-dependent model 4, the adjusted HR was 1.91. With a mean follow-up time of approximately 6.3 years for both cohorts, Kaplan-Meier analysis showed that the overall proportion of subjects free of ESRD was lower for
the cohort with hypertensive disorders in pregnancy compared with the cohort without hypertensive disorders in pregnancy (Figure 1).
Women with preeclampsia or eclampsia were at higher risk of ESRD than those had gestational hypertension only (Table 3). In order to reduce the immediate effect of pregnancy complications on the risk of adverse outcome, an additional analysis excluded the first year postpartum events. The HRs for ESRD were 12.7 (95% CI= 8.65-18.6), 11.2 (95% CI=7.56-16.5), 2.11 (95% CI=1.34-3.30) and 1.44 (95% CI=0.90-2.32) in model 1 through model 4 (data not shown). The interaction between preterm delivery and hypertensive disorders in pregnancy was not significant (p = 0.78).
The ESRD incidence increased much greater for women developed postpartum hypertension than for those develop postpartum diabetes (Table 4). However, among women without postpartum hypertension or without postpartum diabetes, women with hypertensive disorders in pregnancy hadmuch greater hazards of ESRD than women without hypertensive disorders in pregnancy.
Interpretation
Main FindingsThe present study demonstrated an elevated risk of subsequent ESRD associated with hypertensive disorders in pregnancy, which included preeclampsia/eclampsia and
gestational hypertension for the Asian women. In addition, women with preeclampsia/eclampsia are at higher risk than those with only gestational hypertension.
Explanation and comparison with other studies
The pathogenesis of hypertensive disorders in pregnancy includes uteroplacental hypoperfusion and fetal ischemia. The hypoperfused placenta subsequently elaborated anti-angiogenic factors into maternal circulation, leading to systemic endothelial cell dysfunction, hypertension, and proteinuria. Karumanchi et al. reported that glomerular endotheliosis characterizes glomerular lesion in women with hypertensive disorders in pregnancy. Depletion of VEGF through anti-angiogenic factors may be responsible for glomerular endotheliosis. Endotheliosis apparently contributes to proteinuria and decreases glomerular filtration rate. Glomerular endotheliosis usually disappears within 8-week after delivery, concurring with the resolutions of proteinuria and hypertension. However, hypertensive disorders in pregnancy may damage the kidney with incomplete healing or scarring.
Previous studies have reported that the increased prevalence of microalbuminuria lasts for 5 to 7 years after the delivery of women with hypertensive disorders in pregnancy. A systemic meta-analysis demonstrated that women with preeclampsia have a 4-fold increased risk of subsequent microalbuminuria, which increases the risk
of both cardiovascular disease and ESRD. Vikse et al. analyzed the Norwegian registry data and found that women with preeclampsia in the first pregnancy are at risk of having a later kidney biopsy. They also showed that women with preeclampsia in one pregnancy have 3.2-fold (95% CI 2.2–4.5) higher adjusted relative risk of ESRD. The risk is even higher for women with a recurrent preeclampsia. In addition, women with preeclampsia and low-birth-weight infant or preterm delivery also have further increase in risk. These conditions suggest a more severe type of preeclampsia. On the contrary, the serum creatinine level and estimated glomerular filtration rate during the follow-up period are not significantly different between women with and without a history of preeclampsia in the meta-analysis of McDonald.
Women with preeclampsia also have a higher risk compared with women with gestational hypertension only. Consistent with the study of Vikse et al. in defining ESRD, the present study demonstrates that women with hypertensive disorders in pregnancy have a near 14-fold higher incidence of ESRD than women without
hypertensive disorders in pregnancy after excluding preexisting hypertension, diabetes, renal disease, and SLE. The adjusted HR decreased remarkably when hypertension and diabetes are adjusted, indicating that these 2 factors greatly account for the risk attributed to hypertensive disorders in pregnancy as intermediate steps in the development of ESRD. There was no statistically significant interaction between
hypertensive disorders in pregnancy and preterm delivery in our study. We also have an important finding that women with only gestational hypertension may even have a 10-fold higher incidence of ESRD than non-HDP women (3.40 vs. 0.34 per 10,000 person-years).
