Bilateral locked posterior fracture-dislocation of the shoulders due to electric shock
全文
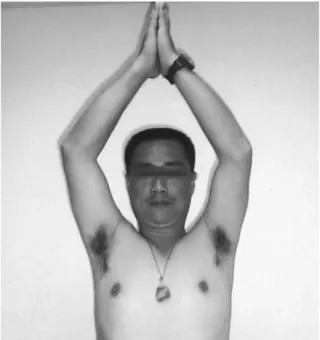
(2) Chin-Jung Hsu, et al.. 133. Fig. 1. Anteroposterior X-ray of the right shoulder shows comminuted fracture of the proximal humerus.. Fig. 2. Anteroposterior X-ray of the left shoulder shows fracture of the proximal humerus.. Fig. 3. CT examination of the right shoulder shows posterior locked fracture-dislocation.. Fig. 4. CT examination of the left shoulder shows posterior locked fracture-dislocation.. N e e r e c l a s s i f i c a t i o n ) ( F i g s . 3,4). Hemiarthroplasties of both shoulders was performed 14 days after injury. Surgery was delayed because of marked swelling of both shoulders and because the heart function needed to be observed. Hemiarthroplasty was performed via an antero-lateral approach between the deltoid and pectoral major muscles. The shoulder joint was operated on after dividing the subscapularis muscle. The humeral head was dislocated posterior to the glenoid fossa and was difficult to remove because it was blocking the posterior glenoid rim; the greater and lesser tuberosities were prepared for reattachment to the shoulder hemiarthroplasty prosthesis. After the operation, the patient wore a Velpeau sling to immobilize. both arms, and gentle pendulum exercises were begun 1 week after the operation. More aggressive physical therapy began after 1 month. The patient was quite satisfied with the surgical result at six year follow-up. X-ray showed good position of both prostheses (Figs. 5, 6). He is pain-free and has mild functional limitation of his shoulders (Fig. 7). Movement in both shoulders recovered to allow 150 degrees of flexion, 150 degrees of abduction, 70 degrees of medial rotation, 45 degrees of lateral rotation and 45 degrees of extension. DISCUSSION. Bilateral posterior fracture-dislocation of the shoulders is a rare injury. Of the 35 cases.
(3) 134. Fig. 5. Anteroposterior X-ray of the right shoulder 6 years after surgery shows good position of the prosthesis.. Fig. 7. Anterior view of the patient shows good range of motion of both shoulders.. which have been reported in the literature, most occurred as a result of seizure; other causes such as electrocution and extreme trauma are less common [3,4]. Our report is the third known case due to electrocution. The cause of bilateral posterior fracture dislocation of the shoulder. Posterior Shoulder Fracture Dislocation. Fig. 6. Anteroposterior X-ray of the left shoulder 6 years after surgery shows good position of the prosthesis.. could be presented as the "triple E syndrome", which describes the causative factors involved in this injury: epilepsy (or any convulsive seizure, including ethanol or drug withdraw seizures), electrocution (including electroconvulsive therapy) and extreme trauma (such as motor vehicle accidents [3,4]. The mechanism of this injury has been described as an extended injury of posterior dislocation [3]. The humeral head is forced superiorly and posteriorly over the glenoid edge as the result of adduction, medial rotation and flexion of muscle spasm. If the convulsion stops, the humeral head stays lodged behind the glenoid, often with a depression noted in the head just medial to the lesser tuberosity. With further convulsive force, however, the glenoid edge shears off the humeral head with associated avulsion of a fragment of the tuberosity caused mainly by spasm of the subscapularis and the infraspinatus muscles. Further comminution is produced by forced contraction of the triceps, the coracobrachialis, the biceps and the deltoid muscles thrusting the fragment of the humeral shaft upwards against the acromion. Thus a fourpart fracture with posterior dislocation is.