Diabetes and hypertension are also the major risk factors for chronic kidney diseases. During the follow-up period, women may develop postpartum hypertension and postpartum diabetes. Among women with hypertension or diabetes in later life, the cohort with hypertensive disorders in pregnancy had a much higher incidence of ESRD than the cohort without hypertensive disorders in pregnancy had. But relative risk between the cohort with and without hypertensive disorders in pregnancy was much greater in women with postpartum diabetes (adjusted HR = 10.6) than in those with postpartum hypertension (adjusted HR = 1.51). Among women with postpartum hypertension, the adjusted HR for ESRD in the cohort with hypertensive disorders in pregnancy was not significant after controlling for covariates compared to the cohort
without hypertensive disorders in pregnancy. Therefore, hypertension appearing after pregnancy in HDP women may mediate the association between hypertensive
disorders in pregnancy and ESRD. Limitations
in the world. This large national cohort study has disclosed hypertensive disorders in pregnancy as a risk factor of ESRD for women. However, the present study has several limitations. First, information on marital status, educational level, smoking habit, body-mass index, and laboratory measures on glomerular filtration rate and proteinuria are unavailable from the claims file. These variables could not be adjusted in the data analysis. However, the smoking prevalence among general women has been low in Taiwan, and less than 2.5% of pregnant women smoke. Second, we excluded patients with preexisting renal disease, hypertension and diabetes. The mild kidney disease may have been unreported or undetected in some women. The
Norwegian cohort study has the similar limitation. Third, our study represents a part of Asian maternal population, and it is possible that they have different risks. The estimated ESRD risk in this population with hypertensive disorders in pregnancy is higher than the Norwegian women with preeclampsia. The follow-up time after pregnancy is relatively short for the measure of the life time subsequent ESRD and comorbidities in our study. Whether the preexisting renal disease causes hypertensive disorders in pregnancy and followed by deterioration of renal function remains unclear. Furthermore, hypertensive disorders in pregnancy and other comorbidities were identified using ICD-9-CM codes. In Taiwan, the prenatal care has been very well preformed for women since the implementation of National Health Insurance.In
addition, auditors of the insurance system may review and validate claims in random to ensure the accuracy of the claims. Although we could not calculate the validity of diagnostic codes for hypertensive disorders in pregnancy, the high validity of the diagnostic codes of the NHRI database has been reported. Finally, the index
pregnancy was the first pregnancy identified during the study period. A small portion of women with a second pregnancy might be misclassified as the first pregnancy.
Conclusions and implications for further research
We found that women with hypertensive disorders in pregnancy are at markedly higher risk of ESRD, compared with those without complicated pregnancy.
Postpartum hypertension and diabetes also increase the ESRD risk further. The risk for the Asian population is likely higher than that for the Western population. Close surveillance for microalbuminuria, blood pressure, and diabetes should be considered for women with a history of hypertensive disorders in pregnancy. Preventive
strategies, such as pharmacological or lifestyle interventions, should also be considered for these high-risk women. Further prospective study is needed for investigating the relationship between hypertensive disorders in pregnancy and subsequent ESRD.
Acknowledgment: All authors would like to thank the Taiwan National Health Research Institute for providing the NHI database. No conflict of financial interest
was declared. References
1. Hauth JC, Ewell MG, Levine RJ, et al. Pregnancy outcomes in healthy
nulliparas who developed hypertension. Calcium for Preeclampsia Prevention Study Group. Obstet Gynecol. 2000;95:24-8.
2. Roberts CL, Ford JB, Algert CS, et al. Population-based trends in pregnancy hypertension and pre-eclampsia: an international comparative study. BMJ
Open. 2011;1:e000101.
3. Helewa ME, Burrows RF, Smith J, Williams K, Brain P, Rabkin SW. Report of the Canadian Hypertension Society Consensus Conference: 1. Definitions, evaluation and classification of hypertensive disorders in pregnancy. CMAJ. 1997;157:715-25.
4. Davis GK, Mackenzie C, Brown MA, et al. Predicting transformation from gestational hypertension to preeclampsia in clinical practice: a possible role for 24 hour ambulatory blood pressure monitoring. Hypertens Pregnancy. 2007;26:77-87.
5. Karumanchi SA, Maynard SE, Stillman IE, Epstein FH, Sukhatme VP. Preeclampsia: a renal perspective. Kidney Int. 2005;67:2101-13.
6. Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335:974.
7. Callaway LK, Lawlor DA, O'Callaghan M, Williams GM, Najman JM, McIntyre HD. Diabetes mellitus in the 21 years after a pregnancy that was complicated by hypertension: findings from a prospective cohort study. Am J
Obstet Gynecol. 2007;197:492 e1-7.
8. Carr DB, Newton KM, Utzschneider KM, et al. Preeclampsia and risk of developing subsequent diabetes. Hypertens Pregnancy. 2009;28:435-47. 9. Irgens HU, Reisaeter L, Irgens LM, Lie RT. Long term mortality of mothers
and fathers after pre-eclampsia: population based cohort study. BMJ. 2001;323:1213-7.
10. Libby G, Murphy DJ, McEwan NF, et al. Pre-eclampsia and the later development of type 2 diabetes in mothers and their children: an
intergenerational study from the Walker cohort. Diabetologia. 2007;50:523-30.
11. Lykke JA, Langhoff-Roos J, Sibai BM, Funai EF, Triche EW, Paidas MJ. Hypertensive pregnancy disorders and subsequent cardiovascular morbidity
and type 2 diabetes mellitus in the mother. Hypertension. 2009;53:944-51. 12. McDonald SD, Malinowski A, Zhou Q, Yusuf S, Devereaux PJ.
Cardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analyses. Am Heart J. 2008;156:918-30.
13. Wang IK, Chang SN, Liao CC, et al. Hypertensive disorders in pregnancy and preterm delivery and subsequent stroke in Asian women: a retrospective cohort study. Stroke. 2011;42:716-21.
14. Wilson BJ, Watson MS, Prescott GJ, et al. Hypertensive diseases of pregnancy and risk of hypertension and stroke in later life: results from cohort study.
BMJ. 2003;326:845.
15. Garovic VD, Hayman SR. Hypertension in pregnancy: an emerging risk factor for cardiovascular disease. Nat Clin Pract Nephrol. 2007;3:613-22.
16. Gaber LW, Spargo BH, Lindheimer MD. Renal pathology in pre-eclampsia.
Baillieres Clin Obstet Gynaecol. 1994;8:443-68.
17. Bar J, Kaplan B, Wittenberg C, et al. Microalbuminuria after pregnancy complicated by pre-eclampsia. Nephrol Dial Transplant. 1999;14:1129-32. 18. McDonald SD, Han Z, Walsh MW, Gerstein HC, Devereaux PJ. Kidney
disease after preeclampsia: a systematic review and meta-analysis. Am J
Kidney Dis. 2010;55:1026-39.
19. Suzuki H, Watanabe Y, Arima H, Kobayashi K, Ohno Y, Kanno Y. Short- and long-term prognosis of blood pressure and kidney disease in women with a past history of preeclampsia. Clin Exp Nephrol. 2008;12:102-9.
20. Vikse BE, Irgens LM, Leivestad T, Skjaerven R, Iversen BM. Preeclampsia and the risk of end-stage renal disease. N Engl J Med. 2008;359:800-9. 21. Huppertz B. Placental origins of preeclampsia: challenging the current
hypothesis. Hypertension. 2008;51:970-5.