(4) Chin-Jung Hsu, et al.. separated from the shaft and the two fragments of the tuberosity [5]. Initial scapular anteroposterior, lateral and axillary X-ray examinations are essential. The axillary view is difficult to perform because it requires patients to abduct their shoulders, which is not always possible after injury. It is not easy to confirm the final diagnosis by X-ray examination, especially if an axillary view cannot be obtained. Computer tomography is essential for this kind of injury and provides excellent visualization of the relationship between the glenoid and the humeral head. The presence, size, and shape of the humeral defect are well demonstrated on CT images, which is useful to the surgeon when surgical intervention is a consideration [6,7]. In our patient, we could not make an accurate diagnosis after viewing the anteroposterior and lateral view of X-ray films of both shoulders. However, a reverse Hill-Sach lesion (> 50 % of articular surface) and extreme fragmenting of both humeral heads were noticeable on CT. There are several methods for treating posterior fracture-dislocations of the shoulder: closed reduction, open reduction and internal fixation, McLaughlin's procedure and its modifications, hemiarthroplasty, total shoulder arthroplasty, and arthrodesis, depending on a number of factors: patient age, the chance of avascular necorsis, duration of the dislocation, defect of the articular surface of the humeral head, and extent of damage to the glenoid [8]. The major arterial supply of the humeral head is via the anterior humeral circumflex artery. The vessel runs parallel to the lateral aspect of the tendon of the long head of the biceps and enters the humeral head where the proximal end of the intertubercular groove meets the greater tuberosity [9]. After a four-part fracture, open reduction with internal fixation is essential if arcuate artery is preserved. The radiographic indication for arcuate artery preservation is the attachment of the neck's medial cortex to the shaft [10]. In our experience, closed reduction is rarely successful for treating acute posterior fracture-. 135. dislocation. Martens and Hessels [11] described a method with a small posterior arthrotomy that allowed reduction of the humeral head using a finger; however, many reports suggest treating these lesions with open reduction [3,12,13] and internal fixation or hemiarthroplasty [14,15]. When an extensive fragmentation is present, especially in four-part fracturedislocations, the risk of avascular necrosis increases and hemiarthroplasty is preferred. In young patients, hemiarthroplasty should be avoided only when the risk of avascular necrosis is high. Because of extensive fragmentation and severe cartilage compression in our patient, open reduction with internal fixation was impossible and hemiarthroplasties were performed although the patient was young. Excellent functional results in both shoulders were achieved postoperatively. REFERENCES. 1. Neer CS 2nd. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg (Am) 1970;52:1077-89. 2. Neer CS 2nd. Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J Bone Joint Surg (Am) 1970;52:1090-103. 3. Brackstone M, Patterson SD, Kertesz A. Triple "E" syndrome: bilateral locked posterior fracture dislocation of the shoulders. Neurology 2001;56:1403-4. 4. O'Flanagan PH. Fracture due to shock from domestic electricity supply. Injury 1975;6:244-5. 5. Din KM, Meggitt BF. Bilateral four-part fractures with posterior dislocation of the shoulder. A case report. J Bone Joint Surg (Br) 1983;65:176-8. 6. Wadlington VR, Hendrix RW, Rogers LF. Computed tomography of posterior fracture-dislocations of the shoulder: case reports. J Trauma 1992;32:113-5. 7. Aparicio G, Calvo E, Bonilla L, et al. Neglected traumatic posterior dislocations of the shoulder: controversies on indications for treatment and new CT scan findings. J Orthop Sci 2000;5:37-42. 8. Mancini GB, Lazzeri S. Bilateral posterior fracturedislocation of the shoulder. Orthopedics 2002; 25:433-4. 9. Gerber C, Schneeberger AG, Vinh TS. The arterial vascularization of the humeral head. An anatomical study. J Bone Joint Surg (Am) 1990;72:1486-94..
(5) 136. 10. Brooks CH, Revell WJ, Heatley FW. Vascularity of the humeral head after proximal humeral fractures. An anatomical cadaver study. J Bone Joint Surg Br 1993; 75:132-6. 11. Martens C, Hessels G. Bilateral posterior four-part fracture-dislocation of the shoulder. Acta Orthop Belg 1995;61:249-54. 12.Blasier RB, Burkus JK. Management of posterior fracture-dislocations of the shoulder. Clin Orthop Relat Res 1988;232:197-204. 13.Lindholm TS, Elmstedt E. Bilateral posterior. Posterior Shoulder Fracture Dislocation. dislocation of the shoulder combined with fracture of the proximal humerus. A case report. Acta Orthop Scand 1980;51:485-8. 14. Page AE, Meinhard BP, Schulz E, et al. Bilateral posterior fracture-dislocation of the shoulders: management by bilateral shoulder hemiarthroplasties. J Orthop Trauma 1995;9:526-9. 15. Reckling FW. Posterior fracture-dislocation of the shoulder treated by a Neer hemiarthroplasty with a posterior surgical approach. Clin Orthop Relat Res 1986;207:133-7..
(6) 137. 1,3. 2,3. 3. 1,3 1. 2 3. 6 2006;11:132-7. 404. 2. 2005. 11. 2006. 1. 8 5. 2005. 12. 15. 1,3.
(7)
數據

相關文件
We also used reduction and reverse reduction to design a novel boosting ap- proach, AdaBoost.OR, to improve the performance of any cost-sensitive base ordinal ranking algorithm..
Animal or vegetable fats and oils and their fractiors, boiled, oxidised, dehydrated, sulphurised, blown, polymerised by heat in vacuum or in inert gas or otherwise chemically
Milk and cream, in powder, granule or other solid form, of a fat content, by weight, exceeding 1.5%, not containing added sugar or other sweetening matter.
In fact, one way of getting from Fourier series to the Fourier transform is to consider nonperiodic phenomena (and thus just about any general function) as a limiting case of
Root the MRCT b T at its centroid r. There are at most two subtrees which contain more than n/3 nodes. Let a and b be the lowest vertices with at least n/3 descendants. For such
1 As an aside, I don’t know if this is the best way of motivating the definition of the Fourier transform, but I don’t know a better way and most sources you’re likely to check
Wang, Solving pseudomonotone variational inequalities and pseudocon- vex optimization problems using the projection neural network, IEEE Transactions on Neural Networks 17
In BHJ solar cells using P3HT:PCBM, adjustment of surface energy and work function of ITO may lead to a tuneable morphology for the active layer and hole injection barrier