22. Maynard SE, Thadhani R. Pregnancy and the kidney. J Am Soc Nephrol. 2009;20:14-22.
23. Sugimoto H, Hamano Y, Charytan D, et al. Neutralization of circulating vascular endothelial growth factor (VEGF) by anti-VEGF antibodies and soluble VEGF receptor 1 (sFlt-1) induces proteinuria. J Biol Chem. 2003;278:12605-8.
24. Thadhani R, Solomon CG. Preeclampsia--a glimpse into the future? N Engl J
Med. 2008;359:858-60.
25. Nisell H, Lintu H, Lunell NO, Mollerstrom G, Pettersson E. Blood pressure and renal function seven years after pregnancy complicated by hypertension.
Br J Obstet Gynaecol. 1995;102:876-81.
cardiovascular disease events in nonhypertensive and nondiabetic individuals: the Framingham Heart Study. Circulation. 2005;112:969-75.
27. Hallan SI, Ritz E, Lydersen S, Romundstad S, Kvenild K, Orth SR. Combining GFR and albuminuria to classify CKD improves prediction of ESRD. J Am Soc Nephrol. 2009;20:1069-77.
28. Vikse BE, Irgens LM, Bostad L, Iversen BM. Adverse perinatal outcome and later kidney biopsy in the mother. J Am Soc Nephrol. 2006;17:837-45.
29. Collins AJ, Foley RN, Herzog C, et al. Excerpts from the US Renal Data System 2009 Annual Data Report. Am J Kidney Dis. 2010;55:S1-420, A6-7. 30. Wen CP, Cheng TY, Lin CL, et al. The health benefits of smoking cessation
for adult smokers and for pregnant women in Taiwan. Tob Control. 2005;14 Suppl 1:i56-61.
31. Liu TC, Chen CS. The role of Taiwan's National Health Insurance program in influencing adequate prenatal care. Int J Health Plann Manage. 2004;19:113-30.
32. Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan.
Pharmacoepidemiol Drug Saf. 2011;20:236-42.
33. Lin CC, Lai MS, Syu CY, Chang SC, Tseng FY. Accuracy of diabetes diagnosis in health insurance claims data in Taiwan. J Formos Med Assoc. 2005;104:157-63.
Legends
Figure 1: The estimated ESRD-free proportions for cohorts with and without
Table 1: Demographic characteristics and comorbidity in cohorts with and without hypertensive disorders in pregnancy.
Hypertensive disorders in pregnancy p-value
No N = 213,397 Yes N = 26,651 Age, year n % n % 1.00 19 to 24 28,164 13.2 3,515 13.2 25 to 29 68,695 32.2 8,580 32.2 30 to 34 74,148 34.8 9,259 34.7 35 to 40 42,390 19.9 5,297 19.9 Mean (SD) 29.5 (4.75) 29.6 (4.80) Urbanization level n 213359 26648 < 0.001 1 68,310 32.0 8,412 31.6 2 69,253 32.5 8,493 31.9 3 36,961 17.3 4,586 17.2 4 25,023 11.7 3,215 12.1 5 13,812 6.5 1,942 7.3 Baseline comorbidity
Coronary artery disease 88 0.04 11 0.04 1.00
Congestive heart failure 45 0.02 12 0.05 0.02
Hyperlipidemia 119 0.06 37 0.14 < 0.001
After index pregnancy
Coronary artery disease 148 0.07 97 0.36 <0.001 Congestive heart failure 131 0.06 130 0.49 <0.001
Hypertension 549 0.26 973 3.65 < 0.001
Preterm delivery 14,091 6.60 6,551 24.6 < 0.001
Abruption 1,264 0.59 632 2.37 < 0.001
Table 2: Crude and adjusted hazard ratios for chronic kidney disease among women with and without postpartum hypertension
and diabetes during follow-up.
ESRD
Incidence rate per
10 000 person-years Crude HR (95% CI) Adjusted HR (95% CI)
No hypertensive disorders in pregnancy
90 0.67 1.00 1.00
Hypertensive disorders in pregnancy 121 7.24 10.8 (8.20-14.2) 9.38 (7.09-12.4)
Hypertension during follow-up
No hypertensive disorders in pregnancy
43 86.6 1.00 1.00
Hypertensive disorders in pregnancy 94 121 1.39 (0.97-2.00) 1.35 (0.94-1.94)
No hypertension during follow-up
No hypertensive disorders in pregnancy
47 0.35 1.00 1.00
Hypertensive disorders in pregnancy 27 1.69 4.81 (3.00-7.72) 4.37 (2.71-7.07)
Diabetes during follow-up
No hypertensive disorders in pregnancy
5 2.12 1.00 1.00
Hypertensive disorders in pregnancy 19 19.4 9.20 (3.43-24.6) 7.62 (2.80-20.8)
No diabetes during follow-up
No hypertensive disorders in pregnancy
Hypertensive disorders in pregnancy 102 6.47 10.0 (7.53-13.4) 8.92 (6.65-12.0) Note: HR = hazard ratio, CI = confidence interval.
Table 3: Multivariable Cox proportional hazards regression analysis for risk of end-stage renal disease in women.
Incidence rate per 10 000 person-years
Model 1 Model 2 Model 3 Model 4
Variable N ESRD HR (95% CI) HR (95% CI) HR (95% CI) HR (95% CI)
No hypertensive disorders in pregnancy 213,397 45 0.34 1.00 1.00 1.00 1.00 Hypertensive disorders in pregnancy 26,651 79 4.72 14.1 (9.76-10.3) 12.4 (8.54-18.0) 2.72 (1.76-4.22) 1.91 (1.20-3.07) Type of hypertensive disorders in pregnancy Gestational hypertension 8,653 18 3.40 10.2 (5.89-17.6) 9.03 (5.20-15.7) 1.81 (0.99-3.30) 1.38 (0.74-2.57) Preeclampsia/eclampsia 17,998 61 5.33 15.9 (10.8-23.3) 14.0 (9.43-20.7) 3.19 (2.02-5.02) 2.17 (1.33-3.54) p for trend < 0.0011 < 0.0012 < 0.0012 < 0.0012 0.001
Note: HR = hazard ratio, CI = confidence interval. Model 1: crude hazard ratio.
Mode 2: adjusted for urbanization, coronary artery disease, congestive heart failure, hyperlipidemia and abruption. Mode 3: adjusted for the variables in model 2, plus hypertension and diabetes during follow-up. .
Model 4: time-depended model, adjusted for the variables in model 3. 1 Poisson regression; 2 Cox proportional hazards regression
and diabetes during postpartum follow-up ESRD
Incidence rate per
10 000 person-years Crude HR (95% CI) Adjusted HR (95% CI)
Hypertension during follow-up
No hypertensive disorders in pregnancy 25 49.7 1.00 1.00 Hypertensive disorders in pregnancy 61 76.8 1.56 (0.98-2.48) 1.51 (0.95-2.41)
No hypertension during follow-up
No hypertensive disorders in pregnancy 20 0.15 1.00 1.00 Hypertensive disorders in pregnancy 18 1.13 7.56 (4.00-14.3) 6.67 (3.48-12.8)
Diabetes during follow-up
No hypertensive disorders in pregnancy 2 0.85 1.00 1.00 Hypertensive disorders in pregnancy 9 9.14 11.3 (2.44-52.4) 10.6 (2.31-51.0)
No diabetes during follow-up
No hypertensive disorders in pregnancy
43 0.33 1.00 1.00
pregnancy
Note: HR = hazard ratio, CI = confidence interval.